Abstract
Purpose
The purpose of this study was to present the preliminary clinical and radiographic outcomes of the treatment of femoral head osteochondral defects in eight consecutive symptomatic patients with fresh-stored osteochondral allografts via a trochanteric osteotomy.
Methods
This study included all consecutive patients treated in our department between 2008 and 2010 for worsening pain and mechanical symptoms of femoral head osteochondral defects. Each patient had preoperative routine hip radiographs and a preoperative magnetic resonance imaging study that determined and recorded the defect size and femoral head diameters. Allograft donors were identified through the Multiple Organ Retrieval and Exchange program (Ontario, Canada).
Results
The osteochondral defects were secondary to osteochondritis dissecans in four patients, avascular necrosis in three and femoral head fracture without dislocation in one. The patients’ average age at surgery was 23.7 (range 17–42), and the average follow-up was 41 months (range 24–54). Follow-up included clinical and radiographic examinations at standard intervals. The average Harris hip scores improved from 57.7 (range 50–65) points preoperatively to 83.9 (range 72–94) points at latest follow-up. Five patients had good-to-excellent clinical outcomes, and one had a fair outcome. One patient was converted to a total hip arthroplasty due to progression of arthritis. Another patient’s graft subsided and he underwent a successful repeat transplantation. An additional patient required the removal of the screws transfixing her trochanter due to persistent irritation.
Conclusions
These findings indicate that fresh-stored osteochondral allograft transplantation using a trochanteric slide and surgical dislocation is a viable treatment option for femoral head defects in young patients.
Introduction
Femoral head defects can occur as a result of several conditions, among them trauma, osteochondritis dissecans (OCD) and avascular necrosis (AVN) [1, 2]. Patients may experience severe pain and develop early degenerative changes similar to full-thickness cartilage defects of other weight-bearing surfaces, such as the knee or the ankle. Potential treatment options include microfracture, autologous chondrocyte implantation, autologous whole-tissue transplantation, periacetabular osteotomy, femoral osteotomy and hip arthroplasty [3–5]. The goal of any cartilage repair technique should be restoration of articular surface congruity to enable normal joint kinematics with pain-free range of motion.
Fresh-stored osteochondral allografts have been in use for the past four decades for the treatment of osteochondral allografts about the knee and ankle [6–8], yet the literature regarding their use for the treatment of femoral head defects is scarce. There are only two studies in the literature that present the outcomes of fresh-stored osteochondral allografts for the treatment of femoral head lesions. Meyers et al. described a technique by which femoral heads with AVN were treated by debriding the defect to bleeding bone, packing with morselised bone graft and covering the defect using a 5-mm thick subchondral bone with an articular allograft [5]. All 21 operations in that series were performed through a posterior approach and a T-shaped capsulotomy. Those authors reported successful outcomes in 15 of the 21 studied hips (71 %) after a follow-up of 18 months. The success rate in patients with AVN due to steroid intake in their cohort, however, was only 50 %. Evans and Providence described a defect of a single case of OCD in the weight-bearing area of the femoral head that was treated with a large 12-mm thick fresh osteochondral allograft using a trochanteric osteotomy with a very good outcome at the one-year follow-up [9, 10]. The authors of both of those latter studies concluded that the use of fresh osteochondral allografts is promising, especially when the natural history of symptomatic ostechondral defects of the femoral head is rather poor [2, 11].
Our study presents the preliminary clinical and radiographic outcomes of the treatment of femoral head osteochondral defects by means of fresh-stored osteochondral allografts via a femoral trochanteric osteotomy in symptomatic patients.
Method
Participants
All patients’ medical records in the departmental database from 2008–2010 were reviewed after institutional review board (IRB) approval was obtained. Informed consent was obtained. Eight consecutive patients (eight hips) with symptomatic femoral head osteochondral defects who had complained of worsening pain and mechanical symptoms, including catching and locking related to activities of daily living, fulfilled study entry criteria.
Each patient had preoperative routine hip radiographs (anteroposterior of the pelvis as well as anteroposterior and lateral of the involved hip). In addition, all eight patients had a preoperative magnetic resonance imaging (MRI) study in which the size of the defect and the femoral head diameters were determined and recorded. After the preoperative evaluation, the patients were put on a waiting list until a suitable donor became available.
