Abstract
Purpose
Accurate orientation of acetabular and femoral components are important during THA. However, no study has assessed the use of the CT-based fluoro-matched navigation system during THA. Therefore, we have evaluated the accuracy of stem orientation by CT-based fluoro-matched navigation.
Methods
The accuracy of stem orientation by CT-based fluoro-matched navigation was assessed by postoperative CT data. Furthermore, we compared the postoperative stem orientation with the intraoperative registration errors.
Results
The average antetorsion error of the stem (navigation records − postoperative CT) was −0.5° ± 5.2°. The stem valgus error was 0.4° ± 2.7°. The accuracy of the navigation record for the orientation of the stem valgus was dependent on the intraoperative registration errors.
Conclusions
The clinical accuracy of CT-based fluoro-matched navigation is adequate for stem alignment orientation, and the intraoperative verification of registration errors is valuable for checking the accuracy of stem orientation by navigation.
Introduction
Cup and stem orientation during total hip arthroplasty (THA) are critical factors for achieving an optimal range of motion and joint stability. Several studies have focused on cup orientation with positioning in the safe zone during THA by navigation, as outlined by Lewinnek et al. [1]. Sariali et al. [2] who predicted stem antetorsion using computerised three-dimensional (3D) preoperative planning. However, antetorsion of the stem was significantly different from the antetorsion of the manually implanted stem even when an anatomically shaped cementless stem was used [3]. The average error between pre- and postoperative antetorsion was 11° [3]. Although stem orientation can be estimated by the surgeon during the operation, the intraoperative estimation of femoral antetorsion was found to have limited accuracy [4]. Thus, computer-assisted navigation is the only method that can obtain precise information about stem antetorsion [5].
In recent years, the following three types of navigation systems have been developed and used in clinical settings: Computed tomography (CT)-free, CT-based, and CT-based fluoro-matched navigation systems. The CT-free (imageless) navigation system does not require pre- or intraoperative image acquisition [6, 7]; rather, this system only requires intraoperative pointer-based registration. The registration of the CT-based navigation system is achieved by matching the intraoperative surface shapes of the patient’s anatomical landmarks with the preoperative CT data, whereas the registration of the CT-based fluoro-matched navigation system is achieved by matching the fluoroscopic image of the patient’s anatomical landmarks with the preoperative CT data. Several studies have demonstrated that component orientation positioning is achieved more accurately using the CT-based navigation system rather than by using a CT-free navigation system [5, 8, 9]. In contrast, Kilties did not observe any significant differences between CT-based and CT-free navigation; however, both navigation systems reduced the variation in the component positioning compared with the conventional free-hand method [10]. Furthermore, they demonstrated that CT-based navigation might have some advantages over the CT-free system in patients with abnormal anatomy such as hip dysplasia [10].
Several manuscripts have reported the relationship between BMI and the accuracy of cup orientation during navigation THA [11–14]. However, no report has described the relationship between clinical parameters and the accuracy of stem orientation in navigation THA and CT-based fluoro-matched navigation THA. Therefore, we have evaluated the clinical factors affecting stem angle accuracy during navigation THA.
Although several studies have assessed the accuracy of femoral component orientation during THA with CT-free and CT-based navigation systems [5, 15, 16], no study has assessed the accuracy of a CT-based fluoro-matched navigation system during THA. Therefore, the aim of this study was to assess the accuracy of femoral component orientation of THAs inserted using a CT-based fluoro-matched navigation system.
