Abstract
Purpose
The aim of this study was to examine the effect of an integrated care pathway (ICP) for total hip and knee arthroplasty (THA/TKA) on length of stay (LOS), day of surgery admission rate (DOSA) and postoperative length of stay (POLOS).
Methods
Three hundred and eight THAs and 299 TKAs were assessed in a retrospective before–after trial design. LOS, POLOS and DOSA were recorded for patients before and after introduction of the ICP. The ICP encompassed a patient education programme, specific daily management goals, variance mapping, daily facilitated meetings and a DOSA policy. Subgroup analysis according to age and gender was also performed.
Results
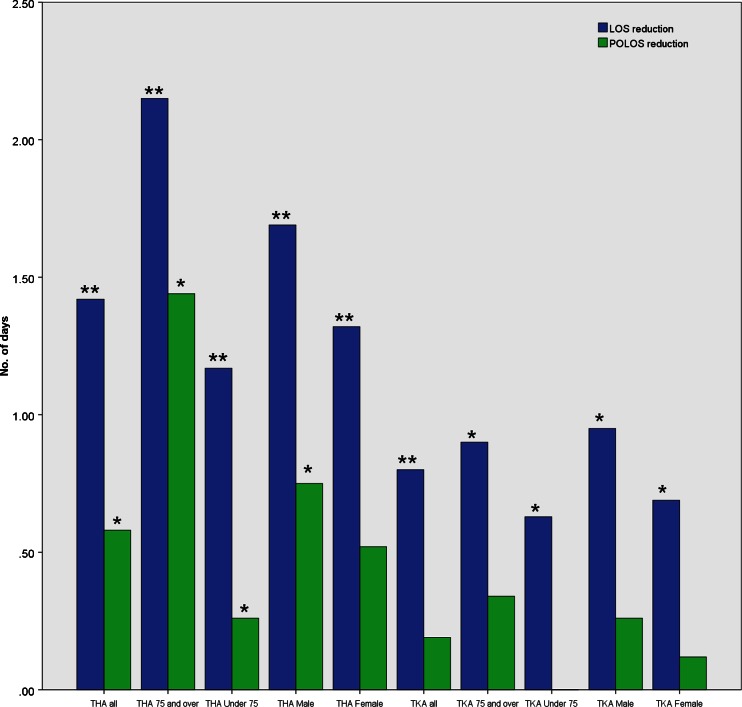
Mean LOS was significantly reduced by 1.4 (from 6.9 to 5.5) days for THA and 0.8 (from 6.4 to 5.6) days for TKA. Elderly patients and men achieved greater LOS reductions than their counterparts for both operations. Younger patients undergoing THA achieved a significantly higher DOSA rate than older patients (89 % vs 71 %, p = 0.010); however, this difference was not observed in the TKA population. Mean POLOS for THA was reduced by 0.6 (from 5.9 to 5.3) days, again with the greatest benefit seen in elderly and male patients. POLOS for TKA patients was not significantly affected by the ICP.
Conclusions
The introduction of an ICP reduced LOS by 1.4 days for THA and 0.8 days for TKA. Elderly and male patients benefitted most.
Introduction
In England in the financial year 2008–2009, more than 60,900 primary total knee arthroplasties (TKA) and over 57,600 total hip arthroplasties (THA) were carried out. Recent trends suggest this will increase further [1]. With the current financial climate in the UK National Health Service (NHS), the UK government is pledging to deliver £15–20 billion in savings in the health sector by 2013–2014 [2]. This has resulted in an emphasis on streamlining services. Integrated Care Pathways (ICPs) have been shown to reduce hospital length of stay (LOS) [3–8], complication rates [5] and readmission rates [4], and improve postoperative joint function in hospital [8] and at one year follow-up [3], improve quality of life [9] and aid in cost containment [3, 6, 7, 9] for patients undergoing arthroplasty. A recent Cochrane Review of 27 controlled clinical trials across all specialties concluded that ICPs, in general, reduce in-hospital complication rates and improve documentation without negatively impacting on LOS or cost [10]. A meta-analysis of 20 studies on the benefits of ICPs in arthroplasty came to the conclusion that ICPs reduced complication rate, LOS and cost [11].
