Abstract
Objective. To examine student pharmacists’ perceptions of interprofessional roles before and after completing an advanced pharmacy practice experience on solid organ transplantation.
Methods. Student pharmacists across the United States participating in an APPE on a solid organ transplant team completed an online pre- and post-APPE survey instrument examining perceptions of interprofessional roles, communication, and teamwork.
Results. Student pharmacists’ scores on interprofessionalism increased significantly on 17 of 22 items. Positive changes were seen in the interprofessional education core competency areas of roles and responsibilities, interprofessional communication, and teams and teamwork.
Conclusion. Student pharmacist participation in interprofessional clinical APPEs can positively influence their professional development as they prepare to become members of multi-disciplinary teams in the healthcare workforce.
Keywords: interprofessional education, advanced practice pharmacy experience, multidisciplinary care
INTRODUCTION
Interprofessional education (IPE) encourages joint learning by practitioners and students from multiple professions with the goals of improving collaborative practice and the healthcare outcomes of patients.1 Some of the changes in Medicare, as well as many aspects of the Patient Protection and Affordable Care Act of 20102 and the National Committee for Quality Assurance Patient-Centered Medical Home 2011, promote team-based care models. These policies are expected to improve how healthcare professional curricula embraces IPE, both in the United States and globally. In 2011, an expert panel of professionals from pharmacy, nursing, medicine, public health, and dentistry developed and published a comprehensive report on Core Competencies for Interprofessional Collaborative Practice that highlights the necessity for IPE in order to provide high quality, safe care to all patients.3
The most important focus of IPE is the ability of the interdisciplinary team to improve patient outcomes. These include, but are not limited to, the enhancement of the quality of patient care, lowered costs, decreased patient length of stay, and reduced medical errors.4 Working as a team has improved care and outcomes for patients in the areas of geriatrics, respiratory disease management, primary care, orthopedic surgery, and chronic pain, as well as in other specialty areas.5 An Institute of Medicine report attributes many health care errors to diminished interprofessional cooperation and ineffective communication, suggesting that a goal of reducing patient errors by 50% in 5 years is achievable through improved interprofessional collaboration.6 In addition to patient safety benefits, interprofessional teamwork is now recognized as an important strategy for shared decision making, a process that supports patient participation in achieving informed, preference-based choice.7 IPE is believed to be key to the success of shared decision-making models within primary care, with a focus on understanding interprofessional sensitivities and interprofessional roles.
Interprofessional education is recognized as an essential component of graduate and professional curricula. Students who engage in interprofessional experiences are more confident in their roles and in working with other health professionals.8-10 Interprofessional education appears to allow health professions students to become well-rounded, actively engage in patient care, and work toward the common goal of improving patient outcomes. Also, IPE increases health professions students’ confidence in their own roles as well as how they view other healthcare professionals, improves students’ ability to collaborate with and understand other health disciplines, and improves leadership, communication, and problem-solving skills.8-10 These interactions may change perceptions or stereotypes of other health care roles a student may hold to a more realistic perspective.11,12
Along with other healthcare disciplines, pharmacy educators support and promote the inclusion of interprofessional education in the doctor of pharmacy (PharmD) curricula as is evidenced by the 2009 Interprofessional Education supplement published by the Journal.8,9,13-15 Standard 12 of the Accreditation Council for Pharmacy Education’s 2012 Accreditation Standards and Guidelines places a strong emphasis on interprofessional education.16 The degree to which IPE is incorporated into the pharmacy curricula may vary because of the overall lack of directives requiring pharmacist involvement in patient care teams in clinical practice.
Historically, the presence of pharmacists on specialized medical teams has not been compulsory for regulatory compliance or financial reimbursement. However, in 2004 and 2007, the United Network for Organ Sharing and the Centers for Medicare and Medicaid Services, respectively, issued mandates requiring the documented participation and inclusion of a pharmacist on a multidisciplinary team in order to meet accreditation standards, making transplantation the only specialty in the United States to have such a requirement.17,18 Along with pharmacists, solid organ transplant teams include physicians, surgeons, nurse coordinators, dieticians, social workers, financial coordinators, donor advocates, and chaplains, making them an excellent example of a multidisciplinary team.
