Abstract
Background:
The introduction of the smartphone with high-quality, built-in digital cameras and easy-to-install software may make it more convenient to perform teledermatology. In this study we looked at the feasibility of using a smartphone (iPhone 4®) with an installed application especially developed for teledermatology (iDoc24®) and a dermoscope (FotoFinder Handyscope®) that is customized to attach to the smartphone to be able to carry out mobile teledermoscopy.
Objectives:
To study the diagnostic accuracy of this mobile teledermoscopy solution, to determine the interobserver concordance between teledermoscopists (TDs) and a dermatologist meeting the patient face-to-face (FTF), and to assess the adequacy of the TDs’ management decisions and to evaluate the image quality obtained.
Patients/Methods:
During a 16-week period, patients with one or more suspicious skin lesions deemed to need a biopsy or excision were included. The smartphone app was used to send a clinical image, a dermoscopy image and relevant clinical information to a secure Internet platform (Tele-Dermis®). Two TDs assessed the incoming cases, providing a specific primary diagnosis and a management decision. They also graded the image quality. The histopathological diagnosis was used as the gold standard.
Results:
Sixty-nine lesions were included. The FTF dermatologist’s diagnostic accuracy was 66.7%, which was statistically higher than TD 1 (50.7%, P=0.04) but similar to TD 2 (60.9%, P=0.52). The interobserver concordances between the FTF dermatologist and the two TDs and between the respective TDs showed moderate to substantial agreement. The TDs provided adequate management decisions for 68 (98.6%) and 69 (100%) lesions, respectively. The image quality was rated as excellent or sufficient in 94% and 84% of the cases by the respective TDs.
Conclusion:
This novel mobile teledermoscopy solution may be useful as a triage tool for patients referred to dermatologists for suspicious skin lesions.
Keywords: mobile teledermoscopy, smartphone application, teledermatology, malignant melanoma, non-melanoma skin cancer
Introduction
The incidence of skin cancer is increasing among fair-skinned individuals worldwide due to excessive sun exposure, an older population, and an increase in the number of immunosuppressed patients [1,2]. In 2010, melanoma and squamous cell carcinoma represented 14% of all cancers diagnosed in Sweden [3]. Furthermore, 15% of male and female Swedes will develop at least one basal cell carcinoma before the age of 74 years [4]. Meanwhile, national health budgets in the western world are strained with limited resources to handle an aging population [5].
In Sweden, referrals from general practitioners (GPs) are paper-based, are sent by post, and contain no photographic documentation. In addition, they often lack important descriptive clinical details. With written paper referrals, there is a theoretical risk that patients with malignant lesions can be incorrectly triaged as having a low level of suspicion with subsequent long waiting times and vice versa. Therefore, novel and more effective approaches to how skin cancer patients are referred to dermatologists are warranted.
Sending digital images of skin lesions with relevant clinical information to a dermatologist for his/her opinion is known as teledermatology [6]. When dermoscopic images of the lesions are included, the consultation is called teledermoscopy [7]. Teledermatology and teledermoscopy have shown promising results with high concordance in diagnostic accuracy in comparison with face-to-face (FTF) visits [8–16]. Clinical and dermoscopic images and relevant clinical information can be sent by email [8,14], through specialized telemedicine software and virtual private networks for online consultation [9,10,12,13,15] or via Multimedia Messaging System (MMS) [17]. Today, with the introduction of smartphones with built-in digital cameras and Internet connectivity, one could also use a so-called mobile application or “app” for teledermatology. Moreover, several companies have also started producing dermoscopes that can be coupled with smartphones. In other words, mobile teledermoscopy referrals could become a reality if GPs were provided with a smartphone with a pre-installed teledermoscopy referral app and a customized dermoscope.
The primary objective of this study was to determine the diagnostic accuracy of a digital referral process using a novel mobile teledermoscopy app. The secondary objectives were to analyze the interobserver concordances between two teledermoscopists (TDs) and a FTF dermatologist, the adequacy of the management decisions provided by the TDs, as well as the quality of the acquired images.
Materials and methods
During a 16-week period, consecutive patients with one or more suspicious skin lesions were included in the study if a biopsy or excision was deemed to be necessary after clinical and dermoscopic examination during a FTF visit with a single dermatologist. All patients had previously been referred to the Department of Dermatology at Sahlgrenska University Hospital by a GP. The exclusion criteria were: patients under 18 years, patients with no knowledge of the Swedish language, skin lesions located on a part of the skin that did not allow for digital photography with the smartphone and customised dermoscope used in the study and skin lesions in which histopathological examination was not performed. The local ethics committee approved the study and all patients gave written informed consent prior to inclusion.
