Abstract
Purpose
Patella resurfacing or nonresurfacing in total knee arthroplasty remains controversial. The aim of this study was to evaluate the efficacy of patellar resurfacing through an evaluation of the current literature.
Methods
We carried out a meta-analysis of randomised controlled trials comparing total knee arthroplasties performed with and without patellar resurfacing. Outcomes of reoperation, anterior knee pain and knee scores were analysed.
Results
Fourteen trials assessing 1,725 knees were eligible. The absolute risk of reoperation was reduced by 4 % (95 % confidence interval, 2–6 %) in the patellar resurfacing arm (between-study heterogeneity, P = 0.05, I2 = 42 %), implying that one would have to resurface 25 patellae (95 % confidence interval, 17–50 patellae) in order to prevent one reoperation. There was no difference between the two groups in terms of anterior knee pain, knee pain score, Knee Society score and knee function score. But in the studies followed up for a mean time of not less than five years, a difference was found between the two arms in Knee Society scores (RR = 2.14, 95 % confidence interval, 0.76–3.52; P = 0.002).
Conclusions
The available evidence indicates that patellar resurfacing reduces the risk of reoperation after total knee arthroplasty. Patellar resurfacing patients may make a difference in long-term follow-up (five or more 5 years) of Knee Society scores. In other aspects, the benefit of patellar resurfacing is limited. Additionally, more carefully and scientifically designed randomised controlled trials are required to further prove the claim.
Introduction
Management of the patella in total knee arthroplasty (TKA) remains controversial. Some surgeons prefer resurfacing because of the increasing rate of secondary patellar revision or other reoperations and anterior knee pain in patients without patellar resurfacing. Other surgeons do not resurface the patella during TKA to avoid complications such as fracture, loosening, instability and patella tendon damage [1]. There are various studies about the patellar resurfacing puzzle, including randomised controlled trials (RCTs), retrospective studies, meta-analysis and systematic review, but no final conclusion has been drawn. Since the latest meta-analysis of patellar resurfacing was done in 2010 and published in 2011 [2, 3], and many RCTs have been conducted since then, it is necessary to engage a new analysis containing these latest RCTs. We therefore conducted a meta-analysis of all available RCTs comparing TKAs with and without patellar resurfacing to evaluate the efficacy of this aspect of the procedure.
Materials and methods
Identification and eligibility of relevant RCTs
We searched MEDLINE (1966 to present), EMBASE and the Cochrane databases for randomised trials comparing total knee arthroplasties performed with and without patella resurfacing. Inclusion criteria were [3]: (1) English literature, (2) adults undergoing primary TKA for osteoarthritis, (3) all available prospective RCTs comparing patellar resurfacing to nonresurfacing in TKA, (4) patellar resurfacing not at the same time as primary TKA, (5) data for reoperation, anterior knee pain and knee scores (Knee Society score, knee pain score, knee function score). Exclusion criteria were: non-English language literature, unpublished data, proceedings of meetings, non-randomised controlled trials, studies of body specimens and studies of TKA but not patellar resurfacing. To avoid double counting, multiple articles of the same patient population were pooled as one study.
Outcomes
The number of reoperations, cases suffering postoperative anterior knee pain, symptom and function scores such as the Hospital for Special Surgery score (HSS) [4], the WOMAC score [5], the Bristol knee score [6] and the Knee Society score (KSS) [7] were sorted successively for further analysis.
Data extraction
The relevant data were extracted from every article by two of the authors independently and were checked by a third researcher against the original information in order to avoid anthropic mistakes. The extracted data included publication information, numbers of reoperations for any reason, follow-up time and numbers lost to follow up, numbers of patients who suffered any grade of postoperative anterior knee pain, and the relevant knee scores.
