Abstract
Objective. To design and implement a Medical Outreach Experience elective course and assess its impact on students’ level of confidence in organizing future medical outreach trips, providing population-specific pharmaceutical care, and achieving learning outcomes.
Design. A 2-credit hour elective course was designed for second- and third-year pharmacy students. The course was structured to include 3 sections over 1 semester, a 10-week training and preparation phase, followed by a weeklong international outreach experience and post-outreach reflection.
Assessment. Student achievement of curricular outcomes was measured using in-class activities, readings, reflections, and longitudinal projects, as well as performance during the outreach trip. Results from pre- and post-course surveys demonstrated significant improvement in student-rated confidence in several components of outreach trip organization and provision of pharmaceutical care.
Conclusions. Students completing the course exhibited increased confidence in their abilities to organize and practice on a medical outreach trip. All students met the learning outcomes of the course, which included providing comprehensive patient-specific pharmaceutical care, communicating effectively, promoting health improvement and self-care, thinking critically, and appropriately managing and using resources of the healthcare system. Students agreed that the elective course was a valuable addition to the curriculum.
Keywords: medical missions, public health, curriculum, elective course, pharmaceutical care
INTRODUCTION
Standard 12 of the Accreditation Council for Pharmacy Education (ACPE) guidelines requires pharmacy students to be able to demonstrate population-based health care as a professional competency prior to graduation.1 Additionally, the educational outcomes developed by the American Association of Colleges of Pharmacy Center for the Advancement of Pharmaceutical Education (CAPE) address the need for courses in pharmacy curricula that provide educational opportunities in the areas of public health as well as patient-centered and population-based pharmaceutical care.2 Public health training has historically been limited within pharmacy school curricula, leading to less involvement of pharmacists in public health efforts compared with other healthcare professionals.3
Medical outreach is 1 area of public health service wherein pharmacy involvement is being increasingly documented. Using their expertise, pharmacists provide population-based health care to underserved and at-risk populations. Pharmacists’ knowledge and skills in pharmacotherapeutics, drug information, formulary development, compounding, drug distribution, patient counseling, and pharmacy organization and workflow make them essential members of multidisciplinary medical outreach teams.4 An article published by Clements and colleagues reported that 97.2% (n=36) of nonpharmacy professionals strongly agreed that pharmacists’ contributions to the team were necessary for the success of the medical outreach trip.5
A few pharmacy colleges and schools have capitalized on the educational benefit gained from student involvement on these trips.5-7 Students gain hands-on experience through assisting in triaging patients, developing patient care plans with physicians, educating patients, and dispensing medications.7 References to medical outreach trips offered for introductory or advanced pharmacy practice experiences (IPPEs or APPEs) and elective credit can be found in the literature, but data regarding the design and assessment of these courses are limited.
An elective course, the Medical Outreach Experience, was approved by the University of Louisiana at Monroe College of Pharmacy for the spring semester of 2012. The elective course was designed to train pharmacy students in the provision of patient care to underserved populations through preparation and participation in an international medical outreach trip. The purpose of this article is to describe the design and implementation of the 2012 offering of the Medical Outreach Experience elective and to assess the impact of the elective course on student’s level of confidence in organizing future public health efforts and providing population-specific pharmaceutical care. Student attainment of the course-specific outcomes of providing comprehensive patient-specific pharmaceutical care, communicating effectively, promoting health improvement and self-care, thinking critically, and appropriately managing and using resources of the healthcare system is also discussed.
DESIGN
Medical Outreach Experience was a 13-week, 2-credit hour elective course offered to second and third-year doctor of pharmacy (PharmD) students during the spring semester of 2012. The course was structured to include 3 sections: a 10-week training and preparation phase, the weeklong international outreach experience, and the post-outreach reflection. In order to maximize interactions between students and faculty members and to ensure student exposure to all aspects of pharmacy practice, the class size was capped at 8 students. Prior to registration, any interested students were required to contact the course coordinator. Because of the limited class size and the substantial number of interested students, preference was given to students in their third year. In the event that more than 8 third-year students expressed interest in enrolling, class participants were to be determined by random selection. Students were not asked to provide additional information prior to enrolling in the course.
The course was co-taught by 4 pharmacy faculty members with previous experience in medical outreach work. Faculty members collaborated to determine the pertinent discussion topics to include in the 10-week training and preparation phase of the course. The topics were chosen to prepare students for the upcoming outreach trip and equip them to coordinate future trips (Table 1). In addition to past experiences of faculty members, publications documenting various pharmacist roles in medical outreach were used to identify the most pertinent subject matter.4,7-9 Faculty members relied heavily on resources from the World Health Organization (WHO) and Centers for Disease Control and Prevention in preparation for classroom lectures.
Table 1.
