Abstract
BackgroundSplenic preservation during a distal pancreatectomy (SPDP) may be performed with splenic vessel ligation, known as Warshaw's Technique (WT) or splenic vessel preservation (SVP). The consensus on which approach is best is divided. A systematic review of evidence in the literature was undertaken with the aim of analysing the merits and disadvantages of both WT and SVP.
MethodsA systematic search of medical literature from 1985–2011 was undertaken to identify all comparative studies and case series on SPDP. Non-English papers, series with < 5 patients, technical reports and reviews were excluded. The remaining articles were reviewed considering the study design, surgical technique, outcomes and complications.
ResultsIn 23 relevant studies, 356 patients underwent WT and 572 underwent SVP. In WT patients, the mean operating time (160 versus 215 min, P < 0.001), mean estimated blood loss (301 versus 390 ml, P < 0.001) and length of stay (8 versus 11 days, P < 0.001) was significantly less than the SVP patients, respectively. Considering complications, splenic infarction and splenectomy occurred more frequently in WT patients (P < 0.05).
DiscussionWT is technically easier to perform than SVP but has a higher incidence of subsequent splenectomies. Surgeons should be able to perform both procedures and tailor the technique according to the patient.
Introduction
A distal pancreatectomy is commonly performed for benign tumours with a low malignant potential, chronic pancreatitis and trauma affecting the tail of the pancreas. This can be performed with or without preservation of the spleen. A number of previous studies have shown the feasibility and benefits of splenic preservation during a distal pancreatectomy, including a lower risk of developing post-splenectomy sepsis and malignancies in the future.1
Spleen preservation can be achieved with ligation and transection or preservation of splenic vessels. Splenic preservation with ligation and transection of the splenic artery and vein, relying on collateral circulation from the short gastric vessels, was described by Warshaw in 1988 in an open distal pancreatectomy.2 Since then many reports have confirmed the feasibility and safety of this procedure in the absence of locally advanced disease or splenomegaly.3,4,5 An alternative technique is to preserve the splenic artery and vein, and divide the small branches to the distal pancreas (SVP) (Fig. 1). Theoretically this is technically more challenging; however, it may cause less spleen-related complications. The number of spleen-preserving distal pancreatectomies using Warshaw's technique remains small and published series are often based on limited personal experience. No randomized controlled trial has been performed to date and as such the superiority of one technique over another is not apparent.
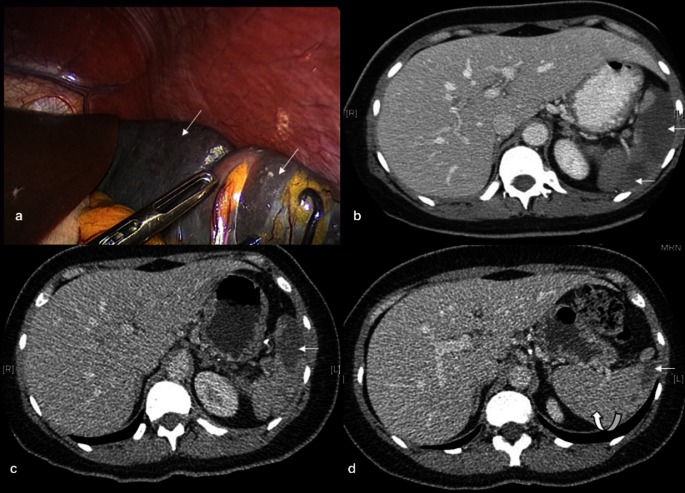
Figure 1.
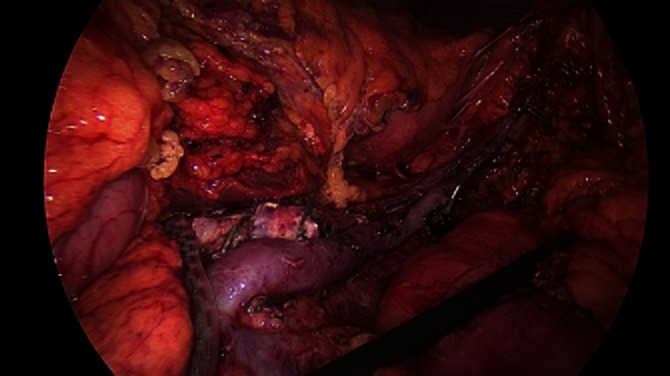
Laparoscopic splenic vessel preserving distal pancreatectomy in a patient with mucinous cystadenoma in the body of the pancreas
The aim of this systemic review was to analyse the merits and disadvantages of Warshaw's Technique (WT) and a spleen vessel preserving (SVP) distal pancreatectomy.