Because it includes members from a broad range of health care disciplines, the authors felt that a solid organ transplant APPE would be an ideal setting in which to study interprofessional roles. Pharmacy literature evaluating IPE has focused primarily on the implementation and evaluation of IPE in the classroom. This study is novel in that it was designed to examine advanced pharmacy practice experience (APPE) student pharmacist perceptions of interprofessional roles before and after completing a solid organ transplant APPE and aimed to examine the impact of IPE during experiential learning. In addition, the study explored possible factors which may have contributed to student pharmacists’ opinions regarding interprofessional collaboration.
METHODS
Questions for the survey instrument administered in this study were modified from items used by Dobson and colleagues in their study on quality improvement to promote interprofessional collaboration among health professions students and on Clark’s Interdisciplinary Team Weekly Inventory, which was used to evaluate interdisciplinary teamwork on a gerontology team.9,10 The items included on the pre- and post-APPE survey instruments were identical.
Once the survey questions were developed, content validation by experts in solid organ transplant teams and survey methodology was completed. This included evaluation of the survey items for relevance and readability, revision of existing items, and addition of survey items. Prior to the initiation of the survey, a final review by test developers was completed to ensure that all content domains were covered. The final 29-item survey instrument contained 4 sections: forced choice, closed-ended items on demographics; forced-choice, close-ended items on previous experiential learning experiences; Likert-scale items regarding the respondent’s role as a health professions student; and Likert-scale items on the respondent’s perceptions of interprofessional teams.
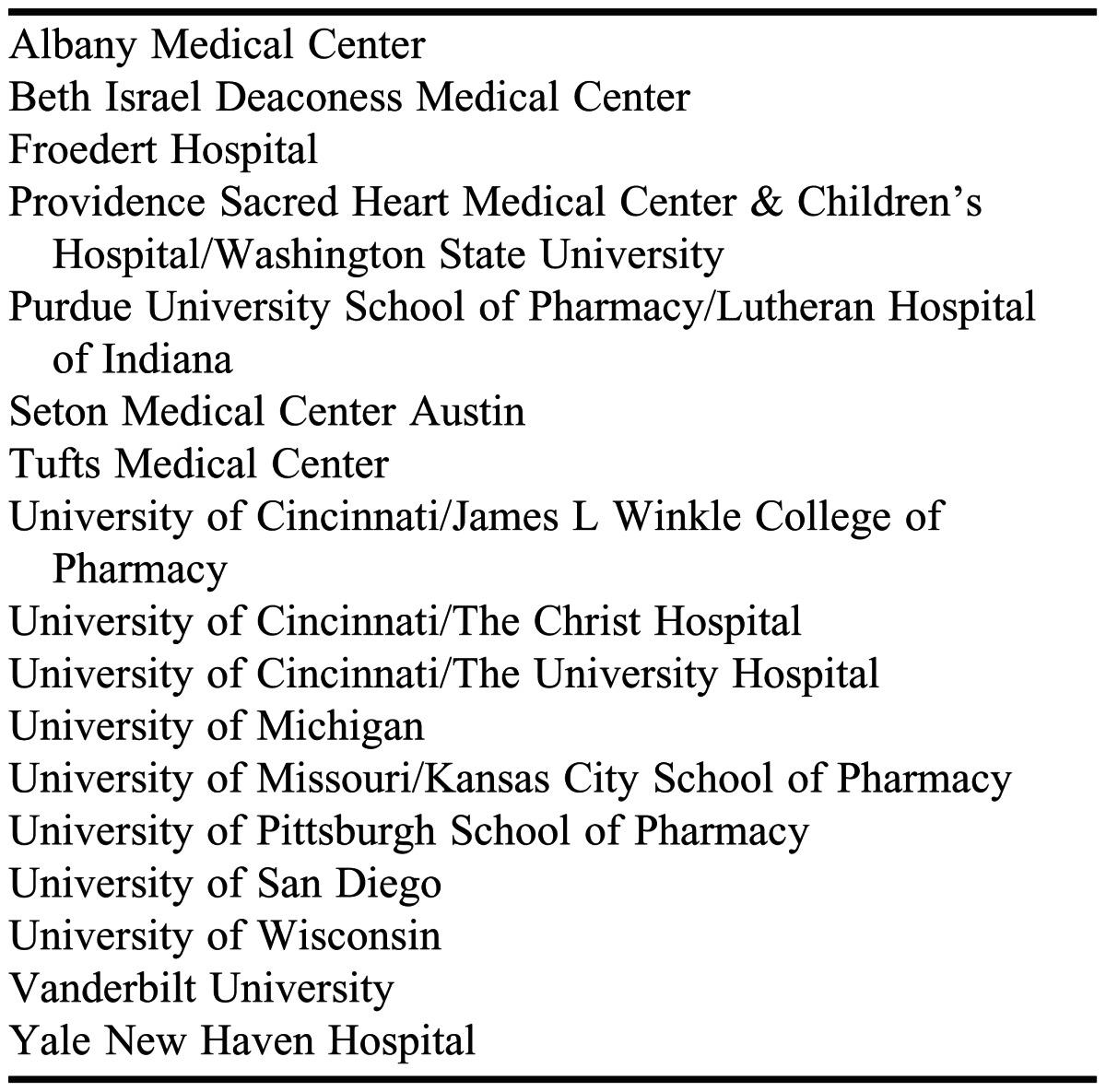
An e-mail was sent to the American College of Clinical Pharmacy Immunology and Transplantation Practice and Research Network list serve inviting pharmacy preceptors to participate in the study. The network had approximately 271 members including pharmacists working in transplantation within academia, clinical pharmacy, research, industry, and leadership. The network list was cross-referenced with the membership list of the American Society of Transplantation Transplant Pharmacy Community of Practice to ensure that transplant pharmacists who were not part of the network were included. Twenty solid organ transplant programs responded and 17 agreed to participate in the study (Table 1). All APPE students completing a solid organ transplant practice experience with a pharmacist preceptor at a participating center were eligible to participate.