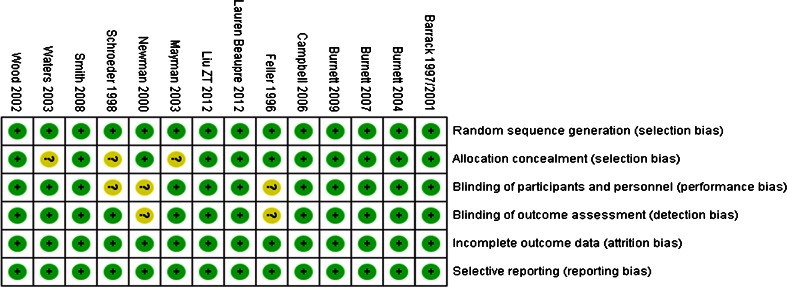
Assessment of methodological quality
Two of the authors independently assessed the methodological quality of each article with respect to random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data and selective reporting by the computer software developed by the Cochrane Collaboration, RevMan (RevMan 5.2).
Meta-analysis
Data was analysed by the software RevMan (RevMan 5.2). The fixed model and the random-effects model were used to analyse the pooled data. A P value of < 0.1 was considered suggestive of statistical heterogeneity. In case of significant heterogeneity, the random-effects model was used. Referring to the study of Fu et al. [3], 95 % confidence limits and risk differences were calculated for reoperation and the presence of postoperative anterior knee pain (AKP) of any grade, weighted mean differences and 95 % confidence limits calculated for the KSS knee score of relative studies and the studies with a mean length of follow-up not less than five years. The number of knees needed to be treated in order to avoid reoperations or postoperative AKP was also calculated (1/|risk difference|).
Results
After detailed evaluation, 14 independent randomised trials [6, 8–20] with a cumulative sample size of 1,725 knees at final follow-up were included in the overall meta-analysis (Table 1). The methodological quality is shown in Fig. 1 to see the risk of bias. All 14 studies provided data on reoperations during follow-up. Ten provided particular data of the prevalence of postoperative anterior knee pain of any grade [6, 9, 11, 12, 14–18, 20]. Nine studies reported Knee Society score [8, 10–12, 14–16, 18, 20], and five of them had a mean length of follow-up of five or less years [12, 14, 15, 18, 20]. Seven studies provided details on the knee function score [10–12, 14, 16, 18, 20], and four of them had a length of follow-up five or more years [12, 14, 18, 20]. Only four trials provided details on knee pain scores at the last follow-up [14, 16, 19, 20].
Table 1.
Characteristics of studies
