Abstract
Background
Abdominal abscesses are a common complication in Crohn’s disease (CD). Percutaneous drainage of such abscesses has become increasingly popular and may deliver outcomes comparable to surgical treatment; however, such comparative data are limited from single center studies. There have been no nationally representative studies comparing different treatment modalities for abdominal abscesses.
Methods
We identified all adult CD-related non-elective hospitalizations from the Nationwide Inpatient Sample 2007 that were complicated by an intra-abdominal abscess. Treatment modality was categorized into 3 strata – medical treatment alone, percutaneous drainage, and surgery. We analyzed the nationwide patterns in the treatment and outcomes of each treatment modality and examined for patient demographic, disease, or hospital-related disparities in treatment and outcome.
Results
There were an estimated 3,296 hospitalizations for abdominal abscesses in patients with CD. Approximately 39% were treated by medical treatment alone, 29% with percutaneous drainage, and 32% with surgery with a significant increase in the use of percutaneous drainage since 1998 (7%). Co-morbidity burden, admission to a teaching hospital, and complicated Crohn’s disease (fistulae, stricture) were associated with non-medical treatment. Use of percutaneous drainage was more common in teaching hospitals. Mean time to percutaneous drainage and surgical treatment were 4.6 and 3.3 days respectively and early intervention was associated with significantly shorter hospitalization.
Conclusions
We describe the nationwide pattern in the treatment of abdominal abscesses and demonstrate an increase in the use of percutaneous drainage for the treatment of this subgroup. Early treatment intervention was predictive of shorter hospitalization.
Keywords: Crohn’s disease, percutaneous drainage, abdominal abscess, surgery, bowel resection
BACKGROUND
Crohn’s disease (CD) is a chronic intestinal inflammatory disease that is characterized by involvement of the small intestine in over three-fourths of patients. Such involvement is often transmural, increasing the likelihood of developing penetrating complications1. One such complication associated with considerable morbidity is the development of intra-abdominal abscesses1. Previously, the treatment of such abscesses was surgical drainage, often with the need for bowel resection and/or creation of a temporary or permanent stoma1–3. However, increasingly, percutaneous drainage of such abscesses is gaining popularity and is associated with delay in surgery, and in many cases, avoidance of surgery over a long-term follow up3–9.
Retrospective series have demonstrated the treatment success with such percutaneous drainage, either in isolation, or using surgical treatment as a comparison group. Disease, demographic, and institutional factors appear to predict which treatment modality is preferred. However, such literature arises from single-center referral studies which are susceptible to biases relating to both disease severity and physician treatment practices5, 7–9. To our knowledge, there are no published large nationwide multi-center studies examining treatment patterns and outcomes of intra-abdominal abscesses in patients with CD.
We performed this study using a nationally representative hospitalization sample to (1) examine temporal trends in the treatment of abdominal abscesses in CD; (2) identify individual patient, regional, as well as hospital characteristics that may predict the specific treatment modality; and (3) examine the effect of procedure type on length of stay and hospitalization costs.
METHODS
Data Source
The primary source of data for our study was the Nationwide Inpatient Sample (2007), which is the largest all-payer hospitalization database in the United States10. The database comprises all hospitalizations from a stratified random sample of over 1,000 hospitals across 44 states. Each hospitalization is coded with one primary diagnosis responsible for the hospitalization and up to fourteen secondary diagnoses. In addition, there is information on up to fifteen procedures associated with the hospitalization with all diagnoses and procedures coded using the International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM) codes. Our study population comprised all adult (19 years and older) CD (ICD-9-CM 555.x) hospitalizations with an associated code for intra-abdominal abscess (ICD-9-CM 540.1, 567.22, 569.5). Hospitalizations that were coded as being ‘elective’ were excluded. Information was obtained from the NIS on age, gender, race, income for ZIP code of residence, and primary insurance source for the hospitalization. Co-morbidity was assessed using the Elixhauser co-morbidity index, a widely used and validated measure of co-morbidity in hospitalized patients using administrative data11. The co-morbidity burden was stratified based on the presence of 0, 1, 2, and 3 or more co-morbid conditions. Hospital characteristics were also obtained from the NIS and included hospital teaching status, bed-size, and region (Northeast, South, West, and Midwest). Complicated Crohn’s disease was defined as the presence of enteric fistulae (ICD-9-CM 569.81) or intestinal strictures (ICD-9-CM 560.9).