Table 1.
Participating Colleges and Schools of Pharmacy With Solid Organ Transplant Programs
The study was conducted from March 1, 2011, through May 31, 2012, which coincided approximately with 1 academic year and a complete cycle of APPE students. Transplant pharmacist preceptors were e-mailed a reminder with survey links at the beginning and end of each practice experience with instructions to have each student pharmacist complete the pre-APPE survey instrument within the first week of the APPE and the post-APPE survey instrument prior to the last day of their APPE. Student pharmacists were not directly contacted by the research team. Communication regarding pre- and post-APPE surveys occurred only through contact with their primary preceptor, although primary preceptors did not know which students were participating in the survey. Participation in the survey was completely voluntary and not linked to a grade or requirements for the APPE.
Students completed the pre- and post-APPE survey instruments using Skylight, version 1.03.25, (Washington State University, Pullman, WA) an online proprietary survey application. At the end of each survey instrument, students were asked to enter the last 4 digits of their Social Security number for purposes of matching pre-and post-APPE survey responses. As an incentive to complete the post-APPE survey instrument, respondents who returned the survey completion certificate by mail were entered in a drawing for a $100 VISA gift card. While all students were invited to participate in the pre- and post-APPE surveys, only those that completed both survey instruments were included in the analysis. The survey and methods were declared exempt from review by the Washington State University Institutional Review Board.
The Wilcoxon signed rank test was used to examine changes over time in each of the closed-end items. To assess change in total scores from the pre- to the post-APPE survey, normality assumptions were checked, internal consistency was determined via Cronbach alpha, and a paired-samples t test was conducted. A mixed ANOVA was used to examine potential interaction between gender and age groups from total score pre- to post-APPE survey values. Tukey’s HSD (honestly significant difference) post hoc tests were used across age groups as appropriate. Nonparametric and parametric tests were considered significant at p ≤ 0.05. Statistical analyses were performed using SPSS for Windows, version 19 (IBM Corp, Armonk, NY).
