Abstract
Purpose
The height of navicular bone from the floor is in proportion with the height of longitudinal arch of the foot. The study was conducted to evaluate correlation of navicular bone height with most often used angles, heel valgus and a foot print in order to simplify the procedure for the diagnosis of flatfoot.
Methods
A total of 218 operated children (436 feet) because of flexible flatfoot were evaluated clinically and radiologically. Meary angle, lateral talonavicular angle, talocalcaneal angle, calcaneal pitch, heel valgus and arch index (Staheli) were evaluated pre-operatively and postoperatively. In 121 (242 feet) chosen children (age eight to 15) with all clinical values and pre-operative angles corresponding flatfoot, all postoperatively measured values were within the normal range. We got the navicular index by dividing length of longitudinal arch with navicular height. Values of navicular index were then compared with pre-operatively and postoperatively measured values. Pearson correlation and ROC test were used for statistical analysis.
Results
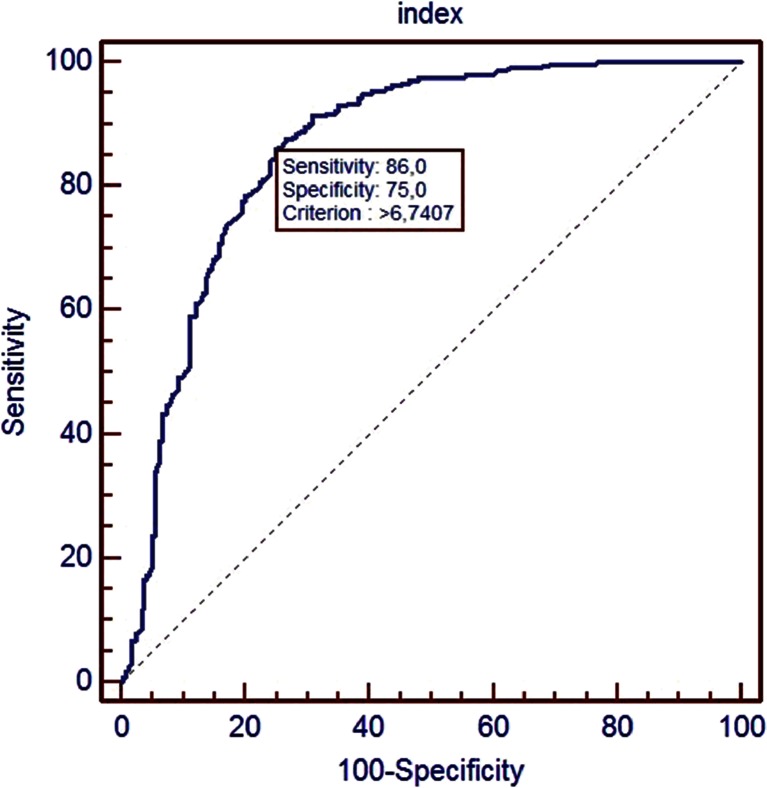
Values of the navicular index for flatfeet were in the interval from 4.75 to 31.2 (median 8.98), and for normal-arched feet 3.58–22.6 (median 5.48). Pearson correlation of arch index and measured parameters were significant in majority, and degree according to Colton was good. Area under the ROC curve was 0.861 (p = 0.0001). The cut-off value with 86 % sensitivity and 75 % specificity was 6.7407.
Conclusion
Navicular index can be used reliably, without measures of the other parameters, to differentiate flatfoot from normal-arched foot. Therefore, the navicular index has an ability to distinguish between the flatfoot and normal-arched foot.
Introduction
Flat feet deformity is a medical condition which is defined as a deformity where the arch on the inside border of the foot is more flat than normal and the entire sole of the foot comes into near-complete or complete contact with the ground [1]. This deformity can occur at any age, but is most common in children [2]. When this deformity occurs in children, it is referred to as paediatric flatfoot [3]. Paediatric flatfoot represents a group of medical conditions that occur in infants, children, and adolescents [4]. These medical conditions differ among themselves by anatomy and aetiological factors [5–11]. Regarding paediatric flatfoot, it may exist as an isolated pathology or as part of a larger clinical entity [7], such as generalized ligamentous laxity, neurologic and muscular abnormalities, genetic conditions and syndromes, and collagen disorders [12].
