Abstract
Purpose
We carried out this study to test the efficacy of the olecranon memory connector (OMC) in olecranon fractures.
Methods
We designed a prospective randomised controlled trial involving 40 cases of olecranon fractures. From May 2004 to December 2009, 40 patients with olecranon fractures were randomly assigned into two groups. Twenty patients were treated with OMC, while another 20 patients were fixed with locking plates in our hospital. The DASH score, MEP score, range of motion and radiographs were used to evaluate the postoperative elbow function and complications.
Results
For MEP score, OMC was better than the locking plate; for DASH score, complication rate, and range of elbow motion, the two methods presented no significant difference.
Conclusion
The study showed that OMC could be an effective alternative to treat olecranon fractures.
Introduction
Olecranon fractures are a common upper extremity injury, accounting for approximately 10 % [1, 2] of all fractures around the elbow. Various treatment methods for olecranon fractures can be employed to recover the elbow function and reconstruct the anatomical structure. During past decades, internal fixation for olecranon fractures has been greatly improved, including Kirschner wires, tension-band wiring, plate fixation and intramedullary screws and nailing systems [3–6]. Kirschner wires and tension-band wiring are the common methods. However, in some cases with Kirschner wires [7], the authors have described impaired forearm rotation with normal flexion and extension of the elbow due to the damage of the ulnar cortex or soft tissues. In addition, Kirschner wires perforating the anterior ulnar cortex may result in radioulnar synostosis [8]. Probably, the mechanism is the calcification of the haematoma produced by the soft tissue when Kirschner wires pass through the interosseus membrane and its surroundings [9, 10]. The most common complication of the tension-band wiring is pin protrusion leading to pain and skin irritation [11]. Furthermore, tension-banding wiring usually needs to be removed due to discomfort. Romero et al. [12] reported that 67.4 % of all patients demanded removal of the tension-band wiring.
Ni-Ti alloy is well known for its shape memory, wear resistance, corrosion resistance and biocompatibility. It was first approved for clinical application in 1990s by the FDA. As a major biomaterial innovation, it leads to significant improvement of clinical treatment. Before this study, we had designed Ni-Ti memory alloy swan-like bone connector to treat 156 patients with humeral shaft nonunion, in which the recovery rate was 98.7 % [13]. For olecranon fractures, the olecranon memory connector(OMC) was designed based on the anatomical structure of the olecranon and has been studied for its efficacy in the treatment of olecranon fractures.
Patients and methods
A prospective randomised controlled trial was designed to compare the therapeutic effects of OMC and locking plates. This study was authorised by the hospital ethics committee. The patients included all signed informed consent documents in the presence of a third party.
A total of 40 patients were enrolled in the study according to the inclusion and exclusion criteria (Table 1). All 40 patients with different types of olecranon fractures were randomly divided into the OMC group(20 cases) and the locking plate group(20 cases) in Changhai Hospital between May 2004 and December 2009 (Table 2). Patients in the first group were treated with OMC while the second group received locking plate fixation, which was regarded as the control group. All reviewers were blinded to evaluate the postoperative function by means of a randomised block design.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Mayo type II and type III olecranon fracture | Mayo type I olecranon fracture |
| transverse or slight oblique olecranon fracture | Non-traumatic fracture |
| Fresh closed olecranon fracture | Serious comminuted fracture |
| Stable vital signs | Old olecranon fracture |
| Psychological and/social conditions with poor compliance |
Table 2.
Patients demographics, fracture classification
| Variables | OMC group | Locking plate group |
|---|---|---|
| N = 20 | N = 20 | |
| Age, years | 47.85 ± 17.6 | 48.9 ± 15.5 |
| (21–77) | (28–64) | |
| Sex, males/females | 12/8 | 10/10 |
| Mayo classification, type II/type III | 13/7 | 14/6 |
| Follow-up time, months | 36.5 ± 7.4 | 36.6 ± 9.3 |
Data presented as mean values ± SD . No statistically significant between-group differences
The follow-up took eight years from January 2004 to January 2012. The average length of follow up was 3.2 years (range two to five years) with no loss of follow-up. In the OMC group, 12 (60 %) were men with an average age of 50.6 years (range, 31–77) and eight were women with an average age of 48.9 (range, 21–64). Of the 20 cases, ten (50 %) were the left olecranon and the rest were right olecranon. In the locking plate group, ten (50 %) were men with a mean age of 49 years (range, 28–64), and ten (50 %) were women with a mean age of 48.8 years (range, 37–60). Of the 20 cases, 11 (55 %) injured the right olecranon and nine (45 %) the left olecranon. The main cause of the fractures in both groups was a fall. In the OMC group, 11 (55 %) were due to a fall, six (30 %) were due to traffic accidents, two (10 %) resulted from falling objects and one (5 %) was attributable to sports injury. Fractures included ten (50 %) IIA type, four (20 %) IIB type, four (20 %) IIIA type and two (10 %) IIIB type. In the locking plate group, 12 (60 %) fractures were due to a fall, seven (35 %) resulted from traffic accidents and one (5 %) was attributable to sports injury. Fractures included nine (45 %) IIA type, six (30 %) IIB type, four (20 %) IIIA type and one (5 %) IIIB type. All of the patients were operated upon and given antibiotics after surgery (Table 2).