Donors are identified through the M.O.R.E. (Multiple Organ Retrieval and Exchange) program of Ontario (Canada) as being eligible for tissue donation according to the criteria set by the American Association of Tissue Banks [12]. Blood for serology and cultures is collected, but no tissue typing or matching is required [5, 12]. During the harvesting process, the donor’s femoral head is measured by a caliper and matched to a respective recipient within a one millimetre difference in head diameter. The fresh osteochondral femoral head allograft is then placed in a sterile container with 1 g cefazolin and 50,000 units bacitracin per litre of Ringer’s lactate solution (B. Braun Medical Inc, Vaughan, Ontario). The container is stored at 4 °C until transplantation. Although fresh osteochondral material remains viable for transplantation for up to four weeks [13], we preferred to perform the transplantation within two weeks of harvesting, after all the culture and serology tests determined that it was clear of infection.
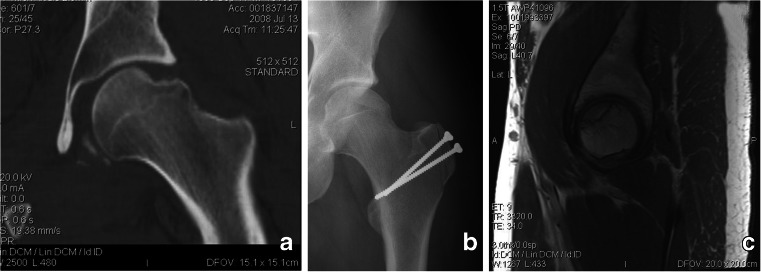
The patients’ average age at surgery was 23.7 ± 8.5 years (range 17–42, Table 1). The osteochondral defects were secondary to OCD in four patients, AVN in three and femoral head fracture without dislocation in one. One AVN was due to prior hip dislocation, one to steroid intake (as part of her leukaemia treatment) and one was idiopathic. The average follow-up was 41.1 ± 11.7 months (range 24–54 months, Table 1), and it consisted of clinical and radiographic examination at standard intervals (preoperative, postoperative at six weeks, at six months, at one year and then annually). Clinical evaluations included the determination of Harris hip scores (HHS) that were recorded preoperatively and at each follow-up visit [14]. The initial six-week postoperative routine hip series of radiographs served as the baseline to which all subsequent radiographs (Fig. 1a–b) were compared by two of the authors (O.S. and Y.K.) who determined whether there had been osteochondral graft collapse or narrowing of the hip joint space. Postoperative MRI was not routinely performed due to cost containment issues, and was performed only when there was a clinical or radiographic suspicion of graft failure (Fig. 1c).
Table 1.
Patients’ demographic and clinical characteristics of the femoral head defects
| Patient number | Gender | Side | Preop. diagnosis | Age at surgery | Complications | Follow-up (months) | Preop. HHS | Latest postop. HHS |
|---|---|---|---|---|---|---|---|---|
| 1 | Male | Left | OCD | 33 | Constant pain lateral hip | 36 | 61 | 80 |
| 2 | Female | Right | OCD | 18 | 42 | 57 | 84 | |
| 3 | Female | Right | OCD | 42 | 48 | 50 | 72 | |
| 4 | Male | Left | AVN | 25 | 54 | 57 | 94 | |
| 5 | Male | Right | Post-trauma AVN | 18 | Collapsed graft | 30 | 53 | 84 |
| 6a | Female | Right | Steroid-induced AVN | 18 | Failed graft | |||
| 7 | Male | Left | Traumatic femoral head fracture | 22 | 54 | 61 | 84 | |
| 8 | Male | Left | OCD | 17 | 24 | 65 | 89 | |
| Min | 17.0 | 24.0 | 50.0 | 72.0 | ||||
| Max | 42.0 | 54.0 | 65.0 | 94.0 | ||||
| Average | 23.7 | 41.1 | 57.7 | 83.9 | ||||
| Median | 20.0 | 42.0 | 57.0 | 84.0 |
OCD osteochondritis dissecans, AVN avascular necrosis
aThe Harris hip score (HHS) of patient 6 was not included due to graft failure
Fig. 1.
