Abstract
A key factor in the development of type II diabetes is the loss of insulin-producing beta-cells. Human islet amyloid polypeptide protein (human-IAPP) is believed to play a crucial role in this process by forming small aggregates that exhibit toxicity by disrupting the cell membrane. The actual mechanism of membrane disruption is complex and appears to involve an early component before fiber formation and later component associated with fiber formation on the membrane. By comparing the peptide-lipid interactions derived from solid-state NMR experiments of two IAPP fragments that bind the membrane and cause membrane disordering to IAPP derived peptides known to cause significant early membrane permeabilization, we show here that membrane disordering is not likely to be sufficient by itself to cause the early membrane permeabilization observed by IAPP, and may play a lesser role in IAPP membrane disruption than expected.
Introduction
Type II diabetes is a progressive disease linked to both inadequate insulin production and resistance to insulin’s effects. In the first phase of the disease, the body develops resistance to insulin; in response, pancreatic secretion of insulin is elevated (hyperinsulinemia).1 In the second phase, insulin producing pancreatic β-cells begin to die and the production of insulin declines.1 The combination of both decreased insulin sensitivity and decreased insulin production has been hypothesized to contribute to the development of overt type II diabetes.
Plaques of the aggregated protein amylin, or human islet amyloid polypeptide protein (human-IAPP), have been found upon post-mortem examination in the pancreatic β-cells in >90 % of type 2 diabetic patients, but not in aged-matched non-diabetic cohorts.1-3 Since their secretion is physiologically linked, an elevation in insulin production results concurrently in elevated levels of human-IAPP. Consequently, the human-IAPP is thought to damage insulin-producing β-cells, eventually resulting in type II diabetes.4 The mechanism by which human-IAPP induces cytotoxicity has been the focus of extensive investigation. Several models have been reported primarily focusing on IAPP-mediated cellular membrane damage, including the formation of membrane pores similar to ion-channels5-7 and a total disruption of the bilayer by direct uptake of phospholipid molecules during fibrillogenesis.8-13 To obtain a more detailed understanding on the cell toxicity, it is necessary to understand how the peptide affects the physical properties of the membrane.
Previous investigations showed membrane disruption by human-IAPP12-15 and other amyloidogenic peptides such as Aβ1-4016 actually consists of two separate processes. Immediately after its addition to the membrane, human-IAPP increases membrane permeability while leaving the membrane structurally intact. In a later process correlated with amyloid fibril formation, the membrane structural integrity is lost and the membrane fragmented. The second process is relatively well understood and seems to be related to the extraction of lipid molecules into the exposed fiber surfaces as fiber formation proceeds on the surface of the membrane.8, 11, 17, 18 The initial process, on the other hand, is less well understood. For the Aβ1-40 protein, single channel recording measurements and fluorescence measurements have suggested early membrane permeabilization before amyloid formation likely corresponds to the formation of channels that are at least superficially similar to traditional ion channels. 16, 19 Studies on human-IAPP are much less clear. Electrical recording of human-IAPP has variously showed either discrete conductance changes consistent with ion channel-like structures6, 20, 21 or non-specific conductance changes more consistent with membrane thinning.22, 23 Similarly, fluorescence studies have suggested either stable pores24 or a non-selective transient pores25, 26 may be responsible for this early stage of membrane disruption.
A greater understanding of the actual mechanism of membrane disruption by human-IAPP can be achieved by separating the two processes. The relative efficiency of these two processes is affected by membrane composition11, 13 and membrane fragmentation can be blocked completely by amyloid inhibitors.10, 12 Furthermore, these two processes appear to be localized in two different regions of the peptide. Recent models suggest that the membrane toxicity by human-IAPP may be mediated first by insertion of the N-terminal region (presumably via electrostatic interactions with the negatively charged phospholipids) and then aggregation via the 20-29 region.27 The N-terminal fragment of human-IAPP (human-IAPP1-19) can strongly disrupt β-cell membranes28 and certain types of artificial liposomes.14, 28 Interestingly, this peptide does not form amyloid when bound to the membrane.14 On the other hand, a stretch of amino acids within the central region of the peptide (20-29) is sufficient to both form amyloid fibers and cause membrane fragmentation.10 However, human-IAPP20-29 does not appear to cause the initial stage of membrane disruption.28 Therefore, there is considerable interest in investigating the interaction of these peptides with phospholipid membranes in an effort to solve the conflicting mechanistic models of membrane damage caused by IAPP.
In the current study, the membrane interaction of the 20-29 fragment of human-IAPP (SNNFGAILSS) and the non-amyloidogenic and non-toxic rat-IAPP version (SNNLGPVLPP) is characterized by differential scanning calorimetric (DSC), fluorescence, and solid-state NMR experiments. We show that the binding of both human-IAPP20-29 and rat-IAPP20-29 cause considerable disorder in the membrane. However, this disorder is not linked in either peptide to substantial membrane disruption. Furthermore, the particular type of disorder is substantially different from that caused by IAPP1-19 samples. These findings suggest the initial phase of membrane disruption may not be related to disorder in the membrane and instead may reflect a separate process such as the formation of channels.
