Discussion
Dermoscopy is a non-invasive tool that is largely recognized and used in the diagnosis of pigmented and non-pigmented skin tumors. A steadily increasing number of publications on alternative applications of dermoscopy suggest, however, that dermoscopy aids also the recognition of skin manifestations in general dermatology.
The increasing use of dermoscopy in general dermatology can be partially explained by commercially available new generations of handheld dermoscopes, which are small enough to be easily placed in every dermatologist’s pocket. Moreover, some devices do not require direct contact between the patient’s skin and the optical glass plate, thus enabling a rapid and safe examination without the risk of possible transfection.
The wide and variable spectrum of traditional and newer applications of dermoscopy can be subdivided into the following six new main indications:
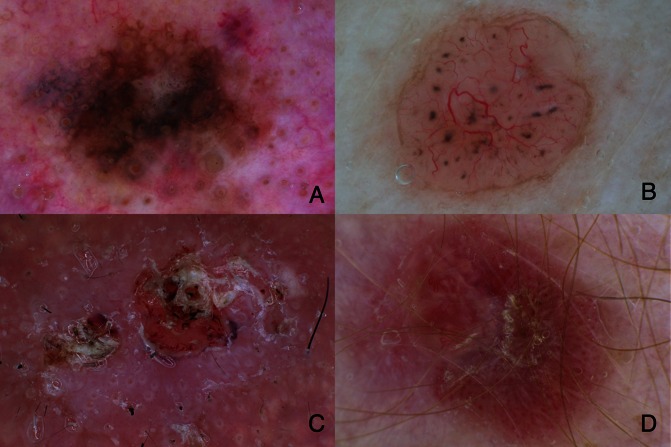
Classic dermoscopy for the diagnosis of pigmented and non-pigmented skin tumors (Figure 1) including melanocytic and non-melanocytic and benign and malignant skin tumors [1–5].
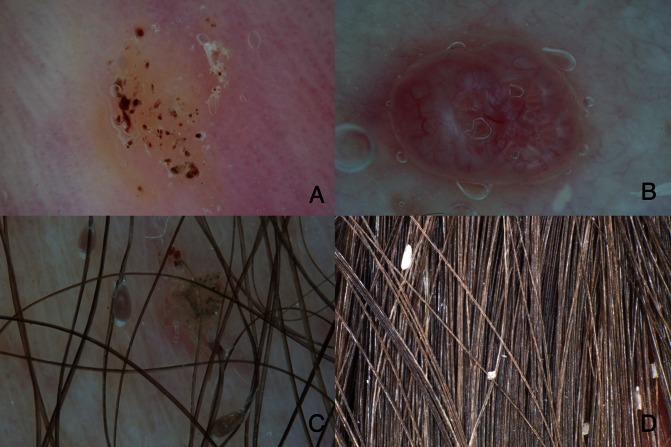
Entomodermoscopy for the diagnosis of skin infections and infestations (Figure 2) caused by parasites or viral, bacterial, fungal or protozoan infections [6–9].
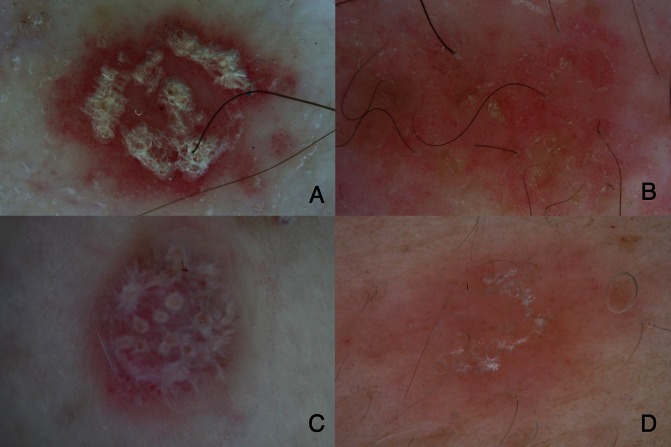
Inflammoscopy for the diagnosis of inflammatory skin diseases (Figure 3), such as psoriasis, lichen ruber planus, pityriasis rosea and many others [10–12].