RESULTS
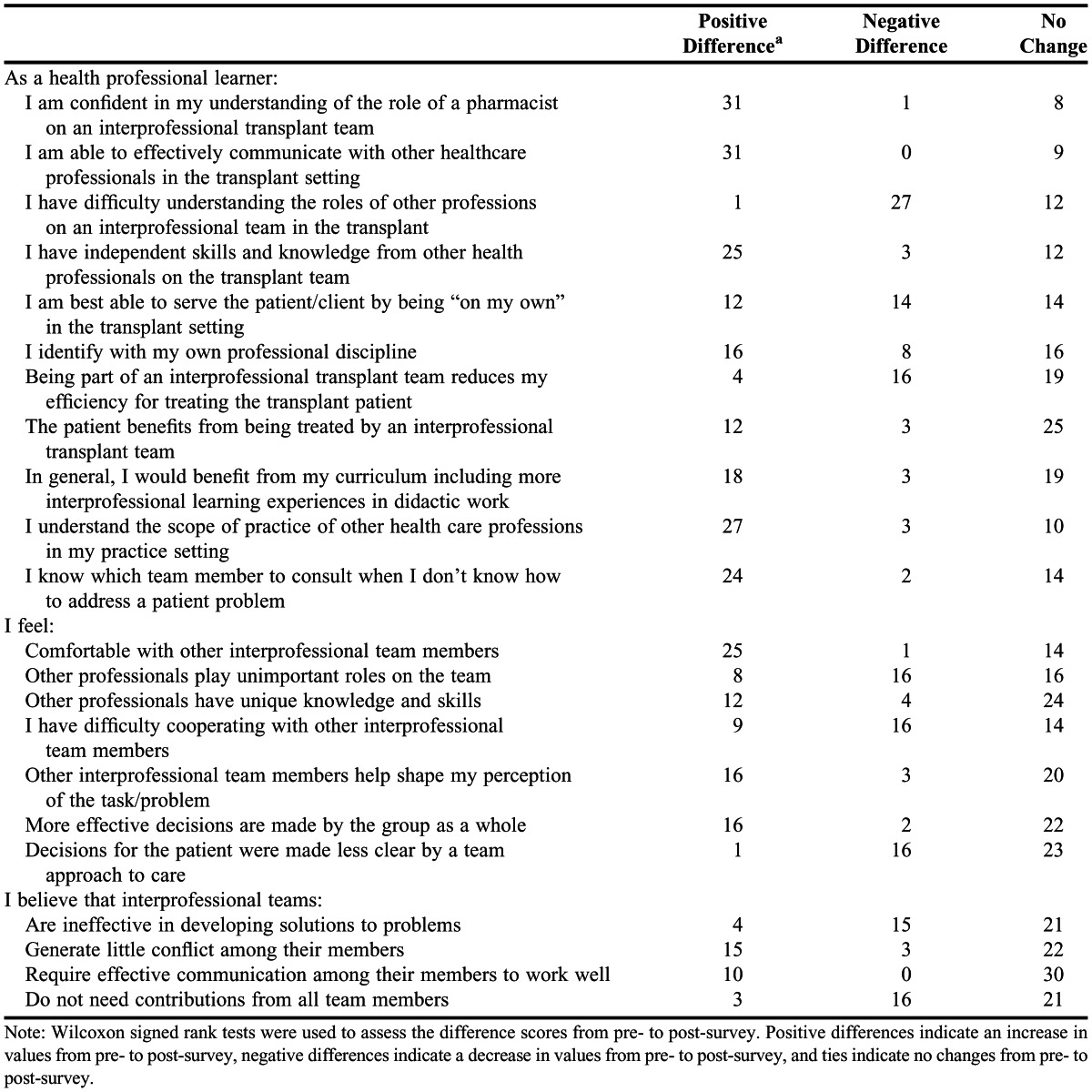
Ninety students from 17 institutions were eligible to complete the pre-and post-APPE survey instruments. Sixty-three students completed the pre-APPE survey instrument and 37 students completed the pre-APPE and post-survey instrument. Therefore, the final sample size was 37 participants. Table 2 provides demographic information of the 37 survey respondents. Table 3 presents the Wilcoxon signed rank test statistic and differences (type of change from pre- to post-APPE survey) for each survey item. A significant improvement in scores (ie, increased interprofessionalism) was seen on 17 of 22 survey items from pre- to post-APPE survey. The total pre-APPE survey (skewness statistic = -0.57, kurtosis statistic = 0.42) and post-survey (skewness statistic = -0.49, kurtosis statistic = - 0.83) scores were normally distributed, therefore parametric tests were used to assess change over time. Cronbach alpha indicated that the survey items were internally consistent for the pre-APPE survey (α = 0.78) and post-APPE survey (α = 0.80). The paired-samples t test showed a significant increase in total scores from pre-APPE survey (85.7 ± 7.1) to post-APPE survey (97.2 ± 6.8p < 0.001). There did not appear to be a gender or age effect on survey responses given a nonsignificant gender x repeated measures interaction (p = 0.38) and a nonsignificant age group x repeated measures interaction (p = 0.52).