The study was carried out using a smartphone (iPhone® 4, Apple, Cupertino, California, USA), a dermoscope customised to be attached to the smartphone (FotoFinder Handyscope®, FotoFinder Systems GmbH, Bad Birnbach, Germany), a secure web-based teledermoscopy platform (Tele-Dermis®, iDoc24® AB, Gothenburg, Sweden) and an iPhone app (iDoc24® AB, Gothenburg, Sweden) installed on the smartphone. This equipment is shown in Figure 1. A dermatologist with several years of experience in the fields of skin cancer and dermoscopy first evaluated the skin lesions clinically and with manual dermoscopy during a FTF visit. Before performing a biopsy or an excision, a case was created in the smartphone app for each skin lesion simulating a teledermoscopy referral.
Figure 1.
Technologic equipment used in the mobile teledermoscopy solution: (A) the smartphone (iPhone 4®) with the iDoc24® app showing on the display; (B) the dermoscope (Fotofinder Handyscope®) with its six light-emitting diodes lit; (C) the dermoscope attached to the smartphone displaying a dermoscopic image of a reticular nevus; and (D) a dermatologist viewing a case on the Internet platform (Tele-Dermis®). [Copyright: ©2013 Börve et al.]
The app first prompted the user to take one clinical overview image of the skin lesion with the smartphone’s 5-mega-pixel digital camera using the autofocus function. In order to standardize photography as much as possible, the user was advised to acquire the images in a well-illuminated room, using a neutral background, no flash, autofocus and an appropriate distance from the patient to include the detail as well as important surrounding skin structures. Then, a single dermoscopic image was taken with the same camera after attaching the smartphone to the customised dermoscope. The contact dermoscope used polarized light from light-emitting diodes and provided up to 20x magnification. The resulting digital photographs had a size of 1024 × 766 pixels. Finally, all relevant clinical information about the patient and lesion were added to a standardized query form in the app including: age, sex, a lesion description, size (mm), localization, duration, symptoms, previous treatments and other relevant medical information. The referral was then sent to the Tele-Dermis® platform using the smartphone’s 3G Inter-net connection. The whole referral process required approximately two minutes to carry out per case.
All information sent through the app was anonymous. Upon sending the referral, the app automatically created a unique 8-digit identification code that was saved in the referring physician’s smartphone and on the Tele-Dermis® platform. The system simultaneously sent email notifications to the two TDs for assessment. The participating TDs were two specialists in dermatology who also had several years of experience within the fields of skin cancer and dermoscopy. The email received by the TDs contained a direct link to the Tele-Dermis® platform. After logging in, the cases were assessed and triaged independently by both TDs on a computer screen (19-inch liquid crystal display monitor). They were asked to assess if the lesion was benign or malignant and if it was melanocytic or non-melanocytic. They were also asked to choose one of the following specific primary diagnoses: melanoma, melanoma in situ, dysplastic nevus, benign nevus, basal cell carcinoma, squamous cell carcinoma, squamous cell carcinoma in situ, actinic keratosis, seborrhoeic keratosis, dermatofibroma, angioma or other. Potential differential diagnoses were not taken into consideration. Furthermore, they provided a management decision (excision, biopsy, follow-up with digital dermoscopy or no treatment), they evaluated the image quality (excellent, sufficient or poor) and they judged the level of diagnostic difficulty (high or low). The same assessment was also carried out separately by the FTF-dermatologist.
The assessments regarding the nature of the lesion (benign vs. malignant, melanocytic vs. non-melanocytic and the specific primary diagnosis) were compared to the histopathological diagnosis (gold standard) in order to analyse the diagnostic accuracy of the FTF-dermatologist and both TDs. In order to study any differences between the FTF-dermatologist and the respective TDs or between TD 1 and TD 2, exact McNemar tests were carried out. The interobserver concordances for these parameters were also calculated using Raw Rate and Cohen’s Kappa (κ) analyses. Furthermore, interobserver concordances were analysed using the same statistical methods in regards to the management decision, the image quality and the level of diagnostic difficulty. Statistical significance was taken as P <0.05.