Topics and Assignments in the Medical Outreach Experience Elective Course
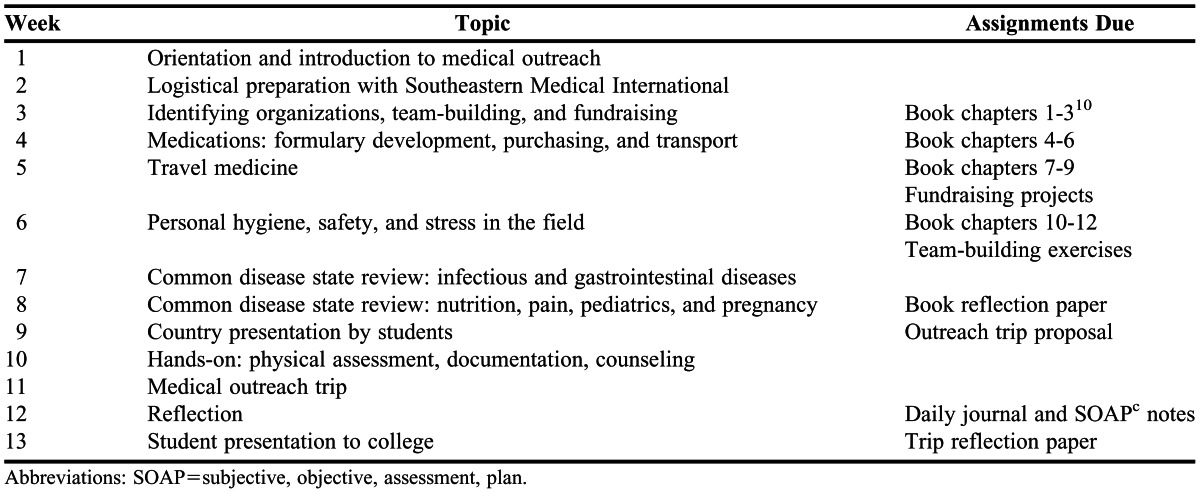
Various teaching strategies were used for each phase of the course. During the training and preparation phase, 2-hour classes were held once weekly for 10 weeks. A combination of classroom lectures, discussion, and problem-based and active-learning techniques were used during class time. The goal of this phase was to introduce students to the role of pharmacy in medical outreach and to prepare them to lead and participate on future medical trips. Based on the activities and information presented within this section of the course, students were expected to be able to coordinate and plan a medical trip from its inception or join and offer pharmacy expertise to an existing team.
To expose students to possible rewards and challenges encountered in international public health service, a book entitled This is a Soul: The Mission of Rick Hodes was used as a required reading.10 This book highlights the poverty and substandard medical care in a third world country and the life of an American physician who dedicated his career to serve there. It was chosen for the course to expose students to the contrast in availability and quality of medical care around the world and to highlight effective attitudes and behaviors when interacting with patients. A portion of class time was used for discussion each week, and students were required to write a reflection on the book upon completion.
Along with the book discussion, the first 6 class periods covered topics dealing with outreach trip preparation and organization (Table 1). Students were divided into 2 groups to design fundraising activities and team-building exercises during this time. Students were offered the opportunity to implement the 2 fundraising activities with proceeds distributed equally among participants, but the implementation was not required. The 2 team-building exercises were used to develop relationships and build trust among team members. Completion of each of these activities was factored into the participation grade of the course.
Following the organizational component of the course, class time was devoted to reviewing commonly encountered disease states and training in basic physical assessment and clinical skills. A case-based teaching strategy was used for reviewing common disease states. Using the medication formulary created by faculty members for the upcoming trip, students designed and presented patient care plans for each assigned disease state. Medications included on the formulary by faculty members were determined using the WHO model list of essential medicines and other example formularies published previously.4,8,11 To conclude the 10-week training and preparation phase of the course, a guest speaker familiar with the destination country was invited to teach students common cultural practices and customs to prepare them for upcoming patient interactions.
To reinforce concepts taught during the initial phase of the course, students were required to create a written outreach trip proposal and country presentation. On the first day of class, students were divided into pairs, each of which was assigned a different country. As 1 component of the project, students were required to research, develop, and present a Microsoft PowerPoint presentation detailing the demographics, healthcare resources, and common disease states endemic to their respective countries. This exercise was included as a component of the course to show students the importance of background research for the development of a successful outreach trip. In addition to the background information, the outreach trip proposal included sections on logistics and planning, medications and supplies, and implementation. Items to be included in the logistics and planning section of the proposal were a fictional multidisciplinary team composition list, timeline, travel itinerary, cost breakdown, and fundraising project. For the medication and supplies section, students developed a country-specific formulary and supply list with quantities, costs, and suppliers. The implementation section included necessary team documents and a clinic schedule. Each of these required components correlated with concepts taught within the first portion of the course. This project allowed students to get hands-on experience using practical strategies taught in the course to create a comprehensive medical outreach trip plan. Students were required to complete and present the outreach trip proposal prior to the class trip.
The medical outreach trip was scheduled to coincide with the students’ spring break holiday. The trip was planned in collaboration with a nonprofit organization specializing in medical trips. Through previous medical outreach experience, faculty members had established a partnership with the organization to provide a yearly trip for pharmacy students to meet the objectives of the course. Working closely with faculty members throughout the year, the organization facilitated development of a trip itinerary, including destination, lodging, food, transportation, and clinic sites. Other members of the multidisciplinary team were also recruited by the organization. Leaders from the organization met with students during the second class period to introduce policies and procedures as well as to prepare students for upcoming travel.