Methods and materials
Study design
A comprehensive literature search was performed using Medline, Embase, PubMed and Cochrane between January 1985 and July 2011. The following search terms were used: ‘spleen preserve*’, ‘spleen preserving’, ‘spleen preservation’, splenic vessel preserv*, ‘splenic vessel preserving’, ‘splenic vessel preservation’, ‘distal pancreatectomy’, ‘left pancreatic resection’, ‘left pancreatectomy’ and ‘Warshaw technique’. The search strategies were combined which revealed papers with a spleen-preserving distal pancreatectomy (SPDP) irrespective of the technique of splenic preservation. The PRISMA guidelines and flowchart was used for this study.6
Data extraction and eligibility criteria
The abstracts of identified papers were assessed and those that dealt with SPDP were retained. Excluded papers included those that were not in the English language and translations could not be obtained, technical reports, reviews, animal and human cadaveric studies. In order to reduce publication bias, case reports, case series of less than five patients were excluded.
Of the remaining abstracts full articles were obtained. Papers that did not have sufficient data on the two methods of SPDP were excluded. Where more than one pancreatic procedure was reported in an article, only data relating to the distal pancreatectomy were included for analysis. Where sequential reports were presented from the same Institution, only the most recent data from that Centre was included for analysis to avoid duplication of patients.
Data collection
All articles included for analysis were reviewed by two independent reviewers (G.J. and S.C.). In the case of any ambiguity, the senior author (A.G.P.) was asked to review the study to reach a consensus. The presence of any bias was assessed. The technique of SPDP based on splenic vessel preservation or splenic vessel ligation and transection was noted. In each group, the patient characteristics, indications for the operation, estimated blood loss, operative time, post-operative events and outcomes, complications including splenectomy rates and conversions, tumour characteristics and histology were reviewed. Morbidity and mortality rates were also noted.
Statistical analysis
Data extracted for the Warshaw and SVP distal pancreatectomy groups were described in terms of weighted mean and percentages. The categorical variables were compared using the chi-square test, with continuous variables compared using the non-parametric Mann–Whitney U-test. SPSS statistical package version 17 was used for the analysis (SPSS Inc., Chicago, IL, USA).
Results
The initial search identified 547 relevant articles with 23 articles included in the final analysis (Fig. 2). All papers were published between 1988 and July 2011. No randomized controlled trials were identified. There were two comparative studies (1 prospective and 1 retrospective) and 21 case series (16 retrospective and 5 prospective articles) with a total of 928 patients treated (Table 1). Within the case series two multicentre studies were identified. Two articles from the same institution were included which covered two different time periods. Seven series performed both a Warshaw and a SVP distal pancreatectomy; however, only two studies compared the outcomes between these groups. The remaining 16 series performed either a WT or SVP distal pancreatectomy.
Figure 2.
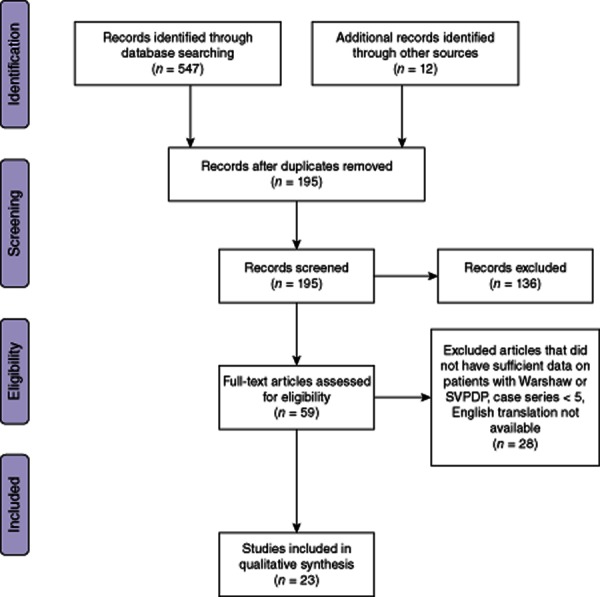
PRISMA flow diagram
Table 1.
