ABSTRACT
INTRODUCTION
The U.S. faces a critical gap between residency training and clinical practice that affects the recruitment and preparation of internal medicine residents for primary care careers. The patient-centered medical home (PCMH) represents a new clinical microsystem that is being widely promoted and implemented to improve access, quality, and sustainability in primary care practice.
AIM
We address two key questions regarding the training of internal medicine residents for practice in PCMHs. First, what are the educational implications of practice transformations to primary care home models? Second, what must we do differently to prepare internal medicine residents for their futures in PCMHs?
PROGRAM DESCRIPTION
The 2011 Society of General Internal Medicine (SGIM) PCMH Education Summit established seven work groups to address the following topics: resident workplace competencies, teamwork, continuity of care, assessment, faculty development, ‘medical home builder’ tools, and policy. The output from the competency work group was foundational for the work of other groups. The work group considered several educational frameworks, including developmental milestones, competencies, and entrustable professional activities (EPAs).
RESULTS
The competency work group defined 25 internal medicine resident PCMH EPAs. The 2011 National Committee for Quality Assurance (NCQA) PCMH standards served as an organizing framework for EPAs.
DISCUSSION
The list of PCMH EPAs has the potential to begin to transform the education of internal medicine residents for practice and leadership in the PCMH. It will guide curriculum development, learner assessment, and clinical practice redesign for academic health centers.
KEY WORDS: patient-centered medical home, entrustable professional activities, graduate medical education, internal medicine, primary care
INTRODUCTION
The United States faces a significant primary care workforce shortage.1 By 2025, primary care physicians will see their workload increase by an estimated 29 % at the same time the workforce is projected to expand by only 2–7 %.1 This deficit represents a shortage of approximately 40,000 adult primary care physicians.1 Many factors contribute to this crisis, including poorly functioning work environments and medical education systems that fail to prepare physicians for contemporary ambulatory care practice.2 As a result, recruitment into primary care remains a significant challenge.3 Today’s medical students report serious concerns about primary care as a career, and only 2 % plan to enter general internal medicine.4,5 In graduate medical education, residents often train in academic practices with limited resources and complex patient populations that stress the capacity of individual clinicians to meet patients’ needs. Negative experiences in these practices turn physicians-in-training away from primary care.6 In 2003, only 19 % of first year internal medicine residents and 27 % of third year residents planned to practice general medicine, resulting in a 37 % decline in the number of internal medicine residency graduates pursuing primary care between 1998 and 2005.1,7
To address the dysfunctional primary care work environment, the American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP), and American Osteopathic Association (AOA) identified seven joint principles of the patient-centered medical home (PCMH): 1) Personal physician, 2) Physician-directed medical practice, 3) Whole person orientation, 4) Coordinated and integrated care, 5) Quality and safety, 6) Enhanced access, and 7) Payment alignment.8 The PCMH represents a new clinical microsystem that is widely promoted and implemented to improve access, quality, and enhance sustainability and attractiveness to clinicians.9 In 2009, there were 94 PCMH demonstration projects involving 14,000 physicians and 5 million patients; 26 projects in 18 states included payment reform.10 While large-scale patient outcomes remain unchanged, some have demonstrated improved specific chronic condition patient outcomes, decreased provider burn-out, and increased patient satisfaction.11–14
Redesigning the primary care work environment has widened the gap between typical residency ambulatory training and the knowledge, skills, and attitudes essential for work in a PCMH. While the PCMH may make primary care a more attractive career choice by improving clinical, administrative, and financial support, residents will be unprepared to practice in this new setting unless our current training model is substantially changed.
The Society of General Internal Medicine (SGIM), Alliance for Academic Internal Medicine (AAIM), Association of Program Directors in Internal Medicine (APDIM), and others are calling for reform of the internal medicine residency ambulatory experience to include training in patient-centered team-based clinical systems like PCMH’s.15–20 Early residency education redesign initiatives, including the Academic Chronic Care Collaborative,21,22 Health Resources and Services Administration (HRSA) efforts,23 and Veterans Affairs Centers of Excellence in Primary Care Education, are significant investments.24 However, most residents still train in poorly organized practices, with few, if any, PCMH elements.20,25 Thus, they continue to face a mismatch between today’s clinical education and tomorrow’s health care practices.
In 2011, the Josiah Macy Jr. Foundation and others (see acknowledgements) sponsored a SGIM Education Summit to address two questions. First, what are the educational implications of current practice transformations to primary care home models? Second, what must we do differently to prepare internal medicine residents for their futures practicing in and leading PCMHs? The Summit begins to build a framework for the education of internal medicine residents in PCMHs. In this paper, we describe methods used to convene the Summit and results of its deliberations; in particular, those of the competency work group.