Structure and working principles of the OMC
The OMC was designed on the basis of the anatomical structure of the olecranon and manufactured from 1.8–2.5 mm thick Ni-Ti shape memory alloy plate (Ni 50–53 %). The OMC is composed of a intramedullary fixing lock, a base arc and two compression fixing arms (Fig. 1). Depending on material properties, the memory direction of OMC is set as a one way memory in order to obtain the largest memory kinetic energy. The transition temperature is set between 28 °C and 33 °C, so that memory kinetic energy and elastic force are produced in during transition from plastic deformation phase in low temperature (martensite phase) to previous shape in high temperature (austenite phase), which can continuously provide lateral compressive force. The mechanical features are as follows: density: 6.5 g/cm3, tension intensity: 1,000–1,300 MPa, fatigue intensity: 550 MPa. Biomechanical evaluation using a strain gauge patch method on a cadaveric ulna showed that the active pressure was 7.49 kg.
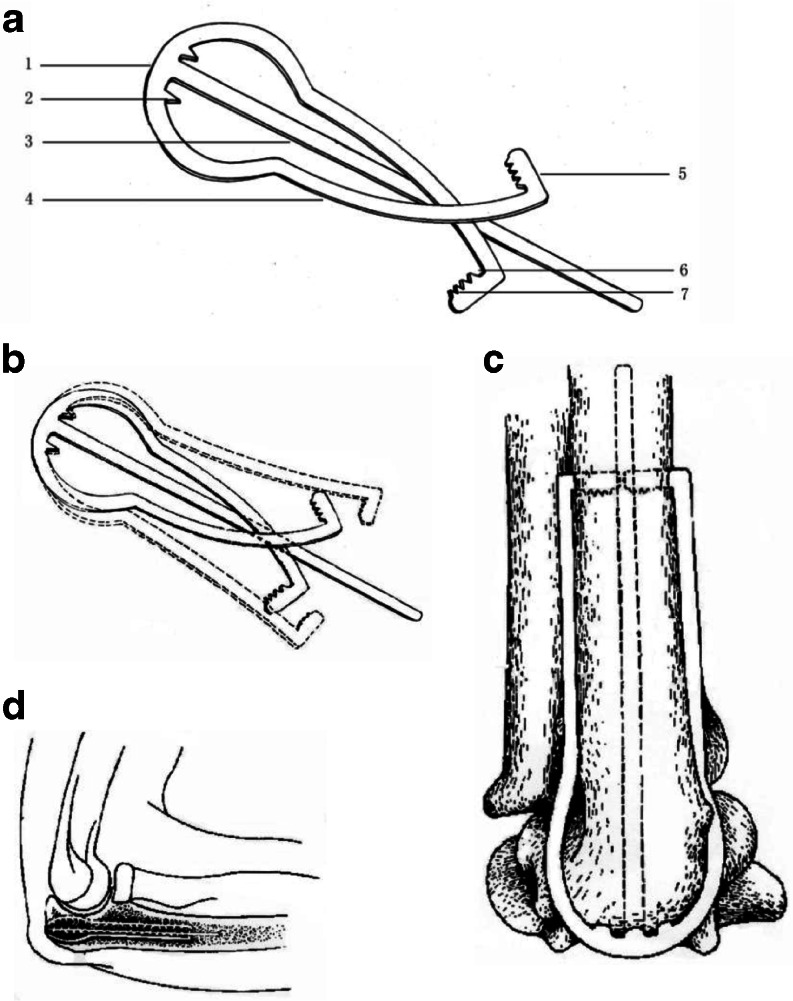
Fig. 1.