Materials and methods
Patients
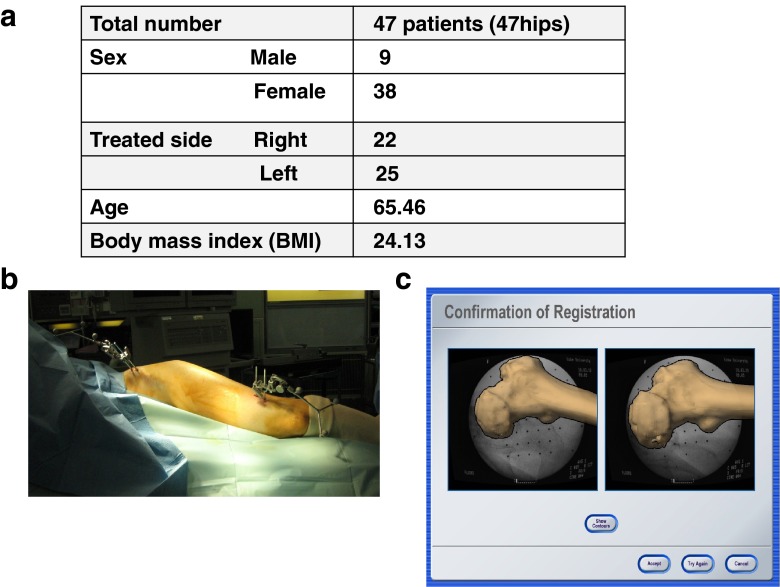
This study analysed 61 hips (29 right hips and 32 left hips) of 11 men and 50 women. The mean age of the patients was 65.46 years, and the average body mass index (BMI) was 24.13 (Fig. 1a). All patients underwent THA with a CT-based fluoro matched navigation system (VVHIP3.5; Brainlab, Feldkirchen, Germany) between January 2010 and May 2012 for osteoarthritis (52 joints in 52 patients) or idiopathic osteonecrosis of the femoral head (nine joints in nine patients). All patients underwent THA with a Summit stem (DePuy, Warsaw, IN). The navigation system was used for preoperative planning. Fourteen hips were excluded from this study because femoral trackers were not verified or the trackers seemed to loosen during THA. Finally, 47 hips were analysed in this study. The study protocol was approved by the Kobe University Graduate School of Medicine Ethics Committee, and all patients provided informed consent.
Fig. 1.
a Patient demographics. b Pelvic tracker on the iliac crest and a femoral tracker on the distal femur. c Registration of the intraoperative fluoro image and preoperative three-dimensional computed tomography (CT) data
Registration of navigation THA
The registration was performed using fluoroscopic imaging with reference landmarks on the patient’s anatomy relative to the tracked reference arrays. A pelvic tracker was percutaneously fixed to the iliac crest and a femoral tracker was fixed to the anterolateral aspect of the distal femur (Fig. 1b).
The software provides the surgeon with real-time information on the location of surgical instruments relative to the patient’s anatomy by associating the positions of the registered anatomical landmarks relative to the reference arrays with the 3D representations of the patient’s bones calculated from segmentation of the patient’s CT scans. For the registration procedures, fluoro images of the proximal femur including the femoral head were taken first, and the medial and lateral epicondyle landmarks were then recorded with a pointer. Subsequently, fluoro images were matched with preoperative CT images (Fig. 1c). Finally, the registration accuracy was verified by touching the proximal femur with a pointer, and registration was concluded prior to skin incision.
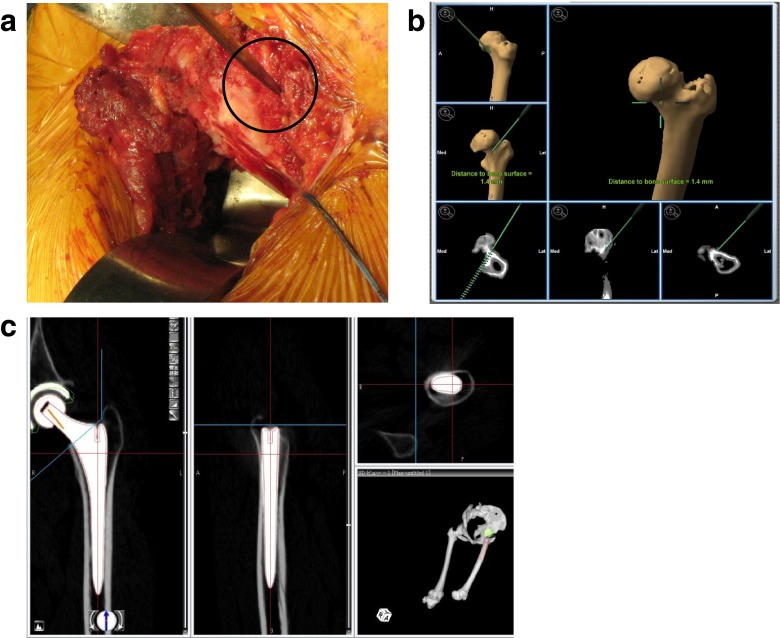
Intraoperative measurement of registration errors
In order to check the accuracy of registration during surgery, we verified that the position of the pointer in the dialog views corresponded very closely to the actual position of the pointer tip on the bone. For example, the pointer touched the surface of the anterior sides of the femur in Fig. 2a, but Fig. 2b shows that the position of the pointer in the dialogue views was a distance of 1.4 mm from the bone. We defined this distance as a registration error. The verification points were the tip of the greater trochanter, the lesser trochanter, and the anterior and posterior sides of the femur near the neck resection line. The registration error was calculated by average values of the distance to the bone at verification points. Because we believed that the accuracy of the stem alignment orientation of the navigation records was dependent on the intraoperative registration errors, we compared the postoperative stem antetorsion/valgus measurements with the intraoperative registration errors.