The main distinction between physiological and pathological paediatric flatfoot is the degree of flexibility. Given these considerations, paediatric flatfoot can be divided into two main categories, flexible and rigid. Flexible flatfoot is characterized by a normal arch during nonweightbearing and a flattening of the arch on stance [12]. Conversely, rigid flatfoot is characterized by a stiff, flattened arch on and off weightbearing [12]. Due to the absence or presence of symptoms, flexible flatfoot may be asymptomatic or symptomatic.
For the diagnosis of paediatric symptomatic flexible flatfoot, it is important to take into account the following factors: medical history of the paediatric patient, the degree of severity of subjective symptoms, physical findings obtained during the clinical examination, analysis of the obtained footprint, and diagnostic imaging studies, which may include weightbearing radiographs, bone scans, computed tomography (CT), and magnetic resonance imaging (MRI) [12].
To determine the degree of deformity, beside the footprints, a set of radiological parameters for assessing this deformity is used to measure the specific angles obtained by standard dorsoplantar and lateral radiographs of the weightbearing feet. There are numerous angles described in literature for diagnosis of flexible flatfoot. The procedure of determining these angles is often not easy and expeditious, and it depends on a quality of X-ray and skill of an observer. We noticed that a height of navicular bone is in proportion with a height of longitudinal arch of the foot. Therefore, this study was conducted to evaluate correlation of navicular bone height with most often used angles, heel valgus and a footprint in order to simplify procedure for definitive diagnosis.
Patients and methods
Subjects
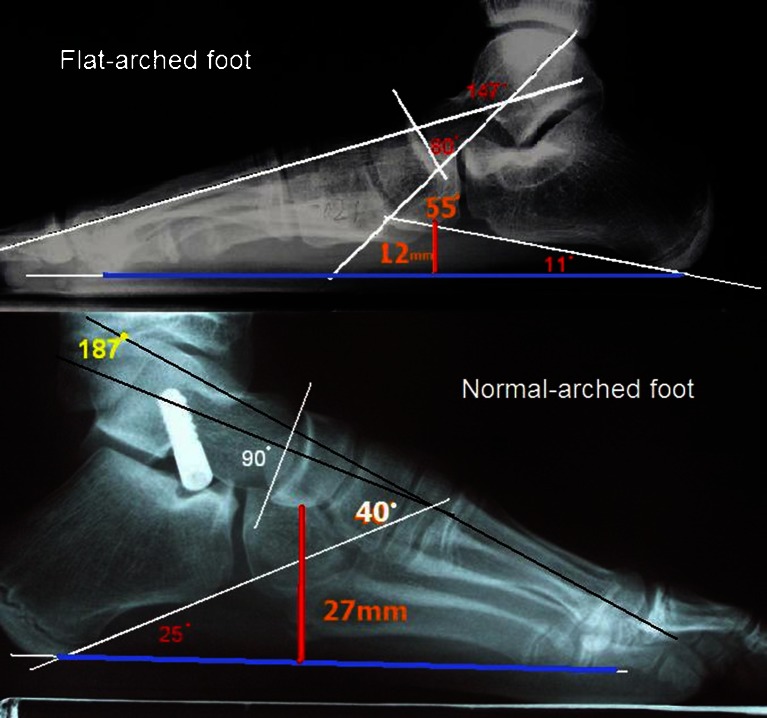
From 1997 to 2010, 218 children (436 ft) were treated surgically because of idiopathic flexible flatfoot. They were all evaluated clinically and radiologically pre-operatively and postoperatively. Lateral talometatarsal (Meary’s) angle, lateral talonavicular angle, lateral talocalcaneal angle and calcaneal pitch, heel valgus and Staheli’s arch index (SAI) were evaluated. From these 218 children, we included in the study 121 (242 ft) chosen children 78 boys (64.46 %; mean age = 11.08 year, standard deviation [SD] = 1.58) and 43 girls (35.52 %; mean age = 10.74 year, SD = 1.45) aged between eight and 15 years (mean age = 10.96 year, SD = 1.54) who had all pre-operative clinical and radiological values corresponding flatfoot, while postoperative values were within the normal range, i.e., postoperative values corresponded the values of the healthy population. This way we got a radiologically measured healthy group that was needed to compare with values of the group with flatfoot. To our knowledge, and in the literature review, we did not find such a big group with a radiologically measured of navicular bone height. For each foot we made the calculation of the navicular index pre-operatively and postoperatively by dividing the length of the longitudinal arch with navicular height, by which we removed possible mistakes that we would get with different sizes of X-ray images (Fig. 1). Also, the obtained values of navicular index were compared with all others measured values pre-operatively and postoperatively. Total follow up period was in the range of three to eight years (mean follow up period was five years).
