Abstract
Purpose
The purpose of this study was to compare the results of hallux valgus surgery between feet fixed with Kirschner wires and those fixed with a plate and screws.
Methods
Between December 2008 and November 2009, 53 patients (62 feet) were treated with proximal chevron osteotomy and distal soft tissue procedure for symptomatic moderate to severe hallux valgus deformity. Thirty-four patients (41 feet) were stabilised with Kirschner wires (K-wire group) and 19 patients (21 feet) were stabilised with a locking plate (plate group). Clinical results were assessed using American Orthopaedic Foot and Ankle Society (AOFAS) score. Radiographic parameters were compared between these groups. Recurrence rate at the last follow-up was compared between the K-wire and plate groups.
Results
Mean AOFAS score was lower in the plate group, however, the difference between the groups was not statistically significant in AOFAS score at the last follow-up. Hallux valgus angle and intermetatarsal angle were significantly larger in the plate group at the last follow-up. Mean 1–2 metatarsal (MT) distance on immediately postoperative radiographs was significant larger in the plate group. Four (9.8 %) of the 41 feet in the K-wire group and 7 (33.3 %) of the 21 feet in the plate group showed hallux valgus recurrence at the last follow-up. The plate group had a significantly higher risk of recurrence than the K-wire group.
Conclusions
Fixation of proximal chevron osteotomy using a plate and screws has a greater risk of hallux valgus recurrence than fixation using Kirschner wires.
Introduction
Increased intermetatarsal angle can be adequately corrected with proximal metatarsal osteotomy [1, 2]. However, transfer metatarsalgia often occurs due to the long moment arm of the distal fragment and insecure fixation. Accordingly, several different methods have been introduced to enhance the stability of the fixation [3–6].
Fixation using Kirschner wires is easily performed, but has several problems, such as less capacity to stabilise the osteotomy, pin migration, skin irritation, and the necessity of pin removal. Although fixation using plate is a more complicated procedure and requires more soft tissue dissection [7], it has been reported to achieve secure fixation, to be less liable to cause skin irritation, and to have a lower likelihood of hardware removal than fixation using Kirschner wires.
Varner et al. [7] reported that a dorsal plate is biomechanically more stable than a single cancellous screw when applied to proximal crescentic osteotomy. Gallentine et al. [5] concluded that a proximal chevron osteotomy fixed with low profile locking plate demonstrates good stability and less complication associated with hardware. No previous clinical study has compared the results of proximal osteotomy according to the method of stabilisation by Kirschner wires and a plate and screws.
We postulated that fixation with Kirschner wires would have better results than fixation with a plate and screws. The aim of this study was to compare the clinical and radiographic results of hallux valgus surgery between the feet fixed with Kirschner wires and those fixed with a plate and screws
Materials and methods
The study was approved by our Institutional Review Board. We retrospectively reviewed 80 consecutive proximal chevron osteotomies in 69 patients with symptomatic moderate to severe hallux valgus deformity (hallux valgus angle of ≥20° and intermetatarsal angle of ≥12°) performed by a single surgeon between December 2008 and November 2009. The first 44 patients (53 feet) were stabilised with Kirschner wires (K-wire group) and the latter 40 patients (45 feet) were stabilised with a 2.4-mm mini locking plate (Synthes, USA) (plate group). Thirteen patients (13 feet) were lost to follow-up and three patients (five feet) were excluded due to the absence of a medial sesamoid. Exclusion criteria included the following conditions: rheumatoid arthritis, hallux rigidus, and failed previous hallux valgus surgery. Thus finally, 53 patients (62 feet) were included in this study, of which 34 patients (41 feet) were in the K-wire group and 19 patients (21 feet) were in the plate group. All patients were female, and mean patient age was 52 years (range 25–68 years) in the K-wire group and 52.2 years (range 19–75 years) in the plate group. Mean duration of follow-up was 15.3 months (range 12–31 months) in the K-wire group, and 16.9 months (range 12–28 months) in the plate group. The two groups were similar in terms of sex, age, and duration of follow-up (P > 0.05). Closing wedge osteotomy of the proximal phalanx was performed in 41 patients (47 feet) with residual hallux valgus deformity after proximal chevron osteotomy.
Clinical results were assessed using the AOFAS hallux metatarsophalangeal interphalangeal scale [8] and the VAS for pain. Although the AOFAS score is not validated, it is commonly referred to in the literature. We therefore we used it in an attempt to enhance extrapolation of our results.