MATERIALS AND METHODS
Peptide synthesis
All protected amino acids were purchased from Bachem, Anaspec, and Synthetech. Coupling agents and resins were purchased from Bachem and Midwest Biotech. Solvents and deprotecting agents were obtained from Fisher Scientific and Aldrich Chemical Co. The peptide was prepared on a PS3 Automated Peptide Synthesizer from Protein Technologies using standard solid phase techniques for fluorenylmethyloxycarbonyl (Fmoc) protected amino acids on Rink amide p-methylbenzhydrylamine (MBHA) resin (0.64 mmole/g) on a 0.1 mmole scale. This resin produces a C-terminally amidated peptide upon cleavage similar to the naturally produced peptide which also facilitates comparison to previous studies.10 The side chains of Ser and Thr were protected as the t-butyl derivatives. The deprotection solution for the N-terminal amine was 20% piperidine in N,N-dimethylformamide (DMF). O-(Benzotriazol-1yl)-1, 1, 3, 3-tetramethyluronium hexafluorophosphate (HBTU) was used as a coupling agent, activated by 0.4 M N,N-diisopropylethylamine (DIEA) in DMF. The N-terminal Fmoc group was removed, and acetylation was accomplished by treatment with acetic anhydride. Simultaneous deprotection and cleavage from the resin were accomplished by treatment with 11 mL 90% trifluororacetic acid (TFA)/10% scavenger cocktail (anisole, thioanisole, phenol, water). The reaction was begun at 0 °C, allowed to warm to room temperature and stirred for 2 hours. The uncharged resin was separated from the solution by filtration. The peptide was precipitated with cold diethyl ether, filtered, redissolved in 30% acetonitrile/70% water and lyophilized. Crude peptides were purified to homogeneity by preparative reversed-phase high performance liquid chromatography (RP-HPLC) on a Waters instrument with a Phenomenex Jupiter C18 column (2.2 × 25.0 cm, 10 mL/min). A linear gradient of 10% acetonitrile (0.1% TFA)/water (0.1% TFA) to 50% acetonitrile (0.1% TFA)/water (0.1% TFA) was employed, followed by lyophilization. Peptide purity was assessed by analytical reversed phase-HPLC. The peptide was >97% pure as analyzed by peak integration. Electrospray or matrix-assisted laser desorption ionization time-of-flight (MALDI-TOF) mass spectroscopy confirmed the appropriate molecular weight.
Preparation of large unilamellar vesicles (LUVs) and dye leakage assay
Lipid vesicles were created and filled with carboxyfluorescein, which upon disruption of the membrane leak into the surrounding buffer. The release of the carboxyfluorescein results in an increase in fluorescence due to the elimination of self-quenching of carboxyfluorescein within the vesicle. Baseline controls were compared to runs with added peptide and added detergent (which acted as a positive control to give 100% leakage). Percent leakage could then be plotted versus time to monitor the peptide-induced membrane disruption.
Vesicles with externally added human- or rat-IAPP20-29 were prepared by taking 5 mg of 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphoglycerol (POPG), a negatively charged phospholipid purchased from Avanti Polar Lipids (Alabama), and dissolving it in 2 mL of chloroform. Vesicles with incorporated peptide were prepared similarly except human- or rat-IAPP20-29 dissolved at 4 mg/ml in methanol was added to the sample. The chloroform was evaporated by a stream of nitrogen gas to create a thin film of dry lipids on the sides of a test tube, which was then dried in a vacuum dessicator overnight. 500 μL of a 30 mM carboxyfluorescein dye solution in pH 7.5 sodium phosphate buffer solution was added to the previously prepared dried lipid to make a 13 mM solution of multilamellar vesicles (MLVs). This solution was vortexed to thoroughly mix the components and then subsequently frozen using liquid nitrogen and thawed five times consecutively. This solution was then extruded 21 times through polycarbonate filters (pore size 100 nm) using a mini-extruder from Avanti Polar Lipids, fitted with two 0.5 mL Hamilton gastight syringes, producing LUVs. To remove nonencapsulated carboxyfluorescein, the LUV solution was placed on a Sephadex G50 gel exclusion column and the first colored fragment, the separated dye-containing vesicles, was collected.
To make the peptide solution, the purified peptide was dissolved in dimethyl sulfoxide (DMSO) and sonicated for one minute. This peptide solution was added in aliquots to the vesicle solution. The isolated LUVs containing the carboxyfluorescein were analyzed using scanning FT-vis spectroscopy to determine that the wavelength of maximum absorption was 490 nm. Using a scanning spectrofluorometer, the wavelength of maximum absorbance was set as the excitation wavelength and the emission wavelength was determined to be 520 nm. An aliquot of 40.0 μL of the vesicle solution was added to 3.00 mL of sodium phosphate buffer in a clear plastic 4 mL cuvette to make a 173 μM solution of LUVs and then the peptide solution was added in increasing amounts per sample. Immediately upon adding the peptide solution, the cuvette was inverted and inserted into the spectrofluorometer, and a time-course fluorescence spectrum was taken over at least 300 seconds. A fresh vesicle solution was used for each experiment. The control used to determine 100% leakage was detergent, 40.0 μL Triton X, (10% v/v in buffer), which induced the release of any remaining dye from vesicles, resulting in the highest possible fluorescence. Dye leakage was reported by the following equation:
where Fbaseline is the fluorescence of the LUVs without the peptide.