Variables
Our main variable of interest was the modality used for the treatment of the abscess. Percutaneous drainage was defined using the administrative code for “percutaneous abdominal drainage” (ICD-9-CM 54.91). We excluded a small proportion of patients with co-existing liver disease or ascites, as the same code in such patients may be used for abdominal paracentesis. Surgical treatment was defined as undergoing bowel resection or exploratory laparotomy. To exclude patients who may have undergone surgery for an unrelated reason and subsequently developed an intra-abdominal abscesses as a post-operative complication, we performed a sensitivity analysis where we excluded such patients with concomitant codes for post-operative infection (ICD-9-CM 998.5x). Time to percutaneous drainage and time to surgical treatment were ascertained using the ‘time to procedure’ information available in the NIS. Our primary outcomes of interest were time to intervention (percutaneous drainage or surgery), length of hospitalization, hospitalization charges and need for a temporary or permanent stoma in patients undergoing surgical treatment.
Statistical Analysis
All data was analyzed using Stata 11.1 (StataCorp, College Station, TX) using the appropriate svy commands and survey weights provided to account for the stratified sample design of the NIS. Continuous variables were summarized using means and standard deviations while categorical variables were expressed as proportions. Univariate and multivariate logistic regression models were constructed to identify independent predictors of each individual treatment modality, ‘operative intervention’ (defined as undergoing either percutaneous or surgical drainage), and undergoing percutaneous drainage compared to surgical treatment. Similar models were constructed to examine the effect of treatment modality on in-hospital mortality and need for TPN while linear regression models were used to estimate their effect on length of stay and hospitalization charges. All variables were selected for inclusion in the multivariate model based on attainment of statistical significance in the univariate analysis at p-values < 0.05.
As allocation to treatment group is non-random and there is significant likelihood of confounding by indication with allocation of sicker patients to surgical intervention, we created a propensity score predicting likelihood of receiving surgical treatment (vs. non-surgical treatment). Variables used to create this propensity score included patient characteristics (age, co-morbidity, gender, zip code level income, insurance status), disease characteristics (disease behavior, anemia, malnutrition, severity of disease by DRG), and hospital characteristics (bed-size, region, teaching status). We then adjusted for this propensity in our final model. The study was approved by the Partners Healthcare Institutional Review Board.
RESULTS AND DISCUSSION
Study Population
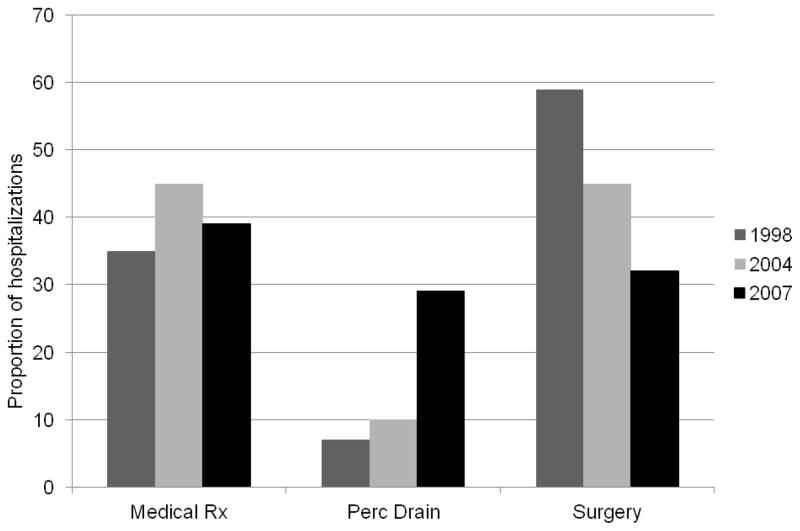
There were an estimated 3,296 hospitalizations with intra-abdominal abscesses in CD patients in 2007 (2.7% of all CD hospitalizations). The mean age was 41.3 years. Just over half the patients were men (55%) and a similar proportion were of Caucasian race (58%). One-third of patients was treated with medical treatment alone and did not undergo percutaneous drainage or surgery (38%). Approximately 29% were treated with percutaneous drainage and 32% were treated surgically with laparotomy and/or bowel resection. In 1998, a similar proportion of patients were treated medically (34%) while only 7% were treated with percutaneous drainage and 59% underwent surgery. At the mid-point of our study period, in 2004, the proportion of patients undergoing percutaneous drainage further increased to 10% while those undergoing surgery decreased to 44% suggesting that there has been a significant trend towards reduced use of surgery and increased use of percutaneous drainage nationally over the past decade (Figure 1).