However, a number of authors [5, 10–12] conclude that there is insufficient knowledge on which key elements of the ICP affect outcome. The aim of this study was to examine the effect of an ICP for lower-limb arthroplasty on LOS, including a subgroup analysis according to age and sex. There is substantial evidence for gender and age differences in the prevalence and severity of osteoarthritis [13] and functional outcome after arthroplasty [14–17], but to our knowledge, there is no published literature on the differential effects of an ICP according to age or gender.
Methods
Intervention: integrated care pathway
As part of the effective patient care programme launched at our hospital in 2006, a pathways group was created involving clinical, nursing and management leaders. In response to the success of the fractured neck of femur pathway, a multidisciplinary team (MDT) consisting of trust pathways lead, orthopaedic surgeon, nursing lead, physiotherapy lead, occupational therapy lead, orthopaedic manager and IT manager, was formed in January 2008 to design a pathway (Table 1) for lower-limb arthroplasty. The aim was to provide standardised, high-quality, cost-effective, evidence-based care. The scheme was piloted from March 2008 onwards and fully implemented by July 2008. From July 2008 onwards, all patients undergoing primary total hip (THA) or total knee (TKA) arthroplasty were treated on the pathway.
Table 1.
Key changes introduced as part of the lower-limb total joint replacement clinical pathway
| Lower-limb arthroplasty integrated care pathway |
|---|
| Noncompulsory patient education programme (including new information packs and facilitated session) |
| Paper-based integrated care pathway (ICP), including formalised specific patient management goals to replace patient notes |
| Staff education in the use of the ICP to overcome barriers to implementation |
| Variance mapping |
| Daily facilitated meetings (nurses, physiotherapists, occupational therapists) |
| Day of surgery admission policy |
Preoperative care
Patients were seen in the preassessment clinic two to six weeks prior to surgery. This involved a consultation with a surgeon or nurse specialist, further consultations with a physiotherapist and occupational therapist, blood tests and X-rays of the joint. Patients were given a questionnaire, returned prior to admission, regarding their home circumstances to identify the need for adaptive equipment. They were given information leaflets on the procedure and postoperative goals. An anaesthetic review was not part of the preassessment clinic.
The patient education programme consisted of an optional two-hour group session (ten–20 patients) two to four weeks prior to surgery. It was led by an orthopaedic nurse specialist along with a physiotherapist and occupational therapist. Patients were encouraged to bring a relative with them. The aims were to reduce anxiety for both patients and their relatives by outlining the patient’s journey [18] and discharge arrangements. A meeting with the members of the MDT was considered important to discourage patients from adopting the sick role and empowering them to take an active role in treatment and rehabilitation.
Operative care
Seven consultant surgeons and their trainees performed the operations. The Genesis II knee implant (12 % uncemented, 88 % cemented) and the Exeter (cemented and hybrid) hip system implant (60 % cemented, 26 % hybrid, 14 % uncemented) were used. Policies on anaesthesia or the use of lower-limb nerve blocks remained unchanged. No intra-articular pain relief was used in our unit. All TKAs received a low-vacuum drain and autologous reinfusion system (Astratech Healthcare, Mölndal, Sweden).
Postoperative care
Aggressive physiotherapy and occupational therapy from postoperative day (POD) one remained the standard. The ICP was used to formalise mobilisation goals (Table 2), and patients were mobilised with full weight bearing unless there were specific contraindications in the postoperative instructions. The therapy was adjusted on an individual basis in the light of the patient’s clinical condition and pain. Thromboprophylaxis and pain relief protocols remained unchanged. A referral to the community-supported orthopaedic discharge team was made if indicated, as well as the provision of home adaptive equipment. There was regular communication with patients and relatives. Follow-up included removal of clips in the community two weeks postsurgery and outpatient follow-up at six weeks, three to six months if required, and one year.
Table 2.