Fig. 1.
calculation of the navicular index by dividing length of longitudinal arch with navicular height
Parental consent for participation was obtained for each child that was included in the study. The study was approved by the Medical ethics committees of the Clinical Hospital Center Rijeka, and School of Medicine, University of Rijeka, Croatia.
Surgical procedure
All patients included in this study have undergone the calcaneo-stop surgical procedure for anterograde screw implantation, which was previously described in detail in several papers [13–16]. Namely, in general or regional anesthesia with the patient in the supine position on the operating table, using the principles of minimal invasiveness (small incision in the line of the screw for placement in the talus), we use original BoneStar® titanium cannulated screw implant (Instrumentaria d.o.o., Zagreb, Croatia) length of 30–40 mm and three Kirschner (K) wires (length of 15 cm and diameter of 2 mm). Two of these three K-wires are used for percutaneous placement of the implant through the sinus tarsi into the talus from the bottom side (one K-wire for the right, and second K-wire for the left foot, if we treat both feet simultaneously), and third K-wire is used to determine the required length of the implant. There are three available lengths of implants - 30, 35 and 40 mm (total length of implant with its head) because of the different sizes of feet. After proper (parallel with facies articularis fibularis tibiae in the talus at 35° on coronal and sagittal plane) percutaneous placement of the wire in talus, using the drill and X-ray image enhancer, we make a small, longitudinally orientated incision in the skin and subcutaneous tissue with a total length of 8–10 mm. Surrounding ligamentary structures are separated with the help of scissors, and in such a way we clear the passage for the implant through sinus tarsi in the direction of the guide wire. With the help of cannulated wrench, we put the chosen implant on the guide wire and introduce it to the bottom surface of the talus with reverse-clockwise movement. Then, pressing the surrounding periost, with clockwise movement we introduce the implant in talus till it is fully implanted. Before covering the implant with surrounding ligamentary structures, subcutaneous tissue and skin, we make a radiological control to verify the proper position of the implant and then take out the guide wire using the drill. With this technique (using titanium cannulated screw implant with the help of the K-wire and X-ray image enhancer), installation and removal of the implant is facilitated, incision is only 8–10 mm long, and the time of the surgical procedure is shortened.
Postoperative rehabilitation protocol and assessment of the functional status
Another advantage of this minimally invasive surgical procedure is early rehabilitation; namely, the patient is mobilised the second day after surgery with full weightbearing of the treated feet and walks independently with the help of physiotherapist, without immobilization. Early postoperative protocol of learning a new form of walking lasts two weeks, after which the sutures are removed, and the child is fully trained for independent gait. The screw (implant) is installed up to three years, which presents a period that is normally required for proper formation of tarsal bones during growth, and during this entire time the child can carry out sports activities. Periodical examinations are every three months, and radiological controls of the implanted screw is every six months.