Solid-state NMR experiments
DMPC/DHPC bicelles at a q-ratio of 3 and a hydration level of 66% (wt/wt) were prepared as described previously using a solution of rat-IAPP20-29 in methanol to incorporate the peptide prior evaporation of the lipid film.29 All NMR experiments were performed on a Chemagnetics/Varian Infinity 400 MHz solid-state NMR spectrometer using a double-resonance 5 mm MAS probe. 31P NMR spectra, used to confirm the magnetic-alignment of bicelles, were recorded using a spin-echo pulse sequence (90°–τ–180°–τ-acquisition; τ=125 μs) with a 5 μs 90°-pulse length and a 30 kHz RF decoupling of protons. 31P chemical shift spectra were referenced relative to the isotropic chemical shift peak of phosphoric acid (0 ppm). 14N NMR spectra were obtained using a quadrupolar-echo pulse sequence (90°–τ–90°–τ-acquisition; τ=80 μs) without proton decoupling. 2D Proton detected local field (PDLF) spectra correlating 13C chemical shift and 1H-13C dipolar coupling were recorded as described elsewhere.30, 31 A ramped-cross-polarization (ramp-CP) pulse sequence to transfer the proton magnetization to 13C after the t1 period with a 3 ms contact time, 70 t1 increments, a 5 s recycling delay, and a 25 kHz FLOPSY-8 proton decoupling were used to obtain 2D PDLF spectra. All measurements were performed at 37 °C by keeping the bilayer normal of aligned bicelles perpendicular to the direction of the external magnetic field. The samples were equilibrated for 30 minutes at 37 °C before acquisition.
Differential scanning calorimetry (DSC)
DSC experiments were performed using a Nano-DSC II instrument (Calorimetry Sciences, Provo, UT, USA) over a temperature range of 5-45 °C with a total of four heating and four cooling scans. Heating scans were run at 0.25 °C/min, and cooling scans at 1.0 °C/min, with a 10 min equilibration period in between. The raw data were converted to molar heat capacity using the CP Calc program provided with the calorimeter. Experiments were performed on 1,2-dimyristoyl-sn-glycero-3-phosphocholine (DMPC) MLVs, prepared as described above for the dye leakage experiments, with human-IAPP20-29/lipid mole ratios of 0.5%, 1%, and 4% and rat-IAPP20-29/lipid mole ratios of 0.5%, 0.75%, 1%, 2%, and 4%. Sodium phosphate buffer (10 mM) with 150 mM NaCl at pH 7.3 was used to hydrate the samples and this buffer solution was used as a reference cell.
RESULTS
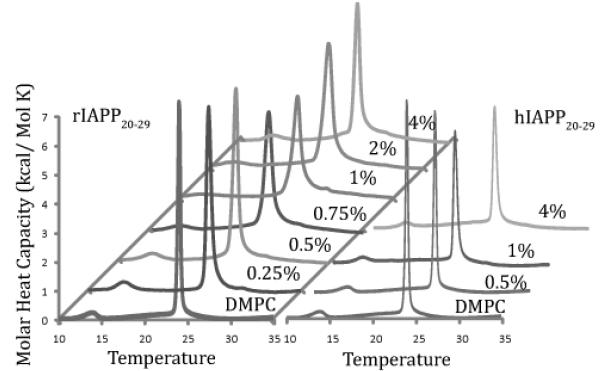
Both human- and rat-IAPP20-29 likely bind at the membrane surface
The effect of human and rat-IAPP20-29 on phospholipid membranes was first measured with differential scanning calorimetry. The DSC experiments measure the molar heat capacity required for the phase transition from the more ordered gel phase to the more disordered liquid crystalline phase. If the gel phase of the lipid bilayer is already disordered due to the interfering effects of a peptide like IAPP, then the heat required for the transition is lowered relative to the pure lipid sample. The molar heat capacity for the phase transition is decreased in the presence of both the human and rat versions of IAPP20-2928. In particular, the thermograms of both human and rat-IAPP20-29 show substantial broadening of the phase transition at low (<1%) concentrations, while full-length human and rat-IAPP1-37 and the rat and human N-terminal 1-19 fragments only show broadening at higher concentrations.28, 32 This indicates that both human and rat-IAPP20-29 peptides may penetrate partly into the hydrophobic core, disrupting lipid-lipid interactions and inhibiting the cooperativity of the phase transition, resulting in a decrease in peak intensity relative to the pure lipid. Rat-IAPP20-29 shows an unusual membrane disrupting effect that increases with increasing concentration up to 1% peptide (Figure 1), and then decreases again (effect reversed) as the percentage of peptide rises above 1% (Figure 1), which may indicate self-association into domains at higher concentrations. Overall, the results are suggestive of a surface-associated mode of binding for both peptides, since a peptide with deeper penetration creates less void spaces and therefore has less of an effect on the lipid-lipid interactions within the hydrophobic core of lipid bilayers.
Fig. 1.
Effect of human-IAPP20-29 or rat-IAPP20-29 on the gel phase to liquid crystalline phase transition of DMPC bilayers as a function of the peptide concentration. Low concentrations of both human-IAPP20-29 and rat-IAPP20-29 cause a substantial decrease in the molar heat capacity.