Day-to-day management goals for a patient undergoing total hip or knee arthroplasty
| Patient management goals | |
| Preadmission clinic | Preoperative bloods (FBC, U & E, clotting screen, G & S) |
| Preoperative radiograph | |
| Physiotherapy assessment | |
| Occupational therapy (OT) assessment | |
| Day of surgery (preoperative) | Consent form signed |
| Anaesthetic assessment | |
| Commence fluid chart, assess need for catheter | |
| Observations 4 hourly | |
| Nil by mouth 6 h for food, 3 h for clear fluids | |
| Nutrition risk assessment | |
| Pain score assessment explained | |
| Moving and handling risk assessment | |
| Falls risk assessment | |
| Waterlow pressure sore risk assessment | |
| Thromboprophylaxis: TED stockings + LMWH prescribed | |
| Discharge planning discussed with patient and relatives | |
| Return of home situation questionnaire | |
| IV antibiotics at induction (flucloxacillin unless penicillin allergic) | |
| Day of surgery (postoperative) | PCA |
| Autologous blood reinfusion | |
| 3x IV antibiotics | |
| IV fluid | |
| 30-min observations, including limb | |
| Check patient-passed urine (assess need for catheter) | |
| POD-1 | Discontinue PCA and prescribe step-down analgesia (regular oral paracetamol + regular weak opioid + oramorph as required for breakthrough pain) |
| Remove drain and dress site | |
| Wound-site dressing checked | |
| Postoperative blood tests: FBC, U & E, others as required | |
| Postoperative radiograph | |
| Oralisation of fluid intake | |
| Check pressure areas | |
| Deep breathing exercises | |
| Bed physiotherapy exercises | |
| Mobilise out of bed and transfer bed to chair with assistance | |
| POD-2 | Wound-site dressing change if heavily soiled |
| Drain-site dressing checked | |
| Dressed in own clothes to discourage sick role | |
| Expected discharge date finalised with MDT | |
| Sitting/standing exercises | |
| Sit to stand from chair | |
| Mobilise 10 m/to toilet with aids | |
| POD-3 | Review analgesia |
| Teach self-administration of LMWH | |
| Check OT equipment in place at home | |
| Independent standing balance without aids | |
| Independent with transfers | |
| Negotiate one step with aids | |
| POD-4 | Discharge documentation ready, including community referrals if indicated |
| Independent mobilisation (including sideways, backwards) with aids | |
| Negotiate stairs with aids | |
| Knee flexion to 90° while sitting (TKA only) | |
| POD-5 | Discharge home |
POD postoperative day, FBC full blood count, U & E urea and electrolytes, G & S group and screen, PCA patient-controlled analgesia, IV intravenous, MDT multidisciplinary team, LMWH low molecular weight heparin, OT occupational therapy, TKA total knee arthroplasty
Variance mapping
This was used for daily colour-coded documentation of a patient’s progress along the pathway. Amber indicated problems such as pain, vomiting or mobility issues; green indicated good progress; blue indicated fitness for discharge; pink indicated actual discharge. The variance mapping was discussed at daily meetings to identify patients not reaching pathway targets so that extra support could be provided.
Data collection
Data on age, sex, length of stay (LOS), postoperative LOS (POLOS) and day of surgery admission (DOSA) were collected retrospectively. A before-and-after pathway implementation analysis was chosen to compare the time period September 2007 to January 2008 (Pre-ICP) with September 2008 to January 2009 (Post-ICP). The period of development and initial piloting of the ICP was excluded to avoid contamination of the Pre-ICP results, i.e. Incorporation of researched evidence into their daily practice [19]. Inclusion criteria were THA or TKA within the above-specified periods. Exclusion criteria were revision arthroplasty, simultaneous bilateral arthroplasty, medically unrelated confounding factors (e.g. diagnosis of a brain tumour in the postoperative period). Exclusion criteria were kept lenient in comparison with other studies [4, 20] because the authors wanted to assess the effectiveness of a care pathway in normal clinical practice. All data was maintained in a Microsoft Excel spreadsheet (Microsoft Corp, Redmond, WA, USA).
Statistical analysis
SPSS statistics (version 17.0, SPSS Inc., Chicago, IL, USA) was used for all statistical analysis. LOS, POLOS and age comparisons between before and after cohorts were undertaken using a Mann–Whitney U test, as all three variables were shown to be non-normally distributed using the Shapiro–Wilks test. Transformation of data by using the natural logarithm did not result in normally distributed data, as in other studies [12]. Differences in sex ratio and DOSA rates were compared using a 2 × 2 χ2 test. Results were considered statistically significant at the 95 % confidence interval (CI) level and highly statistically significant at the 99.9 % CI level.