Results
Sixty-two consecutive patients (24 female and 38 male) with a mean age of 64 years (range 25–94 years) were included in the study. Six patients had multiple lesions. Four of them had two lesions and two patients had three, which were initially included. However, one of the patients with three lesions ended up only having two excised during surgery. Thus, one lesion was excluded, giving a total of 69 included lesions.
The histopathological diagnoses and the nature of these 69 lesions are shown in Table 1. In total, there were 40 malignant lesions (58%, 12 melanocytic and 28 non-melanocytic) and 29 benign lesions (42%, 18 melanocytic and 11 non-melanocytic). The number of melanocytic and non-melanocytic lesions was thus 30 (43.5%) and 39 (56.5%), respectively.
TABLE 1.
Number of benign or malignant and melanocytic or non-melanocytic lesions included in the study. [Copyright: ©2013 Börve et al.]
| Histopathological diagnosis | Number of lesions (%) |
|---|---|
| Malignant melanocytic lesions | |
| Melanoma | 5 (7.2%) |
| Melanoma in situ | 7 (10.1%) |
| Benign melanocytic lesions | |
| Dysplastic nevus | 12 (17.4%) |
| Benign nevus | 6 (8.7%) |
| Malignant non-melanocytic lesions | |
| Basal cell carcinoma | 25 (36.2%) |
| Squamous cell carcinoma | 1 (1.4%) |
| Squamous cell carcinoma in situ | 1 (1.4%) |
| Cutaneous metastasis | 1 (1.4%) |
| Benign non-melanocytic lesions | |
| Seborrhoeic keratosis | 6 (8.7%) |
| Angioma | 2 (2.9%) |
| Other | 3 (4.3%) |
| Total | 69 (100%) |
The diagnostic accuracy of the FTF dermatologists and the two TDs is shown in Table 2.
TABLE 2.
Diagnostic accuracy of the face-to-face dermatologist and the two teledermoscopists in relation to the specific primary diagnosis and the classification of the lesion in different diagnostic categories. [Copyright: ©2013 Börve et al.]
| Diagnostic level | FTF (95% CI)* | TD 1 (95% CI)* | TD 2* (95% CI)* |
|---|---|---|---|
| Primary diagnosis | 66.7% (54.9–76.6%) | 50.7% (39.2–62.2%) | 60.9% (49.1–71.5%) |
| Benign vs malignant | 87.0% (77.0–93.0%) | 75.4% (64.0–84.0%) | 79.7% (68.8–87.5%) |
| Melanocytic vs non-melanocytic | 89.9% (80.5–95.0%) | 84.1% (73.7–90.9%) | 92.8% (84.1–96.9%) |
| Combination** | 79.7% (68.8–87.5%) | 68.1% (56.4–77.9%) | 76.8% (65.6–85.2%) |
FTF, Face-to-face dermatologist; TD 1, Teledermoscopist 1; TD 2, Teledermoscopist 2; CI, Confidence interval.
Combination of correct classification as benign or malignant and melanocytic or non-melanocytic.
The specific primary diagnosis given by the FTF dermatologist was correct for 46 lesions (66.7%), showing statistically higher accuracy than TD 1 who diagnosed 35 lesions correctly (50.7%, P=0.04) but similar accuracy compared to TD 2 who had 42 correct diagnoses (60.9%, P=0.52). No statistical differences were observed between the two TDs for the specific primary diagnosis (P=0.19). Accuracy increased for all three dermatologists when it came to classifying the lesions as benign or malignant and/or melanocytic or non-melanocytic. As shown in Table 2, the diagnostic accuracy was highest for all three dermatologists when differentiating between melanocytic and non-melanocytic lesions but dropped slightly when classifying the lesions as benign or malignant. Consequently, the diagnostic accuracy in regards to lesion classification combining the diagnostic categories was also lower. For the classification of the lesions as benign or malignant, melanocytic or non-melanocytic and the combination of both criteria, no statistical differences were observed between the FTF dermatologist and the respective TDs or between TD 1 and TD 2.
As shown in Table 3, the interobserver concordance (raw rate) for the specific primary diagnosis was 55% between the FTF dermatologist and TD 1, 57% between the FTF dermatologist and TD 2, and 58% between TD 1 and TD 2. The resulting Cohen’s κ values were 0.47, 0.48 and 0.51, respectively. The interobserver concordances for lesion classification in the different diagnostic categories ranged from 71–91% with κ values of 0.49–0.82. The interobserver concordances observed between the FTF dermatologist and the two TDs and between the respective TDs were practically identical for all levels of diagnosis.