Non-amyloidogenic rat-IAPP20-29 induces disorder in the membrane interior of DMPC bicelles
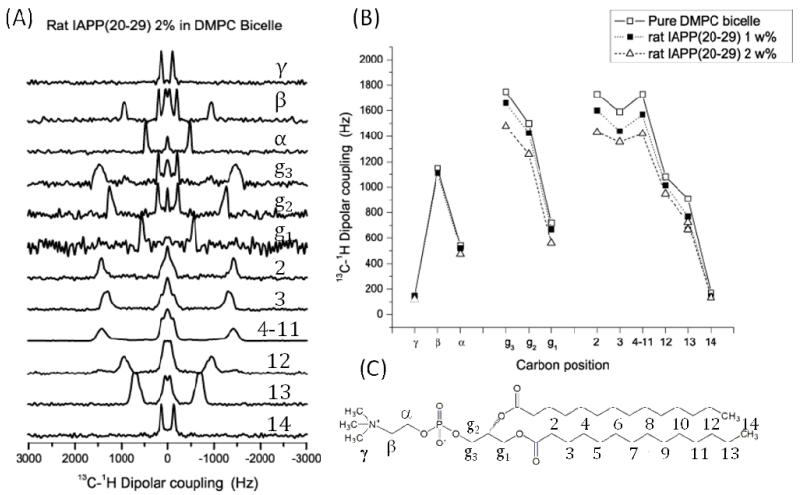
The DSC experiments gave indirect evidence that both human and rat-IAPP20-29 bind near the membrane surface, causing disorder in the membrane. For more direct evidence of membrane disorder, we attempted to measure 13C-1H dipolar couplings from magnetically-aligned bicelles using the 2D PDLF solid-state NMR experiment. The measured values of dipolar couplings are closely connected to the order parameter of the membrane, an increase in acyl chain motion at a particular atomic site in the lipid for example will decrease the measured dipolar coupling due to additional motional averaging of the dipolar interaction at that location. Attempts at aligning bicelles containing human-IAPP20-29 failed, possibly due to the influence of amyloid formation at high concentration. Based on the DSC results, which showed surface binding modes are probable for both peptides (Fig.1), we proceeded with bicelles containing non-amyloidogenic rat-IAPP20-29. Dipolar coupling values for bicelles containing rat-IAPP20-29 are presented in Fig. 2. Rat-IAPP20-29 caused a substantial, concentration dependent decrease in the observed dipolar coupling values, consistent with a decrease in the overall order of the membrane. Most of the disordering effect of rat-IAPP20-29 is concentrated within the membrane interior (carbons 2-13) and in the glycerol backbone in the interfacial region (carbons g1, g2 and g3). Little to no disordering occurs in the lipid head group (α, β, and γ positions). This pattern is commonly observed with many antimicrobial peptides31,47 and is consistent with a peptide that lies close to the surface of the lipid bilayer near the interfacial region. This is noticeably different from the pattern of dipolar coupling changes associated with the binding of the N-terminal rat-IAPP1-19 fragment or the full-length rat-IAPP1-37 peptide, neither of which caused a substantial change in the order of the membrane.33 Surface-associated peptides generally create a void within the membrane interior, causing disorder in the packing of the acyl chains, while more deeply penetrating peptides have little influence on acyl chain packing since they do not create such a void volume.
Fig. 2.
13C-1H dipolar coupling values of DMPC in magnetically-aligned 3:1 DMPC:DHPC bicelles with and without rat-IAPP20-29 using 2D PDLF solid-state NMR experiments at 37 °C. (A) Sample 1H-13C dipolar coupling spectral slices extracted from the 2D PDLF spectrum of bicelles containing 2% rat-IAPP20-29. (B) Dipolar coupling values calculated from the 2D PDLF experiment. Carbons 4-11 are poorly resolved and therefore represented as a single average value. (C) Labeling scheme for DMPC.