The destination for the 2012 elective was Mirebalais, Haiti, where 5 clinics were held over the course of a week. The multidisciplinary team included 2 physicians, 1 nurse, 3 pharmacy faculty members involved in the elective course, 8 pharmacy students, and nonmedical personnel. Students rotated through all clinic positions, including triage, clinician assessment, pharmacy, and crowd management. During patient triage, students were partnered with a translator to conduct patient interviews and document the patient’s chief complaint, pertinent medical history, and vital signs. Students assigned to clinician assessment assisted with physical examinations and development of patient treatment plans. In this position, students were able to answer drug information questions and make therapeutic recommendations to influence prescribing habits. In the pharmacy, students evaluated medication orders for appropriateness, carried out all roles of medication dispensing, and provided patient counseling with the assistance of a translator. Preprinted resealable plastic bags depicting the dosage forms, amounts, and administration time were used to overcome language barriers and low literacy. At the end of each clinic day, the team participated in a reflection and discussion led by faculty members. This time was used to review patient cases and debrief on the day’s experiences. Students were responsible for writing daily reflections as well as documenting any clinical interventions using the subjective, objective, assessment, plan (SOAP) format.
After returning from the trip, there was a short reflective phase of the course. The 2 class meetings were used by students and faculty members to evaluate the overall effectiveness of the outreach. Faculty members facilitated a discussion reflecting on what students had learned from the trip and opportunities for improving future trips. Following the discussion, students completed a reflection paper outlining their personal thoughts on the experience. In the final assignment for the course, students collaborated to develop and present an informational slide show documenting the outreach trip to the college of pharmacy.
EVALUATION AND ASSESSMENT
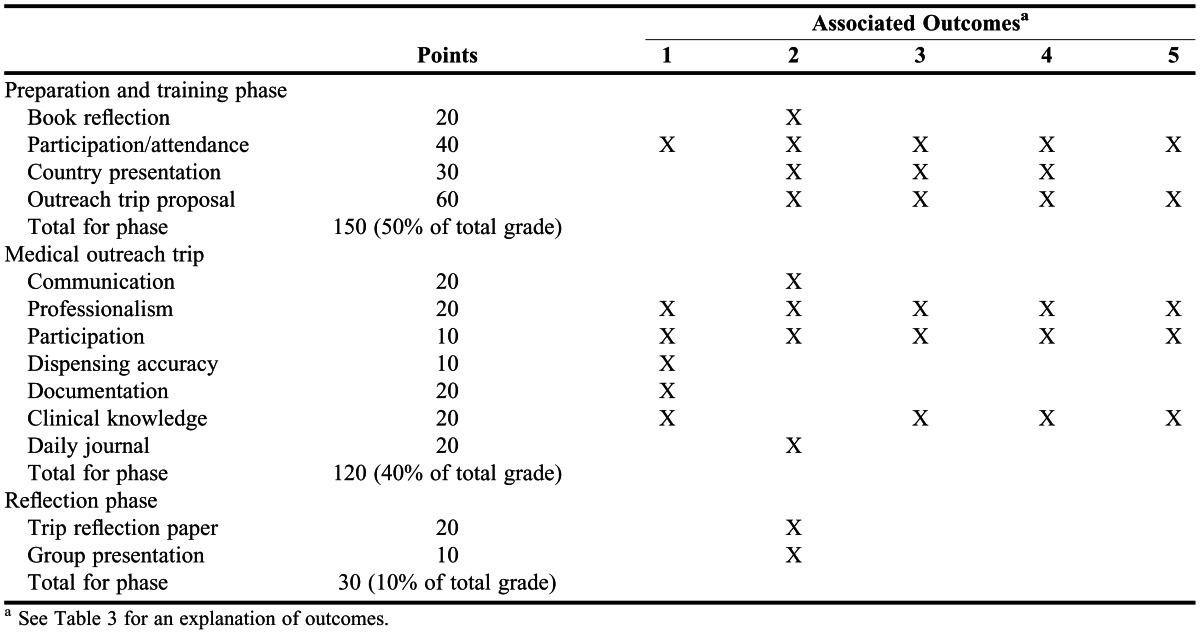
The methods of assessment depended on the phase of the course (Table 2). The training and preparation phase, which accounted for 50% of the total grade, included the book reflection, participation grade, outreach trip proposal, and country presentation. The outreach experience accounted for 40% of the total grade. Students were assessed based on their performance and participation throughout the week. The reflection paper and group presentation assigned during the reflection phase accounted for the remaining 10% of the course grade.
Table 2.