Fig. 2.
a Postoperative CT data was transferred to the planning module and was reconstructed to axial, frontal, and sagittal planes. The computer-aided design model of the femoral implant was superimposed. b Verification point of the anterior side of the femur. c The position of the pointer in the dialogue views shows a distance of 1.4 mm from the bone
Postoperative measurement of stem antetorsion and valgus angles
For postoperative evaluation, a CT was taken from the pelvis to the knee joint and was transferred to 3D template software (Zed hip, Lexi, Tokyo, Japan). Computer-aided design (CAD) models of the implants were manually adjusted for postoperative multi-planar reconstruction in CT images (Fig. 2c). Stem antetorsion and valgus angles were measured with respect to the mechanical axis of the femur. The mechanical axis was estimated from the centre of both epicondyles of the femur and the femoral head. The estimated mechanical axis in the 3D template was the same as in the navigation system. We measured the postoperative stem alignment by using the manual template, and we checked the reliability of this method by measuring the inter- (N = 5) and intra- (N = 5) observer variabilities. Because the main aim of this study was to evaluate the accuracy of femoral component orientation by the CT-based fluoro-matched navigation system, we compared intraoperative navigation records and the postoperative CT scan findings. In order to analyse the accuracy of intraoperative navigation records for stem antetorsion and valgus angles, we compared the intraoperative stem antetorsion/valgus angles using navigation records and the postoperative stem antetorsion/ valgus angles using postoperative CT data.
Correlation of stem orientation accuracy and clinical parameters
We compared the measurement errors of stem antetorsion/valgus angles and clinical parameters such as sex, treated side, age, height, body weight, and BMI.
Statistical analysis
The comparisons of stem antetorsion and valgus angles between the navigation records and postoperative CT findings were performed using one-way analysis of variance with Tukey’s post hoc test for multiple comparisons of paired samples. The results are presented as mean values with 95 % confidence intervals (95 % CI). The correlation between stem anteversion or the valgus angle and intraoperative registration errors, sex, treated side, age, height, body weight, or BMI were calculated by the Pearson chi-square test. In all cases, P values < 0.05 were considered statistically significant.
Results
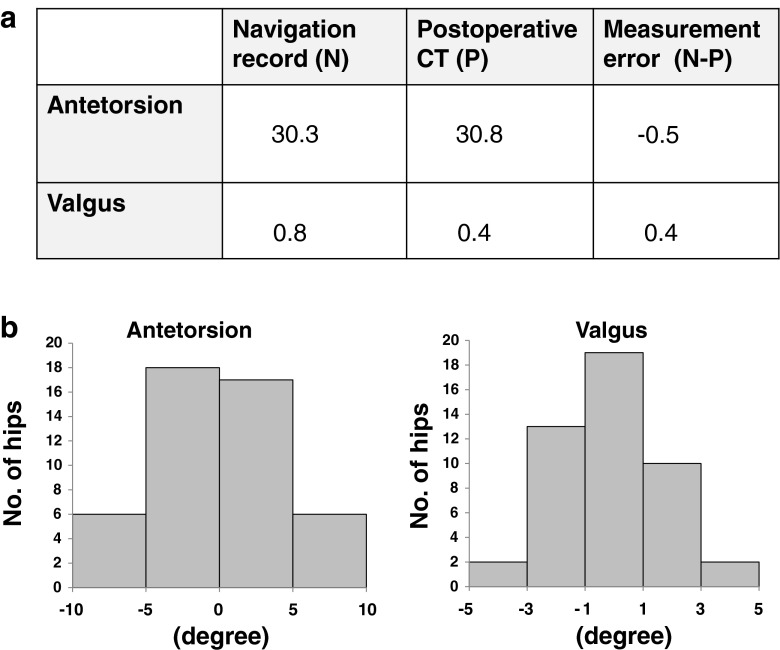
Accuracy of stem antetorsion and valgus angles
We did not find any difference between the navigation records (antetorsion: mean = 30.3, 95 % CI = 27.5–33.1; valgus: mean = 0.8, 95 % CI = −0.1–1.7) and the postoperative CT evaluation (antetorsion: mean = 30.8, 95 % CI = 27.9–33.7; valgus: mean = 0.4, 95 % CI = −0.3–1.1) (Fig. 3a). The average measurement errors (navigation records − postoperative CT) were −0.5° ± 5.2° (antetorsion) and 0.4° ± 2.7° (valgus) (Fig. 3a). The measurement error of antetorsion within 5° was 74.5 % (range, −7.82 to 9.77°) in all cases (Fig. 3b). Furthermore, the measurement error of valgus within 3° was 74.5 % (range, −3.93 to 3.36°) for all cases (Fig. 3b).