| First author | Journal | Year of publication | Number of knees (RS / NRS) | Mean age(year) | Loss to follow-up (knees) | Mean years of follow-up | Outcomes | Level of evidence | Treatment | Number of reoperations | Main reasons for reoperations | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Feller [8] | JBJS | 1996 | 19 | 19 | 70.8 | 2 | 2 | HSS, patellar score, patellar pain | I | PCA (HOWMEDICAL) | RS:2/NRS:0 | Suprapatellar adhesions, posterolateral pain |
| Barrack [9, 21] | JBJS | 1997, 2001 | 58 | 60 | 66.2 | 25 | 5-7 | KSS, AKP, patient satisfaction, ROM | I | Miller-Galante II (ZIMMER) | RS:0/NRS:7 | AKP |
| Schroeder [10] | Arch Orthop Trauma | 1998 | 20 | 20 | 72.6 | 0 | 2 | KSS, AKP, climbing staris, radiographs | I | DURACON (HOWMEDICA) | RS:1/NRS:3 | AKP, lateral subluxation of patella |
| Newman [6] | KNEE | 2000 | 42 | 42 | 72 | 0 | 5 | Bristol score, patellar score | I | KINEMATIC (HOWMEDICA) | RS:0/NRS:6 | AKP |
| Wood [11] | JBJS | 2002 | 92 | 128 | 73.7 | 22 | 4 | KSS, AKP, stair climbing, radiographs, patient satisfaction | I | Miller-Galante II (ZIMMER) | RS:9/NRS:15 | AKP, maltracking, patella dislocation/loosening/fracture, infection, loose bodies |
| Waters [12] | JBJS | 2003 | 243 | 231 | 69 | 0 | 5.3 | KSS, AKP, patient satisfaction, function score, ROM, radiographs | I | Press-Fit Condylar prosthesis (Johnson & Johnson) | RS:3/NRS:11 | AKP |
| Mayman [13] | J Arthroplasty | 2003 | 50 | 50 | 70 | 29 | 10 | KSS, AKP | I | AMK (Depuy) | RS:2/NRS:2 | Pain, patella fracture and other patellofemoral complications |
| Burnett [14] | CORR | 2004 | 42 | 48 | 78 | 0 | 10 | KSS, AKP, ROM, patient satisfaction, radiographs | I | AMK (Depuy) | RS:1/NRS:3 | AKP, sepsis, tibial base plate PE wear, osteolysis, patella necrosis, quadriceps tendon rupture |
| Campbell [15] | JBJS | 2006 | 46 | 54 | 72 | 42 | 10 | WOMAC scores, AKP, radiographs | I | Miller-Galante II (ZIMMER) | RS:1/NRS:2 | AKP |
| Smith [16] | JBJS | 2008 | 73 | 86 | 71.5 | 2 | 4 | KSS, AKP, patient satisfaction, radiographs | I | Profix Total Knee System (Smith and Nephew) | RS:1/NRS:1 | PF nodule, locked knee, infection, tibial insert exchange |
| Burnett [17] | CORR | 2007 | 28 | 28 | NR | 0 | 10 | KSS, AKP, patient satisfaction | I | Miller-Galante II (ZIMMER) | RS:1/NRS:2 | AKP, PF-related aseptic loosening, sepsis, tibial liner exchange |