Figure 1.
Distribution of treatment practices in Crohn’s disease patients with intra-abdominal abscess
Predictors of Treatment Modality
Table 1 presents the differences in characteristics of patients by treatment type. Non-medical treatment was more common in teaching hospitals, primarily due to a significantly greater proportion undergoing percutaneous drainage (35% vs. 22%, p=0.0009). On multivariate analysis, the independent predictors of undergoing non-medical treatment were presence of Elixhauser co-morbidity index of 3 or higher (odds ratio (OR) 1.72, 95% CI 1.07 – 2.93)), admission to a teaching hospital (OR 2.02, 95% CI 1.36 – 2.98), region of hospital location in the South (OR 1.71, 95% CI 1.06 – 2.75) or West (OR 2.38, 95% CI 1.22 – 4.61) compared to the North-east, and the presence of complicated CD (OR 1.75, 95% CI 1.16 – 2.66). Age, gender, race, insurance status, or income did not predict likelihood of non-interventional treatment. Among the subgroup of patients undergoing interventional treatment, the presence of complicated CD increased likelihood of surgical treatment (OR 1.54, 95% CI 1.00 – 2.38) while admission to a teaching hospital increased likelihood of percutaneous drainage with a reduced odds ratio for undergoing surgery (OR 0.59, 95% CI 0.36 – 0.97).
Table 1.
Characteristics of patients, by modality of treatment of intra-abdominal abscess
| Medical Treatment (n=1,273) | Percutaneous Drainage (n=962) | Surgical Treatment (n=1,060) | |
|---|---|---|---|
| Age | |||
| 19–35 years | 39.8 | 28.4 | 31.8 |
| 35–50 years | 33.2 | 32.5 | 34.3 |
| ≥ 51 years | 41.3 | 28.1 | 30.6 |
| Female | 39.7 | 29.8 | 30.5 |
| Non-white race | 37.7 | 30.6 | 31.7 |
| Elixhauser co-morbidity | |||
| 0 | 42.9 | 28.9 | 28.2 |
| 1 | 37.9 | 28.6 | 33.6 |
| 2 | 40.4 | 26.9 | 32.7 |
| ≥ 3 | 30.1 | 32.9 | 37.0 |
| Insurance | |||
| Private | 39.3 | 27.5 | 33.2 |
| Medicare | 38.5 | 30.7 | 30.8 |
| Medicaid | 34.2 | 38.6 | 27.2 |
| Self-pay | 40.5 | 25.3 | 34.2 |
| Complicated disease* | 18.1 | 25.3 | 32.3 |
| Current smoking | 45.4 | 28.4 | 26.2 |
| Steroid use | 45.1 | 27.6 | 27.3 |
| Emergent admission | 41.2 | 28.3 | 30.5 |
| Hospital teaching status | |||
| No | 46.2 | 21.7 | 32.1 |
| Yes | 33.0 | 34.8 | 32.2 |
Complicated disease comprised those with internal fistulae or intestinal strictures
Percutaneous drainage – Time to drainage and Outcomes
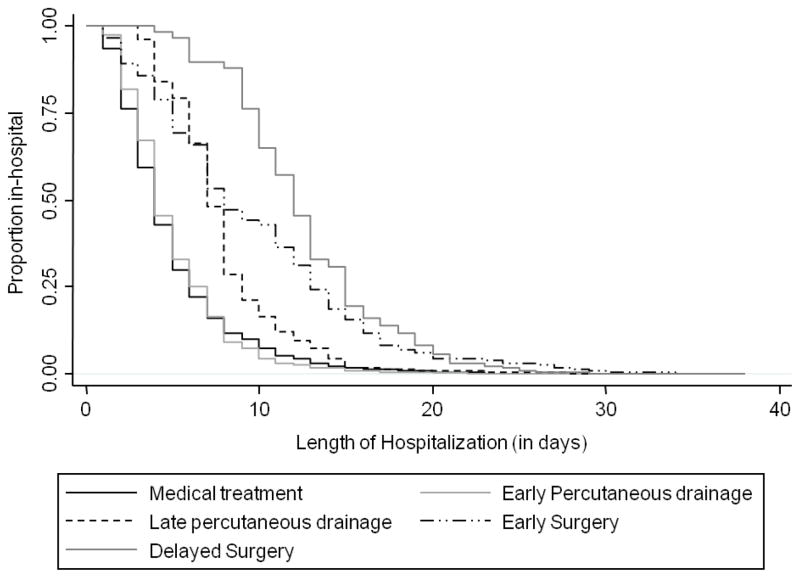
The mean time to percutaneous drainage procedure was 4.6 days. We examined predictors of time to drainage among this subgroup of patients. Approximately half the patients (51.4%) treated percutaneously underwent the drainage procedure within 2 days. The mean length of hospital stay in such patients was significantly reduced compared to those who went delayed drainage procedure (Figure 2) (6.5 days vs. 16.5 days) (p < 0.0001). Greater co-morbidity significantly lengthened time to percutaneous drainage (+5.8 days, 95% CI 3.1 to 8.6 days) while the presence of ongoing steroid use resulted in earlier drainage (−0.8 days, 95% CI −7.3 to −0.4 days). None of the hospital characteristics predicted time to undergoing drainage procedure. On multivariate analysis, early drainage was also associated with significantly lower hospitalization charges (−$ 46,133).