Fig. 3.
Stem antetorsion and valgus results
The intra-observer and inter-observer variabilities were 0.16° ± 0.22° (correlation coefficient = 0.99) and 0.01° ± 0.26° (correlation coefficient = 0.99), respectively, for stem antetorsion, and 0.16° ± 0.34° (correlation coefficient = 0.98) and 0.12° ± 0.25° (correlation coefficient = 0.98), respectively, for the stem valgus angle. These data confirmed the reproducibility of the measurement method.
The navigation record accuracy of stem valgus orientation was dependent on intraoperative registration errors
In order to check the accuracy of the navigation records of stem angle orientation during navigation THA, we compared the postoperative stem antetorsion/valgus measurements with the intraoperative registration errors.
A significant correlation was not found between the intraoperative registration errors and the postoperative measurement errors of the antetorsion angles (Table 1). However, the correlation between the intraoperative registration errors and the postoperative measurement errors of stem valgus angles was statistically significant (correlation coefficient = 0.47, P = 0.03) (Fig. 3). Generally, a correlation coefficient value over 0.4 represents a certain correlation. Therefore, we propose that the correlation between the mean registration error values and the accuracy of stem orientation is clinically significant.
Table 1.
Comparisons of the postoperative stem antetorsion/valgus measurements and intraoperative registration errors
| Measurement | Antetorsion | Valgus |
|---|---|---|
| Correlation coefficient | 0.04 | 0.47 |
| P-value | 0.84 | 0.03 |
A correlation was not found between stem orientation accuracy and clinical parameters
Significant differences were not found between the measurement errors of stem antetorsion/valgus angles and sex/treated side (data not shown). Furthermore, the correlation between the measurement errors of stem antetorsion/valgus angles and age, height, body weight, and BMI were not statistically significant (Table 2). These results indicated that the stem orientation accuracy was not dependent on clinical parameters during navigation THA.
Table 2.
Comparisons of stem orientation accuracy and clinical parameters
| Measurement | Age | Height | Body weight | BMI | |
|---|---|---|---|---|---|
| Correlation coefficient | Antetorsion valgus | 0.03 | 0.05 | 0.03 | 0.02 |
| 0.19 | 0.08 | 0.04 | 0.16 | ||
| P-value | Antetorsion valgus | 0.90 | 0.81 | 0.89 | 0.91 |
| 0.42 | 0.74 | 0.86 | 0.50 | ||
Discussion
Several studies have investigated stem positioning in navigation THA [5, 15, 16]. Dorr et al. analysed the accuracy of CT-free navigation and demonstrated that the average stem antetorsion in the navigation record was 10.9° ± 9.0° and the postoperative measurement with CT data was 10.6° ± 8.0° [5]. However, they did not show the measurement error. Kitada et al. [8], who also analysed the accuracy of CT-based navigation, reported that the average stem antetorsion of the navigation record was 31.1° ± 11.7° and the postoperative measurement with CT data was 31.7° ± 11.7°; furthermore, they reported an average stem valgus in the navigation record of −0.1° ± 2.6° and a postoperative measurement with CT data of 0.1° ± 1.8°. These authors reported measurement errors to be −0.6° ± 4.8° for antetorsion and −0.2° ± 1.8° for valgus [8]. In our study, we analysed the accuracy of CT-based fluoro-matched navigation and demonstrated measurement errors of −0.5° ± 5.2° and 0.4° ± 2.7° for stem antetorsion and valgus, respectively. These average measurement error values were similar to previously reported values from CT-based navigation. However, because Kitada reported standard deviation and not confidence intervals, we cannot compare the accuracy differences between CT-based fluoro-matched navigation and CT-based navigation. Kitada et al. also demonstrated that 77 % of all cases achieved a measurement error within 5° of stem antetorsion [6]. In our study, we achieved measurement errors within 5° antetorsion in 74.5 % of cases and within 3° valgus in 91.5 % of cases, suggesting that the CT-based fluoro-matched navigation system is accurate in clinical use. However, the measurement errors of almost 25 % of cases were over 5° antetorsion and 10 % were over 3° valgus. These results suggest that the navigation system should be used with caution in these types of cases and that the system requires further improvements.
The navigation system can be used with confidence if the accuracy of the navigation record can be checked during THA. This study is the first to propose the accuracy of this confirmation method. We demonstrated the ability to measure registration errors during the operation and showed that the reduction of registration errors was valuable for the accuracy of the navigation record of stem valgus orientation.