| Burnett [18] | JBJS | 2009 | 58 | 60 | NR | 40 | 10 | ROM, KSS, AKP, patient satisfaction | II | Miller-Galante II (ZIMMER) | RS:5/NRS:7 | AKP |
| Lauren Beaupre [19] | BMC Research Notes | 2012 | 21 | 17 | 63,6 | 6 | 10 | WOMAC, ROM, RAND 36 score | I | Profix Total Knee System (Smith and Nephew) | RS:1/NRS:3 | AKP |
| Zhong-tang Liu [20] | KNEE | 2012 | 68 | 64 | 67.7 | 12 | 7 | AKP, KSS, ROM, radiographs | I | Press-Fit Condylar prosthesis (DePuy) | RS:0/NRS:1 | Infection |
RS resurfacing, NRS nonresurfacing, AKP anterior knee pain, HSS hospital for special surgery, ROM range of motion, WOMAC Western Ontario McMaster Osteoarthritis Index, PF patella-femoral, PE polyethylene
Fig. 1.
Risk of bias
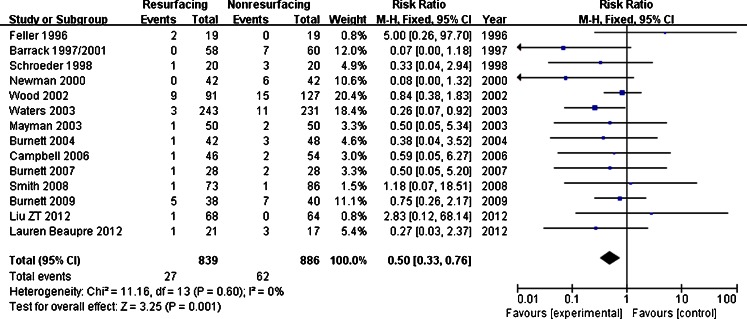
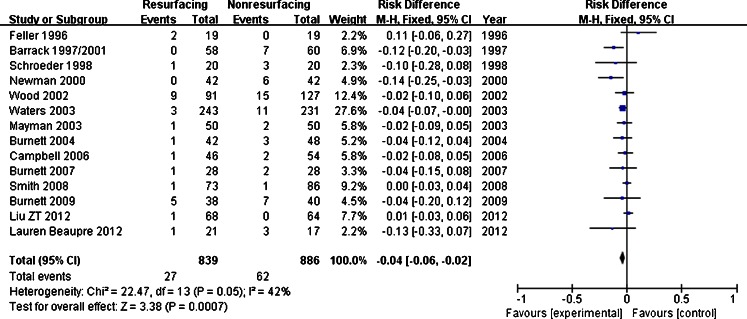
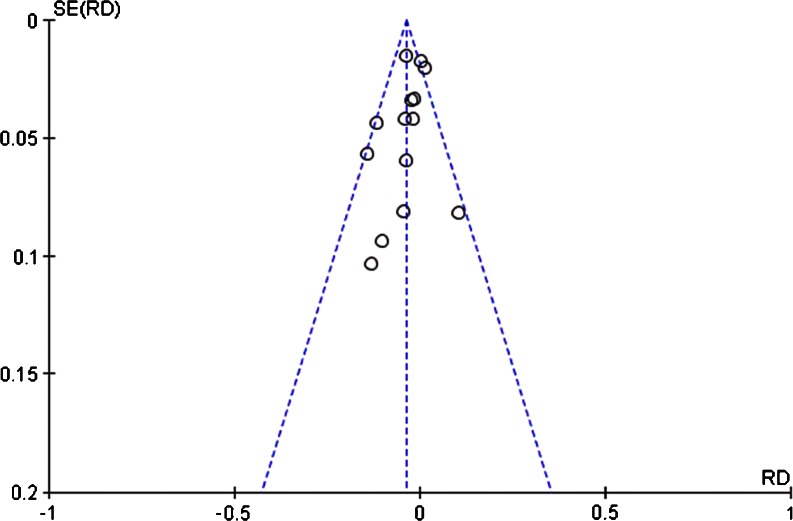
The relative risk for reoperation favoured patellar resurfacing (RR = 0.50, 95 % CI, 0.33-0.76; P = 0.001 < 0.05) (Fig. 2). The test for homogeneity was not significant, implying that there was no heterogeneity between these 14 studies (P = 0.60). The absolute risk of reoperation was reduced by 4 % (95 % CI, 2–6 %) in the patellar resurfacing group compared with the nonsurfacing arm (Fig. 3). A funnel plot of the reoperation data of the 14 articles showed low publication bias (Fig. 4). The result implied one would have to resurface 25 patellae (95 % CI, 17–50 patellae) in order to prevent one reoperation.
Fig. 2.
Reoperation
Fig. 3.
Reoperation–risk difference
Fig. 4.
Funnel plot
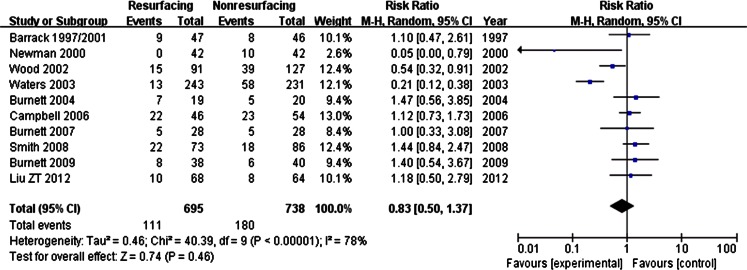
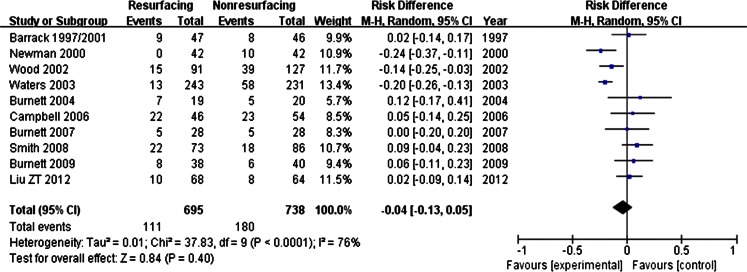
The relative risk for postoperative anterior knee pain of the ten studies was 0.83 (95 % CI, 0.50–1.37; P = 0.46). The difference was not significant (Figs. 5 and 6). The studies were heterogeneous since the test for homogeneity was significant (P < 0.00001). So a random effects model was used. In our point, the heterogeneity might have a relationship with different length of follow-up or different kinds of implants. But no major differences in the studies could explain the observed heterogeneity convectively.