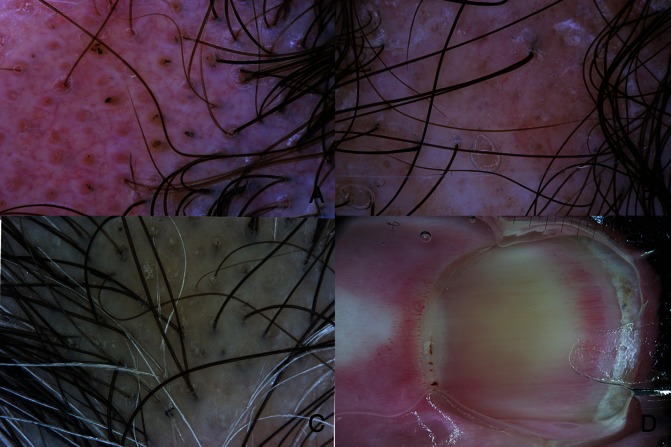
Trichoscopy for diagnosing hair and scalp disorders (Figure 4A, B, C) [13–15].
Capillaroscopy of the nail fold capillaries for the screening of autoimmune diseases (Figure 4D) [16–18].
Dermoscopy for treatment decision and monitoring: This application gains importance especially in the light of the steadily increasing availability and use of topical treatment options for non-melanoma skin cancer (Figure 5) [20–22].
Figure 1.
Classic dermoscopy improves the early diagnosis of melanoma and non-melanoma skin cancer. (A) Melanoma in situ, lentigo maligna subtype, showing gray, brown and white colors as well as gray circles (asymmetric pigmented follicular openings and gray dots (gray pepper-like granules). (B) Nodular basal cell carcinoma showing loosely arranged gray globules and focused branching, arborizing vessels. (C) Invasive squamous cell carcinoma showing a white-pink background intermingled with white circles (targetoid appearing follicular openings consisting of an inner yellow globule and an outer white rim) and central yellow-white-red structureless areas (=keratin). (D) Amelanotic melanoma characterized by dotted and linear-irregular vessels (=polymorphous vessels). Original magnification x10. [Copyright: ©2013 Zalaudek et al.]
Figure 2.
Entomodermoscopy improves the diagnosis of skin infestations and infections. (A) Stereotypical appearance of plantar viral wart showing structureless white-yellow areas and multiple small linear brown to red dots and streaks (=splinter hemorrhages). (B) Molluscum contagiosum is typified by central opaque yellowish globules, which are surrounded by blurred linear vessels (=crown vessels). (C) Dermoscopy of phthiriasis pubis with vital nits attached to the hair shaft. Vital nits have a convex end and appear translucent brownish. (D) Dermoscopy of pseudo-nits due to hair casts, which appear as white amorphous structures attached to the hair shaft. Original magnification x10. [Copyright: ©2013 Zalaudek et al.]
Figure 3.
Inflammoscopy improves the differential diagnosis of inflammatory skin disorders. (A) Dermoscopy of psoriasis shows regularly arranged dotted vessels and white scales. (B) Dermoscopy of nummular eczema is typified by dotted vessels in a patchy arrangement and yellow scales. (C) Lichen ruber planus shows white streaks (=Whickham striae) over a red background and dotted and linear vessels. (D) Pityriasis rosea is characterized a red-brown structureless color and fine white translucent scales that “hang” from the periphery towards the center like a curtain. Original magnification x10. [Copyright: ©2013 Zalaudek et al.]
Figure 4.
Trichoscopy and capillaroscopy. (A) Clinical image of a patient with alopecia areata showing yellow globules corresponding to hair follicles, cadaverized and exclamation hairs. (B) Dermoscopy of scarring alopecia due to discoid lupus erythematosus. There is a significant reduction of the hair follicles. Some linear vessels are additionally seen. (C) Dermoscopy of lichen planopilaris is characterized by keratotic scales within and around the hair shaft and reduced number of follicular openings. (D) Capillaroscopy of the nail fold of a patient with systemic scleroderma reveals twisted and elongated nail fold capillaries as well as micro-hemorrhages in the cuticula. Original magnification x10. [Copyright: ©2013 Zalaudek et al.]