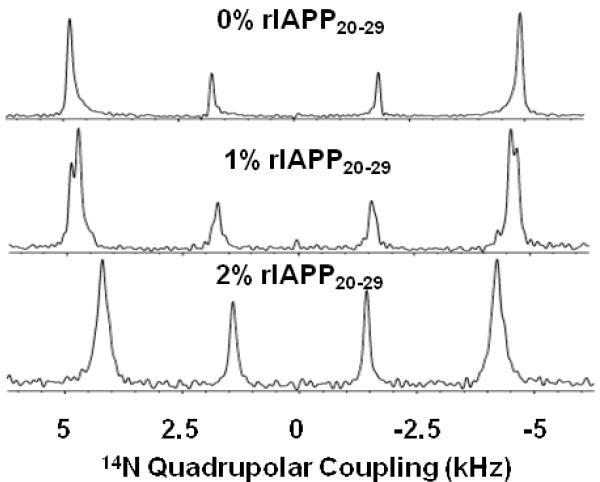
14N quadrupole coupling NMR spectra suggest rat-IAPP20-29 localizes in flat, DMPC rich regions of the bicelle
The bicelles used here are composed of two lipids, DMPC and DHPC, which are phase segregated in the bicelles to form DMPC rich flat lamellar regions and curved DHPC perforations.34 The N-terminal 1-19 fragment of rat-IAPP, but not the full length rat-IAPP1-37 peptide, has the somewhat unusual property of localizing to the curved regions of the bicelles where DHPC resides.33 This localization to curved regions was correlated with the increased ability of toxic versions of IAPP to favor formation of curvature in the membrane relative to rat-IAPP1-37. The localization rat-IAPP1-19 to the curved regions of the bicelle was most clear in the 14N quadrupolar spectra in which the quadrupolar splitting of DHPC is strongly increased while 14N quadrupolar coupling splitting of DMPC is relatively unaffected.33 On the other hand, rat-IAPP1-37 predominantly changes the 14N quadrupolar splitting of DMPC in bicelles, suggesting localization to the flat lamellar regions. The 14N quadrupolar coupling spectra of 1 and 2 mole % rat-IAPP20-29 is shown in Fig. 3. The outer and inner quadrupolar doublets in the spectra originate from DMPC and DHPC respectively. As seen from Fig. 3, the interaction of peptide with bicelles decreases the quadrupole splittings associated with both DMPC and DHPC. The presence of 1% rat-IAPP20-29 results in 2 partially resolved resonances for DMPC: the quadrupolar splitting for one is identical to peptide-free bicelles and in the other quadrupole splitting is slightly decreased. The addition of 2 mole % peptide greatly reduces the intensity of the DMPC resonance while leaving the DHPC relatively unaffected. While the intensity of the DMPC resonance is greatly reduced, the line-width is similar to other samples. This finding suggests the 14N quadrupolar signal of a substantial population of the DMPC lipid molecules is broadened beyond detection, consistent with the DSC results suggesting possible phase segregation of rat-IAPP20-29 in the membrane. The relative changes in the intensity and, to a lesser extent, the relative changes in the quadrupolar splitting in the 14N spectra are not consistent with rat-IAPP20-29 localizing in the curved regions of the bicelles like rat-IAPP1-19. Instead, rat-IAPP20-29 appears to be distributed throughout the bicelles, probably more in the flat DMPC region at least at higher concentrations.
Fig. 3.
14N quadrupole coupling spectra of magnetically-aligned 3:1 DMPC:DHPC bicelles containing rat-IAPP20-29.
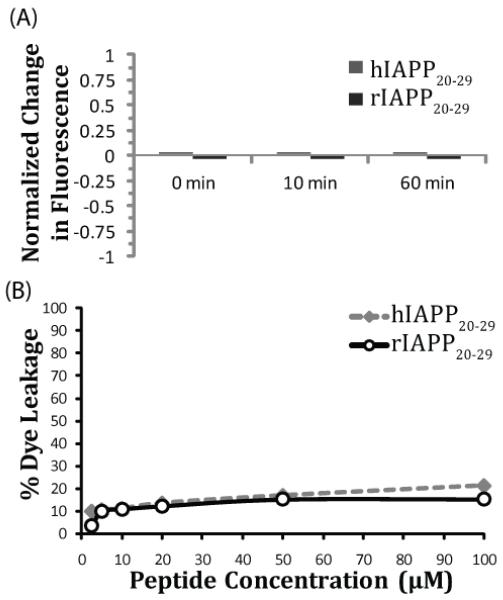
Neither rat nor human-IAPP20-29 causes significant membrane permeabilization in the absence of amyloid formation
The DSC experiments suggest both human and rat-IAPP20-29 perturb the interior of the membrane which was confirmed for rat-IAPP20-29 by measurements of 13C-1H dipolar couplings. Given that both peptides apparently disorder the membrane, it is natural to ask if either peptide is capable of causing membrane permeabilization. Previous results indicate that the degree of membrane disruption by human-IAPP20-29 before fiber formation is relatively minor,35 even when it is incubated with anionic POPG vesicles which should maximize binding.14 Results from the dye leakage experiments to measure membrane permeabilization can be found in Figure 4. However, all of the DSC and NMR experiments were performed with the peptide incorporated into the lipid film before hydration of the vesicles, which may lead to difference when compared to samples in which peptide in solution is allowed to bind the membrane from the external solution. Such a difference has been observed for Aβ1-40 in which Aβ1-40 pre-incorporated into the membrane has a much greater helical content and different response to membrane charge than Aβ1-40 added externally.36
Fig 4.
Dye leakage assay for human and rat-IAPP20-29. (A) Normalized fluorescence changes for 1 mole % rat and human-IAPP20-29 incorporated into the POPC vesicles before the assay. (B) Percent dye leakage in POPG vesicles for rat and human-IAPP20-29 added externally. Lipid concentration for this experiment is 173 μM.
Recognizing this possibility, we first measured membrane permeabilization of vesicles with human and rat-IAPP20-29 incorporated into the membrane in a manner similar to the DSC and NMR experiments (Figure 4a). In this assay, disruption of vesicles by the peptide induces dye leakage. In this particular assay, lower fluorescence than the control sample indicates that the dye has leaked out of the vesicle before the separation of the dye-filled vesicles and the free dye. A higher fluorescence would result if membrane disruption is slower and the majority of the dye leakage occurs after separation of the free dye. Higher fluorescence in this situation occurs because leakage of the dye from the vesicles eliminates the self-quenching effect of carboxyfluorescein at high concentrations. It can be seen from Figure 4a that neither human nor rat-IAPP20-29 affects the membrane integrity even when directly incorporated into the membrane at 1 mole %. We also confirmed that neither human nor rat-IAPP20-29 could efficiently permeabilize the membrane even at saturating concentrations, using anionic POPG vesicles to maximize binding (Figure 4b). In these samples, only a slight increase in dye leakage could be detected after the addition of the peptide, even after the peptide concentration was increased from 2.5 μM (1.4 mole %) to a saturating concentration of 20 μM (11.5 mole %).