Characteristics of studies on a spleen-preserving distal pancreatectomy
| Study | Year | Type | Centre | Technique | No. of patients | Operating time (min) | Blood loss (ml) | Splenic infarction | Splenectomy | Stay (days) |
|---|---|---|---|---|---|---|---|---|---|---|
| Beane7 | 2011 | Comparative, retrospective | USA, 2002–2009 | Warshaw | 41 | 200 | 507 | 16 | — | 6.3 |
| SVP | 45 | 200 | 224 | 1 | — | 4.5 | ||||
| Fernández-Cruz3 | 2004 | Comparative, prospective | Spain, 1999–2004 | Warshaw | 8 | 165 | 275 | 3 | 1 | — |
| SVP | 10 | 223 | 495 | 0 | — | — | ||||
| Ferrone4 | 2011 | Case series | USA, 1986–2009 | Warshaw | 158 | — | — | 15 | 3 | — |
| Tien27 | 2010 | Case series | Taiwan, 2002–2007 | Warshaw | 37 | 116 | 140 | — | — | 8.4 |
| Song28 | 2011 | Case series | South Korea 2005–2010 | Warshaw | 28 | — | — | 13 | — | — |
| SVP | 150 | — | — | — | — | — | ||||
| Kimura29 | 2010 | Case series | Japan 2001–2007 | SVP | 16 | 367 | 243 | — | — | 21 |
| Lee17 | 2010 | Case series | South Korea, 1995–2006 | SVP | 37 | 215 | 396 | 1 | — | 16 |
| Laxa30 | 2010 | Case series | USA, 2005–2007 | SVP | 6 | 164 | 58 | — | — | — |
| Taylor11 | 2010 | Case series | Australia, 1996–2006 | Warshaw | 5 | — | — | 2 | 0 | — |
| SVP | 9 | — | — | — | — | — | ||||
| Bruzoni10 | 2008 | Case series | USA, 2001–2007 | SVP | 11 | 152 | 362 | 0 | — | 9 |
| Yadav23 | 2008 | Case series | India, 2001–2005 | SVP | 5 | 4.75 | — | 0 | — | — |
| Melotti18 | 2008 | Case series | Italy, 1999–2005 | Warshaw | 5 | — | — | 1 | 1 | — |
| SVP | 28 | — | — | — | — | — | ||||
| Kleeff31 | 2008 | Case series | Germany 1993–2006 | SVP | 59 | 200 | 500 | — | — | 10 |
| Goh32 | 2008 | Case series | Singapore, 1986–2006 | SVP | 21 | 150 | — | — | 0 | 7 |
| Uranues33 | 2006 | Case series | Austria, 2003–2005 | SVP | 5 | 174 | — | — | — | — |
| Carrere5 | 2006 | Case series | France, 1990–2005 | Warshaw | 36 | — | — | — | — | — |
| Dulucq19 | 2005 | Case series | France,1995–2003 | Warshaw | 16 | 154 | 162 | — | — | 10.8 |
| Mabrut20 | 2005 | Case series | Multicentre European 1995–2002 | Warshaw | 7 | — | — | 1 | 2 | — |
| SVP | 54 | — | — | — | —— | — | ||||
| Miura34 | 2005 | Case series | Japan, 1995–2003 | Warshaw | 9 | — | — | 0 | 0 | — |
| Shoup1 | 2002 | Case series | USA, 1983–2000 | SVP | 46 | 2.9 | 350 | — | — | 7 |
| Lillimoe16 | 1999 | Case series | USA, 1994–1997 | SVP | 37 | 5.1 | 566 | — | — | 21 |
| Benoist35 | 1999 | Case series | France, 1992–1997 | SVP | 15 | — | — | 0 | 0 | — |
| Aldridge15 | 1991 | Case Series | UK, 1978–1990 | Warshaw | 5 | — | — | 0 | 0 | — |
| SVP | 30 | — | — | — | — | — |
Study heterogeneity and bias
Most of the studies emphasized the feasibility of splenic preservation and did not necessarily report all relevant data individually on patients with both techniques. The articles discussing the WT were mainly case series performed by experts in WT. Similarly, there were case series performed by experts in the SVP technique. Thus, a low level of evidence was essentially available for this review. The best evidence lay in the two comparative studies. In the prospective comparative study by Fernández-Cruz et al.3 no definite matching was mentioned, whereas the matched comparative study by Beane et al.7 was retrospective allowing a risk of a selection bias in both studies. A meta-analysis could not be performed as the studies were too heterogeneous and measures of dispersion for the outcomes of interest were not readily available for both techniques.