Structures of the OMC (a) A view of the OMC (1. a base arc 2. fixing tips 3. a intramedullary fixing lock 4. compression fixing arms 5. head hooks 6. angle between a head hook and a compression fixing arm 7. tips of a head hook). b extension of compression fixing arms (c) An anterior view of the OMC molded to the olecranon (d) A lateral draft of the OMC molded to the olecranon
The OMC was cooled with ice for two to four minutes before implantation. A hole was drilled at the tip of olecranon, where the intramedullary fixing lock was inserted parallel to the ulnar. Then two holes were drilled at the ulnar diaphysis with a hole on each side, consistent with the head hook of the compression fixing arm. The OMC was fixed to the olecranon automatically with warm water after inserting the head hooks into the ulnar diaphysis.
Surgical procedure for the locking plate
A dorsal incision was made over the olecranon. The ulnar nerve was protected and various fracture fragments were carefully examined. The fracture reduction was achieved by hinging the proximal olecranon fragment on its triceps attachment and scar tissues and necrotic bone debris were cleared. A clamp was placed around the tip of the olecranon and the Kirschner wire was used to temporarily maintain the reduction. After reduction, a locking plate was used to fit the tip of the olecranon. Drills were screwed onto the plate to help fixing. Then screws were used to achieve a stable mechanical structure. After fixation, the elbow was gently moved to make sure that the locking plate was firmly fixed to the olecranon.
For OMC, a posterolateral approach was adopted. To avoid the ulnar nerve located at the medial of the ulna, the incision was at its lateral side. The ulnar nerve was exposed during surgery. After clearance of the scar tissues and the necrotic bone debris, the articular cavity was cleared and the olecranon was repositioned using Kirschner wires. Then the base arc and compression fixing arms were prepared with ice. The placement of the intramedullary fixing lock is described above. With the base arc and compression fixing arms parallel to the ulna, the fixing tips of the base arc were embedded into the olecranon. Head hooks were inserted into the ulnar diaphysis into the previously holes (Fig. 2). After the OMC warming to cause recovery of the preset shape, fixing conditions were examined by moving the elbow.
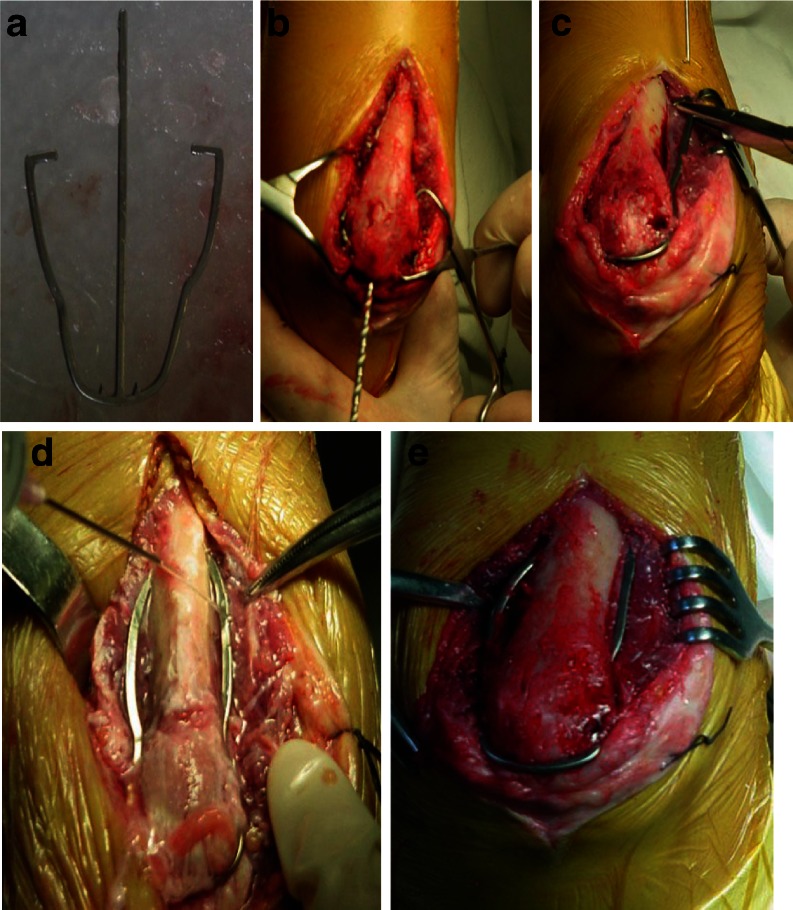
Fig. 2.