Fig. 5.
Postoperative anterior knee pain
Fig. 6.
Postoperative anterior knee pain–risk difference
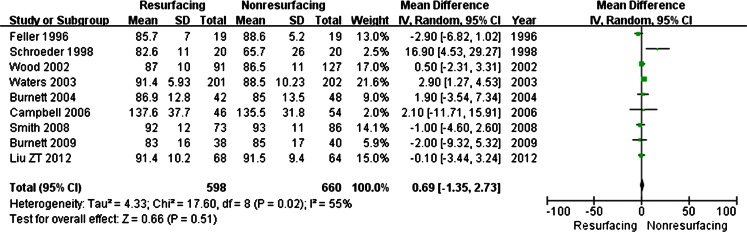
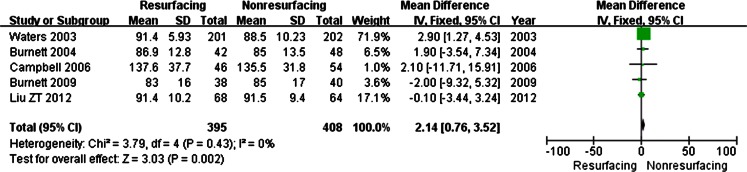
The nine studies [8, 10–12, 14–16, 18, 20] which reported the details of the Knee Society score showed a significant heterogeneity (P = 0.02) (Fig. 7); so we could draw no conclusion from the data. In addition, we analysed Knee Society scores of studies with a long-term follow-up (five or more years) individually. Five studies were recorded [12, 14, 15, 18, 20], and the test for homogeneity was not significant (P = 0.43). A significant difference was found between the two groups (RR = 2.14, 95 % CI, 0.76–3.52; P = 0.002) (Fig. 8). This might imply that during the long-term follow-up (five or more years), patellar resurfacing patients may get a higher Knee Society score than the nonresurfacing patients.
Fig. 7.
Knee score
Fig. 8.
Knee score (≥5 years)
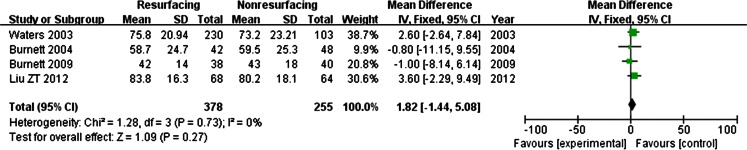
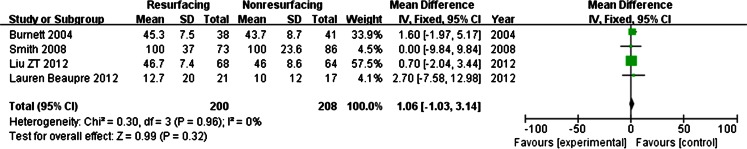
Knee function score and knee pain score are part of the Knee Society score. In the seven studies which provided details on the knee function score [10–12, 14, 16, 18, 20], there was no heterogeneity (P = 0.23), and no difference was shown between the two groups (P = 0.14) (Fig. 9). The same conclusion was drawn in the four long-term follow-up studies [12, 14, 18, 20] (no heterogeneity: P = 0.73; no significant difference: P = 0.27) (Fig. 10) and only four studies provided knee pain scores [14, 16, 19, 20] (no heterogeneity, P = 0.96; no significant difference, P = 0.99) (Fig. 11).
Fig. 9.
Function score
Fig. 10.
Function score (≥5 years)
Fig. 11.