Patient characteristics
A total of 356 patients underwent WT, whereas 572 patients underwent a SVP distal pancreatectomy. Age was specified in only six articles and the weighted mean age for the Warshaw and SVP patients was similar (Table 2). Cystic neoplasms were the commonest indication for the procedure. Of the total 928 patients, 401 patients underwent a laparoscopic distal pancreatectomy with splenic preservation of which 105 (30%) underwent a laparoscopic Warshaw's technique and 296 (52%) underwent a SVP laparoscopic distal pancreatectomy.
Table 2.
Patient characteristics
| Warshaw's technique | SVP technique | |
|---|---|---|
| Age (years)a | 52 (47–58) | 48 (25–66) |
| Gender (male : female) | 100:195 | 43:69 |
| Indications:b | ||
| Cystic and solitary pseudo papillary neoplasms: | 39% (95/247) | 30% (37/124) |
| IPMN | 18% (44/247) | 31% (39/124) |
| Neuroendocrine tumours | 16% (41/247) | 9% (11/124) |
| Malignancy | 4% (10/247) | 10% (12/124) |
| Others (cysts, pancreatitis, trauma) | 23% (57/247) | 20% (25/124) |
Data in weighted mean (range).
Data in percentage (number of patients/ total number of reported patients).
IPMN, intraductal papillary mucinous neoplasm.
Intra-operative data
Operative time was reported in 13 articles. Warshaw's technique took significantly less time than SVP (P < 0.001) (Table 3). The mean estimated blood loss was reported in 371 patients. Blood loss with the Warshaw technique was significantly less than the SVP group (P < 0.001). The mean length of stay (LOS) was reported in 367 patients. LOS for WT patients was significantly less than for SVP patients (P < 0.001). Many series included laparoscopic operations and including both techniques after laparoscopy the conversion rate was 5.5% and the length of stay was a mean of 7 days. A separate subgroup analysis in laparoscopic patients was not possible because of a lack of relevant data.
Table 3.
Peri-operative outcomes
| Warshaw's technique | SVP technique | P-value | |
|---|---|---|---|
| Operating time (min) | 160 (116–200) | 215 (150–367) | < 0.001 |
| Blood loss (ml) | 301 (140–507) | 391 (58–566) | < 0.001 |
| Length of stay (days) | 8 (6–11) | 11. (4–21) | < 0.001 |
All data in weighted mean (range).
Complications
An intra-operative splenectomy was similar in the SVP (1.2%, n = 77) and WT patients (0.6%, n = 2) (P = 0.49). A post-operative splenectomy after Warshaw's technique was significantly higher than SVP (2% v 0%, P < 0.01) and the main indication for a splenectomy was splenic infarction. (Table 4) Overall, the incidence of a splenic infarction was significantly higher in the Warshaw group than in the SVP group (P < 0.001). Splenomegaly was observed only in the Warshaw group (4.2%, n = 15). Both submucosal and perigastric varices were only seen in the Warshaw's technique group; however, only one patient (1%) suffered from bleeding. None of the patients in the SVP group were reported to have varices; however, this difference did not reach statistical significance. The post-operative outcome of Warshaw's technique was better evaluated compared with SVP as a post-operative computed tomography (CT) scan was routinely performed in all patients who underwent the Warshaw's technique but only selectively performed in SVP patients. There was no difference in the pancreatic fistula rate between the WT and SVP group. The incidence of intra-abdominal collections was also similar in both groups. Five patients (38%) who underwent Warshaw's technique developed significant post-operative pain, but none in the SVP group reported chronic abdominal pain (P < 0.05). Death was reported in one patient (0.2%) in the SVP group, after a traumatic splenic injury, which was thought to be as a result of undetected post-operative bleeding.
Table 4.