Hallux valgus angle, intermetatarsal angle, and sesamoid position were compared between the groups. To avoid potential bias, an independent observer, who was not part of the operative team, assessed the radiographs. The radiographic parameters were measured preoperatively, immediately postoperatively, at six weeks, three months, six months after surgery, and at the last follow-up. Hallux valgus angle was measured as the angle between the line from the centre of the proximal articular surface of the first metatarsal to the centre of the first metatarsal head and the line connecting the midpoints of the proximal and distal articular surfaces of the proximal phalanx [9]. Intermetatarsal angle was measured as the angle between the line of first metatarsal and the line bisecting the diaphyseal portions of second metatarsal bone. The position of the medial sesamoid, in relationship to the longitudinal axis of the first metatarsal on dorsoplantar weightbearing radiograph, was graded from I to VII, as described by Hardy-Clapham [10].
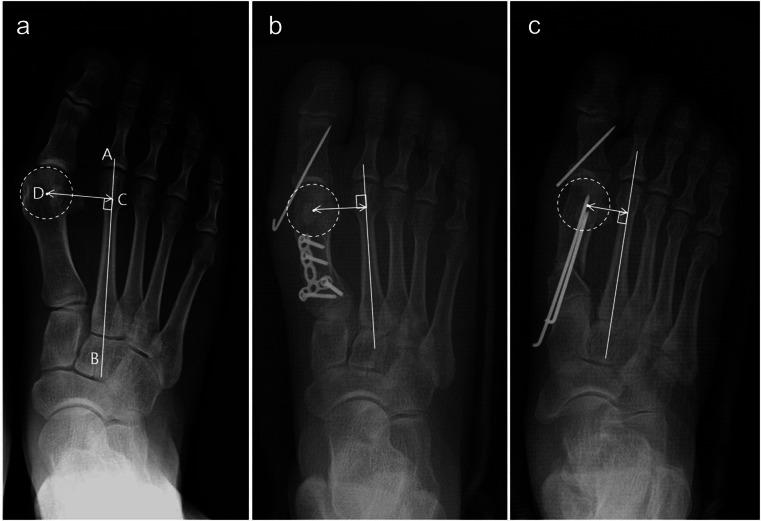
To compare the degree of lateral translation of the first metatarsal head, a first to second MT distance was measured on the immediately postoperative radiograph. This was defined as the shortest distance between the centre of the first metatarsal head and the longitudinal axis of the second metatarsal (Fig. 1). MT declination angle was measured to assess the degree of dorsiflexion of the first metatarsal after surgery. This was defined as the angle between the longitudinal axis of first metatarsal and the line parallel to the plantar foot on standing lateral views. Preoperative metatarsus adductus angle was measured as described by Kilmartin et al. [11] to assess the influence of the metatarsus adductus angle to the recurrence of deformity.
Fig. 1.
a A preoperative radiograph of a 53-year-old woman with hallux valgus. The 1–2 MT distance (CD) was measured as the shortest distance between the centre of the first metatarsal head (D) and the longitudinal axis of the second metatarsal (AB). b An immediately postoperative radiograph showed wide 1–2 MT distance after stabilisation using locking plate and screws. c An immediately postoperative radiograph of a 36-year-old woman showed lateral translation of the metatarsal shaft and narrow 1–2 MT distance after stabilisation using Kirschner wires
Immediately postoperative distal metatarsal articular angle (DMAA) was compared between the groups. DMAA determines the relationship between the articular surface of the distal first metatarsal and the longitudinal axis of the first metatarsal. Because the margin of the distal articular surface could not be defined on several preoperative radiographs, only immediately postoperative DMAA was compared.
Recurrence of hallux valgus was defined as a hallux valgus angle of ≥20°, and recurrence rate at the last follow-up was compared between the K-wire and plate groups. We evaluated the relative risk for the recurrence of hallux valgus between the two groups.
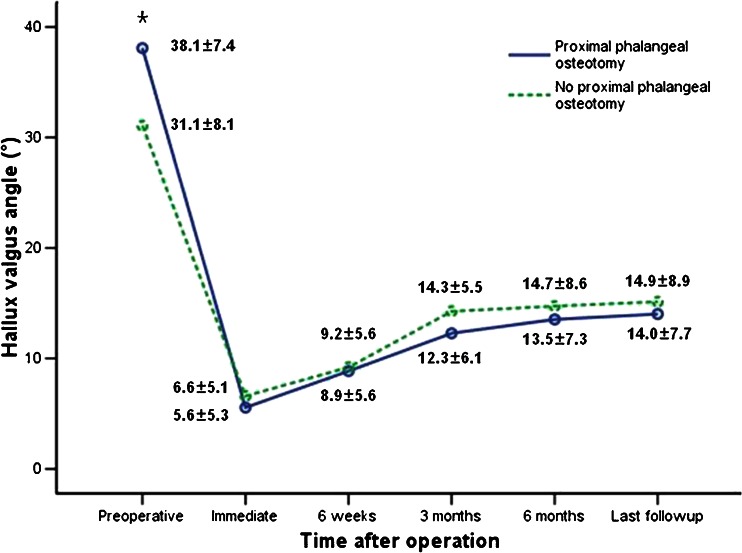
An additional study was conducted to determine the effect of proximal phalangeal osteotomy because this can decrease the postoperative hallux valgus angle. Thus, the feet were divided into two groups based on whether proximal phalangeal osteotomy was performed or not. Changes in hallux valgus angle with respect to time after surgery were compared between the two groups. In addition, the association between proximal phalangeal osteotomy and recurrence were evaluated.