Pain score
Discussion
By this meta-analysis of 1,725 randomised trials, we found that the rate of reoperation was lower following total knee arthroplasty with patellar resurfacing than after total knee arthroplasty without patellar resurfacing. But there was no difference between the two groups in terms of anterior knee pain. Interestingly, we found that during the long-term follow-up (five or more years), the patellar resurfacing group might achieve a higher Knee Society score than the nonresurfacing group. This new conclusion is different from many of the past systematic studies. More high quality and well-designed RCTs with long-term follow-up are needed to support this conclusion. The absolute risk difference for reoperation was the same as the study of Fu et al. [3]. It implies that one would have to resurface 25 patellae in order to prevent one reoperation. The outcome of reoperation was not assessed in this study. In the study of Fu et al. [3], they found that 76 % of the patients who suffered postoperative patella-femoral-related pain benefited from the secondary resurfacing.
When searching for the literature for this meta-analysis, we found many meta-analysis reports or systemic studies of the same theme, as well as prospective studies and some prospective studies that did not mention randomised controlled trials. The results of these studies were sometimes inconsistent. Pakos et al. [22] and Calvisi et al. [23] found that patellar resurfacing might reduce the risks of reoperation and anterior knee pain after AKP and Patel’s cohort study supported this conclusion [24]. But in the studies of Fu et al. [3] and He et al. [2], no difference between the resurfacing group and the nonresurfacing group in terms of anterior knee pain rate was found. They only found significance of reoperation risks between the two groups. And the systematic review of Li et al. had a result similar to the previous two studies [25]. The study of Lindstrand et al. [26] showed that there was no statistical difference in the number of revisions due to patella problems between the two groups. A prospective study from Patil et al. [27] concluded that there were no differences in the improvement of KSS scores, Short-Form 36 scores and satisfaction rates among the patellar resurfacing group, the patellar retention group and the patelloplasty group. A retrospective study conducted by Seo et al. [28] showed that there was no correlation between the degree of patellar articular defect and patellar resurfacing in terms of the clinical and radiological outcomes. And the latest study of Pavlou et al. [29] provided further findings that neither patellar resurfacing nor the prosthetic design affects the clinical results of TKAs. Studies of LCS mobile-bearing total knee arthroplasty [30, 31] showed the importance of soft tissue, especially the ligaments, in the decision for patellar resurfacing or not. Hwang et al. [31] concluded that if soft tissue balancing and a patella-friendly prosthetic design are properly used, patellar retention with a patelloplasty might be viable, even in knees with serious patellofemoral arthritis. Since there have been no final conclusions about resurfacing of patella or not during TKA, more studies are needed to be conducted in the future.
The strengths of this meta-analysis include: (1) this is an update of the present meta-analysis; (2) the design of search strategy, and the inclusion and exclusion criteria are based on the experience of the present meta-analysis; (3) explicit research protocol was developed before the analysis; (4) consensus between two reviewers and checked by a third reviewer to avoid anthropic mistakes; and (5) new finds about long-term follow-up.
Some limitations of our study should be acknowledged: (1) the sample sizes are small; larger and more rigorous prospective randomised controlled studies are needed to strengthen the findings; (2) not all studies provide the details of prevalence of anterior knee pain and knee scores, which may cause bias; (3) the skills of different surgeons may influence the clinical outcomes; we need a standard to assess the surgery skills in order to avoid surgeon bias; and (4) implant designs may affect the outcomes, though a study from Pavlou et al. [29] shows that the prosthetic design may not affect the clinical results of TKAs. There are various prosthetic features in the 14 studies included. This may affect the result of this meta-analysis.
Conclusion
This meta-analysis shows that patellar resurfacing may reduce the risks of reoperation after total knee arthroplasty. It may make a difference in long-term follow-up (five or more years) of Knee Society scores. In other aspects, the benefit of patellar resurfacing is limited. Additionally, more carefully and scientifically designed RCTs with large samples and long-term follow-up are required to further prove the claim. Based on the evidence provided by this study, the authors now prefer not resurfacing the patella during primary TKA operations. Patients with and without patella resurfacing are being followed up carefully in terms of reoperations, anterior knee pain, Knee Society scores and radiographs to assess the long-term outcomes.