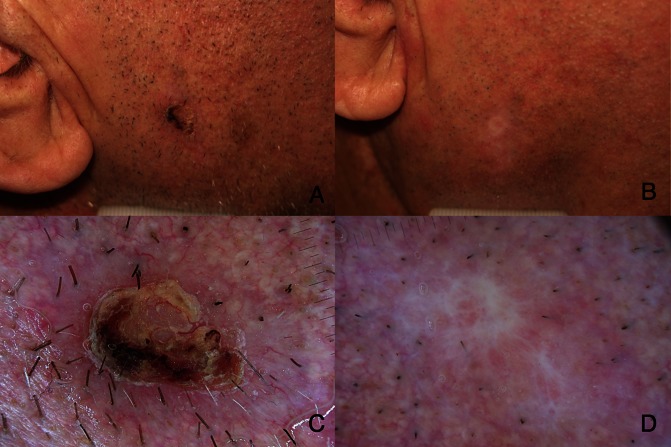
Figure 5.
Clinical image of basal cell carcinoma (A) before and (B) two months after a six-week cycle of imiquimod 5% cream applied five times a week. (C) Dermoscopy of basal cell carcinoma at baseline showing peripheral focused arborizing vessels and a central ulceration. (D) After successful topic treatment, there is absence of criteria suggestive of persistence. Only white scar-like areas are visible. [Copyright: ©2013 Zalaudek et al.]
Conclusion
In summary, dermoscopy should be regarded as a safe and rapid diagnostic tool that assists in clinical examination and management decision in dermatology, as the stethoscope does for diagnosing heart, lung or abdominal problems. As a consequence, dermoscopy can be nowadays seen as the dermatologists’ stethoscope.
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
References
- 1.Vestergaard ME, Macaskill P, Holt PE, Menzies SW. Dermoscopy compared with naked eye examination for the diagnosis of pri-mary melanoma: a meta-analysis of studies performed in a clinical setting. Br J Dermatol. 2008;159(3):669–76. doi: 10.1111/j.1365-2133.2008.08713.x. [DOI] [PubMed] [Google Scholar]
- 2.Fargnoli MC, Kostaki D, Piccioni A, Micantonio T, Peris K. Dermoscopy in the diagnosis and management of non-melanoma skin cancers. Eur J Dermatol. 2012;22(4):456–63. doi: 10.1684/ejd.2012.1727. [DOI] [PubMed] [Google Scholar]
- 3.Zalaudek I, Giacomel J, Schmid K, et al. Dermatoscopy of facial actinic keratosis, intraepidermal carcinoma, and invasive squamous cell carcinoma: a progression model. J Am Acad Dermatol. 2012;66(4):589–97. doi: 10.1016/j.jaad.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Rosendahl C, Tschandl P, Cameron A, Kittler H. Diagnostic accuracy of dermatoscopy for melanocytic and nonmelanocytic pigmented lesions. J Am Acad Dermatol. 2011;64(6):1068–73. doi: 10.1016/j.jaad.2010.03.039. [DOI] [PubMed] [Google Scholar]
- 5.Lallas A, Apalla Z, Lefaki I, et al. Dermoscopy of early stage mycosis fungoides. J Eur Acad Dermatol Venereol. 2012 Mar 9; doi: 10.1111/j.1468-3083.2012.04499.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Tschandl P, Argenziano G, Bakos R, et al. Dermoscopy and entomology (entomodermoscopy) J Dtsch Dermatol Ges. 2009;7(7):589–96. doi: 10.1111/j.1610-0387.2009.07027.x. [DOI] [PubMed] [Google Scholar]
- 7.Zalaudek I, Giacomel J, Cabo H, et al. Entodermoscopy: a new tool for diagnosing skin infections and infestations. Dermatology. 2008;216(1):14–23. doi: 10.1159/000109353. [DOI] [PubMed] [Google Scholar]
- 8.Zalaudek I, Argenziano G. Images in clinical medicine. Dermoscopy of nits and pseudonits. N Engl J Med. 2012;367(18):1741. doi: 10.1056/NEJMicm1103059. [DOI] [PubMed] [Google Scholar]