Surgical technique
A seven centimetre medial incision was made along the inferior margin of the first metatarsal. A full thickness dorsal flap, including skin and subcutaneous tissue, was then elevated to the first web space, just superficial to the extensor hallucis longus and brevis. The tendinous part of the adductor was released and the deep transverse metatarsal ligament incised. A longitudinal incision was then made in the capsule along the dorsal margin of the lateral sesamoid. The adductor tendon was not transferred to the neck of the first metatarsal bone.
Proximal chevron osteotomy was performed on the medial aspect of the first metatarsal. The apex of the chevron was proximally located at seven millimetres distal to the first metatarso-cuneiform joint. The angle of each arm of the chevron was made at 30° to the metatarsal axis. After correction of intermetatarsal angle by translation, angulation and supination at the osteotomy site, two or three Kirschner wires of 1.6-mm diameter were inserted from proximal to distal into the metatarsal head. When residual hallux valgus deformity was apparent despite satisfactory correction of the intermetatarsal angle, closing wedge osteotomy was performed at the base of the proximal phalanx. The capsule of the first metatarsophalangeal joint was repaired using absorbable sutures without tension.
For plate fixation, after correction at the osteotomy site, two Kirschner wires of diameter 1.6 mm were inserted temporarily from the base of the metatarsal to the metatarsal head. The medial protruding portion of proximal fragment was removed flush with the distal fragment. A four-hole locking plate was then contoured to the bony surface and secured to the bone with locking screws of 2.4-mm diameter. Locking screws often could not be inserted due to distortion of the locking screw holes by bending of the plate, and cortical screws were inserted in that case.
Feet were placed in splints for about one week postoperatively. Weightbearing on the first ray was not allowed until the seventh postoperative week. The Kirschner wires used for fixation were removed during the ninth postoperative week.
Wilcoxon’s signed-rank test was used to compare preoperative and postoperative clinical results. The Mann–Whitney U test was used to compare age, duration of follow-up, and clinical and radiological results between the K-wire and plate groups, and to compare the hallux valgus angles between the groups with or without proximal phalangeal osteotomy. The chi-square test was used to analyse the association between fixation method and recurrence, and between proximal phalangeal osteotomy and recurrence. For all tests, P values of <0.05 were considered significant.
Results
No significant difference in AOFAS and VAS scores was observed at the last follow-up between the groups (Table 1).
Table 1.