The data indicate minimal membrane disruption by both human and rat-IAPP20-29 when compared to the full-length IAPP peptide,14, 35 the N-terminal fragment,14, 28, 35 or to other membrane disrupting peptides.37 Previous studies have shown that the full-length rat-IAPP can bind to membranes and can induce membrane disruption in anionic vesicles at high peptide to lipid ratios.38 Similarly, rat-IAPP1-37 is also toxic at high concentrations to cells.39 In this context, it should be noted that the rat-IAPP20-29 analog exhibited a similar membrane disruption to the corresponding human analog (21% at 100 μM peptide concentration for human-IAPP20-29 vs. 17% for rat-IAPP20-29). In fact, at all concentrations tested, the percentage leakage for the rat analog was within five percent of that caused by the human analog, although never greater in magnitude. However, neither peptide caused significant membrane disruption under these conditions.
DISCUSSION
Membrane disruption has been reported to be a key component of amyloidogenic proteins toxicity. However, the complexity of the time-dependent aggregation process makes it difficult to study the peptide-lipid interaction of amyloidogenic proteins in general at the atomic-level. To overcome this obstacle, there is an increase in the use of model peptides that are more stable than the full system but retain some aspects of the properties being studied.40 One such model is the human-IAPP1-19 peptide, which does not form amyloid but does show an early phase of membrane disruption.14, 15, 27, 28, 41 Another minimal model is the human-IAPP20-29 fragment, which is one of the smallest stretch of residues in IAPP that can form amyloid and is where most of the variation between the amyloidogenic human and non-amyloidogenic rat variants of the peptide lies.42 By comparing the types of membrane interactions in both types of peptides, an idea of the relative importance of the two types of interactions in membrane permeabilization can be obtained.
Several differences could be detected in the membrane interaction of human and rat-IAPP20-29 and human and rat-IAPP1-19. First, human and rat-IAPP1-19 bind as helices to the membrane28 while the shorter human-IAPP20-29 adopts a β-turn structure.43 The DSC thermograms of both human and rat-IAPP20-29 indicate relatively strong disordering of the membrane interior at low concentrations (Fig. 1), while membrane disordering is only apparent at higher concentrations for the N-terminal 1-19 fragments.28 Similarly, solid-state NMR of the lipid bilayer directly shows disordering of the membrane when rat-IAPP20-29 binds to bicelles. Rat-IAPP20-29 disorders the hydrophobic core of the membrane and the interfacial glycerol region of the membrane to a lesser extent (Fig. 2). Similar experiments with rat-IAPP1-19 show a completely different pattern. Rat-IAPP1-19 has a minimal effect on membrane order, and the changes that do exist indicate a slight increase in order, rather than decrease.33 Finally, the 14N quadrupole coupling spectra suggest rat-IAPP1-19 primarily localizes to the curved regions of bicelles33 while rat-IAPP20-29 appears to be more uniformly distributed (Fig. 3).
These differences appear to result in a substantial difference in membrane permeabilization in the two peptides. The helical form of human and rat-IAPP1-19 can cause substantial membrane permeabilization in at least some types of membrane vesicles,14,25, 28 and both human and rat-IAPP1-19 have been shown to cause calcium influx in β-cells suggestive of membrane disruption.15, 28 This finding suggests amyloid formation may be sufficient for membrane disruption by IAPP but may not be strictly necessary. There is evidence the inverse of this statement, that IAPP variants with less tendency to form helices are less toxic, is also true. A double mutant of human-IAPP1-37 (L12N/N14L) forms similar fibers as the wild-type IAPP peptide, but has a decreased tendency to form a helical structure.44 This peptide is substantially less toxic than wild-type human-IAPP1-37, suggesting helical, non-fibrillar forms of IAPP may be at least partially responsible for toxicity in vivo.39 On the other hand, early membrane permeabilization by human and rat-IAPP20-29 is negligible in the absence of fiber formation, even at high concentrations designed to minimize the difference in membrane affinities between the two types of peptides (Fig. 4).27 This finding suggests membrane disordering is at least not a sufficient condition for early membrane disruption by IAPP. It should be noted, however, that human-IAPP20-29 can fragment the membrane during fiber formation in a different process,10 which is likely not detected here because of the high concentrations needed for fiber formation by human-IAPP20-29,45, 46 and the apparently narrow concentration range in which this process occurs for human-IAPP20-29.10
Conclusions
The actual relevance of early membrane permabilization to IAPP toxicity relative to later membrane fragmentation is controversial.15, 25 The toxicity of human-IAPP20-29 has not been well studied, although it has been reported that while fibrillar forms of the peptide are moderately toxic at high concentrations, soluble forms of human-IAPP20-29 are non-toxic.45 This finding largely agrees with the two step model of dye leakage, in which membrane fragmentation by IAPP is correlated with fiber formation on the membrane surface and another process not related to fiber formation is related to early membrane disruption.12, 13 As such, the lower toxicity of human-IAPP20-29 would appear to support the importance of early membrane permeabilization in IAPP toxicity.