Methods of Assessment, by Phase of Medical Outreach Course, and Associated Outcomes
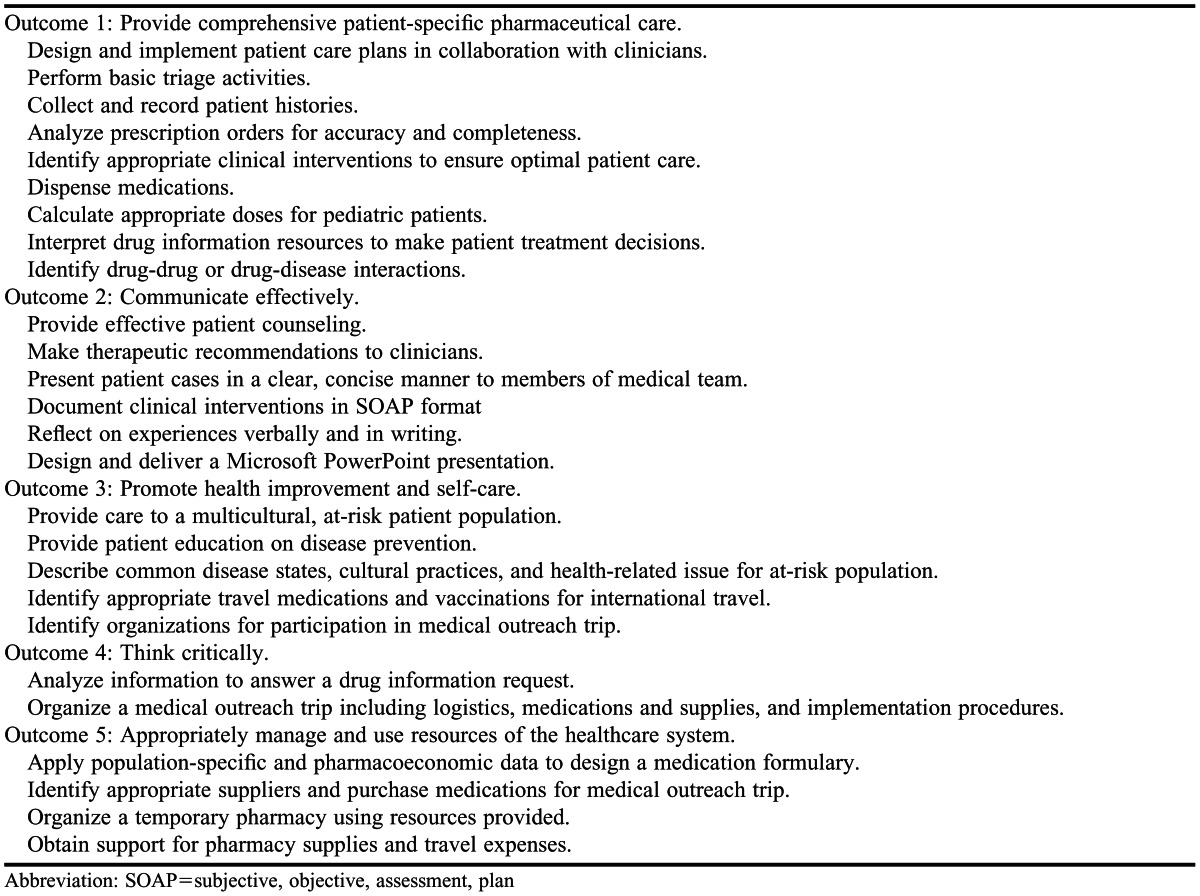
Upon completion of the elective course, students were expected to be able to provide comprehensive patient-specific pharmaceutical care, communicate effectively, promote health improvement and self-care, think critically, and appropriately manage and use resources of the healthcare system. These course outcomes, adapted from ULM College of Pharmacy educational outcomes and competencies, are aligned with CAPE and ACPE guidelines. Specific course objectives were designed to promote student attainment of each outcome (Table 3).
Table 3.
Medical Outreach Course Outcomes and Objectives13
Evaluation of the course, which was accomplished by various means, can be broken into 2 parts: learner evaluation and curriculum evaluation. Table 2 provides a summary of the assessment methods used to evaluate student performance as well as a map of the assignments to corresponding curricular outcomes. The assignments consisted of in-class activities, readings, reflections, and longitudinal projects. Activities were assessed with assignment-specific rubrics that were developed by the course instructors and are available from the corresponding author upon request.
By using various types of assignments throughout the course, achievement of curricular outcomes was measured multiple times. Successful attainment of each outcome is supported by assessment of student performance on outcome-specific assignments. All students received a passing grade for each assignment. All students achieved a 90% or better on 11 of the 13 course assignments. Six of the 8 students received 90% or better on the country presentation and outreach trip proposal project.