Clinical results between the K-wire and plate groups
| Group | AOFAS score | VAS | ||||
|---|---|---|---|---|---|---|
| Preoperative | Last follow-up | P-value | Preoperative | Last follow-up | P-value | |
| K-wire group | 46.5 ± 5.8 | 88.8 ± 7.0 | <0.001 | 6.6 ± 1.0 | 2.1 ± 1.4 | <0.001 |
| Plate group | 43.5 ± 10.0 | 85.4 ± 9.2 | <0.001 | 6.4 ± 1.0 | 1.7 ± 1.3 | <0.001 |
| P-value | 0.369 | 0.244 | 0.407 | 0.198 | ||
AOFAS American Orthopaedic Foot and Ankle Society, VAS visual analogue scale
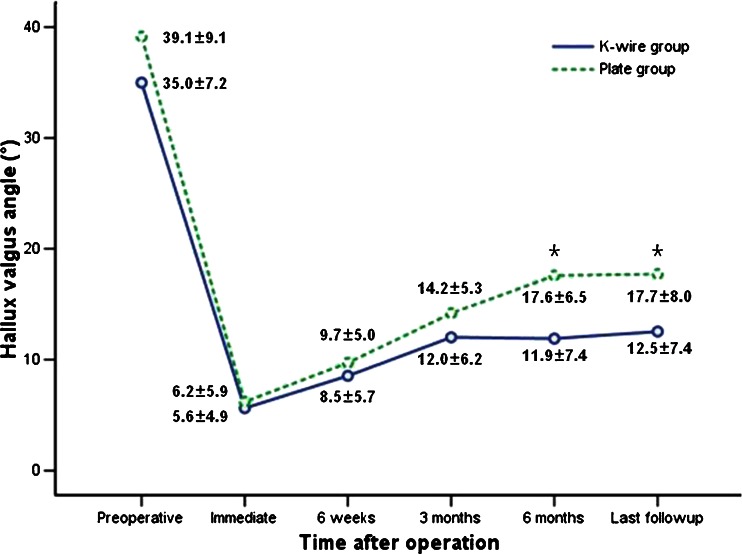
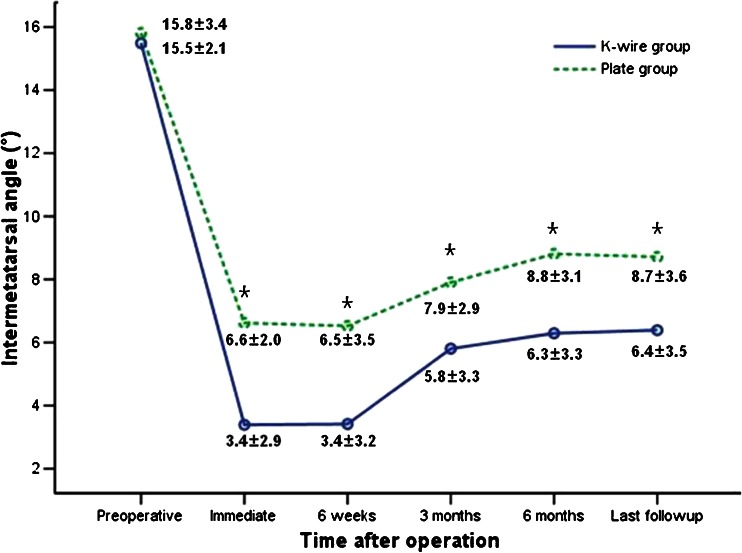
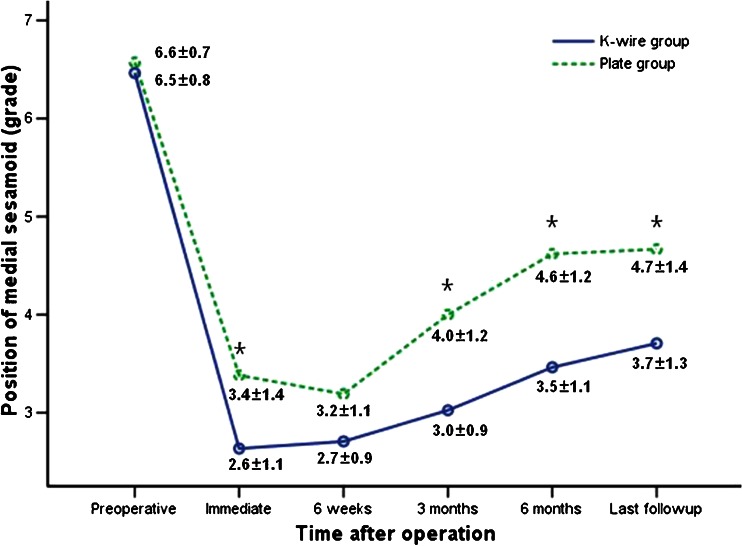
Changes in hallux valgus angle, intermetatarsal angle, and sesamoid position with respect to time after surgery in the K-wire and plate groups are shown in Figs. 2, 3 and 4. Preoperative hallux valgus angle, intermetatarsal angle, and sesamoid position were not different between the groups. No significant difference in hallux valgus angle was observed between two groups until three months after surgery. Hallux valgus angle was significantly larger in the plate group compared to the K-wire group from six months after surgery. Intermetatarsal angle was significantly larger in the plate group compared to those in the K-wire group at all time points after surgery. Mean 1–2 MT distance on immediately postoperative radiograph was significantly larger in the plate group. Mean change of MT declination angle measured preoperatively and at the last follow-up was not significantly different between the groups. No significant difference was observed in preoperative metatarsus adductus angle and immediately postoperative DMAA between the groups (Table 2).
Fig. 2.
Graph showing the change in the hallux valgus angle over time in the K-wire and plate groups (*P < 0.05)
Fig. 3.
Graph showing the change in the intermetatarsal angle over time in the K-wire and plate groups (*P < 0.05)
Fig. 4.