Footnotes
Level of evidence
Therapeutic study; Systematic review; Level II
Kai Chen and Guodong Li contributed equally to the work as co-first authors.
Contributor Information
Kai Chen, Email: magaer@126.com.
Guodong Li, Email: litrue2004@yahoo.com.cn.
Zhengdong Cai, Email: zhd_cai@126.com.
References
- 1.Swan JD, Stoney JD, Lim K, Dowsey MM, Choong PF. The need for patellar resurfacing in total knee arthroplasty: a literature review. ANZ J Surg. 2010;80:223–233. doi: 10.1111/j.1445-2197.2010.05242.x. [DOI] [PubMed] [Google Scholar]
- 2.He JY, Jiang LS, Dai LY. Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty? A meta-analysis of randomized trials. Knee. 2011;18:137–144. doi: 10.1016/j.knee.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Fu Y, Wang G, Fu Q. Patellar resurfacing in total knee arthroplasty for osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19:1460–1466. doi: 10.1007/s00167-010-1365-0. [DOI] [PubMed] [Google Scholar]
- 4.Bach CM, Nogler M, Steingruber IE, Ogon M, Wimmer C, Gobel G, Krismer M. Scoring systems in total knee arthroplasty. Clin Orthop Relat Res. 2002;399:184–196. doi: 10.1097/00003086-200206000-00022. [DOI] [PubMed] [Google Scholar]
- 5.Dunbar MJ, Robertsson O, Ryd L, Lidgren L. Appropriate questionnaires for knee arthroplasty. Results of a survey of 3600 patients from the Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br. 2001;83:339–344. doi: 10.1302/0301-620X.83B3.11134. [DOI] [PubMed] [Google Scholar]
- 6.Newman JH, Ackroyd CE, Shah NA. Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg Br. 1998;80:862–865. doi: 10.1302/0301-620X.80B5.8835. [DOI] [PubMed] [Google Scholar]
- 7.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 8.Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br. 1996;78:226–228. [PubMed] [Google Scholar]
- 9.Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L. Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg Am. 2001;83:1376–1381. [PubMed] [Google Scholar]
- 10.Schroeder-Boersch H, Scheller G, Fischer J, Jani L. Advantages of patellar resurfacing in total knee arthroplasty: two-year results of a prospective randomized study. Arch Orthop Trauma Surg. 1998;117:73–78. doi: 10.1007/BF00703446. [DOI] [PubMed] [Google Scholar]
- 11.Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: a prospective, randomized trial. J Bone Joint Surg Am. 2002;84:187–193. doi: 10.2106/00004623-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2003;85:212–217. doi: 10.2106/00004623-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Mayman D, Bourne RB, Rorabeck CH, Vaz M, Kramer J. Resurfacing versus not resurfacing the patella in total knee arthroplasty: 8- to 10-year results. J Arthroplast. 2003;18:541–545. doi: 10.1016/S0883-5403(03)00150-5. [DOI] [PubMed] [Google Scholar]
- 14.Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. Patella resurfacing versus nonresurfacing in total knee arthroplasty: results of a randomized controlled trial at a minimum of 10 years’ followup. Clin Orthop Relat Res. 2004;428:12–25. doi: 10.1097/01.blo.0000148594.05443.a3. [DOI] [PubMed] [Google Scholar]
- 15.Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, WakeWeld L, Stevenson TM. Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Br. 2006;88:734–739. doi: 10.1302/0301-620X.88B6.16822. [DOI] [PubMed] [Google Scholar]
- 16.Smith AJ, Wood DJ, Li MG. Total knee replacement with and without patellar resurfacing: a prospective, randomised trial using the Profix total knee system. J Bone Joint Surg Br. 2008;90:43–49. doi: 10.1302/0301-620X.90B1.18986. [DOI] [PubMed] [Google Scholar]