Implantation of the OMC (a) The OMC was cooled with ice for extension of compression fixing arms. b A hole was drilled at the tip of olecranon. c Intramedullary fixing lock was inserted through the hole parallel to the long axis of the ulna and compression fixing arms were molded to the olecranon. d Head hooks were inserted into the ulnar diaphysis through holes whose positions were in consistent with those of head hooks. e The OMC was warmed to cause shape memory effect
Clinical outcome evaluation
Patients were immobilised after the surgery and rehabilitation of gentle elbow flexion and extension started two weeks postoperatively. At two weeks and one, two, three, six, 12 and 24 months after OMC implantation, radiographs of the elbow were taken to examine healing and the disability of the arm, shoulder, and hand (DASH) score and the Mayo elbow performance (MEO) score were used to evaluate the elbow joint function. For MEP, the score is considered excellent at over 90 points, good between 75 and 89, fair between 60 and 74 and poor less than 60 points. A higher score indicates more severe disability for DASH score. Student's t test was applied to compare the two groups with p < 0.05 regarded as statistically significant. All clinical assessment in this research was accomplished by independent observers. The results were interpreted independently by two authors(Xiao Chen and Liehu Cao).
Statistical analysis
The statistical analysis was performed with SPSS 12.0 (SPSS Inc., Chicago, IL, USA). For the treatment result, differences between the two groups were compared by t test or chi-square test. Data were presented as mean ± SD. In all cases, a p value of 0.05 was assumed to denote statistical significance.
Results
Of the patients in the OMC group, 17 (85 %) were very satisfied with outcomes and three (15 %) were satisfied with outcomes. In the locking plate group, 17 (85 %) were quite satisfied with outcomes, two (10 %) were satisfied with outcomes and one (5 %) was dissatisfied with the outcome, having suffered from superficial infection after the surgery and pain during rehabilitation.
The mean follow-up of the OMC group was 36.6 months (range, 24–53 months) and that of the locking plate group was 36.7 months (range, 25–56 months). During the follow-up, no infection, nonunion, avascular necrosis or any complications related to the implant occurred in the OMC group while only one patient developed superficial infection in the locking plate group.
DASH score and MEP score were used to evaluate functional recovery of the elbow. In the OMC group, the mean DASH score was 3.3 and it was 4.0 in the locking plate group (p = 0.38). For MEP score, in the OMC group, ten patients (50 %) had an excellent outcome, seven (35 %) had a good outcome and three (15 %) had a fair outcome. Of the patients in the locking plate group, five (25 %) had an excellent outcome, ten (50 %) had a good outcome, four (20 %) had a fair outcome and one (5 %) had a poor outcome. The mean MEP score of the OMC group and the locking plate group were 86.6 and 79.8 points, respectively (p < 0.05). (Table 3)
Table 3.
Comparison of DASH score, MEP score, complications and elbow functions
| Variables | OMC | Locking plate |
|---|---|---|
| DASH scores | 3.3 ± 4.0 | 4.0 ± 6.9 |
| MEP scores | 86.7 ± 12.5* | 79.8 ± 12.3 |
| Elbow function | ||
| Excellent | 10* | 5 |
| Good | 7 | 10 |
| Fair | 3 | 4 |
| Poor | 0 | 1 |
| Very satisfied | 17 | 17 |
| Satisfied | 3 | 2 |
| Dissatisfied | 0 | 1 |
| Complications | 0 | 1 |
Data presented as mean values ± SD. *p < 0.05 OMC group vs. Locking plate group
In the OMC group, the average flexion range was 137.7 ± 4.2° and the mean range of extension was 3.5 ± 1.8°. The average rotation range was 165.0 ± 5.0° with a mean pronation range of 82.6 ± 2.6° and a mean supination range of 82.4 ± 2.4°. In the locking plate group, the average range of flexion was 136.6 ± 5.1° and the mean range of extension was 2.9 ± 1.9°. The average rotation of was 163.4 ± 7.3° with a mean pronation range of 81.5 ± 3.8° and a mean supination range of 81.9 ± 3.5°. No significant differences were found in the range of motion after comparing the two groups. (Table 4)
Table 4.