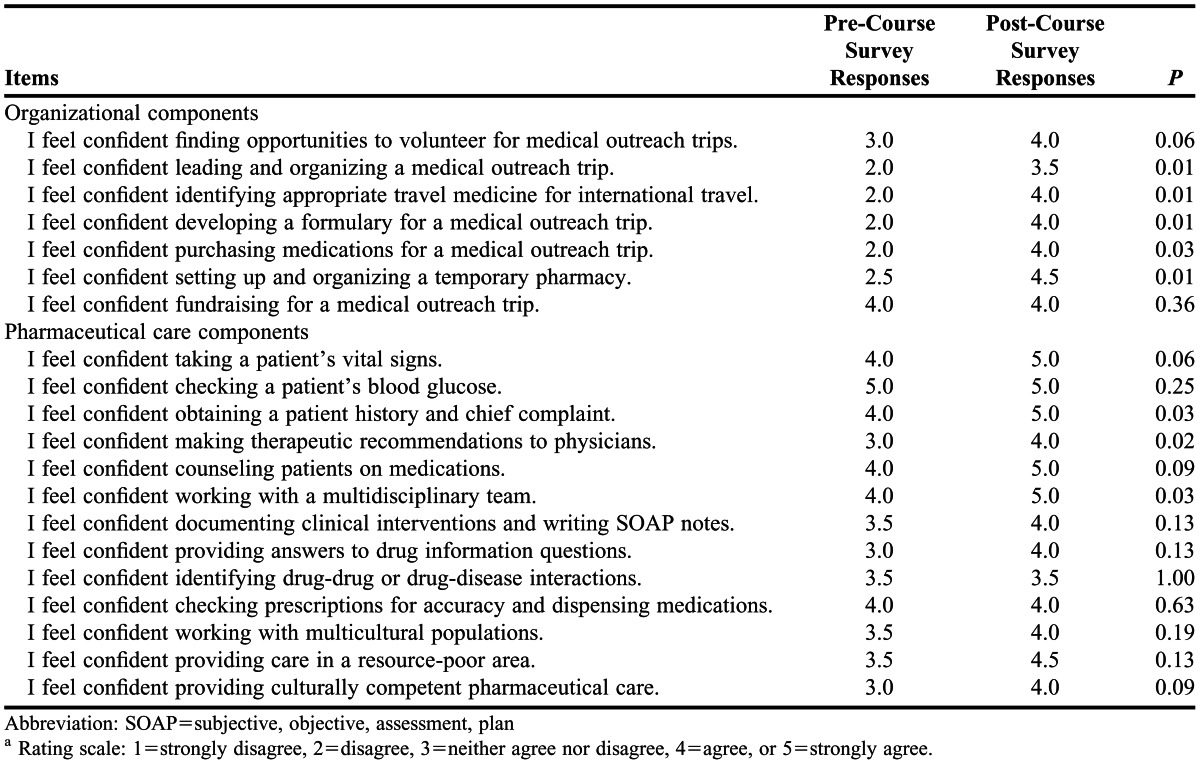
In addition to these course-specific assignments, learner evaluation included a more subjective assessment of student-rated confidence across 2 domains, as measured by pre- and post-course survey instruments. Two domains were covered in the survey instrument: organizational components, which dealt with the logistics of planning and implementing a medical outreach trip; and pharmaceutical care components, which dealt with specific clinical skills required of students in this type of practice. The pre-course survey instrument was administered in 2 parts. The organizational items were given on the first day of class because they dealt with outcomes specific to this course. Because confidence in the various aspects of the pharmaceutical care components could have been influenced by student exposure to clinical material in other courses, this portion of the pre-course survey instrument was administered during the class meeting immediately prior to the trip. Both portions of the post-course survey instrument were administered during the first class meeting after the trip. Survey instruments were approved by the Institutional Review Board at the University of Louisiana at Monroe.
The 8 students enrolled in the course were required to complete the pre- and post-course survey instruments. Seven questions pertained to confidence in organizing components of medical outreach, and 13 questions pertained to students’ level of confidence in providing various aspects of pharmaceutical care. Questions were formatted and scored based on a 5-point Likert scale ranging from 1=strongly disagree to 5=strongly agree. A Wilcoxon signed rank test was used to compare pre- and post-course survey responses, with an alpha < 0.05 considered significant. Of the 7 items in the organizational domain, significant increases in confidence were reported for 5 items (Table 4). Three of the 11 items in the pharmaceutical care domain reflected significant changes in confidence (Table 4).
Table 4.