Graph showing the change in the medial sesamoid position over time in the K-wire and plate groups (*P < 0.05)
Table 2.
Radiographic results between the K-wire and plate groups
| Group | Postoperative 1–2 MT distance (mm) | MT declination angle (°) | Postoperative DMAA (°) | Preoperative MAA (°) | ||
|---|---|---|---|---|---|---|
| Preoperative | Last followup | Mean decrease | ||||
| K-wire group | 23.3 ± 3.2 | 22.4 ± 3.0 | 18.4 ± 6.5 | 4.0 ± 6.6 | 14.2 ± 4.2 | 12.5 ± 5.8 |
| Plate group | 25.8 ± 2.4 | 22.4 ± 3.6 | 20.2 ± 5.3 | 2.2 ± 4.4 | 14.8 ± 4.3 | 11.0 ± 5.5 |
| P-value | 0.003 | 0.404 | 0.348 | 0.461 | 0.917 | 0.398 |
MT metatarsal, DMAA distal metatarsal articular angle, MAA metatarsus adductus angle
Four (9.8 %) of the 41 feet in the K-wire group and seven (33.3 %) of the 21 feet in the plate group showed hallux valgus recurrence at the last follow-up. At the last follow-up, hallux valgus angle was 20–25° in two feet (50 %), 26–30° in one foot (25 %), and ≥31° in one foot (25 %) in the K-wire group and 20–25° in five feet (71.4 %), 26–30° in one foot (14.3 %), and ≥31° in one foot (14.3 %) in the plate group. The plate group had a significantly higher risk of recurrence than the K-wire group (P = 0.029).
Thirty (73.2 %) of the 41 feet in the K-wire group and 17 (81.0 %) of the 21 feet in the plate group underwent proximal phalangeal osteotomy, and there was no difference in the rate of proximal phalangeal osteotomy between the groups (P = 0.498). No significant difference of postoperative hallux valgus angle was observed between the groups with or without proximal phalangeal osteotomy (Fig. 5). At the last follow-up, recurrence occurred in two (13.3 %) of the 15 feet in the no proximal phalangeal osteotomy group and nine (19.1 %) of the 47 feet in the proximal phalangeal osteotomy group. No significant difference in relative risk of recurrence was observed between these two groups (P = 0.610).
Fig. 5.
Graph showing the change in the hallux valgus angle according to the performance of proximal phalangeal osteotomy (*P < 0.05)
Twelve (57.1 %) of the 21 feet had irritation from prominent plate, which was treated by removal of the hardware. One patient had transfer metatarsalgia due to severe dorsal malunion in the K-wire group, and this patient required orthoses. No pin track infection, pin migration, and non-union occurred in any patient.
Discussion
This study was performed to compare the clinical and radiographic results of proximal chevron osteotomy between the two groups stabilised with two different methods, those fixed with Kirschner wires and those fixed with a plate. Clinical results were similar between the two groups; however, the plate group had greater risk for recurrence of hallux valgus.
The main advantage of proximal chevron osteotomy is the versatility of correction, thus every deformed component of the first metatarsal can be corrected [4, 12, 13]. Widened intermetatarsal angle is corrected by lateral angulation and translation of the distal fragment [4], and supination can be added at the time of correction. However, proximal chevron osteotomy is inherently unstable, because angulation at the osteotomy site makes a medial gap. The gap becomes even greater when the supination is added to the angulation. Therefore, various fixation methods, such as Kirschner wires, screws, and plates have been used to stabilise the osteotomy [3–6].
Stabilisation using screws is common, however, screws can be inadvertently inserted into the first metatarsocuneiform joint or may induce fracture of the dorsal cortical bridge. Furthermore, fixation with one or two screws cannot obtain sufficient stability in osteoporotic bone [14–16]. Another problem of screw fixation is that the loss of correction may occur as the screw compresses the osteotomy site, because the osteotomy site is very unstable due to a long lever arm and the gap at the osteotomy site.
Fixation using Kirschner wires has an advantage in that they can be inserted without disrupting the delicately corrected position; however, it is an insecure method of stabilisation [15]. The stability can be enhanced by adding transverse Kirschner wires to longitudinal Kirschner wires or by using multiple longitudinal Kirschner wires. However, irritation of soft tissue by Kirschner wires is frequent and hardware removal is necessary [17, 18].