Figure 2.
Length of stay in Crohn’s disease patients with intra-abdominal abscess, by treatment type
Surgical Treatment – Time to surgery and Outcomes
The mean time to surgery was 3.3 days for those undergoing surgical treatment of the abdominal abscess. Nonwhite patients had a trend towards longer mean time to surgery (1.6 days, 95% CI −0.1 to 3.4 days) as did those with an Elixhauser co-morbidity score of 2 (+1.7 days) or ≥ 3 (3.1 days). Age, income, insurance status, hospital characteristics, or presence of complicated Crohn’s disease did not influence time to surgery in these patients. Similar to what we observed in the percutaneous treatment arm, early time to surgery was associated with significantly shorter hospitalization length (Figure 2) (p < 0.0001) and a $38,032 savings in healthcare charges.
Approximately one-quarter of the patients undergoing surgery required a stoma (25.3%). However, there were no demographic or clinical variables that predicted requirement for a stoma. Specifically, presence of enteric fistulae (OR 1.39, 95% CI 0.58 – 3.33) or strictures (OR 0.54, 95% CI 0.18 – 1.65) were not associated with requirement for a stoma. Surgical patients who required a stoma had a 4 day longer hospitalization (95% CI 1.1 – 7.5 days) adjusting for age, co-morbidity and other confounding variables.
DISCUSSION
Intra-abdominal abscesses are common in Crohn’s disease and classically required surgical treatment with resection of the involved segment and potential need for temporary or permanent stoma. Recent studies have shown that it is possible to percutaneously drain such abscesses and achieve similar outcomes3, 5, 7–9, 12, 13. However, such data are from single center studies. Using a large nationally representative sample, we describe that (1) there a significant increasing trend towards use of percutaneous aspiration or drainage in the treatment of intra-abdominal abscesses in CD; (2) admission to a teaching hospital increased likelihood of percutaneous drainage while the presence of complicated CD (fistulae or strictures) increased likelihood of surgery; and (3) early drainage (percutaneous or surgery) was associated with significantly shorter hospitalization stays and healthcare costs.
Feagins et al. recently reviewed the efficacy of percutaneous drainage of intra-abdominal abscesses3 and several retrospective studies examined the success rate of percutaneous abscess drainage with the number of patients in each study varying from 10 to 954, 6–9, 12–16. The majority of the abscesses were spontaneous. The definition of success varied between the studies with some authors allowing for delayed elective surgery as a treatment success while others had more restrictive definitions of treatment success. Long-term surgery could be avoided in 14–85% of patients over 2–5 years of follow-up3. While we did not have the ability to examine long-term outcomes in our study, our findings support that percutaneous drainage is an increasingly common modality of treatment of intra-abdominal abscesses in a large representative nationwide sample not restricted to specialty hospitals. Consistent with the findings of Nguyen et al.9, we also found that abscesses that could be treated with percutaneous drainage were associated with shorter hospitalizations and lower treatment costs.
Gutierrez et al. in a prior study from Massachusetts General Hospital examined predictors of each treatment modality8. In their study, age, absence of fistula, longer duration of symptoms, immunomodulator use and admission to the medical service predicted percutaneous drainage versus surgery. Similar to their single center experience, we found that the presence of complicated CD increased the likelihood of undergoing surgical intervention (compared to percutaneous drainage) and that ongoing steroid use was associated with treatment using percutaneous drainage.