Median Responses to Survey Instrument Items Pre- and Post-Coursea
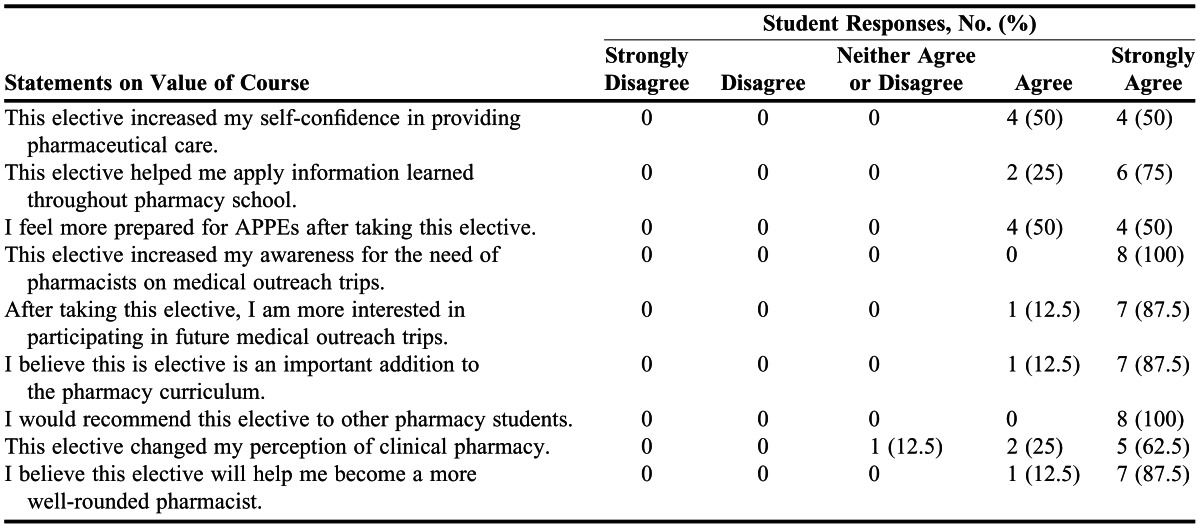
As an additional portion of the post-course survey instrument, students were asked to rate the value of individual course topics and activities (Table 5) and aspects of the course overall (Table 6). Responses to the 9 questions on course value indicated that students perceived the course to be highly valuable. All students (100%) strongly agreed that the elective course increased their awareness of the need for pharmacists on medical outreach teams and would recommend this elective course to other students. All students (100%) either agreed or strongly agreed that the elective course helped them apply information learned throughout pharmacy school, made them feel more prepared for APPEs, prepared them to become more well-rounded pharmacists, and was an important addition to the pharmacy curriculum. Additionally, students’ opinions of the course-specific topics indicated that they perceived the majority of topics to be valuable, with the exception of the fundraising project.
Table 5.
Student Responses to Post-Course Survey Items Related to Individual Course Topics and Activities, N = 8
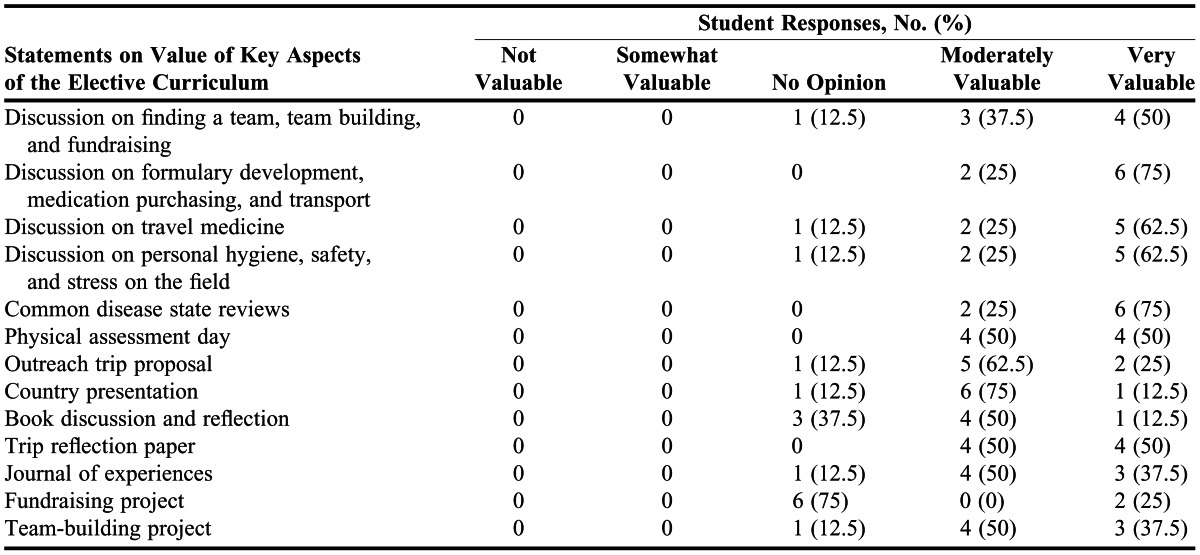
Table 6.
Student Responses to Post-Course Survey Items Related to Overall Value of the Course, N = 8
Subjective feedback was gathered from students’ responses to open-ended questions included in the post-course survey instrument to elicit feedback on the strengths, weaknesses, and value of the elective course. Themes that emerged from student comments were that: (1) the elective course provided a valuable opportunity to gain a different perspective of the practice of pharmacy, specifically as it related to the value of direct patient care and interaction with a multidisciplinary team; (2) the experience in a third-world country humbled them and made them appreciative of the resources available in the United States; and (3) there was a weakness in the spacing of various assignments throughout the course. Students clearly indicated that they felt that this experience would positively impact their careers as future pharmacists for a variety of reasons, including the opportunity to communicate so closely with physicians and patients, the involvement in therapeutic decision-making, and the close personal mentoring they received from course instructors and other medical personnel.
Student effort is also clear in the work report the group completed after they returned, which documented the number of patients treated, prescriptions dispensed, student pharmacist clinical interventions made, and patient counseling. During the trip, students provided medical care to 806 patients; along with faculty members, filled 1,652 prescriptions; and recorded 1,842 clinical interventions that were first approved by the faculty members.