Table 2.
Demographic Characteristics of Participants (%)
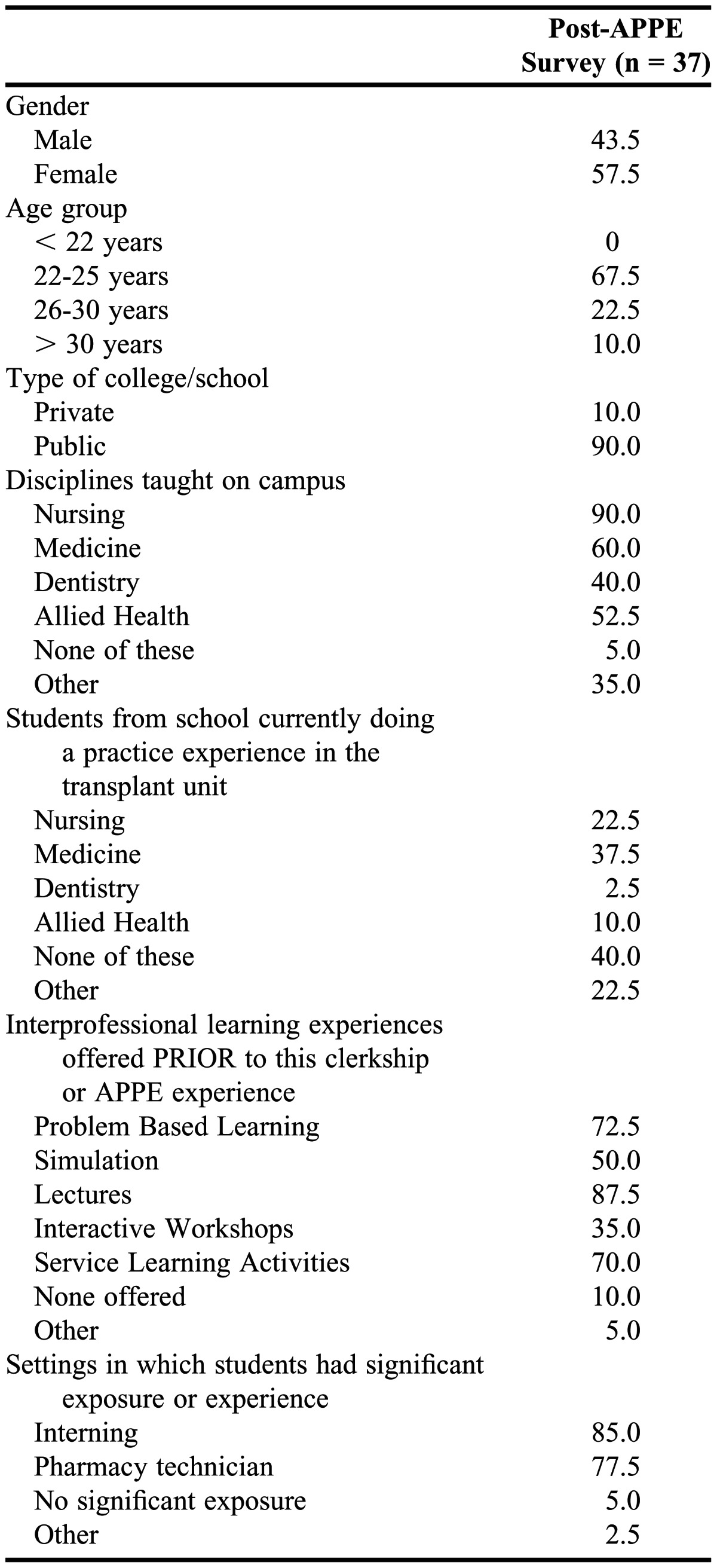
Table 3.