Tsukada et al. demonstrated that obesity decreased the accuracy of acetabular cup placement in CT-free navigation [12]. Furthermore, Hasart et al. demonstrated that BMI and soft tissue thickness affected the accuracy of cup orientation in CT-free navigation [13]. We demonstrated that clinical parameters, including BMI, did not result in a significant difference in the accuracy of stem orientation. In other words, obesity did not affect the accuracy of stem orientation in CT-based fluoro-matched navigation THA in our study.
In conclusion, the clinical accuracy of CT-based fluoro-matched navigation is adequate for the orientation of stem alignment, and the intraoperative verification of registration errors is valuable for checking the accuracy of stem orientation by navigation.
References
- 1.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–220. [PubMed] [Google Scholar]
- 2.Sariali E, Mouttet A, Pasquier G, Durante E, Catone Y. Accuracy of reconstruction of the hip using computerised three-dimensional pre-operative planning and a cementless modular neck. J Bone Joint Surg Br. 2009;91(3):333–340. doi: 10.1302/0301-620X.91B3.21390. [DOI] [PubMed] [Google Scholar]
- 3.Jerosch J, von Hasselbach C, Filler T, Peuker E, Rahgozar M, Lahmer A. Increasing the quality of preoperative planning and intraoperative application of computer-assisted systems and surgical robots—an experimental study. Chirurg. 1998;69(9):973–976. doi: 10.1007/s001040050524. [DOI] [PubMed] [Google Scholar]
- 4.Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21(5):696–701. doi: 10.1016/j.arth.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res. 2009;467(1):119–127. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wixson RL, MacDonald MA. Total hip arthroplasty through a minimal posterior approach using imageless computer-assisted hip navigation. J Arthroplasty. 2005;20(7 Suppl 3):51–56. doi: 10.1016/j.arth.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 7.Najarian BC, Kilgore JE, Markel DC. Evaluation of component positioning in primary total hip arthroplasty using an imageless navigation device compared with traditional methods. J Arthroplasty. 2009;24(1):15–21. doi: 10.1016/j.arth.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Kitada M, Nakamura N, Iwana D, Kakimoto A, Nishii T, Sugano N. Evaluation of the accuracy of computed tomography-based navigation for femoral stem orientation and leg length discrepancy. J Arthroplasty. 2011;26(5):674–679. doi: 10.1016/j.arth.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Ryan JA, Jamali AA, Bargar WL. Accuracy of computer navigation for acetabular component placement in THA. Clin Orthop Relat Res. 2010;468(1):169–177. doi: 10.1007/s11999-009-1003-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalteis T, Handel M, Bathis H, Perlick L, Tingart M, Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Joint Surg Br. 2006;88(2):163–167. doi: 10.1302/0301-620X.88B2.17163. [DOI] [PubMed] [Google Scholar]
- 11.Hohmann E, Bryant A, Tetsworth K. Anterior pelvic soft tissue thickness influences acetabular cup positioning with imageless navigation. J Arthroplasty. 2012;27(6):945–952. doi: 10.1016/j.arth.2011.09.017. [DOI] [PubMed] [Google Scholar]
- 12.Tsukada S, Wakui M. Decreased accuracy of acetabular cup placement for imageless navigation in obese patients. J Orthop Sci. 2010;15(6):758–763. doi: 10.1007/s00776-010-1546-1. [DOI] [PubMed] [Google Scholar]
- 13.Hasart O, Perka C, Christian K, Asbach P, Janz V, Wassilew GI. Influence of body mass index and thickness of soft tissue on accuracy of ultrasound and pointer based registration in navigation of cup in hip arthroplasty. Technol Health Care. 2010;18(4–5):341–351. doi: 10.3233/THC-2010-0601. [DOI] [PubMed] [Google Scholar]
- 14.Lee YS, Yoon TR. Error in acetabular socket alignment due to the thick anterior pelvic soft tissues. J Arthroplasty. 2008;23(5):699–706. doi: 10.1016/j.arth.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 15.Jerosch J, Peuker E, von Hasselbach C, Lahmer A, Filler T, Witzel U. Computer assisted implantation of the femoral stem in THA—an experimental study. Int Orthop. 1999;23(4):224–226. doi: 10.1007/s002640050356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zheng G, Marx A, Langlotz U, Widmer KH, Buttaro M, Nolte LP. A hybrid CT-free navigation system for total hip arthroplasty. Comput Aided Surg. 2002;7(3):129–145. doi: 10.3109/10929080209146024. [DOI] [PubMed] [Google Scholar]