Although the classroom portion of the course did not require additional fees, the trip itself entailed significant direct and indirect costs. All students and faculty members were responsible for their own travel expenses. The associated cost per participant, whether student or faculty member, was $2,000. Additional expenses included mandatory vaccinations and malaria prophylaxis for all participants. The number of vaccinations and the need for prophylactic medications for participants will vary by trip destination. After personal travel items and other miscellaneous expenses were calculated, students reported a total cost of approximately $2,500.
DISCUSSION
The primary goals of the course were to increase pharmacy students’ ability to provide patient care to culturally diverse and underserved populations and to increase students’ interest and participation in public health efforts both locally and internationally. Achievement of the specific course outcomes and objectives (Table 3) is supported by the results of the survey and based on the students’ successful completion of course activities.
Students gained valuable experience and demonstrated improved confidence in several organizational and pharmaceutical care components after completing the elective course, equipping them for future leadership roles in medical outreach. Because many organizations are using pharmacists as team leaders,8 mastery of the organizational skills within the elective course will prove beneficial should the students seek out these roles. There was not a significant increase in confidence for 2 organizational components of the course: finding opportunities to volunteer for medical outreach trips and fundraising for a medical outreach trip. Students did not have the opportunity for practical application of these skills, which were presented in the classroom portion of the course. Although students were required to develop fundraising plans as a course assignment, implementation of these plans was voluntary. All students opted out because of limited available time, the number of previously planned but unrelated school fundraisers held during the semester, and adequate existing monetary support.
In the assessment of pharmaceutical care components of the course, a significant increase in confidence was seen for 3 of the 11 survey items: taking a patient history and chief complaint, making therapeutic recommendations to physicians, and working with a multidisciplinary team. Students were heavily exposed to these areas during clinic time. Many third-year students have not had the opportunity to work closely with physicians and other healthcare professionals. This early and intense exposure created a foundation for their APPEs in the fourth year. The students agreed that the course helped them feel more prepared for APPEs, even commenting that the trip was like a “mini-APPE.” Students are exposed to many of the other pharmaceutical care components at various points in the core curriculum, an experience that may have contributed to higher initial scores seen in the pre-course survey. Overall, the survey analysis reflects positively on the students’ abilities to provide comprehensive patient-specific pharmaceutical care, communicate effectively, promote health improvement and self-care, think critically, and appropriately manage and use resources of the healthcare system.
Based on results from the follow-up questionnaire and open-ended student comments, the students gained far more than was assessed using our evaluation tools. Overall, student comments demonstrated that they were impacted both personally and professionally through experiences on the trip and that they gained significant confidence in their ability to practice pharmacy and interact with patients. This feedback embodies the goal of the elective: not only to impart confidence in the clinical skills necessary to participate in these trips but also to inspire students through the people they meet and the experiences they encounter. Brown and colleagues report that many students returning from medical mission trips have a newfound commitment to serve, a greater respect for their profession, and a sincere sense of gratitude for how well off they are in relation to others.9 The majority of our student comments align with these findings.
Other pharmacy colleges and schools considering initiating a similar course should consider the challenges involved in planning. A key part of the initial planning process for the course was garnering support from university and college administration. As an entirely new type of elective for the college, this part of the planning process was time consuming. The university reviewed the course to ensure legal soundness, which resulted in mandatory paperwork for participants that released the university from any trip-related liability. Chahine and colleagues also cite that this step should precede any serious trip planning.7 For other colleges and schools pursuing an elective course of this kind, initial planning should begin approximately 1 year prior to the anticipated start date for the elective course to allow adequate time for college and university review.
Another challenge was deciding how to select students for enrollment in the class. We used random selection from students who had expressed interest in participating; however, based on the large number of students interested, third-year students were given preference. Because of the small class size desired and the challenges of pretrip planning, it was important to ensure that those selected were committed to completing the course. The students were made aware of all costs and responsibilities prior to selection in order to prevent student dropout. Had unforeseen circumstances occurred and a student was not able to participate in the medical outreach trip, that student would have been required to complete local patient care activities, determined by faculty members, to fulfill the requirement of the elective course. The selection of a group of committed students as early as possible in the process also helped allow time for adequate team-building opportunities and personal preparation.9
Considering the logistical challenges of planning a trip of this type, partnering with an organization that has experience planning international medical outreach trips is a vital element for a successful experience. These organizations can help ensure that appropriate locations and additional team members, if needed, are selected to provide an environment that is conducive to meeting the goals of the course. Many local and national organizations dedicated to medical outreach can be found through online resources, such as www.medicalmissions.org or through word-of-mouth from past participants.12 This crucial step in the planning process should be initiated during the course development or at least 6-12 months prior to the predetermined travel date to ensure there is adequate time to plan the logistics of the trip and meet with the collaborating organization.
Although expenses can quickly become prohibitive when planning a medical outreach, costs have not yet become a problem for student recruitment or participation. Among students who have completed the course, all cite monetary concerns as negligible considerations when enrolling in the course. Nevertheless, fundraising will continue to be part of the course design to help defray the costs to student participants.