METHODS
Designing the Summit
Leaders from national internal medicine organizations served as advisory board members in designing the Summit. Seven work groups were established: 1) Workplace competencies for residents, 2) Teamwork, 3) Continuity of care, 4) Assessment, 5) Faculty development, 6) The Medical Home Builder© tools, and 7) Policy.26 Although the majority of work group members were general internal medicine physicians, membership also included university and community-based educators and leaders in medicine (internal medicine and family medicine), nursing, and pharmacy. External advisors from the Bureau of Health Professions/Health Resources and Services Administration (HRSA), the Macy Foundation, the National Initiative for Children’s Healthcare Quality, the Robert Wood Johnson Foundation, and the Veterans Health Administration Office of Academic Affiliations participated in the Summit. Although each work group had its own charge, the output from the competency work group was foundational for the work of all other groups. This paper details the methods and outcomes of the competency work group.
Preparing for the Summit
The competency work group was charged with defining realistic and tangible activities that residents would need to perform competently to practice in a PCMH setting. The seven members of the competency work group, representing internal medicine and family medicine residency program directors, educators, clinicians, and health services researchers, worked together for five months prior to the Summit through weekly email communication, monthly conference calls, and document-sharing via DropBox®. Preparation included a review of published literature from 1990 to the present, using the search terms “patient-centered medical home, ambulatory education in graduate medical education, interprofessional education and practice, and competency-based education.”
The group considered several frameworks to classify residents’ ability to function in a PCMH, including the U.S. Accreditation Council for Graduate Medical Education (ACGME)27 and the Canadian Royal College of Physicians and Surgeons (CanMEDS) competencies,28 developmental milestones,30 and entrustable professional activities (EPAs).29–31 Formulated by ten Cate in 2005, EPAs represent the key professional activities for a particular discipline.32 We chose EPAs as a framework for three reasons. First, EPAs have emerged as an important framework for competency-based medical education in Europe and the U.S.31,33,34 Second, EPAs operationalize competencies and the complexity of clinical competence. Performing an EPA requires integration of multiple competencies, which, in turn, require activation of multiple skills, knowledge, and attitudes. On the contrary, a trainee’s demonstration of multiple individual competencies may not translate into integrated actions and activities required for clinical practice.32,35 Third, EPAs exemplify tangible clinical activities that front-line clinical supervisors observe on a daily basis. They are more intuitive for learner assessment than competencies. EPAs may be especially useful for education in the PCMH, where coordinated comprehensive care over time is better characterized by broad clinical activities than by individual competencies.
The relationship between milestones, competencies, and EPAs is a complex one. A trainee must demonstrate a certain level of proficiency in multiple competencies (or sub-competencies) to successfully perform an EPA. The level of proficiency in a competency can be determined via milestones, which track a developmental progression of observable behaviors. For example, “performing a comprehensive medication review and reconciliation using an electronic health record that allows electronic prescribing” is an EPA. This EPA incorporates multiple competencies, such as patient care (including the “history taking” sub-competency), medical knowledge, and systems-based practice. A trainee’s proficiency in history taking can be tracked within a sequence of three developmental milestones, progressing from, 1) “Acquire accurate and relevant history from the patient . . .” to 2) “Seek and obtain appropriate, verified, and prioritized data from secondary sources (e.g. family, records, pharmacy)” to 3) “Obtain relevant historical subtleties that inform and prioritize both differential diagnoses and diagnostic plans….”30 This framework can be used to determine the “rate limiting deficiency” if a trainee fails to successfully perform an EPA. Table 1 demonstrates how EPAs encompass and integrate the competencies included in ACGME and other frameworks.
Table 1.