- 17.Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL. A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res. 2007;464:65–72. doi: 10.1097/BLO.0b013e31812f783b. [DOI] [PubMed] [Google Scholar]
- 18.Burnett RS, Boone JL, Rosenzweig SD, Steger-May K, Barrack RL. Patellar resurfacing compared with nonresurfacing in total knee arthroplasty. A concise follow-up of a randomized trial. J Bone Joint Surg Am. 2009;91:2562–2567. doi: 10.2106/JBJS.H.00109. [DOI] [PubMed] [Google Scholar]
- 19.Beaupre L, Secretan C, Johnston D, Lavoie G (2012) A randomized controlled trial comparing patellar retention versus patellar resurfacing in primary total knee arthroplasty: 5–10 year follow-up. BMC Res Notes 5:273 [DOI] [PMC free article] [PubMed]
- 20.Liu ZT, Fu PL, Wu HS, Zhu Y. Patellar reshaping versus resurfacing in total knee arthroplasty. Results of a randomized prospective trial at a minimum of 7 years’ follow-up. Knee. 2012;19:198–202. doi: 10.1016/j.knee.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 21.Barrack RL, Wolfe MW, Waldman DA, Milicic M, Bertot AJ, Myers L. Resurfacing of the patella in total knee arthroplasty. A prospective, randomized, double-blind study. J Bone Joint Surg Am. 1997;79:1121–1231. doi: 10.2106/00004623-199708000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Pakos EE, Ntzani EE, Trikalinos TA. Patellar resurfacing in total knee arthroplasty. A meta-analysis J Bone Joint Surg Am. 2005;87:1438–1445. doi: 10.2106/JBJS.D.02422. [DOI] [PubMed] [Google Scholar]
- 23.Calvisi V, Camillieri G, Lupparelli S. Resurfacing versus nonresurfacing the patella in total knee arthroplasty: a critical appraisal of the available evidence. Arch Orthop Trauma Surg. 2009;129:1261–1270. doi: 10.1007/s00402-008-0801-9. [DOI] [PubMed] [Google Scholar]
- 24.Patel K, Raut V. Patella in total knee arthroplasty: to resurface or not to–a cohort study of staged bilateral total knee arthroplasty. Int Orthop. 2011;35(3):349–353. doi: 10.1007/s00264-010-1063-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li S, Chen Y, Su W, Zhao J, He S, Luo X. Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthop. 2011;35(3):305–316. doi: 10.1007/s00264-010-1109-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lindstrand A, Robertsson O, Lewold S, Toksvig-Larsen S. The patella in total knee arthroplasty: resurfacing or nonresurfacing of patella. Knee Surg Sports Traumatol Arthrosc. 2001;9(Suppl 1):S21–23. doi: 10.1007/s001670000154. [DOI] [PubMed] [Google Scholar]
- 27.Patil N, Lee K, Huddleston JI, Harris AH, Goodman SB. Patellar management in revision total knee arthroplasty: is patellar resurfacing a better option? J Arthroplasty. 2010;25:589–593. doi: 10.1016/j.arth.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 28.Seo SS, Kim CW, Moon SW. A comparison of patella retention versus resurfacing for moderate or severe patellar articular defects in total knee arthroplasty: minimum 5-year follow-up results. Knee Surg Relat Res. 2011;23:142–148. doi: 10.5792/ksrr.2011.23.3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E. Patellar resurfacing in total knee arthroplasty: does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg Am. 2011;93:1301–1309. doi: 10.2106/JBJS.J.00594. [DOI] [PubMed] [Google Scholar]
- 30.Müller W, Wirz D. The patella in total knee replacement: does it matter? 750 LCS total knee replacements without resurfacing of the patella. Knee Surg Sports Traumatol Arthrosc. 2001;9(Suppl 1):S24–26. doi: 10.1007/s001670000159. [DOI] [PubMed] [Google Scholar]
- 31.Hwang BH, Yang IH, Han CD. Comparison of patellar retention versus resurfacing in LCS mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:524–531. doi: 10.1007/s00167-011-1593-y. [DOI] [PubMed] [Google Scholar]