Several prior studies have demonstrated disparities in the receipt of treatment modalities in IBD patients based on race, income, and hospital characteristics raising significant concerns about heterogeneity in the delivery of IBD care17–20. Indeed, such hospital-related disparities appeared to be of greater significance in those with the greatest severity of disease such as those requiring surgery19, 20. In this study of abdominal abscesses, a serious complication of CD, we did demonstrate that hospital teaching status was predictive of receiving percutaneous drainage suggesting that practice variations exist in the treatment of this complication as well. However, reassuringly, there were no significant differences in short-term outcomes including length of stay, need for parenteral nutrition, need for temporary or permanent ileostomy by gender, race, income, or hospital type. We also found that early treatment (either percutaneous or surgical) was associated with a shorter hospitalization stay and lower costs suggesting the importance of early intervention in such patients. This is consistent with other literature on interventional or surgical treatment in the management of IBD where a delayed intervention was associated with poorer outcomes20. Increasing physician education and awareness about the availability and efficacy of operative and non-operative treatment of these complications may help improve short- and long-term outcomes in the management of complicated CD.
Several limitations of our study merit acknowledgment. We did not have longitudinal follow-up of patient outcomes and also lacked information on specific abscess characteristics including size and location. We attempted to adjust for disease severity as much as possible by examining billing codes for complicated Crohn’s disease (stricture, enteric fistulae) as well as for other markers such as malnutrition and need for TPN. Nevertheless, we believe that the use of a nationwide representative sample to examine treatment practices is a key strength of our study by overcoming potential of bias from single referral center studies. The design of the NIS also does not allow the tracking of re-admissions due to lack of longitudinal linkage. We also relied on administrative coding for the ascertainment of our case population, treatment modalities and outcomes. This is susceptible to errors; however, such errors are likely to be non-differential and unlikely to affect the direction of our estimates.
CONCLUSIONS
In conclusion, using a large representative sample, we demonstrate that percutaneous drainage and surgical drainage are used to treat approximately one-third each of patients with CD who are hospitalized with intra-abdominal abscess with the proportion of such hospitalizations being treated with percutaneous aspiration demonstrating a steep increase over the past decade. As most data on the comparative effectiveness of various modalities in the management of CD have come from single tertiary centers, there is continued need for multicenter co-operative cohorts across different institutional characteristics to confirm the generalizability of the results and inform treatment practices in the management of complicated CD.
Acknowledgments
This work was presented in part at the Digestive Disease Week 2012, San Diego, CA.
Source of funding: Ananthakrishnan is supported in part by a grant from the American Gastroenterological Association
Abbreviations
- CD
Crohn’s disease
Footnotes
Conflicts of interest: None
Competing interests:
There are no competing interests.
Authors’ information
ANA - study concept and design, analysis and interpretation, drafting of the manuscript; ELM – obtained data for analysis, critical revision and approval of final manuscript.
References
- 1.Greenstein AJ, Sachar DB, Greenstein RJ, Janowitz HD, Aufses AH., Jr Intraabdominal abscess in Crohn’s (ileo) colitis. Am J Surg. 1982;143:727–30. doi: 10.1016/0002-9610(82)90046-0. [DOI] [PubMed] [Google Scholar]
- 2.Cellini C, Safar B, Fleshman J. Surgical management of pyogenic complications of Crohn’s disease. Inflamm Bowel Dis. 16:512–7. doi: 10.1002/ibd.20984. [DOI] [PubMed] [Google Scholar]