A Sample Entrustable Professional Activity (EPA) and Related Competencies
| Sample PCMH EPA: | ||||
|---|---|---|---|---|
| Facilitate a patient’s participation in a health care decision using informed decision-making (or using formal decision-aid) | ||||
| Clinical Example: | ||||
| Shared decision-making for stroke prevention in a patient with atrial fibrillation and relative low stroke risk | ||||
| Specific behavioral elements of sample EPA | Solicit history, perform physical exam, and order/ interpret laboratory tests for cardiovascular disease | Know the risk of stroke in atrial fibrillation | Identify relevant clinical questions | Work with health educators and other team members in helping patient make decision about stroke prevention strategies |
| Educate patient/family about stroke prevention and outcomes | Know the effectiveness and risks of stroke prevention strategies | Acquire, appraise, and apply new information about primary stroke prevention in atrial fibrillation | Document patient assessment and decision-making process in medical record | |
| Solicit patient preferences for primary prevention of stroke | Know potential stroke outcomes | Solicit and respond to feedback about shared decision-making encounter with patient | Communicate risk for outcomes of stroke prevention options | |
| ACGME competencies27 | Patient care | Medical knowledge | Practice-based learning and improvement | Interpersonal/communication skills |
| Relevant ACGME sub-competencies | Residents must be able to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health | Residents must demonstrate knowledge of established and evolving biomedical, clinical, epidemiological and social-behavioral sciences, as well as the application of this knowledge to patient care | Identify strengths, deficiencies, and limits in one’s knowledge and expertise | Communicate effectively with patients, families, and the public, as appropriate, across a broad range of socioeconomic and cultural backgrounds |
| Identify and perform appropriate learning activities | Communicate effectively with physicians, other health professionals, and health related agencies | |||
| Incorporate formative evaluation feedback into daily practice | Work effectively as a member or leader of a health care team or other professional group | |||
| Locate, appraise, and assimilate evidence from scientific studies related to their patients’ health problems | Maintain comprehensive, timely, and legible medical records, if applicable | |||
| Use information technology to optimize learning | ||||
| Relevant joint principles for PCMH education competencies39 | Personal physician | Quality and safety | Physician directed medical practice | |
| Demonstrate knowledge about the definition of patient-centeredness the ability to provide patient centered care in their clinical encounters | Use point-of-care evidence-based clinical decision support and use information to make decisions within practice via interpretation of quality reports, patient and family engagement, self-assessment of one’s own performance, knowledge of the principles of community health assessment, and awareness of the need for patient and family advocacy skills | Demonstrate collaborative care via leadership skills that result in effective information exchange and teaming with patients, their patients’ families, and professional associates | ||
| Whole person orientation | ||||
| Provide patient care that is compassionate, coordinated, appropriate, and effective for the treatment of health problems and the promotion of health | ||||
| CanMEDS* | Medical expert | Scholar | Communicator | |
| Collaborator | ||||
PCMH = patient-centered medical home; ACGME = the U.S. Accreditation Council for Graduate Medical Education
*CanMEDS is a Royal College of Physicians and Surgeons of Canada initiative to define competencies needed in medical education and practice28
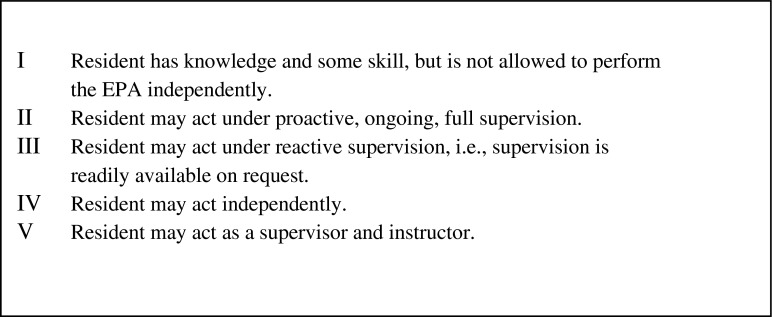
Entrustment refers to the granting to trainees the privilege to perform the professional activity, or EPA, without supervision within the context of a residency program (Text Box 1).36 An EPA can be distinguished from a competency by completing this sentence: “Tomorrow the resident will be entrusted to. . .”37
Text Box 1: Levels of Entrustment in Entrustable Professional Activities (EPAs)34
We limited our PCMH EPAs to those activities that specifically prepare internal medicine residency graduates to work in a PCMH environment, as opposed to those pertinent to the larger domain of ambulatory medicine. Each work group member began by identifying EPAs from daily clinical tasks within their practice and consulting with team members representing multiple disciplines. We used task analysis, practice profiling, and narrative writing to develop the initial set of PCMH EPAs. The group refined this list through review of published descriptions of PCMH.8–10 We then categorized these EPAs using the 2011 National Committee for Quality Assurance (NCQA) PCMH standards: 1) Enhance access and continuity, 2) Identify and manage patient populations, 3) Plan and manage care, 4) Provide self-care and community support, 5) Track and coordinate care, and 6) Measure and improve performance.38 We chose the NCQA standards to expand our thinking beyond traditional educational frameworks.