TABLE 3.
Interobserver concordance. [Copyright: ©2013 Börve et al.]
| FTF vs TD 1* | FTF vs TD 2* | TD 1 vs TD 2* | ||||
|---|---|---|---|---|---|---|
| Diagnostic level | IOC (95% CI)* | κ* | IOC (95% CI)* | κ* | IOC (95% CI)* | κ* |
| Primary diagnosis | 55% (43–67%) | 0.47 | 57% (44–68%) | 0.48 | 58% (45–70%) | 0.51 |
| Benign vs malignant | 77% (65–86%) | 0.50 | 78% (67–87%) | 0.50 | 78% (67–87%) | 0.49 |
| Melanocytic vs non-melanocytic | 88% (78–95%) | 0.77 | 91% (82–97%) | 0.82 | 88% (78–95%) | 0.77 |
| Combination** | 71% (59–81%) | 0.60 | 72% (60–83%) | 0.61 | 71% (59–81%) | 0.59 |
FTF, face-to-face dermatologist; TD 1, teledermoscopist 1; TD 2, teledermoscopist 2; IOC, interobserver concordance; CI, confidence interval; κ, kappa value.
Combination of correct classification as benign or malignant and melanocytic or non-melanocytic.
Management decisions were only considered to be adequate for malignant melanocytic lesions if the dermatologist chose to excise them. Biopsy or excision was considered adequate management for malignant non-melanocytic lesions, whereas any alternative was considered adequate for all benign lesions. The TDs were not completely blinded from the FTF dermatologist’s management decision since they knew that all lesions were going to be either biopsied or excised, but they still elected follow-up with digital dermoscopy or no treatment for some cases as shown in Table 4. Subsequently, TD 1 provided adequate management decisions in 68 cases (98.6%). In one case, ‘no treatment’ would have been chosen for a melanoma in situ that was given a primary specific diagnosis of benign nevus. TD 2 would have managed all 69 cases (100%) adequately. The interobserver concordance in regards to the management decisions between the TDs was 68% (95% CI, 56–79%) with a κ value of 0.34.
TABLE 4.
Management decisions. [Copyright: ©2013 Börve et al.]
| Management | FTF* | TD 1* | TD 2* |
|---|---|---|---|
| Excision | 53 | 46 | 51 |
| Biopsy | 16 | 9 | 9 |
| FU digital dermoscopy* | 0 | 2 | 5 |
| No treatment | 0 | 12 | 4 |
FTF, face-to-face dermatologist; TD 1, teledermoscopist 1; TD 2, teledermoscopist 2; FU, follow-up
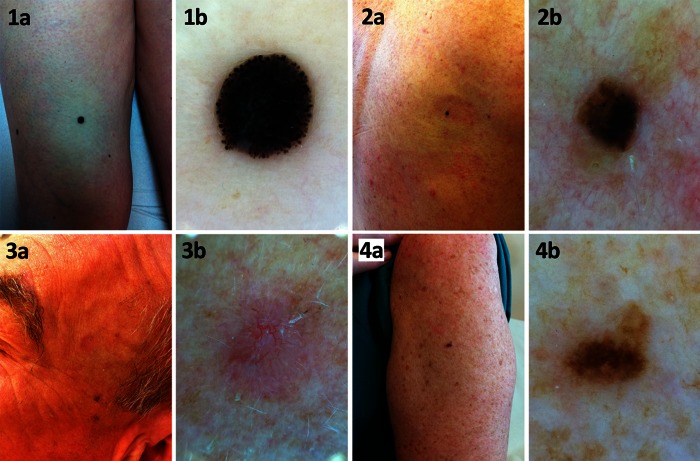
Regarding the diagnostic difficulty of the 69 lesions, the FTF dermatologist considered that 37 lesions had a high diagnostic difficulty (53.6%). However, TD 1 and TD 2 scored 60 (87.0%) and 42 lesions (60.9%) respectively as having a high diagnostic difficulty. The image quality was deemed to be excellent in 61 cases (88.4%) and sufficient in 8 cases (11.6%) by the FTF dermatologist. TD 1’s ratings were clearly worse with 65 cases (94.2%) rated as having sufficient quality and 4 cases (5.8%) as having poor quality. TD 2’s scores were in between, resulting in 15 cases (21.7%) with excellent quality, 43 cases (62.3%) with sufficient quality and 11 cases (15.9%) with poor quality. There was poor agreement between all three dermatologists regarding the image quality (κ values around 0). Three examples of the image quality obtained are shown in Figure 2.