- 9.Dupuy A, Dehen L, Bourrat E, et al. Accuracy of standard dermoscopy for diagnosing scabies. J Am Acad Dermatol. 2007;56(1):53–62. doi: 10.1016/j.jaad.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 10.Zalaudek I, Argenziano G, Di Stefani A, et al. Dermoscopy in general dermatology. Dermatology. 2006;212(1):7–18. doi: 10.1159/000089015. [DOI] [PubMed] [Google Scholar]
- 11.Lallas A, Apalla Z, Lefaki I, et al. Dermoscopy of discoid lupus erythematosus. Br J Dermatol. 2012;168(2):282–8. doi: 10.1111/bjd.12044. [DOI] [PubMed] [Google Scholar]
- 12.Lallas A, Kyrgidis A, Tzellos TG, et al. Accuracy of dermoscopic criteria for the diagnosis of psoriasis, dermatitis, lichen planus and pityriasis rosea. Br J Dermatol. 2012;166(6):1198–205. doi: 10.1111/j.1365-2133.2012.10868.x. [DOI] [PubMed] [Google Scholar]
- 13.Olszewska M, Rudnicka L, Rakowska A, Kowalska-Oledzka E, Slowinska M. Trichoscopy. Arch Dermatol. 2008;144(8):1007. doi: 10.1001/archderm.144.8.1007. [DOI] [PubMed] [Google Scholar]
- 14.Rudnicka L, Olszewska M, Rakowska A, Slowinska M. Trichoscopy update 2011. J Dermatol Case Rep. 2011;5(4):82–8. doi: 10.3315/jdcr.2011.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol. 2012;67(5):1040–8. doi: 10.1016/j.jaad.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 16.Bergman R, Sharony L, Schapira D, Nahir MA, Balbir-Gurman A. The handheld dermatoscope as a nail-fold capillaroscopic instrument. Arch Dermatol. 2003;139(8):1027–30. doi: 10.1001/archderm.139.8.1027. [DOI] [PubMed] [Google Scholar]
- 17.Vázquez-López F, Marghoob AA. Dermoscopy vs capillaroscopy of nontumoral dermatoses. Arch Dermatol. 2004;140(5):617. doi: 10.1001/archderm.140.5.617-a. [DOI] [PubMed] [Google Scholar]
- 18.Hasegawa M. Dermoscopy findings of nail fold capillaries in connective tissue diseases. J Dermatol. 2011;38(1):66–70. doi: 10.1111/j.1346-8138.2010.01092.x. [DOI] [PubMed] [Google Scholar]
- 19.Beltrán E, Toll A, Pros A, Carbonell J, Pujol RM. Assessment of nailfold capillaroscopy by x 30 digital epiluminescence (dermoscopy) in patients with Raynaud phenomenon. Br J Dermatol. 2007;156(5):892–8. doi: 10.1111/j.1365-2133.2007.07819.x. [DOI] [PubMed] [Google Scholar]
- 20.Kaçar N, Sanli B, Zalaudek, Yildiz N, Ergin S. Dermatoscopy for monitoring treatment of actinic keratosis with imiquimod. Clin Exp Dermatol. 2012;37(5):567–9. doi: 10.1111/j.1365-2230.2011.04272.x. [DOI] [PubMed] [Google Scholar]
- 21.Micantonio T, Fargnoli MC, Peris K. Usefulness of dermoscopy to monitor clinical efficacy of imiquimod treatment for lentigo maligna. Arch Dermatol. 2006;142(4):530–1. doi: 10.1001/archderm.142.4.530-b. [DOI] [PubMed] [Google Scholar]
- 22.Micantonio T, Fargnoli MC, Piccolo D, Perris K. Letter: Changes in dermoscopic features in superficial basal cell carcinomas treated with imiquimod. Dermatol Surg. 2007;33(11):1403–5. doi: 10.1111/j.1524-4725.2007.33303.x. [DOI] [PubMed] [Google Scholar]