Follow-up elbow function evaluations
| Group | Flexion (°) | Extension (°) | Pronation (°) | Supination (°) |
|---|---|---|---|---|
| OMC | 137.7 ± 4.2 | 3.5 ± 1.8 | 82.6 ± 2.6 | 82.4 ± 2.4 |
| Locking plate | 136.6 ± 5.1 | 2.9 ± 1.9 | 81.5 ± 3.8 | 81.9 ± 3.5 |
Data presented as mean values ± SD. No statistically significant between-group differences
Typical case
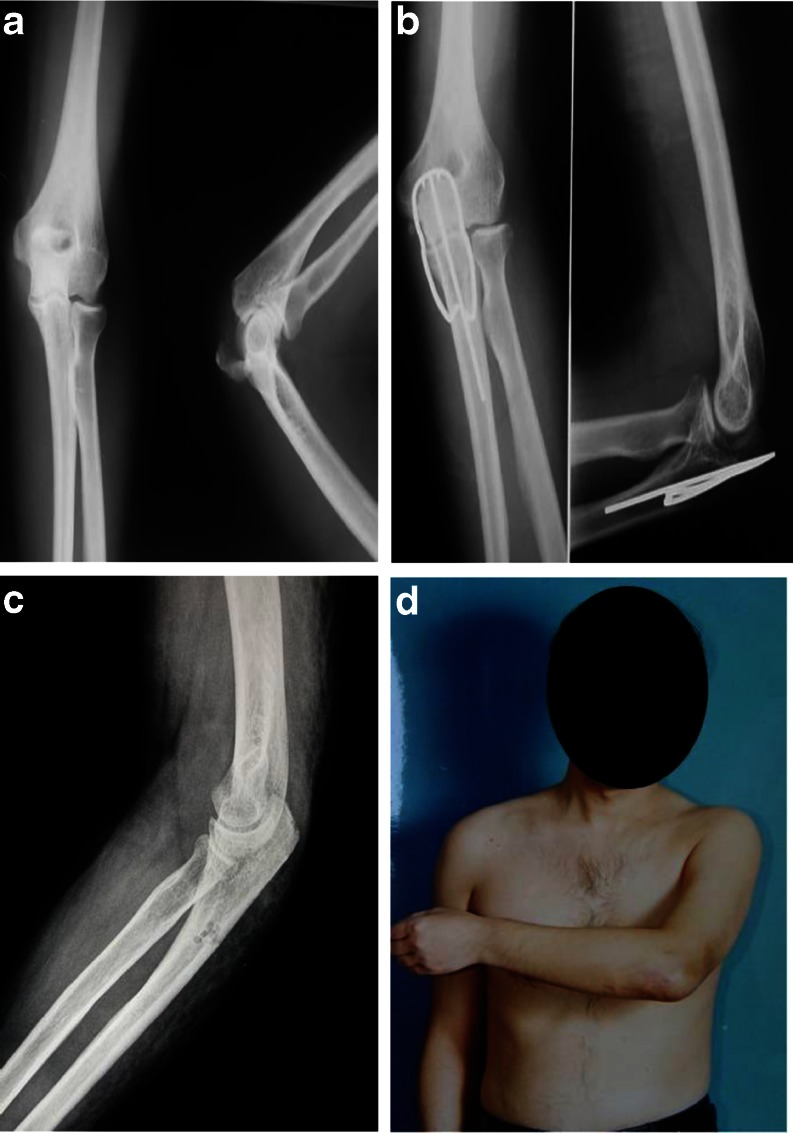
A 34-year-old man sustained olecranon fractures (type IIA) in the left upper limb due to falling. The patient underwent an operation with OMC implantation two days after admission. The radiographs taken 12 months later revealed fractures healing well and no abnormal ossification emerging at the olecranon. The patient was followed up for 30 months with satisfactory rehabilitation of function of the elbow joint. The DASH and MEP score was 1 and 100 respectively. The range of flexion and extension was 143° and 6° respectively (Fig. 3).
Fig. 3.
Typical case (a) A 34-year-old man had olecranon fractures. b The patient was treated with the OMC and radiographs were taken twelve months after implantation. No abnormal ossification was noted. c The olecranon fracture healed well after removal of the OMC. d The elbow function was excellent
Discussion
In this study, we compared two different treatment methods for olecranon fracture and demonstrated that OMC was better than the locking plate as for MEP score and these two treatments presented no significant difference with respect to DASH score, complication rate and range of elbow motion. It can be concluded that OMC could be an effective alternative to treat olecranon fractures in clinical practice which is worth publishing.