A 25-year-old male patient with a left hip femoral head fracture. a Preoperative coronal plane MRI image. b Immediate postoperative AP radiograph. c MRI performed at latest follow-up. Note good sphericity and no evidence of narrowing or collapse of the graft
Surgical technique and postoperative protocol
All operations were performed via a modified trochanteric osteotomy in the lateral decubitus position by one of the surgeons (O.S.) at our institution [15]. The femoral head was dislocated and the osteochondral lesion was identified (Fig. 2a) [10]. The lesion was defined by first removing the centre of defective cartilage followed by removal of the remaining defective cartilage until healthy edges were reached.
Fig. 2.
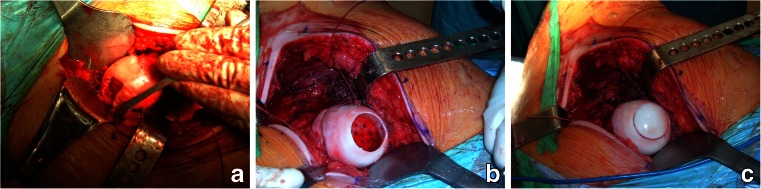
An 18-year-old female patient with an osteochondral defect. a Intra-operative image of the defect. b Intra-operative image of the host bone prepared for the implantation. Note the bleeding bone at the bottom of the defect. c Intra-operative image after tapping in the fresh osteochondral graft
A commercially available system (Arthrex, Naples, FL) was used to prepare the host bone and donor graft for implantation. The host defect was prepared to receive the allograft by creating a cylindrical defect using a power reamer over a guidewire. The reamer was advanced until bleeding bone was reached (Fig. 2b). The host bed was measured for its depth at 12, 3, 6 and 9 o’clock with respect to a reference point chosen during surgery. Next, the matching area was harvested from the donor femoral head using a hollow trephine reamer. The plug height was shaped according to the depth of the host bed dimensions. The osteochondral plug was then placed gently into the defect and tamped into position until the articular surface was flush with the host articular cartilage (Fig. 2c). The hip was reduced and the capsule was closed. The greater trochanter was transfixed with 4.5-mm malleolar screws. After surgery, the patient was allowed to perform toe touch weightbearing for six weeks. Progression to full weight bearing was allowed after healing of the greater trochanter was confirmed radiographically.
Results
The average HHS improved from 57.7 ± 5.1 (range 50–65) points preoperatively to 83.9 ± 6.9 (range 72–94) points at latest follow-up (Table 1). All trochanteric osteotomies were radiographically well healed at six weeks after surgery, and the patients were allowed to bear weight. At latest follow-up, six of the eight patients were fully mobile and did not require a repeated arthroplasty. Five of these six patients had good-to-excellent clinical outcomes, while the remaining patient had a fair outcome [16].
Two patients required a repeat arthroplasty. The first patient (patient #6, Table 1), whose AVN was due to steroids, had progression of her arthritis with increased pain. She was converted to total hip arthroplasty (THA) six months after her femoral osteochondral allograft transplantation. THA was also performed on her contralateral hip, without any attempt to salvage her femoral head due to her prior history with an osteochondral graft. At latest follow-up, 36 months following her hip arthroplasties, the patient is fully mobile and does not require walking aids. The second patient (patient #5, Table 1) did not adhere to the postoperative weight-bearing guidelines and started full weight bearing immediately after surgery. Consequently, the osteochondral graft subsided. Since there was no evidence of joint space narrowing on either the radiographs or on MRI, an additional fresh osteochondral graft was implanted in a similar fashion. He is currently 30 months following the second implantation, and his HHS at latest follow-up was 84 points. One of the six patients who did not have a repeated arthroplasty (patient #1, Table 1) complained of lateral thigh pain which improved substantially after removal of the two screws that were placed to secure the trochanteric osteotomy. Two years after the removal of the screws her HHS at the latest follow-up was 80 points.
No dislocations or superficial or deep infections were encountered in any of the study patients. No clinical signs of femoroacetabular impingement were observed throughout the follow-up period.