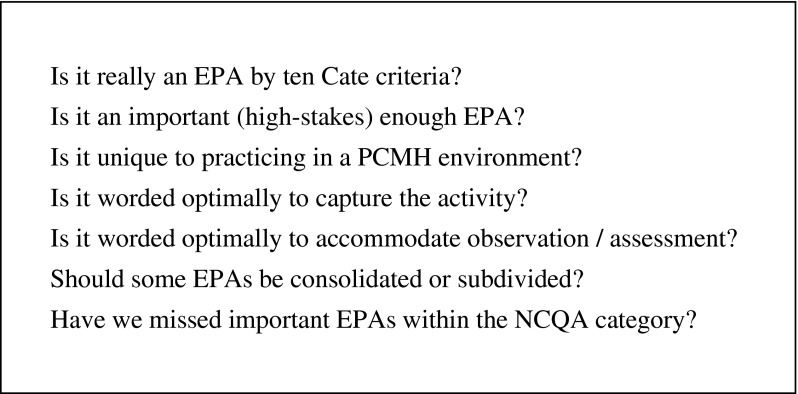
During the Summit
In March of 2011, the work groups gathered at the 2-day Summit for three face-to-face activities. First, each work group presented their pre-Summit work. Next, participants were redistributed into new small groups based on NCQA PCMH standards. Facilitated by a member of the competency work group, each new small group revised the EPAs in their NCQA category by applying brainstorming questions in Text Box 2. Finally, the resulting EPAs were circulated to the entire Summit, where everyone participated through a nonbinding multi-vote process to generate a list of high priority EPAs. By voting for top priority EPAs, all summit participants contributed to the list of EPAs determined to be most important. The competency work group collated these EPAs and Summit notes for subsequent review.
Text Box 2: Patient-Centered Medical Home (PCMH) Education Summit Brainstorming Questions
After the Summit
The competency work group revised EPAs based on input from the Summit. Work group members presented the EPAs in a PCMH symposium at the 2011 SGIM annual meeting, and revised the EPAs again based on audience feedback. Finally, each member solicited reviews from senior general medicine clinician, educator, and administrator colleagues.
RESULTS
The final list of 25 internal medicine resident PCMH EPAs is shown in Text Box 3. We classify each EPA as discrete (D) or longitudinal (L). Discrete EPAs occur within one care encounter, whereas longitudinal EPAs occur over a period of time. We use the NCQA PCMH standards (in bold below) to organize the EPAs and describe the standards in more detail here.
Text Box 3. Entrustable Professional Activities (EPAs) for Internal Medicine Residents in the Patient-Centered Medical Home*
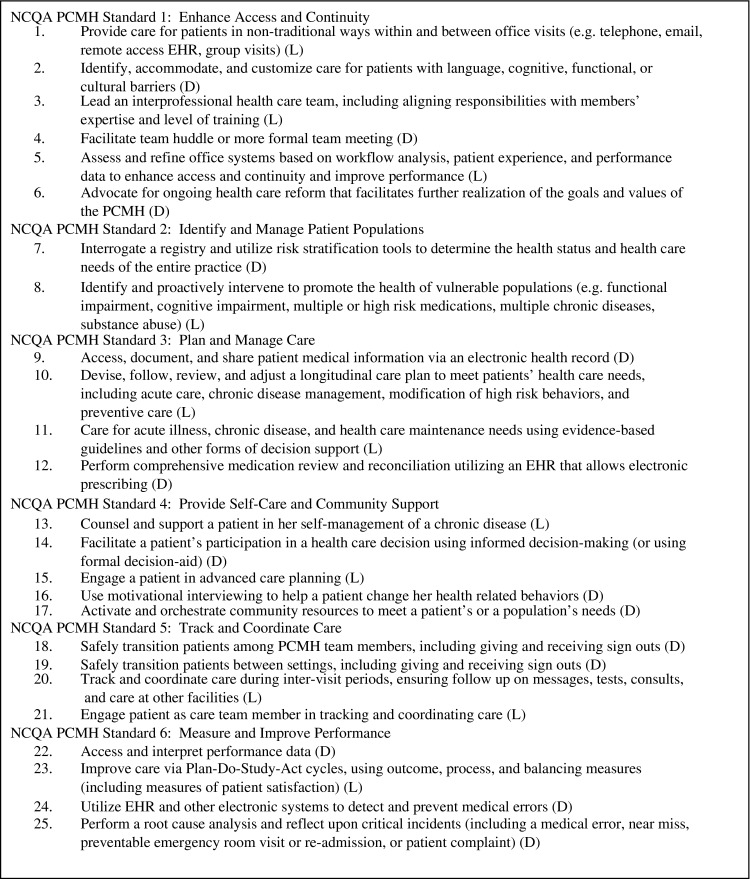
*Letters in parentheses after each EPA indicates classification into two types of EPAs:
(D) = Discrete EPAs
(L) = Longitudinal EPAs
Enhance Access and Continuity
EPAs in this NCQA PCMH standard prepare residents to deliver patient-centered care where access is enhanced by technology and teamwork. Technological advances allow us to engage patients as members of the team (e.g. patient portals in electronic health records), to reach patients efficiently (e.g. telemedicine), and to refine expectations for continuity. Continuity of care occurs between a coordinated health care team (e.g. physician, nurse, medical assistant, pharmacist, social worker), an activated patient, and her support network. Residents participate as members of the multidisciplinary team, using multiple modalities of communication to support effective face-to-face and asynchronous communication among team members.