The most common operative method for treating Mayo type II and type III olecranon fractures is open reduction and internal fixation (ORIF). Of all metallic implants, the most frequently used are Kirschner wires, tension band-wiring, intramedullary screws and nailing systems and plate fixing. Tension-banding wiring as first described by Weber and Vasey in 1963 was used along with Kirschner wires or alone in certain conditions [14]. Villaneuva et al. [15] reviewed 37 patients with olecranon fractures treated with tension-banding wiring. 89 % of patients had no pain or mild pain 4-years postoperatively and 86 had good or excellent MEP scores with average motion range of 124°. When correctly performed, tension band wiring allows less soft-tissue stripping, does not result in synostosis (unless the k-wires are inadequately placed), allows immediate postoperative gentle motion, and is cost effective. Nevertheless, the most obvious disadvantage is high removal rate due to discomfort. Larsen et al. [16] reported that the removal rate was 70 % in treatment with tension-band wiring and a modification of the Netz pin. Several studies [17] have reported that Kirschner wires caused the most common complications of tension-band wiring. The position of placement of Kirschner wires is still controversial. Intramedullary Kirschner wires may cause pain and pressure on soft tissues and skin irritation [18]. When Kirschner wires penetrate the anterior cortex, they require approximately twice the force of intramedullary K-wires to “pull out” [19]. However, some studies have shown that restriction of forearm rotation might result from Kirschner wires penetrating the anterior cortex due to impingement of the radial neck, the supinator or the biceps insertion [7]. In addition, the median nerve and ulnar artery were the most vulnerable structures to Kirschner wires penetration according to Prayson et al. [19]. The beneficial effects of surgery are compromised in up to 10 % of cases, due to postoperative complications associated with tension band wiring, such as infection, nonunion, malunion and ulnar nerve palsy [12, 20].
Intramedullary screws and nailing systems are another method with quite good outcomes [21]. Some biomechanical studies have demonstrated that there is significant variability regarding fixing length of intramedullary screws [22] and an analysis indicated that intramedullary screw was inferior to AO tension band, screw and wire [6]. Anderson et al. [23]. tried using plate fixation using a precontoured locking plate. He concluded that it was a safe option permitting early movement.
Locking plate is also a popular treatment method for comminuted olecranon fractures. More unstable fractures that are comminuted or extend distally from the centre of the trochlear notch require more rigid fixation. And locking plate is a popular treatment for comminuted olecranon fractures [24]. Locking plates possess the advantages of superior fixation and studies have shown that the locking plate fixation has excellent outcomes [18, 25]. Buijze et al. [26] reported that in the treatment of comminuted olecranon fractures, a contoured locking compression plate combined with an intramedullary screw could provide sufficient stability for early postoperative functional rehabilitation, with an excellent fracture union rate and very good clinical outcomes. However, irritation has been a common complication that often requires a secondary procedure for removal, with rates ranging between 20 % and 100 % [18, 25].
Ni-Ti shape memory alloy possesses excellent properties of wear and corrosion resistance and good biocompatibility. Su et al. [13] designed a swan-like memory pressure connector in treating humeral shaft nonunion, in which the recovery rate was 98.7 % demonstrating good efficacy. With gradual advancement of shape memory alloy, it is playing a prominent part in treating injury or trauma [27]. Compression of traditional internal fixing is sometimes discontinuous, passive and static. When absorption of fracture lines occurs, compression will disappear, which will easily result in nonunion [28]. Due to Ni-Ti shape memory alloy, the OMC possesses the following advantages: (1) Kirschner wires, tension-band wiring, plate or intramedullary screws will occupy more space at the olecranon. However, due to thin skin and limited space at the olecranon, these implants may lead to skin irritation, whereas the OMC occupies less space after implantation, thus hardly causing skin irritation. (2) Given less occupied space, it should not cause pain, which will decrease the removal rate. (3) The surgical procedure is quite simple. Only two towel forceps for stabilisation and an electric drill are needed. (4) Pressure which derives from compression fixing arms of the OMC is continuous, active and dynamic. As a result, it is beneficial for fracture healing. (5) The OMC is manufactured with Ni-Ti shape memory alloy. So it molds well to the olecranon after it is cathed with warm water. (6) Implantation of the OMC is quite convenient because it itself can produce sufficient force to stabilise the fracture without any further management after implantation. Removal is also easy. (7) The Ni-Ti shape memory alloy is biologically friendly [29].