Figure 2.
Image quality of four different lesions included in the study. Clinical and dermoscopic images of: (A,B) a spitzoid nodular melanoma; (C,D) a seborrheic keratosis (note: this was the only case in which both teledermoscopists rated the images as having poor quality); (E,F)) a basal cell carcinoma; and (G,H) a dysplastic nevus. [Copyright: ©2013 Börve et al.]
Discussion
The diagnostic accuracy of the TDs using this novel mobile teledermoscopy app was comparable to that of the FTF dermatologist in regards to the primary diagnosis and in regards to the classification of the lesions in the various diagnostic categories. The only statistically significant difference was the lower diagnostic accuracy of TD1 in regards to the primary diagnosis (50.7%), when compared to the FTF dermatologist (66.7%). Overall, the diagnostic accuracy in regards to the primary diagnosis in our study was within the ranges observed in two teledermoscopy studies designed similarly to ours. In these studies, the diagnostic accuracy for the primary diagnosis was 46.8 % for nonpigmented neoplasms and 51.6%–56.9% for pigmented neoplasms depending on the type of dermoscope used [9,10].
In comparison with other teledermoscopy studies, however, the diagnostic accuracy of the TDs in our study was slightly lower, which in most cases may be due to differences in study design. Tan et al obtained a diagnostic accuracy of 72.3% using teledermoscopy, but included evidently benign lesions and did not use histopathology as their gold standard [15]. In a Swiss study including 55 histopathologically verified lesions, the diagnostic accuracy was 74.5 % when classifying the lesions in diagnostic categories [12]. In a study by Blum et al, three TDs with varying experience in dermoscopy reviewed 157 lesions and were able to recognize the correct diagnostic category in 87.0%–90.7% of the cases [11]. A recent study using dermoscopic images taken with a mobile phone camera manually applied onto a pocket dermoscope showed a diagnostic accuracy of 75%. However, this study included differential diagnoses, 8% of the lesions were excluded due to poor image quality and not all lesions were confirmed histopathologically [13]. A study by Piccolo et al on 66 lesions resulted in a diagnostic accuracy of 86%, but 97% of the lesions were benign [16]. Similarly, a Spanish study including 61 cases rendered an accuracy of 94%, but only two lesions were malignant [14]. Interestingly though, another study by Piccolo et al. showed a very high diagnostic accuracy, varying from 77% to 95%, with greater accuracy among TDs with more experience in dermoscopy. In this study, lesions with a high diagnostic difficulty were included and histopathology was used as their gold standard [8].
In our study, a relatively high interobserver concordance with moderate to substantial agreement between the FTF dermatologist and the TDs and between the two TDs was observed. The interobserver concordance was highest when distinguishing between melanocytic and non-melanocytic lesions. The TDs would have recommended ‘no treatment’ for a few lesions. This could have resulted in inadequate management of a patient with MM in situ. It is therefore important to remember that such a risk exists if teledermoscopy is to be used to avoid FTF visits. Melanomas have been underdiagnosed as benign melanocytic nevi or seborrheic keratoses in other teledermoscopy studies as well [8,9,11,15,18].
The rating of the image quality varied greatly between the three dermatologists. The FTF dermatologist found all images to have a satisfactory image quality, whereas the TDs rated 4 and 11 cases (14 different cases), respectively, as having poor quality. This may be due to a grading bias since the FTF dermatologist acquired the images himself, whereas the TDs were perhaps influenced negatively by the high diagnostic difficulty of these 14 cases. In fact, both TDs graded all of these cases as having a high diagnostic difficulty and the FTF dermatologist graded 12 of these 14 cases in the same way. Nevertheless, no images needed to be excluded due to poor quality. As seen in other teledermoscopy studies, poor image quality did not correlate with lower diagnostic accuracy for any of the three dermatologists [8,9,16]. In images with suboptimal quality, the inclusion of relevant clinical information about the patient and the lesion may act as a complement to the images and help the dermatologist with his/her assessment [11].