Complications
| Warshaw's technique | SVP technique | aP-value | |
|---|---|---|---|
| Splenic complications: | |||
| Post-operative splenectomy | 2% (7/356) | 0% (0/574) | 0.001 |
| Splenic infarction | 22% (51/233) | 2% (2/103) | <0.001 |
| Perigastric varices | 17% (39/232) | 0% (0/15) | 0.14 |
| Submucosal varices | 11% (5/46) | 0% (0/15) | 0.58 |
| Intra-abdominal collections | 6% (7/111) | 4% (12) | 0.29 |
| Pancreatic fistula | 11% (17/148) | 16% (41/253) | 0.15 |
| Chronic left-sided abdominal pain | 38% (5/13) | 0% (0/15) | 0.048 |
All data in percentage (number of patients/total number of reported patients).
P-values calculated using the chi-square test.
Discussion
Malignant tumours of the body and tail of the pancreas require a distal pancreatectomy and splenectomy to achieve oncological clearance as lymph node involvement is commonly seen in pancreatic adenocarcinoma (30–70%), invasive intraductal papillary mucinous neoplasms (46%) and invasive mucinous cystic neoplasms (24%).5,8,9,10,11 A splenectomy is associated with a lifetime risk for developing overwhelming post splenectomy infection (OPSI) of 1% to 5% in the general population and OPSI is associated with a mortality of 50–70%.12 Patients are required to undergo pre-operative prophylactic vaccinations and a lifelong commitment to antibiotic treatment to prevent sepsis.13 In 985 patients who underwent a splenectomy in conjunction with surgery for non-traumatic or non-malignant conditions of adjacent organs, a 40% elevated risk of total cancer was found 5–9 years later, with significant increases of lung and ovarian cancers.14 Therefore, preserving the spleen has a number of health advantages. As a result, splenic preservation is becoming the preferred approach when undertaking a distal pancreatectomy in benign conditions or diseases with a low malignant potential. Comparative studies on distal pancreatectomy with and without spleen preservation have shown that the spleen can be safely preserved and that it carries the same risk of post-operative morbidity when compared with a distal pancreatectomy with splenectomy.15,16 A case-matched study demonstrated better long-term outcomes and fewer complications with splenic preservation methods.5 A laparoscopic approach to a distal pancreatectomy is growing in popularity and several series from 2004 to 2011, have successfully used a laparoscopy for both techniques with a low conversion rate (5.5%).3,7,17,18,19,20
While splenic preservation is considered the operation of choice during a distal pancreatectomy for benign disease, the surgical technique for splenic preservation is yet to be decided. Spleen preservation with ligation and transection of splenic vessels was described by Warshaw in 1988 in an open distal pancreatectomy.2A SVP distal pancreatectomy was performed initially by paediatric surgeons.21 It was later successfully performed by Aldridge in 199115 and has since then been popularized by Kimura et al.22 In a retrospective matched comparative study,7 45 SVP patients were compared with 41 WT patients. SVP patients were found to have significantly less blood loss and splenic infarctions than the WT patients. Conversely, in the only prospective comparative study, 11 SVP patients were compared with eight WT patients3 and here the WT patients had significantly less blood loss and a shorter operating time than the SVP group. These contrasting results highlight the difficulty in choosing one technique over the other.
The Warshaw approach to a distal pancreatectomy may be considered less technically demanding than splenic vessel preservation which involves meticulous dissection and control of the pancreatic branches of the splenic vessels. This difference in surgical approach is reflected in shorter operating times (160 versus 215 min, P < 0.001) and less blood loss (P < 0.01) seen in WT patients compared with SVP. Intra-operative complications requiring a splenectomy were similar in the SVP group (1.2%, n = 7)3,19,23 and the WT group (0.6%, n = 2). The main reason for proceeding with an intra-operative splenectomy was bleeding from the splenic vessels.3,18 If the intended surgical approach was a SVP technique, the success rate ranged from 55–84% and in the unsuccessful patients quite often WT was attempted.3,4,18 However, in the WT, the procedure was successfully completed in 95–100% of patients.3,5
It is felt that WT can lead to more post-operative problems compared with SVP. In WT, splenic vessel ligation and transection places the spleen at a greater risk of ischaemia compared with SVP. Sato et al.24 found that on assessment with colour Doppler after WT, the blood supply to the spleen was half of that seen pre-operatively; however, the blood supply recovered within 10 days after surgery. In an analysis of splenic artery embolization after trauma, 63% of patients' experienced splenic infarction with proximal embolization but all resolved over time.25 After routine post-operative screening in his patients, Warshaw felt that a splenic infarction is well tolerated as long as the area affected is less than a third of the spleen and in these patients an intervention may not be required.26 The findings of this review confirm that splenic infarction rates were significantly higher in WT (22%) compared to SVP patients (1.9%, P < 0.01). However, the post-operative splenectomy rate after a WT is only 2% (SVP group 0%). There is probably a process of cell necrosis in the infarcted spleen with regeneration of viable splenic tissue supplied by the short gastric vessels (Fig. 3). As sequelae of this it is not uncommon for patients to experience pain.3,11 Chronic pain was significantly higher in the Warshaw group (38%) than the SVP group (0%).