Discussion
Osteochondral defects can result from AVN of the femoral head or hip dislocation. They can also occur due to OCD, although only 2 % of all of cases of OCD actually occur at the femoral head [2]. However, unlike OCD of the knee, the lesions of the hip are most often at the weight-bearing dome which, together with the high loading forces across the hip, promote the development of early degenerative changes about the joint [2]. When symptomatic coxarthrosis occurs due to an osteochondral defect in younger patients, both the surgeon and patient face a dilemma [17]. Unlike similar lesions in the knee and ankle, there are no studies which provide evidence that autogenic osteoarticular transfers are successful. The literature does not support the use of other articular surface restoration procedures, such as drilling, owing to poor outcomes [18]. There is only one case report that describes the use of autologous osteoarticular transfer (“mosaicplasty”) for treatment of large articular defects of the femoral head caused by a misplaced reabsorbable screw after fixation of a large acetabular wall fragment. That defect was treated with relative success by using osteoarticular plug transfers from the ipsilateral knee [19]. Technical challenges associated with mosaicplasty of the hip include matching host-site geometry and regional differences in the material properties between the knee and the hip [20]. An additional case report described the use of a fresh-stored osteochondral allograft for treatment of OCD in the weight-bearing area of the femoral head through a trochanteric osteotomy [9]. The patient described in that latter report was pain free and had a good range of motion at the one-year follow-up.
A rotational femoral osteotomy is a viable option since it is a joint-preserving technique and may delay the need for total hip arthroplasty until later. However, it is considered as being major surgery that may involve prolonged recovery and limited success in the treatment of defects at the weight-bearing surface [21–23]. In addition, THA following femoral osteotomy is challenging due to the deformed geometry, and it may entail a higher complication rate due to the previously placed hardware and deformed anatomy [23, 24]. Although THA is the gold standard for pain relief and restoration of function, the concern in young active patients is reduced implant longevity and survivorship compared with arthroplasty performed in the older osteoarthritic population [25–28].
Osteochondral allografts may be a viable option for osteochondral defects since they are associated with a survival rate of 75–85 % at ten years for chondral and osteochondral defects of the femoral condyles or the tibial plateau [7]. It is unclear, however, whether these outcomes can be expected in the hip joint, given that the implantation of the fresh-stored osteochondral grafts around the knee was reported to be systematically accompanied by an offloading varus or valgus osteotomy in those studies [29]. As such, the true effect of an offloading osteotomy is uncertain, since load bearing did have a positive effect on the viability of chondrocytes in a sheep model [30].
We present the preliminary clinical and radiographic outcomes of the treatment of femoral head osteochondral defects by means of fresh-stored osteochondral allografts via a femoral trochanteric osteotomy in eight symptomatic patients. Seven of our eight (87.5 %) study patients did not require total hip arthroplasty at an average follow-up of 41 months. Five of those seven patients had a good-to-excellent HHS and one patient had a fair HHS [16]. The osteochondral allograft subsided in the remaining patient, most probably due to early weight bearing (lack of compliance with instructions), but the joint space was nevertheless preserved, as documented on an MRI. A reimplantation was carried out, and the patient had an HHS of 84 points and was fully mobile at latest follow-up 30 months later. One of the patients had persistent irritation from the screws that were transfixing her trochanteric osteotomy, and these symptoms resolved after the removal of the screws.
Our patient who required conversion to THA had bilateral AVN due to steroid intake. Meyers et al. also found that steroid-induced AVN patients had high failure rates [5]. Thus, we consider that femoral heads with AVN may not be suitable hosts for osteochondral grafts, possibly due to the diffuse metabolic damage, subchondral bone sclerosis and compromised vascularity that can hinder osteointegration of the graft [31].
The limitations of the study are the relatively short follow-up and small number of patients in the series. Since this is the first series reporting this mode of treatment, however, we wanted to share our preliminary experience with our colleagues, especially since the results were promising, with seven of the eight patients in this study having had no progression of the degenerative process in their hips.
Conclusion
Seven of our eight symptomatic patients that were treated for femoral head osteochondral defects by means of fresh-stored osteochondral allografts via a trochanteric osteotomy and did not require conversion to THA after an average follow-up of 3.5 years. Based on that experience, we contend that fresh-stored osteochondral allograft transplantation using a trochanteric slide and surgical dislocation is a viable treatment option for femoral head defects in young patients. The patients who are not likely to comply with a restricted weight-bearing protocol and those with steroid-induced AVN may not be appropriate candidates for this surgical approach. The osteochondral allograft procedure described in our study provides the opportunity to retain viable hyaline cartilage for the repair of osteochondral lesions in the femoral head while restoring joint congruity and possibly reducing the risk of coxarthrosis. Longer follow-up on a larger group of patients is required to establish the efficacy of this treatment modality.