Acknowledgments
This work was supported by funds from the NIH (GM084018, GM095640 and RR023597) to AR and by an award of Research Corporation to DLH. We thank Dr. Ulrich Dürr and Dr. Dong-KukLee help with solid-state NMR instrument and measurements.
References
- 1.Hoppener JWM, Ahren B, Lips CJM. N. Engl. J. Med. 2000;343:411–419. doi: 10.1056/NEJM200008103430607. [DOI] [PubMed] [Google Scholar]
- 2.Kahn SE, Andrikopoulos S, Verchere CB. Diabetes. 1999;48:241–253. doi: 10.2337/diabetes.48.2.241. [DOI] [PubMed] [Google Scholar]
- 3.Hull RL, Westermark GT, Westermark P, Kahn SE. J. Clin. Endocrinol. Metab. 2004;89:3629–3643. doi: 10.1210/jc.2004-0405. [DOI] [PubMed] [Google Scholar]
- 4.Westermark P, Andersson A, Westermark GT. Physiol. Rev. 2011;91:795–826. doi: 10.1152/physrev.00042.2009. [DOI] [PubMed] [Google Scholar]
- 5.Demuro A, Mina E, Kayed R, Milton SC, Parker I, Glabe CG. J. Biol. Chem. 2005;280:17294–17300. doi: 10.1074/jbc.M500997200. [DOI] [PubMed] [Google Scholar]
- 6.Mirzabekov TA, Lin MC, Kagan BL. J. Biol. Chem. 1996;271:1988–1992. doi: 10.1074/jbc.271.4.1988. [DOI] [PubMed] [Google Scholar]
- 7.Anguiano M, Nowak RJ, Lansbury PT. Biochemistry. 2002;41:11338–11343. doi: 10.1021/bi020314u. [DOI] [PubMed] [Google Scholar]
- 8.Sparr E, Engel MFM, Sakharov DV, Sprong M, Jacobs J, de Kruijff B, Hoppener JWM, Killian JA. FEBS Lett. 2004;577:117–120. doi: 10.1016/j.febslet.2004.09.075. [DOI] [PubMed] [Google Scholar]
- 9.Green JD, Kreplak L, Goldsbury C, Blatter XL, Stolz M, Cooper GS, Seelig A, Kist-Ler J, Aebi U. J. Mol. Biol. 2004;342:877–887. doi: 10.1016/j.jmb.2004.07.052. [DOI] [PubMed] [Google Scholar]
- 10.Brender JR, Durr UHN, Heyl D, Budarapu MB, Biochim A. Ramamoorthy, Biophys. Acta. 2007;1768:2026–2029. doi: 10.1016/j.bbamem.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Engel MF, Khemtemourian L, Kleijer CC, Meeldijk HJ, Jacobs J, Verkleij AJ, de Kruijff B, Killian JA, Hoppener JW. Proc. Natl. Acad. Sci. U. S. A. 2008;105:6033–6038. doi: 10.1073/pnas.0708354105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brender JR, Lee EL, Hartman K, Wong PT, Ramamoorthy A, Steel DG, Gafni A. Biophys. J. 2011;100:685–692. doi: 10.1016/j.bpj.2010.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sciacca MFM, Brender JR, Lee DK, Ramamoorthy A. Biochemistry. 2012;51:7676–7684. doi: 10.1021/bi3009888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brender JR, Lee EL, Cavitt MA, Gafni A, Steel DG, Ramamoorthy A. J. Am. Chem. Soc. 2008;130:6424–6429. doi: 10.1021/ja710484d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brender JR, Salamekh S, Ramamoorthy A. Acc. Chem. Res. 2012;45:454–462. doi: 10.1021/ar200189b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sciacca MFM, Kotler SA, Brender JR, Chen J, Lee DK, Ramamoorthy A. Biophys. J. 2012;103:702–710. doi: 10.1016/j.bpj.2012.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Milanesi L, Sheynis T, Xue WF, Orlova EV, Hellewell AL, Jelinek R, Hewitt EW, Radford SE, Saibil HR. Proc. Natl. Acad. Sci. U. S. A. 2012;109:20455–20460. doi: 10.1073/pnas.1206325109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michikawa M, Gong JS, Fan QW, Sawamura N, Yanagisawa K. J. Neurosci. 2001;21:7226–7235. doi: 10.1523/JNEUROSCI.21-18-07226.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schauerte JA, Wong PT, Wisser KC, Ding H, Steel DG, Gafni A. Biochemistry. 2010;49:3031–3039. doi: 10.1021/bi901444w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hirakura Y, Yiu WW, Yamamoto A, Kagan BL. Amyloid. 2000;7:194–199. doi: 10.3109/13506120009146834. [DOI] [PubMed] [Google Scholar]
- 21.Quist A, Doudevski L, Lin H, Azimova R, Ng D, Frangione B, Kagan B, Ghiso J, Lal R. Proc. Natl. Acad. Sci. U. S. A. 2005;102:10427–10432. doi: 10.1073/pnas.0502066102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harroun TA, Bradshaw JP, Ashley RH. FEBS Lett. 2001;507:200–204. doi: 10.1016/s0014-5793(01)02972-6. [DOI] [PubMed] [Google Scholar]