Fixation using a plate was introduced to solve these problems of fixation, and has been reported to have an advantage of secure fixation without loss of correction and no need to remove hardware [5]. Plates were used for fixation of opening wedge osteotomy of the proximal metatarsal in most articles [19, 20]. In opening wedge osteotomy, correction is carried out by angulation in one plane. In contrast, in this study, a plate and screws were used to fix complex correction achieved by translation, angulation, and rotation along longitudinal axis. The main problem of plate fixation was that any available plate at present could not be accurately contoured to the irregular bony surface after proximal chevron osteotomy. If the plate is not precisely contoured to the bony surface, some loss of correction could occur during attachment of the plate to the bone. Although the plates used in this series were locking plates, locking screws often could not be inserted because locking holes were distorted by bending of the plate. Thus loss of reduction often occurred while a plate was compressed to the bone. Therefore, a precontoured plate that requires less contouring after proximal chevron osteotomy is required to provide attachment without any loss of delicate correction in three planes. In our study, even though we tried to contour plates to the bony surface, 12 (51.7 %) of the 21 feet had irritation due to a prominent plate, which was resolved after plate removal in all cases.
In this series, mean hallux valgus angle was not different on immediately postoperative radiographs between the two groups, but was significantly larger in the plate group than the K-wire group from six months after surgery. Although the absolute value of intermetatarsal angle was corrected to a satisfactory level in both groups, mean intermetatarsal angle and 1–2 MT distance were larger in the plate group on immediately postoperative radiograph. Furthermore, mean sesamoid position was more displaced in the plate group. In summary, although immediately postoperative hallux valgus angle was not different between the K-wire and plate groups, the plate group had larger intermetatarsal angle, wider 1–2 MT distance, and a more displaced sesamoid position than the K-wire group. We believe these can be attributed to a loss of lateral translation during plate attachment to bone. DMAA [21] and metatarsus adductus angle [22] that were known risk factors for recurrence of hallux valgus were not found to be significantly different between the two groups.
In our study, four (9.8 %) of the 41 feet in the K-wire group and seven (33.3 %) of the 21 feet in the plate group experienced a recurrence. Comparing recurrence rate in this study with previous reports, the plate group had higher recurrence rate [19, 20, 23]. However, most studies either did not mention the recurrence rate or provided recurrence rates without a definition of recurrence [5, 19, 23, 24]. Mean postoperative hallux valgus angle in this study also was comparable to previous reports (Table 3). Furthermore, five (71.4 %) of all recurrent deformity feet in the plate group had hallux valgus angle of 20–25°. In the study, the plate group had the odds ratio of 4.6 times for the recurrence of hallux valgus compared to the K-wire group.
Table 3.
Comparison of results of fixation using plate after proximal metatarsal osteotomy
| Study | Method | Mean FU (months) | Number of cases | Preoperative HVA (°) | Postoperative HVA (°) | Incidence of recurrence | Definition of recurrence |
|---|---|---|---|---|---|---|---|
| Gallentine et al. [5] (2007) | Chevron | No mention | 20 | 33.3 (23–52) | 17.1 (8–36) | No mention | No mention |
| Chow et al. [22] (2008) | Crescentic | 96 | 26 | 34.2 | 17 | 2 (8 %) | No mention |
| Shurnas et al. [19] (2009) | Opening wedge | 27 | 84 | 30 (22–64) | 10 (−15–18) | 3 (3.6 %) | Increase in HVA ≥5° |
| Saragas et al. [18] (2009) | Opening wedge | 20 | 46 | 32.3 (21–48) | 17.6 (0–34) | 2 (4.3 %) | No mention |
| Randhawa et al. [23] (2009) | Opening wedge | 17 | 31 | 31.1 (15–49) | 17.4 (10–37) | No mention | No mention |
| Present study | Chevron | 17 | 21 | 39.1 (24–58) | 17.7 (3–35) | 7 (33.3 %) | HVA ≥20° at last FU |
FU follow-up, HVA hallux valgus angle
The dorsal malunion of the first metatarsal and transfer metatarsalgia after proximal metatarsal osteotomy have been reported in several studies [1, 4, 25, 26]. In this study, no significant difference was observed in a mean decrease of the MT declination angle between the two groups; however, one patient had transfer metatarsalgia due to severe dorsal malunion in the K-wire group. In this patient, the elevation of the first metatarsal was increased by 26° at the last follow-up.
Although mean AOFAS score was lower in the plate group (Table 1), AOFAS score was not statistically different between the groups. VAS score also was not different between the groups. We think the reason for good clinical outcome even in feet with recurrent hallux valgus is the relief of pain by great reduction of preoperative deformity. Because AOFAS score allocated most of the points on subjective pain and function [27], minimal difference of outward appearance was not reflected on the score. However, the patients with recurrent deformity often complained about unsatisfactory cosmetic results. Also we think increased hallux valgus angle may lead to gradual progression of deformity in longer-term follow-up.