Students rated most topics and assignments in the course as valuable. In future course offerings, all topics and assignments will remain with some minor changes. Another class period for disease-state discussion will be added to offer students more opportunities to review pertinent clinical cases. Because many of the physicians look to the students for treatment recommendations, the students felt like an additional day to practice treatment recommendations would be beneficial. Also, the schedule will be adjusted to provide more time between assignments in an attempt to spread the work more evenly throughout the semester. Many students felt that the outreach trip proposal exercise should be split into separate due dates to avoid the temptation to procrastinate working on the project until the last week. The book discussion will also be shortened to occur over 2 class periods instead of 4 to allow for more focused discussion and increased time for other projects and course topics. A final change will be to make the fundraiser implementation a mandatory project and to place it earlier in the semester to allow students to gain experience and confidence in carrying out this key element of the Medical Outreach Experience.
Although it would have been ideal to have provided this experience to all interested students, resources were limited and decisions had to be made to ensure a quality experience for the students involved. While we believe that the design of the course as a semester-long elective is extremely beneficial for the students, other colleges have designed international outreach experiences for APPE elective credit.7 This approach not only consolidates the training and preparation, which we believe is essential to the success of the course, but also allows for more students to be involved. In future years, we may expand the program to include an additional APPE elective in international medical outreach while maintaining the medical outreach elective course.
SUMMARY
More opportunities for direct involvement in public health efforts will be created as the pharmacist’s role in the healthcare system continues to expand. Providing training and experience in international medical outreach gives interested students an opportunity to gain confidence in effectively planning and organizing a medical outreach trip. It also offers a chance to reinforce key pharmaceutical care skills introduced in the core pharmacy curriculum. This combination of experiences will increase students’ ability to provide population-based pharmaceutical care to patients, regardless of their chosen practice area, when they begin their professional career.
ACKNOWLEDGEMENTS
The authors acknowledge Southeastern Medical International for providing logistical support in the planning of this trip. We also thank the students (Dina Abdelhalim, Matthew Autin, Bryan Bordelon, Monica Hartman, Rebecca Overmier, Alison Seaman, William Whited, and Samantha Womack) and patients who made this first elective experience memorable and worthwhile. We also acknowledge Roy Parish, PharmD, and Jeffrey Evans, PharmD, for their contributions to the statistics and editing of this manuscript.
REFERENCES
- 1.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/standards/default.asp. Accessed June 18, 2012. [Google Scholar]
- 2.American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education (CAPE) educational outcomes 2004. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed June 18, 2012. [Google Scholar]
- 3.Vincent WR, Smith KM, Steinke D. Opportunities for pharmacists in public health. Am J Health-Syst Pharm. 2007;64(19):2002–2007. doi: 10.2146/ajhp070219. [DOI] [PubMed] [Google Scholar]
- 4.Johnson CA, Stieglitz N, Schroeder ME. Opportunities and responsibilities for pharmacists on short-term medical mission teams. J Am Pharm Assoc. 2009;49(6):801–807. doi: 10.1331/JAPhA.2009.08172. [DOI] [PubMed] [Google Scholar]
- 5.Clements JN, Rager ML, Vescovi EM. The value of pharmacy services on a short-term medical mission trip: description of services and assessment of team satisfaction. Ann Pharmacother. 2011;45(12):1576–1581. doi: 10.1345/aph.1Q328. [DOI] [PubMed] [Google Scholar]
- 6.Ward CT, Nemire RE, Daniel KP. The development and assessment of a medical mission elective course. Am J Pharm Educ. 2005;69(3) Article 50. [Google Scholar]
- 7.Chahine EB, Nornoo AO. Pharmacist involvement in medical missions: planning, execution, and assessment. Am J Health-Syst Pharm. 2012;69(8):636–643. doi: 10.2146/ajhp110497. [DOI] [PubMed] [Google Scholar]
- 8.Brown D, Ferrill MJ. Planning a pharmacy-led medical mission trip, part 1: Focus on medication acquisition. Ann Pharmacother. 2012;46(5):751–9. doi: 10.1345/aph.1Q531. [DOI] [PubMed] [Google Scholar]
- 9.Brown DA, Brown DL, Yocum CK. Planning a pharmacy-led medical mission trip, part 2: servant leadership and team dynamics. Ann Pharmacother. 2012;46(6):895–900. doi: 10.1345/aph.1Q547. [DOI] [PubMed] [Google Scholar]
- 10.Berger M. This is a Soul: The Mission of Rick Hodes. 1st ed. New York, NY: HarperCollins Publishers; 2010. [Google Scholar]
- 11.World Health Organization. WHO model list of essential medicines, 17th edition (March 2011). http://whqlibdoc.who.int/hq/2011/a95053_eng.pdf. Accessed October 24, 2012. [Google Scholar]
- 12.Medical Missions. Connecting volunteers with medical mission organizations. http://medicalmissions.org/. Accessed August 8, 2012. [Google Scholar]
- 13.The University of Louisiana at Monroe. ULM College of Pharmacy competency statements/educational outcomes. http://ulm.edu/pharmacy/mpaedoutcomes.html. Accessed July 10, 2012. [Google Scholar]