Figure 3.
Laparoscopic Warshaw technique in a patient showing (a) areas of ischaemia (straight arrows) intra-operatively and (b) on computerised tomography (CT) 10 days post-operatively. Serial CT scans show (c) a reduction in ischaemia (straight arrows) at 1 month and (d) regeneration and hypertrophy of the spleen at 6 months (curved arrow)
Three important determinants for a successful Warshaw's technique have emerged from the literature. They include the size of the spleen, acute inflammation and variation in splenic vessel anatomy, such as paucity of short gastric vessels. All of these factors can be assessed on a pre-operative CT scan. Perfusion from the short gastric vessels may not be adequate for splenomegaly patients. WT can increase the pressure in the short gastric vessels causing varices. In this review, perigastric and submucosal varices were seen after WT but this was not significant compared with SVP patients. In a study of 37 patients after WT, on serial CT scan and endoscopy, 11 patients were found to have developed perigastric varices and three had developed gastric submucosal varices. After 18 months, gastric submucosal varices did not show any progression and none of the patients had variceal bleeding after 45.3 months.27 Therefore, developing varices may be a physiological adjustment without any clinical relevance. Other known sequelae including pancreatic fistulae or intra abdominal abscess rates were similar after both surgical techniques.
This review was limited by the level of evidence reported in the literature, a dearth of well-designed comparative studies, a comparison of different case series that could not be matched and the difference in experience of the surgeon performing a particular technique. In spite of these short comings, this systematic review has given us a better understanding of both the Warshaw and SVP techniques.
Conclusion
The WT and SVP technique have certain benefits and disadvantages. The Warshaw technique is easier to perform than SVP as confirmed by a shorter operating time, less blood loss and higher completion rate. However, post-operatively WT is associated with splenic ischaemia and possible chronic pain and a higher rate of splenectomy than SVP. So patients with a normal-sized spleen, good blood supply from short gastric vessels and those who need a short operation may benefit from WT. The SVP technique may be performed in most situations, but WT may still be considered to attempt spleen preservation when SVP fails. In conclusion, both the WT and SVP technique should be present in the armamentarium of the surgeon as both techniques have a specific role to play in a spleen-preserving distal pancreatectomy.
Conflicts of interest
None declared.
References
- Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra D, Conlon KC. The value of splenic preservation with distal pancreatectomy. Arch Surg. 2002;137:164–168. doi: 10.1001/archsurg.137.2.164. [DOI] [PubMed] [Google Scholar]
- Warshaw AL. Conservation of the spleen with distal pancreatectomy. Arch Surg. 1988;123:550–553. doi: 10.1001/archsurg.1988.01400290032004. [DOI] [PubMed] [Google Scholar]
- Fernández-Cruz L, Martínez I, Gilabert R, Cesar-Borges G, Astudillo E, Navarro S. Laparoscopic distal pancreatectomy combined with preservation of the spleen for cystic neoplasms of the pancreas. J Gastrointest Surg. 2004;8:493–501. doi: 10.1016/j.gassur.2003.11.014. [DOI] [PubMed] [Google Scholar]
- Ferrone CR, Konstantinidis IT, Sahani DV, Wargo JA, Fernandez-del Castillo C, Warshaw AL. Twenty-three years of the Warshaw operation for distal pancreatectomy with preservation of the spleen. Ann Surg. 2011;253:1136–1139. doi: 10.1097/SLA.0b013e318212c1e2. [DOI] [PubMed] [Google Scholar]