Results
Total hip arthroplasty
Three hundred and eighty-eight THAs were included (Table 3). Mean pre-ICP LOS was 6.9 (range three–22) days. After the introduction of the ICP, mean LOS was 5.5 (range two–20) days – a highly significant improvement of 1.4 days. Reduction in LOS was also found to be highly statistically significant in a subgroup analysis by age and sex. Patients over 75 years achieved a greater mean reduction in LOS than younger patients (2.2 vs 1.2 days). Male patients achieved a greater mean LOS reduction than female patients (1.7 vs 1.3 days). As LOS was shorter for male than for female patients pre-ICP (6.5 vs 7.2 days, p = 0.0043), this resulted in a widening of the sex gap to 1.1 days. DOSA rates increased significantly after introduction of the ICP to 83 % overall for THA. Patients under 75 years achieved a significantly higher DOSA rate than older patients (89 % vs 71 %, p = 0.010). Differences in DOSA rates between male and female patients were not statistically significant (90 % vs 79 %, p = 0.114). POLOS was significantly reduced for THA patients overall from 5.9 to 5.3 days. POLOS reduction remained significant in subgroup analysis according to age and for male patients but not for female patients. Older patients achieved a greater mean POLOS reduction than younger patients (1.4 vs 0.3 days). Male patients also achieved a greater mean reduction in POLOS than female patients (0.8 vs 0.5 days), widening the sex gap to 0.9 days.
Table 3.
Comparison between pre-ICP and post-ICP groups for THA
| All | Younger than 75 years | 75 years and older | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ICP | Post-ICP | Pre-ICP | Post-ICP | Pre-ICP | Post-ICP | Pre-ICP | Post-ICP | Pre-ICP | Post-ICP | |
| Number | 170 | 138 | 115 | 89 | 55 | 49 | 66 | 48 | 104 | 90 |
| Age (mean ± SD)/years | 68.9 ± 11.7 | 69.8 ± 11.3 | 62.9 ± 9.23 | 63.9 ± 9.84 | 81.2 ± 4.37 | 80.1 ± 4.14 | 66.8 ± 13.4 | 67.5 ± 12.3 | 70.1 ± 10.4 | 70.7 ± 10.6 |
| Male % | 38.6 % | 34.3 % | 41.7 % | 40.4 % | 32.1 % | 23.5 % | 100 % | 100 % | 0 % | 0 % |
| LOS (mean ± SD)/days | 6.94 ± 3.33 | 5.52 ± 3.11b | 5.91 ± 1.63 | 4.74 ± 2.03b | 9.09 ± 4.72 | 6.94 ± 4.12b | 6.52 ± 2.76 | 4.83 ± 2.91b | 7.21 ± 3.64 | 5.89 ± 3.17b |
| POLOS (mean ± SD)/days | 5.92 ± 3.35 | 5.34 ± 3.00a | 4.89 ± 1.63 | 4.63 ± 2a | 8.07 ± 4.73 | 6.63 ± 3.97a | 5.48 ± 2.78 | 4.73 ± 2.80a | 6.19 ± 3.64 | 5.67 ± 3.06 |
| DOSA % | 0.6 % | 82.6 %b | 0.9 % | 88.8 %b | 0 % | 71.4 %b | 0 % | 90.0 %b | 1.0 % | 78.9 %b |
ICP integrated care pathway, THA total hip arthroplasty, SD standard deviation, LOS length of stay, POLOS postoperative length of stay, DOSA days of surgery admission
aSignificance in the before/after comparison at the 95 % confidence level
bSignificance in the before/after comparison at the 99.9 % confidence level
Total knee arthroplasty
Two hundred and ninety-nine TKAs were included in this study (Table 4). The ICP reduced LOS from 6.4 to 5.6 days. Subgroup analysis yielded similar results as those for THA patients, with elderly and male patients achieving greater reductions in LOS than younger and female patients, respectively. However, differences between groups were much smaller (Fig. 1). The DOSA rate increased to 62 % for TKA patients, with no difference according to age. Male patients achieved a higher DOSA rate than female patients (76 % vs 59 %), but again, this was not statistically significant (p = 0.347). DOSA rate was not associated with age. POLOS for TKA patients was not significantly affected by the ICP introduction.