Identify and Manage Populations
These EPAs emphasize the importance of population-based care. Implied here is the commitment of academic health centers to building the information infrastructure for identifying patients belonging to health care teams, promoting preventive health, optimizing care of chronic illnesses, and reporting population data to monitor the effectiveness of the health system to achieve quality goals.
Plan and Manage Care
These EPAs encompass fundamental primary care principles of longitudinal, continuous, comprehensive, evidence-based acute, chronic, and preventive care. The electronic health record (EHR) has an expanded role as a tool to facilitate patient care. Shared decision-making between patients and teams to achieve health care goals is a core concept. Although training is often divided into blocks of time, residents will take responsibility for engaging with health care team members to support patients in achieving their comprehensive health goals.
Provide Self-Care and Community Support
These EPAs address shortcomings of the traditional view of disease, which exclude the patient, family and community context. They require residents to frame patient encounters as partnerships, including dimensions like self-efficacy and health literacy. Effective understanding and activation of community resources to support patients is a necessity.
Track and Coordinate Care
These EPAs require conceptualizing the PCMH as a place where patients engage with the whole health care system, not just one ambulatory practice. Entrusting residents to manage transitions of care to optimize patient safety requires communication skills, knowledge of one’s health system, and the ability to discern best practices while coordinating care with multiple providers.
Measure and Improve Performance
These EPAs require a life-long commitment to continuously improve the performance of one’s own clinical practice and health care system to achieve better, safer, more equitable individual and system-level health outcomes. These require health information systems that report population data to monitor the system’s effectiveness in achieving quality goals. Residents will now connect preparation of a morbidity and mortality case conference, or work on a quality improvement project, to addressing larger systems issues.
DISCUSSION
With considerable momentum for system redesign, we sought to address today’s training-practice gap for internal medicine residents entering primary care. Using an interactive, iterative, and inclusive process, we articulated 25 internal medicine resident PCMH EPAs, which have the potential to close this gap.
Our work adds to prior scholarship in PCMH and medical education. First, we extended the work on joint PCMH principles for medical student education39 by articulating PCMH EPAs for internal medicine residency training. Second, we categorized EPAs by NCQA PCMH standards to create an innovative link between clinical system redesign and graduate medical education. Third, we articulated EPAs rather than competencies. EPAs integrate multiple competencies, avoiding the artificial distinction among individual competencies. They are suitable for workplace learning, because they allow evaluators to assess trainees in observable clinical tasks. The faculty member can directly observe the fully integrated professional activity, rather than trying to assess underlying competencies, which, as abstract abilities, can only be inferred. EPAs have been defined for residency training in obstetrics and gynecology, anesthesiology, and for neurology physician assistant training.35–37,40 Our work, then, extends EPA scholarship to internal medicine and the PCMH.
We make a novel distinction between discrete and longitudinal EPAs. Discrete EPAs, such as “facilitate a team huddle” or “perform a comprehensive medication reconciliation,” represent clinical activities that occur within a single episode of care. Faculty will make several observations and integrate multi-source feedback for each learner prior to making entrustment decisions. Supervisors can observe learners performing discrete EPAs during one continuous block of time, such as one patient visit, or one team meeting. These are similar, in time scale, to EPAs articulated in other specialties.35–37,40 Longitudinal EPAs, such as “track and coordinate care during inter-visit periods” or “supporting a patient in her self-management of a chronic illness,” describe care that unfolds over time. These EPAs require a longitudinal relationship between a resident and patient, or between a resident and the care team, or both. Learner assessment of longitudinal EPAs requires observation over time, across distinct clinical episodes.
While it would be ideal for internal medicine residents to train in fully realized PCMHs, most programs currently lack this infrastructure.20,25 Residency programs with fewer resources can still use this framework to take these steps in moving forward. First, program leaders may use these EPAs to guide curriculum needs assessment. Second, tools like the ACP Medical Home Builder© help program leaders determine their program’s strengths and areas for improvement.26 Third, acknowledging significant resource constraints in many clinical systems, pilot projects may target particular PCMH elements before large-scale systems change. Finally, program evaluation data can support advocacy efforts for institutional transformational change.