In general, the advantages can be concluded as a simple procedure, stable fixation, continuous pressure, allowing early movement and training, less complications and easy removal. The prominent disadvantage is significant soft tissue dissection which did not have significant influence on postoperative recovery as shown in the results. Based on our experience, the indications include olecranon transverse fracture, comminuted olecranon fracture, open olecranon fracture and olecranon non-union. The contraindication is severe comminuted proximal olecranon fracture too difficult to stabilise. No obvious complications were found in clinical practice.
This prospective randomised controlled trial showed that the OMC has the same treatment efficacy as the locking plate. There was no significant difference in the DASH score and elbow function evaluation. And for MEP score, OMC was superior to locking plate.
In conclusion, our study showed that the recovery with the OMC is very satisfactory with no complications. Hence, the efficacy of the OMC has been proved by good clinical outcomes and the study indicates that the OMC is an alternative and effective treatment for olecranon fractures other than Kirschner wires, tension-band wiring and locking plates.
Acknowledgments
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Xiao Chen, Peng Liu and Xiaofei Zhu contributed equally to this work.
This study was authorized by the hospital ethics committee. The patients included all signed informed consent documents with the presence of a third party.
References
- 1.Rommens PM, Kuchle R, Schneider RU, Reuter M. Olecranon fractures in adults: factors influencing outcome. Injury. 2004;35:1149–1157. doi: 10.1016/j.injury.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Veillette CJ, Steinmann SP. Olecranon fractures. Orthop Clin N Am. 2008;39:229–236. doi: 10.1016/j.ocl.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Gordon MJ, Budoff JE, Yeh ML, Luo ZP, Noble PC. Comminuted olecranon fractures: a comparison of plating methods. J Shoulder Elbow Surg. 2006;15:94–99. doi: 10.1016/j.jse.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Karlsson MK, Hasserius R, Besjakov J, Karlsson C, Josefsson PO. Comparison of tension-band and figure-of-eight wiring techniques for treatment of olecranon fractures. J Shoulder Elbow Surg. 2002;11:377–382. doi: 10.1067/mse.2002.124548. [DOI] [PubMed] [Google Scholar]
- 5.Kloen P, Buijze GA. Treatment of proximal ulna and olecranon fractures by dorsal plating. Oper Orthop Traumatol. 2009;21:571–585. doi: 10.1007/s00064-009-2006-y. [DOI] [PubMed] [Google Scholar]
- 6.Murphy DF, Greene WB, Gilbert JA, Dameron TB, Jr (1987) Displaced olecranon fractures in adults. Biomechanical analysis of fixation methods. Clin Orthop Relat Res 210–214 [PubMed]
- 7.Candal-Couto JJ, Williams JR, Sanderson PL. Impaired forearm rotation after tension-band-wiring fixation of olecranon fractures: evaluation of the transcortical K-wire technique. J Orthop Trauma. 2005;19:480–482. doi: 10.1097/01.bot.0000164338.79013.10. [DOI] [PubMed] [Google Scholar]
- 8.De Carli P, Gallucci GL, Donndorff AG, Boretto JG, Alfie VA. Proximal radio-ulnar synostosis and nonunion after olecranon fracture tension-band wiring: a case report. J Shoulder Elbow Surg. 2009;18:e40–e44. doi: 10.1016/j.jse.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Failla JM, Amadio PC, Morrey BF. Post-traumatic proximal radio-ulnar synostosis. Results of surgical treatment. J Bone Joint Surg Am. 1989;71:1208–1213. [PubMed] [Google Scholar]
- 10.Finsen V, Lingaas PS, Storro S. AO tension-band osteosynthesis of displaced olecranon fractures. Orthopedics. 2000;23:1069–1072. doi: 10.3928/0147-7447-20001001-18. [DOI] [PubMed] [Google Scholar]