One of the limitations of this study is the relatively small number of patients in the plate group. A power analysis was conducted to assess whether the sample size was sufficient to confirm a true difference in the recurrence rate between K-wire and plate groups. As a result, a minimum sample size of 48 in each group would be required to detect the difference with 80 % power at a 5 % significance level. Therefore, the sample size in our study was insufficient to detect that such a difference existed. However, increased recurrences in the plate group precluded further use of a plate for fixation and that was the reason for small number in plate group. The second limitation of this study is that the follow-up period was short; the results may change if we had followed the patients for a longer time. However, previous studies have compared one-year radiographic results with longer-term results and concluded that results did not change after one year [28, 29]. Hallux valgus angle and the intermetatarsal angle stabilised at six months after surgery in the K-wire group, although the sesamoid position continued to deteriorate in this study. Therefore, we believe that this study is meaningful with regard to the choice of stabilisation method after proximal metatarsal osteotomy.
In conclusion, fixation of proximal chevron osteotomy using a plate and screws has greater risk of hallux valgus recurrence than fixation using Kirschner wires.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Mann RA, Rudicel S, Graves SC. Repair of hallux valgus with a distal soft-tissue procedure and proximal metatarsal osteotomy. A long-term follow-up. J Bone Joint Surg Am. 1992;74:124–129. [PubMed] [Google Scholar]
- 2.Zettl R, Trnka HJ, Easley M, Salzer M, Ritschl P. Moderate to severe hallux valgus deformity: correction with proximal crescentic osteotomy and distal soft-tissue release. Arch Orthop Trauma Surg. 2000;120:397–402. doi: 10.1007/PL00013769. [DOI] [PubMed] [Google Scholar]
- 3.Amis JA, Porter DA. Correction augmentation and provisional fixation in proximal metatarsal osteotomies using Kirschner wires. Foot Ankle Int. 1999;20:752–753. doi: 10.1177/107110079902001114. [DOI] [PubMed] [Google Scholar]
- 4.Easley ME, Kiebzak GM, Davis WH, Anderson RB. Prospective, randomized comparison of proximal crescentic and proximal chevron osteotomies for correction of hallux valgus deformity. Foot Ankle Int. 1996;17:307–316. doi: 10.1177/107110079601700603. [DOI] [PubMed] [Google Scholar]
- 5.Gallentine JW, Deorio JK, Deorio MJ. Bunion surgery using locking-plate fixation of proximal metatarsal chevron osteotomies. Foot Ankle Int. 2007;28:361–368. doi: 10.3113/FAI.2007.0361. [DOI] [PubMed] [Google Scholar]
- 6.Sammarco GJ, Russo-Alesi FG. Bunion correction using proximal chevron osteotomy: a single-incision technique. Foot Ankle Int. 1998;19:430–437. doi: 10.1177/107110079801900703. [DOI] [PubMed] [Google Scholar]
- 7.Varner KE, Matt V, Alexander JW, Johnston JD, Younas S, Marymont JV, Noble PC. Screw versus plate fixation of proximal first metatarsal crescentic osteotomy. Foot Ankle Int. 2009;30:142–149. doi: 10.3113/FAI.2009.0142. [DOI] [PubMed] [Google Scholar]
- 8.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 9.Shima H, Okuda R, Yasuda T, Jotoku T, Kitano N, Kinoshita M. Radiographic measurements in patients with hallux valgus before and after proximal crescentic osteotomy. J Bone Joint Surg Am. 2009;91:1369–1376. doi: 10.2106/JBJS.H.00483. [DOI] [PubMed] [Google Scholar]
- 10.Hardy RH, Clapham JC. Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br. 1951;33-B:376–391. doi: 10.1302/0301-620X.33B3.376. [DOI] [PubMed] [Google Scholar]
- 11.Kilmartin TE, Barrington RL, Wallace WA. Metatarsus primus varus. A statistical study. J Bone Joint Surg Br. 1991;73:937–940. doi: 10.1302/0301-620X.73B6.1955440. [DOI] [PubMed] [Google Scholar]