- Carrère N, Abid S, Julio CH, Bloom E, Pradère B. Spleen-preserving distal pancreatectomy with excision of splenic artery and vein: a casematched comparison with conventional distal pancreatectomy with splenectomy. World J Surg. 2007;31:375–382. doi: 10.1007/s00268-006-0425-6. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Beane JD, Pitt HA, Nakeeb A, Schmidt CM, House MG, Zyromski NJ, et al. Splenic preserving distal pancreatectomy: does vessel preservation matter? J Am Coll Surg. 2011;212:651–657. doi: 10.1016/j.jamcollsurg.2010.12.014. [DOI] [PubMed] [Google Scholar]
- Glanemann M, Shi B, Liang F, Sun XG, Bahra M, Jacob D, et al. Surgical strategies for treatment of malignant pancreatic tumors: extended, standard or local surgery? World J Surg Oncol. 2008;6:123. doi: 10.1186/1477-7819-6-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kargozaran H, Vu V, Ray P, Bagaria S, Steen S, Ye X, et al. Invasive IPMN and MCN: same organ, different outcomes? Ann Surg Oncol. 2011;18:345–351. doi: 10.1245/s10434-010-1309-4. [DOI] [PubMed] [Google Scholar]
- Bruzoni M, Sasson AR. Open and laparoscopic spleen-preserving, splenic vessel-preserving distal pancreatectomy: indications and outcomes. J Gastrointest Surg. 2008;12:1202–1206. doi: 10.1007/s11605-008-0512-0. [DOI] [PubMed] [Google Scholar]
- Taylor C, O'Rourke N, Nathanson L, Martin I, Hopkins G, Layani L, et al. Laparoscopic distal pancreatectomy: the Brisbane experience of forty-six cases. HPB. 2008;10:38–42. doi: 10.1080/13651820701802312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brigden ML. Overwhelming postsplenectomy infection still a problem. West J Med. 1992;157:440–443. [PMC free article] [PubMed] [Google Scholar]
- Davies JM, Lewis MP, Wimperis J, Rafi I, Ladhani S, Bolton-Maggs PH. British Committee for Standards in Haematology. Review of guidelines for the prevention and treatment of infection in patients with an absent or dysfunctional spleen: prepared on behalf of the British Committee for Standards in Haematology by a working party of the Haemato-Oncology task force. Br J Haematol. 2011;155:308–317. doi: 10.1111/j.1365-2141.2011.08843.x. [DOI] [PubMed] [Google Scholar]
- Linet MS, Nyrén O, Gridley G, Mellemkjaer L, McLaughlin JK, Olsen JH, et al. Risk of cancer following splenectomy. Int J Cancer. 1996;66:611–616. doi: 10.1002/(SICI)1097-0215(19960529)66:5<611::AID-IJC5>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- Aldridge MC, Williamson RC. Distal pancreatectomy with or without splencetomy. Br J Surg. 1991;78:976–979. doi: 10.1002/bjs.1800780827. [DOI] [PubMed] [Google Scholar]
- Lillemoe KD, Kaushal S, Cameron JL, Sohn TA, Pitt HA, Yeo CJ. Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg. 1999;229:693–700. doi: 10.1097/00000658-199905000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SE, Jang JY, Lee KU, Kim SW. Clinical comparison of distal pancreatectomy with or without splenectomy. J Korean Med Sci. 2008;23:1011–1014. doi: 10.3346/jkms.2008.23.6.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melotti G, Butturini G, Piccoli M, Casetti L, Bassi C, Mullineris B, et al. Laparoscopic distal pancreatectomy: results on a consecutive series of 58 patients. Ann Surg. 2007;246:77–82. doi: 10.1097/01.sla.0000258607.17194.2b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulucq JL, Wintringer P, Stabilini C, Feryn T, Perissat J, Mahajna A. Are major laparoscopic pancreatic resections worthwhile? A prospective study of 32 patients in a single institution. Surg Endosc. 2005;19:1028–1034. doi: 10.1007/s00464-004-2182-7. [DOI] [PubMed] [Google Scholar]