Statistical analysis
Measurement of correlation between the calculated navicular index and all above mentioned angles are expressed using the Pearson correlation coefficient (level of significance was p < 0.05) [17]. Degree of correlation between the calculated navicular index and all these measured angles were interpreted according to the guidelines by Colton: 0.00–0.24 = little/no relationship, 0.25–0.49 = fair degree of relationship, 0.50–0.74 = moderate/good relationship, and 0.75–1.00 = good/excellent correlation [18]. To determine the optimal cut-off value that can be achieved with the most effective discrimination between flatfeet and normal-arched feet using the navicular index we created recipient operating characteristic (ROC) analysis (level of significance was p < 0.05) [19, 20]. Indicators of diagnostic accuracy (sensitivity and specificity) were determined using the MedCalc program (MedCalc Software, Version 12.3.0, MedCalc Software bvba, Mariakerke, Belgium).
Results
Descriptive data about the values of measured parameters before and after surgery are listed in Table 1. As we stated earlier, for each foot we have made the calculation of the navicular index pre-operatively and postoperatively by dividing the length of longitudinal arch with navicular height. The values of navicular index before and after surgery are listed in Table 2. We obtained the values of navicular index for flatfeet in the interval from 4.75 to 31.2 (median 8.98, SD = 4.65), and a range for healthy feet was 3.58–22.6 (median 5.48, SD = 3.67). The degree of correlation between the values of measured parameters with calculated navicular index before and after surgery were interpreted according to the guidelines by Colton. Correlation of arch index values and values of other measured parameters is significant in majority, and degree of correlation according to the guidelines by Colton is good (Table 3). ROC test showed that the surface under the curve is 0.861; therefore the navicular index can be a good separator between the flatfoot and normal foot (Table 4). Overall, the boundary index (with 86 % sensitivity and 75 % specificity) of 6.7407 was obtained (Fig. 2). We defined normal values (median 5.48), cut-off value (6.7407) with 86 % sensitivity and 75 % specificity, and pathological values of navicular index (median 8.98) (Table 2, Fig. 2).
Table 1.
Values of measured parameters before and after surgery
| Valid N | Mean | Median | Minimum | Maximum | SD | |
|---|---|---|---|---|---|---|
| Before surgery | ||||||
| MA | 242 | 159.9711 | 161.0000 | 136.0000 | 171.0000 | 7.085371 |
| LTA | 242 | 52.2851 | 52.0000 | 36.0000 | 72.0000 | 6.324334 |
| TA | 242 | 79.1777 | 81.0000 | 51.0000 | 93.0000 | 7.340944 |
| CP | 242 | 11.9669 | 13.0000 | 0.0000 | 16.0000 | 2.753900 |
| HV | 242 | 13.3667 | 13.0000 | 6.0000 | 21.0000 | 3.252121 |
| SAI | 242 | 1.4052 | 1.3850 | 0.6900 | 2.8300 | 0.285243 |
| NAV | 242 | 15.6694 | 16.0000 | 5.0000 | 25.0000 | 4.333386 |
| AR | 242 | 157.3430 | 105.0000 | 293.0000 | 16.94885 | |
| After surgery | ||||||
| MA | 242 | 178.1208 | 179.0000 | 161.0000 | 190.0000 | 4.334109 |
| LTA | 242 | 38.7083 | 39.0000 | 20.0000 | 50.0000 | 4.295363 |
| TA | 242 | 92.3417 | 92.0000 | 82.0000 | 104.0000 | 3.651092 |
| CP | 242 | 17.8083 | 17.0000 | 9.0000 | 27.0000 | 3.330588 |
| HV | 242 | 1.8375 | 2.0000 | −3.0000 | 10.0000 | 1.979669 |
| SAI | 242 | 0.7132 | 0.7100 | 0.3700 | 1.5600 | 0.149897 |
| NAV | 242 | 30.0125 | 30.0000 | 15.0000 | 43.0000 | 5.433879 |
| AR | 242 | 158.3583 | 104.0000 | 203.0000 | 16.67273 | |
AR arch, CP calcanela pitch, HV heel valgus, LTA lateral talonavicular angle, MA Meary’s angle, SAI Staheli’s arch index, SD standard deviation, TA talocalcaneal angle, Valid N valid number, NAV height of navicular bone
Table 2.