- 12.Sammarco GJ, Brainard BJ, Sammarco VJ. Bunion correction using proximal Chevron osteotomy. Foot Ankle. 1993;14:8–14. doi: 10.1177/107110079301400102. [DOI] [PubMed] [Google Scholar]
- 13.Chuckpaiwong B. Comparing proximal and distal metatarsal osteotomy for moderate to severe hallux valgus. Int Orthop. 2012;36:2275–2278. doi: 10.1007/s00264-012-1656-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones C, Coughlin M, Petersen W, Herbot M, Paletta J. Mechanical comparison of two types of fixation for proximal first metatarsal crescentic osteotomy. Foot Ankle Int. 2005;26:371–374. doi: 10.1177/107110070502600505. [DOI] [PubMed] [Google Scholar]
- 15.Lian GJ, Markolf K, Cracchiolo A., 3rd Strength of fixation constructs for basilar osteotomies of the first metatarsal. Foot Ankle. 1992;13:509–514. doi: 10.1177/107110079201300904. [DOI] [PubMed] [Google Scholar]
- 16.Sammarco VJ, Acevedo J. Stability and fixation techniques in first metatarsal osteotomies. Foot Ankle Clin. 2001;6:409–432. doi: 10.1016/S1083-7515(03)00105-0. [DOI] [PubMed] [Google Scholar]
- 17.Ford TC, Maurer LM, Myrick KW. Cortical bone pin fixation: a preliminary report on fixation of digital arthrodeses and distal chevron first metatarsal osteotomies. J Foot Ankle Surg. 2002;41:23–29. doi: 10.1016/S1067-2516(02)80006-0. [DOI] [PubMed] [Google Scholar]
- 18.Thompson FM. Complications of hallux valgus surgery and salvage. Orthopedics. 1990;13:1059–1067. doi: 10.3928/0147-7447-19900901-19. [DOI] [PubMed] [Google Scholar]
- 19.Saragas NP. Proximal opening-wedge osteotomy of the first metatarsal for hallux valgus using a low profile plate. Foot Ankle Int. 2009;30:976–980. doi: 10.3113/FAI.2009.0976. [DOI] [PubMed] [Google Scholar]
- 20.Shurnas PS, Watson TS, Crislip TW. Proximal first metatarsal opening wedge osteotomy with a low profile plate. Foot Ankle Int. 2009;30:865–872. doi: 10.3113/FAI.2009.0865. [DOI] [PubMed] [Google Scholar]
- 21.Bonnel F, Canovas F, Poiree G, Dusserre F, Vergnes C. Evaluation of the Scarf osteotomy in hallux valgus related to distal metatarsal articular angle: a prospective study of 79 operated cases. Rev Chir Orthop Reparatrice Appar Mot. 1999;85:381–386. [PubMed] [Google Scholar]
- 22.Larholt J, Kilmartin TE. Rotational scarf and akin osteotomy for correction of hallux valgus associated with metatarsus adductus. Foot Ankle Int. 2010;31:220–228. doi: 10.3113/FAI.2010.0220. [DOI] [PubMed] [Google Scholar]
- 23.Chow FY, Lui TH, Kwok KW, Chow YY. Plate fixation for crescentic metatarsal osteotomy in the treatment of hallux valgus: an eight-year followup study. Foot Ankle Int. 2008;29:29–33. doi: 10.3113/FAI.2008.0029. [DOI] [PubMed] [Google Scholar]
- 24.Randhawa S, Pepper D. Radiographic evaluation of hallux valgus treated with opening wedge osteotomy. Foot Ankle Int. 2009;30:427–431. doi: 10.3113/FAI.2009.0427. [DOI] [PubMed] [Google Scholar]
- 25.Pearson SW, Kitaoka HB, Cracchiolo A, Leventen EO. Results and complications following a proximal curved osteotomy of the hallux metatarsal. Contemp Orthop. 1991;23:127–132. [PubMed] [Google Scholar]
- 26.Thordarson DB, Leventen EO. Hallux valgus correction with proximal metatarsal osteotomy: two-year follow-up. Foot Ankle. 1992;13:321–326. doi: 10.1177/107110079201300605. [DOI] [PubMed] [Google Scholar]
- 27.Lucijanic I, Bicanic G, Sonicki Z, Mirkovic M, Pecina M. Treatment of hallux valgus with three-dimensional modification of Mitchell’s osteotomy: technique and results. J Am Podiatr Med Assoc. 2009;99:162–172. doi: 10.7547/0980162. [DOI] [PubMed] [Google Scholar]
- 28.Okuda R, Kinoshita M, Morikawa J, Yasuda T, Abe M (2005) Proximal metatarsal osteotomy: relation between 1- to greater than 3-years results. Clin Orthop Relat Res 435:191–196 [PubMed]
- 29.Veri JP, Pirani SP, Claridge R. Crescentic proximal metatarsal osteotomy for moderate to severe hallux valgus: a mean 12.2 year follow-up study. Foot Ankle Int. 2001;22:817–822. doi: 10.1177/107110070102201007. [DOI] [PubMed] [Google Scholar]