- Mabrut JY, Fernandez-Cruz L, Azagra JS, Bassi C, Delvaux G, Weerts J, et al. Laparoscopic pancreatic resection: results of a multicenter European study of 127 patients. Surgery. 2005;137:597–605. doi: 10.1016/j.surg.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Martin LW, Ryckmore FC, Sheldon CA. Experience with 95% pancreatectomy and splenic salvage for neonatal nesidioblastosis. Ann Surg. 1984;200:355–362. doi: 10.1097/00000658-198409000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura W, Inoue T, Futakawa N, Shinkai H, Han I, Muto T. Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein. Surgery. 1996;120:885–890. doi: 10.1016/s0039-6060(96)80099-7. [DOI] [PubMed] [Google Scholar]
- Yadav TD, Natarajan SK, Kishore VM, Lyngdoh S, Wig JD. Spleen-preserving distal pancreatectomy for pancreatic trauma: a series of six cases. JOP. 2007;8:422–428. [PubMed] [Google Scholar]
- Sato Y, Shimoda S, Takeda N, Tanaka N, Hatakeyama K. Evaluation of splenic circulation after spleen preserving distal pancreatectomy by diving the splenic artery and vein. Dig Surg. 2000;17:519–522. doi: 10.1159/000051952. [DOI] [PubMed] [Google Scholar]
- Killeen KL, Shanmuganathan K, Boyd-Kranis R, Scalea TM, Mirvis SE. CT findings after embolization for blunt splenic trauma. J Vasc Interv Radiol. 2001;12:209–214. doi: 10.1016/s1051-0443(07)61827-2. [DOI] [PubMed] [Google Scholar]
- Warshaw AL. Distal pancreatectomy with preservation of the spleen. J Hepatobiliary Pancreat Sci. 2010;17:808–812. doi: 10.1007/s00534-009-0226-z. [DOI] [PubMed] [Google Scholar]
- Tien YW, Liu KL, Hu RH, Wang HP, Chang KJ, Lee PH. Risk of variceal bleeding after spleen preserving distal pancreatectomy with excision of splenic artery and vein. Ann Surg Oncol. 2010;17:2193–2198. doi: 10.1245/s10434-010-0983-6. [DOI] [PubMed] [Google Scholar]
- Song KB, Kim SC, Park JB, Kim YH, Jung YS, Kim MH, et al. Single-center experience of laparoscopic left pancreatic resection in 359 consecutive patients: changing the surgical paradigm of left pancreatic resection. Surg Endosc. 2011;25:3364–3372. doi: 10.1007/s00464-011-1727-9. [DOI] [PubMed] [Google Scholar]
- Kimura W, Yano M, Sugawara S, Okazaki S, Sato T, Moriya T, et al. Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein: techniques and its significance. J Hepatobiliary Pancreat Sci. 2010;17:813–823. doi: 10.1007/s00534-009-0250-z. [DOI] [PubMed] [Google Scholar]
- Laxa BU, Carbonell AM, 2nd, Cobb WS, Rosen MJ, Hardacre JM, Mekeel KL, et al. Laparoscopic and hand-assisted distal pancreatectomy. Am Surg. 2008;74:481–486. [PubMed] [Google Scholar]
- Kleeff J, Diener MK, Z'graggen K, Hinz U, Wagner M, Bachmann J, et al. Distal pancreatectomy: risk factors for surgical failure in 302 consecutive cases. Ann Surg. 2007;245:573–582. doi: 10.1097/01.sla.0000251438.43135.fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh BK, Tan YM, Chung YF, Cheow PC, Ong HS, Chan WH, et al. Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg. 2008;143:956–965. doi: 10.1001/archsurg.143.10.956. [DOI] [PubMed] [Google Scholar]
- Uranues S, Alimoglu O, Todoric B, Toprak N, Auer T, Rondon L, et al. Laparoscopic resection of the pancreatic tail with splenic preservation. Am J Surg. 2006;192:257–261. doi: 10.1016/j.amjsurg.2006.01.031. [DOI] [PubMed] [Google Scholar]
- Miura F, Takada T, Asano T, Kenmochi T, Ochiai T, Amano H, et al. Hemodynamic changes of splenogastric circulation after spleen-preserving pancreatectomy with excision of splenic artery and vein. Surgery. 2005;138:518–522. doi: 10.1016/j.surg.2005.04.020. [DOI] [PubMed] [Google Scholar]
- Benoist S, Dugué L, Sauvanet A, Valverde A, Mauvais F, Paye F, et al. Is there a role of preservation of the spleen in distal pancreatectomy? J Am Coll Surg. 1999;188:255–260. doi: 10.1016/s1072-7515(98)00299-3. [DOI] [PubMed] [Google Scholar]