Identifying PCMH EPAs is one step in closing the training-practice gap. Curriculum revision, learner assessment, and faculty development must occur in parallel with clinical learning environment redesign. Our EPAs can frame curriculum reform for teaching practices in varying stages of PCMH redesign.36,37,41 We suggest Scheele’s criteria for prioritizing EPA implementation.41 In this schema, high-priority EPAs for implementation include those which 1) are critically important in daily practice, 2) address high-risk or error-prone activities, and 3) integrate multiple competencies. Once high-priority EPAs are selected, programs can address feasibility for implementation in the existing training environment, and fashion continuity clinics to maximize opportunities for residents to perform EPAs with supervision, feedback, and repetition. Additionally, authentic interprofessional team experiences will ideally become a part of the clinical learning experience.42,43 Finally, targeted supplemental curricula, using simulation techniques such as standardized patients, can fill gaps left by in-situ clinical training until full transformation to functional PCMH systems.
Although beyond the scope of this paper, faculty development around PCMH, competency-based education, and learner assessment in EPAs will be essential to ambulatory medicine training reform. We will need to refine assessment strategies for EPAs, learning the differences, if any, of assessing discrete vs. longitudinal EPAs. Simply having the framework of graded levels of entrustment, from performing the task under direct supervision to autonomous practice, is essential but not sufficient, given the variability among faculty evaluators.36,40 Lastly, the science on entrustment decisions is still immature, and further study is required before fully effective application of this assessment strategy.40
There are several limitations to our work. We did not perform a formal systematic review of the literature, or an exhaustive sampling of stakeholders. Thus, it is possible we missed important PCMH EPAs. Training environments vary widely. Some practices have already achieved NCQA ‘medical home certification,’ while others lack resources to make transformative changes. The EPAs described here may appear applicable to a limited number of residency programs. Our recommendations might be viewed as premature, assuming practice redesign is a necessary precondition for curricular reform. However, engaging residents during curricular reform and system redesign is a justifiable educational activity. Indeed, residents engaged in the process are likely better prepared for future change.
In conclusion, the national 2011 SGIM PCMH Education Summit generated 25 entrustable professional activities to guide the education of internal medicine residents for practice and leadership in the patient-centered medical home. These EPAs can serve to guide curriculum development, learner assessment, and clinical practice redesign in academic medical centers. We hope this work is an early step toward closing the training gap in internal medicine residency programs. It enhances training programs’ capacity to meet future workforce needs and produce physicians equipped to provide efficient, patient-centered care within a PCMH.
Acknowledgements
Contributors
We thank Karen Hauer, H. Carrie Chen, Patricia O’Sullivan, and C. Seth Landefeld for their thoughtful reviews of the manuscript.
Funders
Josiah Macy Jr. Foundation supported the Education Summit. Additional financial support for the Summit was provided by the United Health Foundation. The American College of Physicians, Primary Care Progress, and the Veterans Health Administration office of Academic Affiliations provided in-kind support.
Prior Presentations
The paper has not been presented. The list of EPAs from this Education Summit was presented at a workshop during the 2011 Annual Meeting of the Society of General Internal Medicine
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Colwill JM, Cultice JM, Kruse RL. Will generalist physician supply meet demands of an increasing and aging population? Heal Aff. 2008;27(3):w232–w241. doi: 10.1377/hlthaff.27.3.w232. [DOI] [PubMed] [Google Scholar]
- 2.Bodenheimer T. Primary care—will it survive? N Engl J Med. 2006;355(9):861–864. doi: 10.1056/NEJMp068155. [DOI] [PubMed] [Google Scholar]
- 3.Julian K, Riegels NS, Baron RB. Perspective: creating the next generation of general internists: a call for medical education reform. Acad Med. 2011;86(11):1443–7. [DOI] [PubMed]
- 4.Hauer KE, Durning SJ, Kernan WN, Fagan MJ, Mintz M, O’Sullivan PS, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA. 2008;300(10):1154–1164. doi: 10.1001/jama.300.10.1154. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz MD, Durning S, Linzer M, Hauer KE. Changes in medical students’ views of internal medicine careers from 1990 to 2007. Arch Intern Med. 2011;171(8):744–749. doi: 10.1001/archinternmed.2011.139. [DOI] [PubMed] [Google Scholar]
- 6.Keirns CC, Bosk CL. Perspective: the unintended consequences of training residents in dysfunctional outpatient settings. Acad Med. 2008;83(5):498–502. doi: 10.1097/ACM.0b013e31816be3ab. [DOI] [PubMed] [Google Scholar]