Values of navicular index before and after surgery
| Valid N | Mean | Median | Minimum | Maximum | SD | |
|---|---|---|---|---|---|---|
| NI before surgery | 242 | 10.55973 | 8.976190 | 4.750000 | 31.20000 | 4.651019 |
| NI after surgery | 242 | 6.53162 | 5.479475 | 3.585366 | 22.60000 | 3.673888 |
NI navicular index, SD standard deviation, Valid N valid number
Table 3.
Correlations between values of measured parameters with navicular index before and after surgery
| Mean | SD | r(X, Y) | r2 | t | p | N | Constant - dep: Y | Slope - dep: Y | Constant - dep: X | Slope - dep: X | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before surgery | |||||||||||
| MA | 159.97 | 7.09 | |||||||||
| NI | 10.56 | 4.65 | −0.57 | 0.33 | −10.77 | 0.0000 | 242 | 70.48 | −0.37 | 169.15 | −0.87 |
| LTA | 52.29 | 6.32 | |||||||||
| NI | 10.56 | 4.65 | 0.18 | 0.03 | 2.80 | 0.0056 | 242 | 3.73 | 0.13 | 49.73 | 0.24 |
| TA | 79.18 | 7.34 | |||||||||
| NI | 10.56 | 4.65 | −0.36 | 0.13 | −5.98 | 0.0000 | 242 | 28.63 | −0.23 | 85.18 | −0.57 |
| CP | 11.97 | 2.75 | |||||||||
| NI | 10.56 | 4.65 | −0.56 | 0.31 | −10.46 | 0.0000 | 242 | 21.87 | −0.95 | 15.47 | −0.33 |
| HV | 13.37 | 3.25 | |||||||||
| NI | 10.56 | 4.65 | 0.32 | 0.10 | 5.13 | 0.000001 | 242 | 4.53 | 0.45 | 11.04 | 0.22 |
| SAI | 1.40 | 0.28 | |||||||||
| NI | 10.56 | 4.65 | 0.07 | 0.01 | 1.12 | 0.2658 | 242 | 8.91 | 1.17 | 1.36 | 0.004 |
| After surgery | |||||||||||
| MA | 178.12 | 4.33 | |||||||||
| NI | 6.53 | 3.67 | −0.23 | 0.05 | −3.58 | 0.000417 | 242 | 40.66 | −0.19 | 179.86 | −0.27 |
| LTA | 38.71 | 4.30 | |||||||||
| NI | 6.53 | 3.67 | −0.21 | 0.05 | −3.36 | 0.000918 | 242 | 13.57 | −0.18 | 40.33 | −0.25 |
| TA | 92.34 | 3.65 | |||||||||
| NI | 6.53 | 3.67 | 0.06 | 0.004 | 0.93 | 0.353039 | 242 | 0.94 | 0.06 | 91.95 | 0.06 |
| CP | 17.81 | 3.33 | |||||||||
| NI | 6.53 | 3.67 | −0.25 | 0.06 | −4.06 | 0.000066 | 242 | 11.53 | −0.28 | 19.32 | −0.23 |
| HV | 1.84 | 1.98 | |||||||||
| NI | 6.53 | 3.67 | −0.02 | 0.0004 | −0.31 | 0.753680 | 242 | 6.60 | −0.038 | 1.91 | −0.01 |
| SAI | 0.71 | 0.15 | |||||||||
| NI | 6.53 | 3.67 | −0.01 | 0.0003 | −0.28 | 0.779372 | 242 | 6.85 | −0.45 | 0.72 | −0.0007 |
Constant - dep: X - , Constant - dep: Y - , CP calcanela pitch, HV heel valgus, LTA lateral talonavicular angle, N number, MA Meary’s angle, r correlation coefficient, r2 coefficient of determination, SAI Staheli’s arch index, SD standard deviation, Slope - dep: X - ,Slope - dep: Y - , t - , TA - talocalcaneal angle, X - , Y -
Table 4.