- 3.Feagins LA, Holubar SD, Kane SV, Spechler SJ. Current strategies in the management of intra-abdominal abscesses in Crohn’s disease. Clin Gastroenterol Hepatol. 9:842–50. doi: 10.1016/j.cgh.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 4.Gervais DA, Hahn PF, O’Neill MJ, Mueller PR. Percutaneous abscess drainage in Crohn disease: technical success and short- and long-term outcomes during 14 years. Radiology. 2002;222:645–51. doi: 10.1148/radiol.2223010554. [DOI] [PubMed] [Google Scholar]
- 5.Jawhari A, Kamm MA, Ong C, Forbes A, Bartram CI, Hawley PR. Intra-abdominal and pelvic abscess in Crohn’s disease: results of noninvasive and surgical management. Br J Surg. 1998;85:367–71. doi: 10.1046/j.1365-2168.1998.00575.x. [DOI] [PubMed] [Google Scholar]
- 6.Lambiase RE, Cronan JJ, Dorfman GS, Paolella LP, Haas RA. Percutaneous drainage of abscesses in patients with Crohn disease. AJR Am J Roentgenol. 1988;150:1043–5. doi: 10.2214/ajr.150.5.1043. [DOI] [PubMed] [Google Scholar]
- 7.Xie Y, Zhu W, Li N, Li J. The outcome of initial percutaneous drainage versus surgical drainage for intra-abdominal abscesses in Crohn’s disease. Int J Colorectal Dis. doi: 10.1007/s00384-011-1338-x. [DOI] [PubMed] [Google Scholar]
- 8.Gutierrez A, Lee H, Sands BE. Outcome of surgical versus percutaneous drainage of abdominal and pelvic abscesses in Crohn’s disease. Am J Gastroenterol. 2006;101:2283–9. doi: 10.1111/j.1572-0241.2006.00757.x. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen DL, Sandborn WJ, Loftus EV, Jr, Larson DW, Fletcher JG, Becker B, Mandrekar J, Harmsen WS, Bruining DH. Similar outcomes of surgical and medical treatment of intra-abdominal abscesses in patients with Crohn’s disease. Clin Gastroenterol Hepatol. 10:400–4. doi: 10.1016/j.cgh.2011.11.023. [DOI] [PubMed] [Google Scholar]
- 10.Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract. 2002;5:143–51. [PubMed] [Google Scholar]
- 11.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Safrit HD, Mauro MA, Jaques PF. Percutaneous abscess drainage in Crohn’s disease. AJR Am J Roentgenol. 1987;148:859–62. doi: 10.2214/ajr.148.5.859. [DOI] [PubMed] [Google Scholar]
- 13.Sahai A, Belair M, Gianfelice D, Cote S, Gratton J, Lahaie R. Percutaneous drainage of intra-abdominal abscesses in Crohn’s disease: short and long-term outcome. Am J Gastroenterol. 1997;92:275–8. [PubMed] [Google Scholar]
- 14.da Luz Moreira A, Stocchi L, Tan E, Tekkis PP, Fazio VW. Outcomes of Crohn’s disease presenting with abdominopelvic abscess. Dis Colon Rectum. 2009;52:906–12. doi: 10.1007/DCR.0b013e31819f27c3. [DOI] [PubMed] [Google Scholar]
- 15.Golfieri R, Cappelli A, Giampalma E, Rizzello F, Gionchetti P, Laureti S, Poggioli G, Campieri M. CT-guided percutaneous pelvic abscess drainage in Crohn’s disease. Tech Coloproctol. 2006;10:99–105. doi: 10.1007/s10151-006-0260-7. [DOI] [PubMed] [Google Scholar]
- 16.Rypens F, Dubois J, Garel L, Deslandres C, Saint-Vil D. Percutaneous drainage of abdominal abscesses in pediatric Crohn’s disease. AJR Am J Roentgenol. 2007;188:579–85. doi: 10.2214/AJR.06.0181. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen GC, Laveist TA, Gearhart S, Bayless TM, Brant SR. Racial and geographic variations in colectomy rates among hospitalized ulcerative colitis patients. Clin Gastroenterol Hepatol. 2006;4:1507–1513. doi: 10.1016/j.cgh.2006.09.026. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen GC, Munsell M, Brant SR, LaVeist TA. Racial and geographic disparities in the use of parenteral nutrition among inflammatory bowel disease inpatients diagnosed with malnutrition in the United States. JPEN J Parenter Enteral Nutr. 2009;33:563–8. doi: 10.1177/0148607109332907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ananthakrishnan AN, McGinley EL, Binion DG. Does it matter where you are hospitalized for inflammatory bowel disease? A nationwide analysis of hospital volume. Am J Gastroenterol. 2008;103:2789–98. doi: 10.1111/j.1572-0241.2008.02054.x. [DOI] [PubMed] [Google Scholar]
- 20.Kaplan GG, McCarthy EP, Ayanian JZ, Korzenik J, Hodin R, Sands BE. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology. 2008;134:680–7. doi: 10.1053/j.gastro.2008.01.004. [DOI] [PubMed] [Google Scholar]