- 7.Garibaldi RA, Popkave C, Bylsma W. Career plans for trainees in internal medicine residency programs. Acad Med. 2005;80(5):507–512. doi: 10.1097/00001888-200505000-00021. [DOI] [PubMed] [Google Scholar]
- 8.American Academy of Family Physicians Joint principles of the patient-centered medical home. Del Med J. 2008;80(1):21–22. [PubMed] [Google Scholar]
- 9.Stange KC, Nutting PA, Miller WL, Jaen CR, Crabtree BF, Flocke SA, et al. Defining and measuring the patient-centered medical home. J Gen Intern Med. 2010;25(6):601–612. doi: 10.1007/s11606-010-1291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bitton A, Martin C, Landon BE. A nationwide survey of patient centered medical home demonstration projects. J Gen Intern Med. 2010;25(6):584–592. doi: 10.1007/s11606-010-1262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jaen CR, Ferrer RL, Miller WL, Palmer RF, Wood R, Davila M, et al. Patient outcomes at 26 months in the patient-centered medical home national demonstration project. Ann Fam Med. 2010;8 Suppl 1:S57,67; S92. [DOI] [PMC free article] [PubMed]
- 12.Maeng DD, Graf TR, Davis DE, Tomcavage J, Bloom FJ, Jr. Can a patient-centered medical home lead to better patient outcomes? The quality implications of geisinger’s ProvenHealth navigator. Am J Med Qual. 27(3):210–6. [DOI] [PubMed]
- 13.Nutting PA, Crabtree BF, Miller WL, Stange KC, Stewart E, Jaen C. Transforming physician practices to patient-centered medical homes: lessons from the national demonstration project. Health Aff (Millwood) 2011;30(3):439–445. doi: 10.1377/hlthaff.2010.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reid RJ, Coleman K, Johnson EA, Fishman PA, Hsu C, Soman MP, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29(5):835–843. doi: 10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]
- 15.Association of Program Directors in Internal Medicine. Fitzgibbons JP, Bordley DR, Berkowitz LR, Miller BW, Henderson MC. Redesigning residency education in internal medicine: a position paper from the association of program directors in internal medicine. Ann Intern Med. 2006;144(12):920–926. doi: 10.7326/0003-4819-144-12-200606200-00010. [DOI] [PubMed] [Google Scholar]
- 16.Bowen JL, Salerno SM, Chamberlain JK, Eckstrom E, Chen HL, Brandenburg S. Changing habits of practice. Transforming internal medicine residency education in ambulatory settings. J Gen Intern Med. 2005;20(12):1181–1187. doi: 10.1111/j.1525-1497.2005.0248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holmboe ES, Bowen JL, Green M, Gregg J, DiFrancesco L, Reynolds E, et al. Reforming internal medicine residency training. A report from the society of general internal medicine’s task force for residency reform. J Gen Intern Med. 2005;20(12):1165–1172. doi: 10.1111/j.1525-1497.2005.0249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huddle TS, Heudebert GR. Internal medicine training in the 21st century. Acad Med. 2008;83(10):910–915. doi: 10.1097/ACM.0b013e3181850a92. [DOI] [PubMed] [Google Scholar]
- 19.Meyers FJ, Weinberger SE, Fitzgibbons JP, Glassroth J, Duffy FD, Clayton CP, et al. Redesigning residency training in internal medicine: the consensus report of the alliance for academic internal medicine education redesign task force. Acad Med. 2007;82(12):1211–1219. doi: 10.1097/ACM.0b013e318159d010. [DOI] [PubMed] [Google Scholar]
- 20.Nadkarni M, Reddy S, Bates CK, Fosburgh B, Babbott S, Holmboe E. Ambulatory-based education in internal medicine: current organization and implications for transformation. results of a national survey of resident continuity clinic directors. J Gen Intern Med. 2011;26(1):16–20. doi: 10.1007/s11606-010-1437-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stevens DP, Bowen JL, Johnson JK, Woods DM, Provost LP, Holman HR, et al. A multi-institutional quality improvement initiative to transform education for chronic illness care in resident continuity practices. J Gen Intern Med. 2010;25(Suppl 4):S574–S580. doi: 10.1007/s11606-010-1392-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stevens DP, Wagner EH. Transform residency training in chronic illness care—now. Acad Med. 2006;81(8):685–687. doi: 10.1097/00001888-200608000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Health Resources and Services Administration Primary Care Residency Expansion Initiative, (HRSA-10-277, 2010).
- 24.VA centers of excellence in primary care education [Internet]. 810 Vermont Avenue, NW - Washington, DC 20420: U.S. Department of Veterans Affairs. Available from: http://www.va.gov/oaa/rfp_coe.asp. Accessed June 22, 2012.
- 25.Babbott SF, Beasley BW, Reddy S, Duffy FD, Nadkarni M, Holmboe ES. Ambulatory office organization for internal medicine resident medical education. Acad Med. 2010;85(12):1880–1887. doi: 10.1097/ACM.0b013e3181fa46db. [DOI] [PubMed] [Google Scholar]
- 26.American college of physicians medical home builder [Internet]. 190 North Independence Mall West, Philadelphia, PA 19106–1572: American College of Physicians; 2011. Available from: https://www.medicalhomebuilder.org/home. Accessed June 22, 2012.