Acknowledgments
Conflict of interest
None on the part of any author.
Contributor Information
Yona Kosashvili, Phone: +972-50-4065320, FAX: +972-3-9376156, Email: yonasofi@gmail.com.
Guy Raz, Email: drguyraz@yahoo.com.
David Backstein, Email: david.backstein@utoronto.ca.
Oren Ben Lulu, Email: benluluoren@gmail.com.
Allan E. Gross, Email: Allan.gross@utoronto.ca
Oleg Safir, Email: olegsafir@gmail.com.
References
- 1.Tannast M, Krüger A, Mack PW, et al. Surgical dislocation of the hip for the fixation of acetabular fractures. J Bone Joint Surg Br. 2010;92:842–852. doi: 10.1302/0301-620X.92B6.22994. [DOI] [PubMed] [Google Scholar]
- 2.Lindholm TS, Osterman K, Vankka E. Osteochondritis dissecans of elbow, ankle and hip: a comparison survey. Clin Orthop Relat Res. 1980;148:245–253. [PubMed] [Google Scholar]
- 3.Buckwalter JA. Evaluating methods of restoring cartilaginous articular surfaces. Clin Orthop Relat Res. 1999;367:S224–S238. doi: 10.1097/00003086-199910001-00022. [DOI] [PubMed] [Google Scholar]
- 4.O'Driscoll SW. The healing and regeneration of articular cartilage. J Bone Joint Surg Am. 1998;80:1795–1812. [PubMed] [Google Scholar]
- 5.Meyers MH, Jones RE, Bucholz RW, et al. Fresh autogenous grafts and osteochondral allografts for the treatment of segmental collapse in osteonecrosis of the hip. Clin Orthop Relat Res. 1983;174:107–112. [PubMed] [Google Scholar]
- 6.LaPrade RF, Botker J, Herzog M, et al. Refrigerated osteoarticular allografts to treat articular cartilage defects of the femoral condyles. A prospective outcomes study. Bone Joint Surg Am. 2009;91:805–811. doi: 10.2106/JBJS.H.00703. [DOI] [PubMed] [Google Scholar]
- 7.Gross AE, Shasha N, Aubin P. Long-term followup of the use of fresh osteochondral allografts for posttraumatic knee defects. Clin Orthop Relat Res. 2005;435:79–87. doi: 10.1097/01.blo.0000165845.21735.05. [DOI] [PubMed] [Google Scholar]
- 8.Jeng CL, Kadakia A, White KL, et al. Fresh osteochondral total ankle allograft transplantation for the treatment of ankle arthritis. Foot Ankle Int. 2008;29:554–560. doi: 10.3113/FAI.2008.0554. [DOI] [PubMed] [Google Scholar]
- 9.Evans KN, Providence BC. Case report: fresh-stored osteochondral allograft for treatment of osteochondritis dissecans the femoral head. Clin Orthop Relat Res. 2010;468:613–618. doi: 10.1007/s11999-009-0997-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Espinosa N, Beck M, Rothenfluh DA. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. Surgical technique. J Bone Joint Surg Am. 2007;89:36–53. doi: 10.2106/JBJS.F.01123. [DOI] [PubMed] [Google Scholar]
- 11.Clanton TO, DeLee JC. Osteochondritis dissecans. History, pathophysiology and current treatment concepts. Clin Orthop Relat Res. 1982;167:50–64. [PubMed] [Google Scholar]
- 12.Jacobs NJ (1987) Establishing a surgical bone bank. In: Tissue banking. Fawcett K (ed). American Association of Blood Banks, Arlington, VA, pp 67–96
- 13.Davidson PA, Rivenburgh DW, Dawson PE, et al. Clinical, histologic, and radiographic outcomes of distal femoral resurfacing with hypothermically stored osteoarticular allografts. Am J Sports Med. 2007;35:1082–1090. doi: 10.1177/0363546507299529. [DOI] [PubMed] [Google Scholar]