Student Pharmacists’ Perceptions of Interprofessional Education After Completing an Advanced Pharmacy Practice Experience as Part of an Interprofessional Solid Organ Transplant Team (N = 37)
DISCUSSION
Integration of IPE into health professions education can occur within the pre-clinical, classroom curriculum as well as the clinical APPE arena. This nationwide study specifically focused on the impact of an APPE in the transplantation clinical setting where mandatory, multidisciplinary teams exist. The Core Competencies for IPE Collaborative Practice defines 4 competency domains, which are values and ethics, roles and responsibilities, interprofessional communication, and teams and teamwork.3 While values and ethics were not specifically addressed, the pre- and post-APPE survey items did evaluate the 3 other domains. Based on the survey results and analyses, student pharmacists demonstrated positive changes in interprofessional perceptions from pre- to post-APPE in the areas of roles and responsibilities, interprofessional communication, teams and teamwork. Student pharmacists’ overall perception of interprofessional education also improved between the pre- and post-APPE survey, indicating the generally positive impact of the experience. Even though 89% of the student pharmacists had previous interprofessional experiences in lectures, simulation, problem-based learning or workshops, participating in a solid organ transplantation APPE positively impacted their perspectives.
The impetus for this study was to demonstrate that a single experience incorporating student pharmacists with practicing clinicians from different disciplines would positively affect their perceptions of multidisciplinary care and dynamics. The results could then be used as a catalyst to increase the incorporation of IPE in the classroom curriculum as well as work towards the goals of multidisciplinary patient care outlined in the Introduction of this paper. Without a strong IPE background, it would be difficult to translate the core competencies learned in classroom lectures into actual clinical practice. Increasing the opportunities and expanding the varieties and types of IPE in the pharmacy school curricula may better prepare student pharmacists for effective involvement on multidisciplinary teams once they become practicing clinicians.
There were several limitations to this study. The response rate for students completing both the pre- and post-survey instruments (59%) was less than desirable and was primarily the result of student errors in the coding procedure that linked the pre- and post-APPE survey responses. Several survey instruments were lost to follow-up because of this problem. This is an area that can be improved for future projects by identifying a more straightforward method for self-reported coding such as internally linking the pre- and post-survey once the survey is initiated by the individual.
Although the survey focused on a specific clinical practice area, the generalizability of the results to other practice settings is possible because none of the questions focused on the content of the practice experience (solid organ transplantation) but rather on the dynamics of the members of the multidisciplinary team. Finally, the study included only PharmD students so it is unknown if other student members of the solid organ transplant teams experienced similar positive changes in perceptions about interprofessional dynamics. Future research in this area could be expanded to other types of APPEs or to other health professions students to evaluate their perceptions of interprofessional teams following training in clinical sites.
CONCLUSION
Student pharmacist perceptions about interprofessional teamwork were positively impacted by participation in a solid organ transplant APPE. These findings emphasize the important role of interprofessional clinical APPEs to influence the professional development of students as they prepare to become members of multidisciplinary teams in the healthcare workforce.
ACKNOWLEDGMENTS
Special thanks to additional reviewers/contributors: Douglas Weeks, Eric Tichy, Lisa McDevitt-Potter, Christin Rogers, Erin Newkirk, Adele Rike-Shields, Janice Sudaria, Ashley Feist, Jennifer McComb, Phyllis Chow, Heather Johnson, Christie Truscott, Erica Maceira, Elizabeth Gorevski, Leah Crow, Tiffany Kaiser, Rita Alloway, Nicole Weimert,-Pilch, Benjamin Duhart Jr., Jamie Park, Jill Boone, Roy Dobson, Susan Wright and Ryan Maynard.