- 27.ACGME outcomes project [Internet]. 515 N. State Street Suite 2000 Chicago, Il 60654: ACGME; 2011. Available from: http://www.acgme.org/acWebsite/home/home.asp. Accessed June 22, 2012.
- 28.Royal College of Physicians and Surgeons of Canada CanMEDS [Internet]: Royal College of Physicians and Surgeons of Canada; 2011. Available from: http://www.royalcollege.ca/public/resources/aboutcanmeds. Accessed June 22, 2012.
- 29.Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the flexner report. N Engl J Med. 2006;355(13):1339–1344. doi: 10.1056/NEJMra055445. [DOI] [PubMed] [Google Scholar]
- 30.Green ML, Aagaard EM, Caverzagie KJ, Chick DA, Holmboe E, Kane G, et al. Charting the road to competence: developmental milestones for internal medicine residency training. J Grad Med Educ. 2009;1(1):5–20. doi: 10.4300/01.01.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.ten Cate O. Entrustability of professional activities and competency-based training. Med Educ. 2005;39(12):1176–1177. doi: 10.1111/j.1365-2929.2005.02341.x. [DOI] [PubMed] [Google Scholar]
- 32.Carraccio C, Burke AE. Beyond competencies and milestones: adding meaning through context. J Grad Med Educ. 2010;2(3):419–422. doi: 10.4300/JGME-D-10-00127.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Frank JR, Snell LS, Cate OT, Holmboe ES, Carraccio C, Swing SR, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638–645. doi: 10.3109/0142159X.2010.501190. [DOI] [PubMed] [Google Scholar]
- 34.ten Cate TJO, Snell L, Carraccio C. Medical competence: the interplay between individual ability and the health care environment. Med Teach. 2010;32(8):669–675. doi: 10.3109/0142159X.2010.500897. [DOI] [PubMed] [Google Scholar]
- 35.Jones MD, Jr, Rosenberg AA, Gilhooly JT, Carraccio CL. Perspective: competencies, outcomes, and controversy–linking professional activities to competencies to improve resident education and practice. Acad Med. 2011;86(2):161–165. doi: 10.1097/ACM.0b013e31820442e9. [DOI] [PubMed] [Google Scholar]
- 36.ten Cate O, Scheele F. Competency-based postgraduate training: can we bridge the gap between theory and clinical practice? Acad Med. 2007;82(6):542–547. doi: 10.1097/ACM.0b013e31805559c7. [DOI] [PubMed] [Google Scholar]
- 37.Mulder H, Cate OT, Daalder R, Berkvens J. Building a competency-based workplace curriculum around entrustable professional activities: the case of physician assistant training. Med Teach. 2010;32(10):e453–e459. doi: 10.3109/0142159X.2010.513719. [DOI] [PubMed] [Google Scholar]
- 38.National committee for quality assurance patient centered medical home 2011 [Internet]. 1100 13th Street, NW, Suite 1000, Washington, DC 20005: National Committee for Quality Assurance; 2011. Available from: http://www.ncqa.org/tabid/631/default.aspx. Accessed June 22, 2012.
- 39.Joint principles for the medical education of physicians as preparation for practice in the patient-centered medical home. American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP), American Osteopathic Association (AOA); 2010. Available at www.aafp.org/online/etc/medialib/aafp_org/documents/news_pubs/ann/joint-principles-for-med-ed.Par/
- 40.Sterkenburg A, Barach P, Kalkman C, Gielen M, ten Cate O. When do supervising physicians decide to entrust residents with unsupervised tasks? Acad Med. 2010;85(9):1408–1417. doi: 10.1097/ACM.0b013e3181eab0ec. [DOI] [PubMed] [Google Scholar]
- 41.Scheele F, Teunissen P, Luijk SV, Heineman E, Fluit L, Mulder H, et al. Introducing competency-based postgraduate medical education in the Netherlands. Med Teach. 2008;30(3):248–253. doi: 10.1080/01421590801993022. [DOI] [PubMed] [Google Scholar]
- 42.Hammick M, Olckers L, Campion-Smith C. Learning in interprofessional teams: AMEE guide no 38. Med Teach. 2009;31(1):1–12. doi: 10.1080/01421590802585561. [DOI] [PubMed] [Google Scholar]
- 43.Parmelee DX, Michaelsen LK. Twelve tips for doing effective team-based learning (TBL) Med Teach. 2010;32(2):118–122. doi: 10.3109/01421590903548562. [DOI] [PubMed] [Google Scholar]