- 14.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 15.Lakstein D, Backstein DJ, Safir O, et al. Modified trochanteric slide for complex hip arthroplasty: clinical outcomes and complication rates. J Arthroplasty. 2010;25:363–368. doi: 10.1016/j.arth.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 16.Marchetti P, Binazzi R, Vaccari V, et al. Long-term results with cementless Fitek (or Fitmore) cups. J Arthroplasty. 2005;20:730–737. doi: 10.1016/j.arth.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Sierra RJ, Trousdale RT, Ganz R, et al. Hip disease in the young, active patient: evaluation and nonarthroplasty surgical options. J Am Acad Orthop Surg. 2008;16:689–703. doi: 10.5435/00124635-200812000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Lindén B, Jonsson K, Redlund-Johnell I. Osteochondritis dissecans of the hip. Acta Radiol. 2003;44:67–71. doi: 10.1034/j.1600-0455.2003.00020.x. [DOI] [PubMed] [Google Scholar]
- 19.Hart R, Janecek M, Visna P, et al. Mosaicplasty for the treatment of femoral head defect after incorrect resorbable screw insertion. Arthroscopy. 2003;19:E1–E5. doi: 10.1016/S0749-8063(03)00377-3. [DOI] [PubMed] [Google Scholar]
- 20.Bugbee WD. Fresh osteochondral allografts. J Knee Surg. 2002;15:191–195. [PubMed] [Google Scholar]
- 21.Belal MA, Reichelt A. Clinical results of rotational osteotomy for treatment of avascular necrosis of the femoral head. Arch Orthop Trauma Surg. 1996;115:80–84. doi: 10.1007/BF00573446. [DOI] [PubMed] [Google Scholar]
- 22.Rijnen WH, Lameijn N, Schreurs BW et al (2009) Total hip arthroplasty after failed treatment for osteonecrosis of the femoral head. Orthop Clin North Am 40:291–8 [DOI] [PubMed]
- 23.Schneider W, Aigner N, Pinggera O. Intertrochanteric osteotomy for avascular necrosis of the head of the femur. Survival probability of two different methods. J Bone Joint Surg Br. 2002;84:817–824. doi: 10.1302/0301-620X.84B6.12837. [DOI] [PubMed] [Google Scholar]
- 24.Kawasaki M, Hasegawa Y, Sakano S, et al. Total hip arthroplasty after failed transtrochanteric rotational osteotomy for avascular necrosis of the femoral head. J Arthroplasty. 2005;20:574–579. doi: 10.1016/j.arth.2005.01.018. [DOI] [PubMed] [Google Scholar]
- 25.Springer BD, Connelly SE, Odum SM, et al. Cementless femoral components in young patients: review and meta-analysis of total hip arthroplasty and hip resurfacing. J Arthroplasty. 2009;24:2–8. doi: 10.1016/j.arth.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 26.Clohisy JC, Oryhon JM, Seyler TM, et al. Function and fixation of total hip arthroplasty in patients 25 years of age or younger. Clin Orthop Relat Res. 2010;468:3207–3213. doi: 10.1007/s11999-010-1468-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramaswamy R, Kosashvili Y, Cameron H. Total hip replacement in patients with multiple epiphyseal dysplasia with a mean follow-up of 15 years and survival analysis. J Bone Joint Surg Br. 2010;92:489–495. doi: 10.1302/0301-620X.92B4.22897. [DOI] [PubMed] [Google Scholar]
- 28.Kosashvili Y, Taylor D, Backstein D, et al. Total hip arthroplasty in patients with Down's syndrome. Int Orthop. 2010;35:661–666. doi: 10.1007/s00264-010-1030-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shasha N, Krywulak S, Backstein D, et al. Long-term follow-up of fresh tibial osteochondral allografts for failed tibial plateau fractures. J Bone Joint Surg Am. 2003;85-A:33–39. doi: 10.2106/00004623-200300002-00005. [DOI] [PubMed] [Google Scholar]
- 30.Gole MD, Poulsen D, Marzo JM, et al. Chondrocyte viability in press-fit cryopreserved osteochondral allografts. J Orthop Res. 2004;22:781–787. doi: 10.1016/j.orthres.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Ma HZ, Zeng BF, Li XL. Upregulation of VEGF in subchondral bone of necrotic femoral heads in rabbits with use of extracorporeal shock waves. Calcif Tissue Int. 2007;81:124–131. doi: 10.1007/s00223-007-9046-9. [DOI] [PubMed] [Google Scholar]