ROC test
| Variable | index |
| Classification variable | diagnosis |
| Sample size | 484 |
| Positive group : diagnosis = 1 (flatfeet) | 242 |
| Negative group : diagnosis = 0 (healthy feet) | 242 |
| Disease prevalence (%) | unknown |
| Area under the ROC curve (AUC) | 0.861 |
| Standard Error a | 0.0174 |
| 95 % Confidence Interval b | 0.827 to 0.891 |
| z statistic | 20.740 |
| Significance level P (Area = 0.5) | 0.0001 |
aDeLong et al. [20]
bBinomial exact
Fig. 2.
ROC curve
Discussion
The most important finding of this study is the ability to prove that navicular index can be introduced as a new parameter for differentiating flatfoot from normal-arched foot. Despite the fact that over the last few decades various methods for diagnosing flatfoot were proposed, until today there is not one, uniform, measure for diagnosing flatfoot.
The relationship between the clinical and radiographic measures of foot posture was also explored in several previously published studies [21–24]. Main findings of these studies were that clinical measures were more strongly associated with the radiographic angles obtained from the lateral view. For this reason lateral talometatarsal (Meary’s) angel, calcaneal pitch, lateral talocalcaneal and talonavicular angel, footprint and heel valgus normative foot values were taken from literature and used to recruit patients with flat-arched feet in our study. Data from these patients were subsequently used to define the boundary between normal- and flat-arched feet. These pieces of information were then used to recruit participants with normal-arched feet [1, 2, 4–6, 10–12, 25].
To the best of our knowledge, there is no previous report in the literature about measuring the height of navicular bone with radiological methods and using mathematical methods to make it independent of size of the feet and distance of the feet from the source of X-ray beam.
Given our experience to date, we believe that it is much easier, more precise and with fewer mistakes, to measure the length of the foot arch and the height of the navicular bone than to measure the axis of the talus, navicular or calcaneus bone. Every above mentioned parameter was compared with navicular index and they were in correlation. Therefore, to determine the status of the feet, it is enough to measure two distances which speed up and simplify the procedure for establishing the diagnosis.
In conclusion, the height of navicular bone (navicular index) can be used fiducially, without measures of other angles, to diagnose flexible flat feet. We defined normal values (median 5.48), cut-off value (6.7407) with 86 % sensitivity and 75 % specificity, and pathological values of navicular index (median 8.98) (Table 2, Fig. 2). Therefore, navicular index can be used reliably, without measures of other parameters, to differentiate flatfoot from normal-arched foot.
Acknowledgments
Conflict of interest statement
All authors disclose any potential conflicts of interest, including specific financial interests relevant to the subject of their manuscript.
Competing interests
None.
Funding
This work was supported by grants from the Primorsko-goranska County of the Republic of Croatia.
Ethics approval
The study was approved by the Medical ethics committees of the Clinical Hospital Center Rijeka, and School of Medicine, University of Rijeka, Croatia.
References
- 1.Lovett HW, Dane J (1896) The affections of the arch of the foot commonly classified as flat-foot. J Bone Joint Surg Am s1–8:78–92.
- 2.Pauk J, Griskevicius J. Ground reaction force and support moment in typical and flat-feet children. Mechanika. 2011;17:93–96. doi: 10.5755/j01.mech.17.1.209. [DOI] [Google Scholar]
- 3.Foot Health Facts. The official consumer website of American College of Foot and Ankle Surgeons™. http://www.foothealthfacts.org/footankleinfo/pediatric-flatfoot.htm (accessed 30/09/2012).