REFERENCES
- 1.Reeves S, Zwarenstein M, Goldman J, Barr H, Freeth D, Hammick M, Koppel I. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2008;(1):CD002213. doi: 10.1002/14651858.CD002213.pub2. [DOI] [PubMed] [Google Scholar]
- 2.H.R. 3590–111th Congress: Patient Protection and Affordable Care Act. (2009) 2012 In: www.GovTrack.us. http://www.govtrack.us/congress/bills/111/hr3590. Accessed September 14. [Google Scholar]
- 3.Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Washington, D.C.: Interprofessional Education Collaborative; 2011. [Google Scholar]
- 4.World Health Organization 2010. Framework for action on interprofessional education and collaborative practice. 2012. http://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf. Accessed October 8. [PubMed] [Google Scholar]
- 5.Allison S. Up a river! Interprofessional education and the Canadian healthcare professional of the future. J Interprof Care. 2007;21(5):565–568. doi: 10.1080/13561820701497930. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine. Washington, DC: National Academies Press; 2003. Crossing the quality chasm: a new health system for the 21st century. [PubMed] [Google Scholar]
- 7.Col N, Bozutto L, Kirkegaard P, et al. Interprofessional education about shared decision making for patients in primary care settings. J Interprof Care. 2011;25(6):409–415. doi: 10.3109/13561820.2011.619071. [DOI] [PubMed] [Google Scholar]
- 8.Odegard PS, Robins L, Murphy N, et al. Interprofessional Initiatives at the University of Washington. Am J Pharm Educ. 2009;73(4):Article 63. doi: 10.5688/aj730463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dobson RT, Stevenson K, Busch A, Scott DJ, Henry C, Wall PA. A quality improvement activity to promote interprofessional collaboration among health professions students. Am J Pharm Educ. 2009;73(4):Article 64. doi: 10.5688/aj730464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clark PG. Learning on interdisciplinary gerontological teams: instructional concepts and methods. Educ Gerontol. 1994;20(4):359–360. [Google Scholar]
- 11.McCaffrey R, Hayes RM, Cassell A, Miller-Reyes S, Donaldson A, Ferrell C. The effect of an educational programme on attitudes of nurses and medical residents towards the benefits of positive communication and collaboration. J Adv Nurs. 2011;68(2):293–301. doi: 10.1111/j.1365-2648.2011.05736.x. [DOI] [PubMed] [Google Scholar]
- 12.Carpenter J. Doctors and nurses: stereotypes and stereotype change in interprofessional education. J Interprof Care. 1995;9(2):157–159. [Google Scholar]
- 13.Buring SM, Bhushan A, Broeseker A, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ. 2009;73(4):Article 59. doi: 10.5688/aj730459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cameron A, Ignjatovic M, Langlois S, et al. An interprofessional education session for first-year health science students. Am J Pharm Educ. 2009;73(4):Article 62. doi: 10.5688/aj730462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buring SM, Bhushan A, Brazeau G, Conway S, Hansen L, Westberg S. Keys to successful implementation of interprofessional education: learning location, faculty development, and curricular themes. Am J Pharm Educ. 2009;73(4):Article 60. doi: 10.5688/aj730460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Accreditation Council for Pharmacy Education. Accreditation standards. 2012 https://www.acpe-accredit.org/pdf/S2007Guidelines2.0_ChangesIdentifiedInRed.pdf. Accessed September 20. [Google Scholar]
- 17.Centers for Medicare and Medicaid Services. Medicare program; hospital conditions of participation: requirements for approval and re-approval of transplant centers to perform organ transplants. Final rule. Fed Regist. 2007;72(61):15197–15280. [PubMed] [Google Scholar]
- 18.United Network for Organ Sharing. 2007. Attachment 1 to appendix B of UNOS bylaws: designated transplant program criteria. 2011 http://optn.transplant.hrsa.gov/policiesandBylaws2/bylaws/OPTNByLaws/pdfs/bylaw_162.pdf. Accessed October 6. [Google Scholar]