Goulart et al recently identified a possible use for dermoscopy in skin self-examination [19]. Although this mobile teledermoscopy app could be used by patients directly, our initial intention is to use it in triaging patients with suspicious skin lesions that are referred to dermatologists from GPs. In this sense, there are several limitations to this study. First of all, there was a selection bias since only lesions requiring biopsy or excision were included. The TDs were aware of this fact, which may have influenced their management decisions. This selection bias also means that the assessed lesions do not reflect the wider spectrum of diagnoses seen among all the patients referred to us in routine clinical practice. If the app were used for referral triage, the proportion of benign lesions would certainly increase and histopathological confirmation would not always be ethically possible. Also, differential diagnoses would have to be taken into account in such a scenario since these could affect patient prioritization. Furthermore, all images in this study were taken by the FTF dermatologist, who had experience in using the imaging equipment. The image quality may be affected negatively when the smartphones are put in the hands of GPs.
In order to assess how this app would perform as a triage tool, our group has initiated a larger prospective, multi-center, teledermoscopy trial in which GPs from multiple primary health care centers will refer patients with suspicious lesions to TDs at two hospitals in western Sweden using this app. Potentially, this could lead to more accurate patient prioritization and the possibility of planning for surgery on the patient’s first visit to the dermatologist when necessary. Also, the referring GP could receive faster feedback regarding the suspected diagnosis and the dermoscopic findings, adding educational value. Furthermore, patients with evidently benign lesions could receive reassuring news almost directly, thereby avoiding the nervous wait of weeks or months before finally meeting with a specialist. Using teledermatology and teledermoscopy for triaging patients with a suspicion of skin cancer has already been shown to be both feasible and economically viable [20–22].
Like other teledermoscopy solutions, the app provides a digital referral system that can transfer all relevant clinical information in combination with high-quality digital clinical and dermoscopic images to a dermatologist within seconds. Contrary to other teledermoscopy solutions, the whole teledermoscopy solution fits in your pocket and does not require any cables or the need to transfer images from a camera to a computer prior to sending the case. Furthermore, the standardized query form minimizes the risk of the GP forgetting to include relevant clinical information in the referral. Lastly, and as we have shown here, this mobile teledermoscopy solution allows TDs to achieve a diagnostic accuracy comparable to that of a FTF dermatologist.
The introduction of smartphones with easy-to-install “apps” can potentially revolutionize the way GPs communicate with dermatologists. In 2009, Massone et al envisioned “one click” skin cancer diagnosis through mobile teledermoscopy, and this app takes us a step closer to this goal [7].
Footnotes
Funding: The study was financed by grants from the federal government under the ALF agreement and a grant from Signe och Olof Wallenius stiftelse.
Competing interests: Alexander Börve is the owner of iDoc24® AB.
All authors have contributed significantly to this publication.
References
- 1.van der Leest RJ, de Vries E, Bulliard JL, et al. The Euromela-noma skin cancer prevention campaign in Europe: characteristics and results of 2009 and 2010. J Eur Acad Dermatol Venereol. 2011;25:1455–65. doi: 10.1111/j.1468-3083.2011.04228.x. [DOI] [PubMed] [Google Scholar]
- 2.Sullivan AN, Bryant EA, Mark LA. Malignant melanoma in transplant patients: a case report and review of the literature. Cutis. 2012;89:133–6. [PubMed] [Google Scholar]
- 3.The National Board of Health and Welfare Cancer incidence in Sweden 2010. 2011.
- 4.The National Board of Health and Welfare Basal Cell Carcinoma in Sweden 2004–2008. 2010.
- 5.The National Board of Health and Welfare The status and development in health care and social services in Sweden 2011. 2012.