- 4.Trott AW. Children’s foot problems. Orthop Clin North Am. 1982;13:641–654. [PubMed] [Google Scholar]
- 5.Caselli MA, Sobel E, McHale KA. Pedal manifestations of musculoskeletal disease in children. Clin Podiatr Med Surg. 1998;15:481–497. [PubMed] [Google Scholar]
- 6.Harris EJ. The oblique talus deformity. What is it, and what is its clinical significance in the scheme of pronatory deformities? Clin Podiatr Med Surg. 2000;17:419–442. [PubMed] [Google Scholar]
- 7.Hefti F. Foot pain. Orthopade. 1999;28(2):173–179. doi: 10.1007/PL00003594. [DOI] [PubMed] [Google Scholar]
- 8.Kumar SJ, Cowell HR, Ramsey PL. Foot problems in children. Part 1. Vertical and oblique talus. Instr Course Lect. 1985;31:235–251. [PubMed] [Google Scholar]
- 9.Kumar SJ, Ramsey PL. Vertical and oblique talus (a diagnostic dilemma) Orthop Trans. 1977;1:108. [Google Scholar]
- 10.Sullivan JA. Pediatric flatfoot (evaluation and management) J Am Acad Orthop Surg. 1999;7:44–53. doi: 10.5435/00124635-199901000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Tonnis D. Skewfoot. Orthopade. 1986;15:174–183. [PubMed] [Google Scholar]
- 12.Harris EJ, Vanore JV, Thomas JL, et al. Diagnosis and treatment of pediatric flatfoot. J Foot Ankle Surg. 2004;43:341–373. doi: 10.1053/j.jfas.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Roth S, Sestan B, Tudor A, Ostojic Z, Sasso A, Durbesic A. Minimally invasive calcaneo-stop method for idiopathic, flexible pes planovalgus in children. Foot Ankle Int. 2007;28(9):991–995. doi: 10.3113/FAI.2007.0991. [DOI] [PubMed] [Google Scholar]
- 14.Roth S. Minimal invasive calcaneo-stop method in cases of pes planovalgus in childhood with “BoneStar®” implant. J Child Orthop. 2007;1(suppl 1):25. [Google Scholar]
- 15.Roth S, Durbesic A, Bajok I. Treatment of the flexible flatfoot in children with the modified calcaneo-stop method with BoneStar® implant. J Child Orthop. 2011;5(suppl 1):S1–S35. [Google Scholar]
- 16.Kellermann P, Roth S, Gion K, Boda K, Tóth K. Calcaneo-stop procedure for paediatric flexible flatfoot. Arch Orthop Trauma Surg. 2011;131(10):1363–1367. doi: 10.1007/s00402-011-1316-3. [DOI] [PubMed] [Google Scholar]
- 17.Gillham EM. A life of Sir Francis Galton: from African exploration to the birth of Eugenics. 1. Oxford: Oxford University Press; 2001. p. 432. [Google Scholar]
- 18.Colton T (1974) Statistics in medicine, 1st edn. Little: Brown & Company, Boston, pp 372
- 19.Zhou XH, McClish DK, Obuchowski NA. Statistical methods in diagnostic medicine. 2. New York: Wiley; 2011. p. 545. [Google Scholar]
- 20.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. doi: 10.2307/2531595. [DOI] [PubMed] [Google Scholar]
- 21.Williams DS, McClay IS. Measurements used to characterize the foot and the medial longitudinal arch: reliability and validity. Phys Ther. 2000;80:864–871. [PubMed] [Google Scholar]
- 22.Shrader JA, Popovich JM, Jr, Gracey GC, et al. Navicular drop measurement in people with rheumatoid arthritis: interrater and intrarater reliability. Phys Ther. 2005;85:656–664. [PubMed] [Google Scholar]
- 23.Murley GS, Menz HB, Landorf KB. A protocol for classifying normal- and flat-arched foot posture for research studies using clinical and radiographic measurements. J Foot Ankle Res. 2009;2:22. doi: 10.1186/1757-1146-2-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graham ME, Jawrani NT, Chikka A. Radiographic evaluation of navicular position in the sagittal plane-correction following an extraosseous talotarsal stabilization procedure. J Foot Ankle Surg. 2011;50:551–557. doi: 10.1053/j.jfas.2011.04.027. [DOI] [PubMed] [Google Scholar]
- 25.Cornwall MW, Mc Poil TG. Relative movement of the navicular bone during normal walking. Foot Ankle Int. 1999;20:507–512. doi: 10.1177/107110079902000808. [DOI] [PubMed] [Google Scholar]