- 23.Kayed R, Sokolov Y, Edmonds B, McIntire TM, Milton SC, Hall JE, Glabe CG. J. Biol. Chem. 2004;279:46363–46366. doi: 10.1074/jbc.C400260200. [DOI] [PubMed] [Google Scholar]
- 24.Last NB, Rhoades E, Miranker AD. Proc. Natl. Acad. Sci. U. S. A. 2011;108:9460–9465. doi: 10.1073/pnas.1102356108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khemtemourian L, Engel MFM, Liskamp RMJ, Hoppener JWM, Killian JA. Biochim. Biophys. Acta. 2010;1798:1805–1811. doi: 10.1016/j.bbamem.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 26.Lee CC, Sun Y, Huang HW. Biophys. J. 2012;102:1059–1068. doi: 10.1016/j.bpj.2012.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Engel MFM, Yigittop H, Elgersma RC, Rijkers DTS, Liskamp RMJ, de Kruijff B, Hoppener JWM, Killian JA. J. Mol. Biol. 2006;356:783–789. doi: 10.1016/j.jmb.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 28.Brender JR, Hartman K, Reid KR, Kennedy RT, Ramamoorthy A. Biochemistry. 2008;47:12680–12688. doi: 10.1021/bi801427c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamamoto K, Soong R, Ramamoorthy A. Langmuir. 2009;25:7010–7018. doi: 10.1021/la900200s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dvinskikh SV, Durr UHN, Yamamoto K, Ramamoorthy A. J. Am. Chem. Soc. 2007;129:794–802. doi: 10.1021/ja065536k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dvinskikh S, Durr U, Yamamoto K, Ramamoorthy A. J. Am. Chem. Soc. 2006;128:6326–6327. doi: 10.1021/ja061153a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sciacca MFM, Pappalardo M, Milardi D, Grasso DM, La Rosa C. Arch. Biochem. Biophys. 2008;477:291–298. doi: 10.1016/j.abb.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 33.Smith PES, Brender JR, J A. Ramamoorthy, Am. Chem. Soc. 2009;131:4470–4478. doi: 10.1021/ja809002a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gaemers S, Bax A. J. Am. Chem. Soc. 2001;123:12343–12352. doi: 10.1021/ja011967l. [DOI] [PubMed] [Google Scholar]
- 35.Heyl DL, Osborne JM, Pamarthy S, Samisetti S, Gray AW, Jayaprakash A, Konda S, Brown DJ, Miller SR, Eizadkhah R, Milletti MC. Int. J. Pept. Res.Therap. 2010;16:43–54. [Google Scholar]
- 36.Bokvist M, Lindstrom F, Watts A, Grobner G. J. Mol. Biol. 2004;335:1039–1049. doi: 10.1016/j.jmb.2003.11.046. [DOI] [PubMed] [Google Scholar]
- 37.McHenry AJ, Sciacca MFM, Brender JR, Ramamoorthy A. Biochim. Biophys. Acta. 2012;1818:3019–3024. doi: 10.1016/j.bbamem.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Knight JD, Hebda JA, Miranker AD. Biochemistry. 2006;45:9496–9508. doi: 10.1021/bi060579z. [DOI] [PubMed] [Google Scholar]
- 39.Magzoub M, Miranker AD. FASEB J. 2012;26:1228–1238. doi: 10.1096/fj.11-194613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cheng PN, Liu C, Zhao ML, Eisenberg D, Nowick JS. Nat. Chem. 2012;4:927–933. doi: 10.1038/nchem.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nanga RPR, Brender JR, Xu JD, Veglia G, Ramamoorthy A. Biochemistry. 2008;47:12689–12697. doi: 10.1021/bi8014357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Westermark P, Engstrom U, Johnson KH, Westermark GT, Betsholtz C. Proc. Natl. Acad. Sci. U. S. A. 1990;87:5036–5040. doi: 10.1073/pnas.87.13.5036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mascioni A, Porcelli F, Ilangovan U, Ramamoorthy A, Veglia G. Biopolymers. 2003;69:29–41. doi: 10.1002/bip.10305. [DOI] [PubMed] [Google Scholar]
- 44.Koo BW, Hebda JA, Miranker AD. Protein Eng. Des. Sel. 2008;21:147–154. doi: 10.1093/protein/gzm076. [DOI] [PubMed] [Google Scholar]
- 45.Tenidis K, Waldner M, Bernhagen J, Fischle W, Bergmann M, Weber M, Merkle ML, Voelter W, Brunner H, Kapurniotu A. J. Mol. Biol. 2000;295:1055–1071. doi: 10.1006/jmbi.1999.3422. [DOI] [PubMed] [Google Scholar]
- 46.Ruschak AM, Miranker AD. Proc. Natl. Acad. Sci. U. S. A. 2007;104:12341–12346. doi: 10.1073/pnas.0703306104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Henzler-Wildman KA, Martinez GV, Brown MF, Ramamoorthy A. Biochemistry. 2004;43:8459–8469. doi: 10.1021/bi036284s. [DOI] [PubMed] [Google Scholar]