- 6.Whited JD. Teledermatology research review. Int J Dermatol. 2006;45:220–9. doi: 10.1111/j.1365-4632.2004.02427.x. [DOI] [PubMed] [Google Scholar]
- 7.Massone C, Brunasso AM, Campbell TM, Soyer HP. Mobile teledermoscopy—melanoma diagnosis by one click? Semin Cutan Med Surg. 2009;28:203–5. doi: 10.1016/j.sder.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Piccolo D, Smolle J, Argenziano G, et al. Teledermoscopy—results of a multicentre study on 43 pigmented skin lesions. J Telemed Telecare. 2000;6:132–7. doi: 10.1258/1357633001935202. [DOI] [PubMed] [Google Scholar]
- 9.Warshaw EM, Lederle FA, Grill JP, et al. Accuracy of teledermatology for pigmented neoplasms. J Am Acad Dermatol. 2009;61:753–65. doi: 10.1016/j.jaad.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 10.Warshaw EM, Lederle FA, Grill JP, et al. Accuracy of teledermatology for nonpigmented neoplasms. J Am Acad Dermatol. 2009;60:579–88. doi: 10.1016/j.jaad.2008.11.892. [DOI] [PubMed] [Google Scholar]
- 11.Blum A, Hofmann-Wellenhof R, Luedtke H, et al. Value of the clinical history for different users of dermoscopy compared with results of digital image analysis. J Eur Acad Dermatol Venereol. 2004;18:665–9. doi: 10.1111/j.1468-3083.2004.01044.x. [DOI] [PubMed] [Google Scholar]
- 12.Braun RP, Meier M, Pelloni F, et al. Teledermatoscopy in Switzerland: a preliminary evaluation. J Am Acad Dermatol. 2000;42:770–5. doi: 10.1067/mjd.2000.103977. [DOI] [PubMed] [Google Scholar]
- 13.Kroemer S, Fruhauf J, Campbell TM, et al. Mobile teledermatol-ogy for skin tumour screening: diagnostic accuracy of clinical and dermoscopic image tele-evaluation using cellular phones. Br J Dermatol. 2011;164:973–9. doi: 10.1111/j.1365-2133.2011.10208.x. [DOI] [PubMed] [Google Scholar]
- 14.Moreno-Ramirez D, Ferrandiz L, Bernal AP, Duran RC, Martin JJ, Camacho F. Teledermatology as a filtering system in pigmented lesion clinics. J Telemed Telecare. 2005;11:298–303. doi: 10.1258/1357633054893364. [DOI] [PubMed] [Google Scholar]
- 15.Tan E, Yung A, Jameson M, Oakley A, Rademaker M. Successful triage of patients referred to a skin lesion clinic using teledermoscopy (IMAGE IT trial) Br J Dermatol. 2010;162:803–11. doi: 10.1111/j.1365-2133.2010.09673.x. [DOI] [PubMed] [Google Scholar]
- 16.Piccolo D, Smolle J, Wolf IH, et al. Face-to-face diagnosis vs tele-diagnosis of pigmented skin tumors: a teledermoscopic study. Arch Dermatol. 1999;135:1467–71. doi: 10.1001/archderm.135.12.1467. [DOI] [PubMed] [Google Scholar]
- 17.Borve A, Holst A, Gente-Lidholm A, Molina-Martinez R, Paoli J. Use of the mobile phone multimedia messaging service for teledermatology. J Telemed Telecare. 2012;18:292–6. doi: 10.1258/jtt.2012.120206. [DOI] [PubMed] [Google Scholar]
- 18.Ferrara G, Argenziano G, Cerroni L, et al. A pilot study of a combined dermoscopic-pathological approach to the telediagnosis of melanocytic skin neoplasms. J Telemed Telecare. 2004;10:34–8. doi: 10.1258/135763304322764176. [DOI] [PubMed] [Google Scholar]
- 19.Goulart JM, Malvehy J, Puig S, et al. Dermoscopy in skin self-examination: A useful tool for select patients. Arch Dermatol. 2011;147:53–8. doi: 10.1001/archdermatol.2010.387. [DOI] [PubMed] [Google Scholar]
- 20.Lim D, Oakley AM, Rademaker M. Better, sooner, more convenient: a successful teledermoscopy service. Australas J Dermatol. 2012;53:22–5. doi: 10.1111/j.1440-0960.2011.00836.x. [DOI] [PubMed] [Google Scholar]
- 21.Moreno-Ramirez D, Ferrandiz L, Nieto-Garcia A, et al. Store-and-forward teledermatology in skin cancer triage: experience and evaluation of 2009 teleconsultations. Arch Dermatol. 2007;143:479–84. doi: 10.1001/archderm.143.4.479. [DOI] [PubMed] [Google Scholar]
- 22.Moreno-Ramirez D, Ferrandiz L, Ruiz-de-Casas A, et al. Economic evaluation of a store-and-forward teledermatology system for skin cancer patients. J Telemed Telecare. 2009;15:40–5. doi: 10.1258/jtt.2008.080901. [DOI] [PubMed] [Google Scholar]