- 11.Hutchinson DT, Horwitz DS, Ha G, Thomas CW, Bachus KN. Cyclic loading of olecranon fracture fixation constructs. J Bone Joint Surg Am. 2003;85-A:831–837. doi: 10.2106/00004623-200305000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Romero JM, Miran A, Jensen CH. Complications and re-operation rate after tension-band wiring of olecranon fractures. J Orthop Sci. 2000;5:318–320. doi: 10.1007/s007760070036. [DOI] [PubMed] [Google Scholar]
- 13.Su JC, Liu XW, Yu BQ, Li ZD, Li M, Zhang CC. Shape memory Ni-Ti alloy swan-like bone connector for treatment of humeral shaft nonunion. Int Orthop. 2010;34:369–375. doi: 10.1007/s00264-009-0726-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weber BG, Vasey H. Osteosynthesis in olecranon fractures. Z Unfallmed Berufskr. 1963;56:90–96. [PubMed] [Google Scholar]
- 15.Villanueva P, Osorio F, Commessatti M, Sanchez-Sotelo J. Tension-band wiring for olecranon fractures: analysis of risk factors for failure. J Shoulder Elbow Surg. 2006;15:351–356. doi: 10.1016/j.jse.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 16.Larsen E, Jensen CM. Tension-band wiring of olecranon fractures with nonsliding pins. Report of 20 cases. Acta Orthop Scand. 1991;62:360–362. doi: 10.3109/17453679108994470. [DOI] [PubMed] [Google Scholar]
- 17.Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am. 1985;67:1396–1401. [PubMed] [Google Scholar]
- 18.Bailey CS, MacDermid J, Patterson SD, King GJ. Outcome of plate fixation of olecranon fractures. J Orthop Trauma. 2001;15:542–548. doi: 10.1097/00005131-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Prayson MJ, Iossi MF, Buchalter D, Vogt M, Towers J. Safe zone for anterior cortical perforation of the ulna during tension-band wire fixation: a magnetic resonance imaging analysis. J Shoulder Elbow Surg. 2008;17:121–125. doi: 10.1016/j.jse.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 20.Parker JR, Conroy J, Campbell DA. Anterior interosseus nerve injury following tension band wiring of the olecranon. Injury. 2005;36:1252–1253. doi: 10.1016/j.injury.2004.12.028. [DOI] [PubMed] [Google Scholar]
- 21.Gehr J, Friedl W. Intramedullary locking compression nail for the treatment of an olecranon fracture. Oper Orthop Traumatol. 2006;18:199–213. doi: 10.1007/s00064-006-1171-5. [DOI] [PubMed] [Google Scholar]
- 22.Fyfe IS, Mossad MM, Holdsworth BJ. Methods of fixation of olecranon fractures. An experimental mechanical study. J Bone Joint Surg Br. 1985;67:367–372. doi: 10.1302/0301-620X.67B3.3997942. [DOI] [PubMed] [Google Scholar]
- 23.Anderson ML, Larson AN, Merten SM, Steinmann SP. Congruent elbow plate fixation of olecranon fractures. J Orthop Trauma. 2007;21:386–393. doi: 10.1097/BOT.0b013e3180ce831e. [DOI] [PubMed] [Google Scholar]
- 24.Argintar E, Martin BD, Singer A, Hsieh AH, Edwards S. A biomechanical comparison of multidirectional nail and locking plate fixation in unstable olecranon fractures. J Shoulder Elbow Surg. 2012;21:1398–1405. doi: 10.1016/j.jse.2011.08.068. [DOI] [PubMed] [Google Scholar]
- 25.Lindenhovius AL, Brouwer KM, Doornberg JN, Ring DC, Kloen P. Long-term outcome of operatively treated fracture-dislocations of the olecranon. J Orthop Trauma. 2008;22:325–331. doi: 10.1097/BOT.0b013e31817283f7. [DOI] [PubMed] [Google Scholar]
- 26.Buijze G, Kloen P. Clinical evaluation of locking compression plate fixation for comminuted olecranon fractures. J Bone Joint Surg Am. 2009;91:2416–2420. doi: 10.2106/JBJS.H.01419. [DOI] [PubMed] [Google Scholar]
- 27.Levi DS, Kusnezov N, Carman GP. Smart materials applications for pediatric cardiovascular devices. Pediatr Res. 2008;63:552–558. doi: 10.1203/PDR.0b013e31816a9d18. [DOI] [PubMed] [Google Scholar]
- 28.Morrey BF. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instr Course Lect. 1995;44:175–185. [PubMed] [Google Scholar]
- 29.Li Q, Zeng Y, Tang X The applications and research progresses of nickel-titanium shape memory alloy in reconstructive surgery. Australas Phys Eng Sci Med 33:129–136. doi:10.1007/s13246-010-0022-8 [DOI] [PubMed]