Table 4.
Comparison between pre-ICP and post-ICP groups for TKA
| All | Younger than 75 years | 75 years and older | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ICP | Post-ICP | Pre-ICP | Post-ICP | Pre-ICP | Post-ICP | Pre-ICP | Post-ICP | Pre-ICP | Post-ICP | |
| Number | 162 | 137 | 101 | 98 | 61 | 39 | 72 | 57 | 90 | 80 |
| Age (mean ± SD)/years | 71.2 ± 9.11 | 69.7 ± 8.49 | 65.8 ± 6.60 | 65.5 ± 5.84 | 80.0 ± 4.70 | 80.1 ± 3.71 | 71.7 ± 8.83 | 69.9 ± 9.21 | 70.8 ± 9.35 | 69.5 ± 8.00 |
| Male % | 44.4 % | 41.6 % | 46.5 % | 37.8 % | 41.0 % | 51.3 % | 100 % | 100 % | 0 % | 0 % |
| LOS (mean ± SD)/days | 6.44 ± 2.65 | 5.64 ± 2.72b | 6.08 ± 2.54 | 5.45 ± 2.81a | 7.03 ± 2.74 | 6.13 ± 2.45a | 6.49 ± 3.00 | 5.54 ± 2.82a | 6.40 ± 2.36 | 5.71 ± 2.67a |
| POLOS (mean ± SD)/days | 5.43 ± 2.64 | 5.24 ± 2.67 | 5.06 ± 2.53 | 5.06 ± 2.74 | 6.03 ± 2.74 | 5.69 ± 2.45 | 5.44 ± 2.99 | 5.18 ± 2.87 | 5.41 ± 2.34 | 5.29 ± 2.53 |
| DOSA % | 3.1 % | 62.0 %b | 2.0 % | 62.2 %b | 4.9 % | 61.5 %b | 2.8 % | 66.7 %b | 3.3 % | 58.8%b |
ICP integrated care pathway, THA total hip arthroplasty, SD standard deviation, LOS length of stay, POLOS postoperative length of stay, DOSA days of surgery admission
aSignificance in the before/after comparison at the 95 % confidence level
bSignificance in the before/after comparison at the 99.9 % confidence level
Fig. 1.
Comparison of the reduction in length of stay (LOS) and postoperative length of stay (POLOS) for patients undergoing total hip arthroplasty (THA) and those undergoing total knee arthroplasty (TKA), as well as subgroup analysis by age and sex
Age and sex
The observed differences in LOS reduction by age and sex prompted further analysis to investigate a possible interaction. For THA patients, this showed that a significantly larger proportion of elderly patients were women in comparison to the under 75 age group (71 % vs 59 % female patients, p = 0.034). Hence, the greater LOS reduction seen in elderly patients is not a result of sex distribution. Conversely, the greater reduction in LOS seen in men is not a result of age distribution. In fact, the difference occurs despite the higher proportion of women among older patients. This was not observed for patients undergoing TKA (elderly vs young: 55 % vs 58 % female patients, respectively, p = 0.65).
Discussion
Age
Our results show that increasing age is associated with prolonged LOS for THA and TKA, in line with published research [21–24]. Introduction of the ICP has helped in markedly reducing this age gap for THA. Assessing whether this translates into an outcome benefit was beyond the scope of this study and should be a focus for further research. Previous studies into the effects of age on pain, function and quality of life post-THA or TKA have shown that it was not a significant determinant of pain or function, with patients of all ages achieving similar preoperative and six-month follow-up Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores [25].
A possible explanation for the prolonged LOS observed in elderly patients with a similar functional outcome (fitness for discharge) compared with younger patients may be that more rehabilitation resources are required to support older patients. This has been corroborated to a degree in other studies that showed older patients undergoing THA and TKA achieved a similar functional independence measure (FIM) improvement at a rehabilitation hospital compared with younger patients but at the expense of increased LOS and higher costs [16, 17]. The absolute FIM scores at admission and discharge were, however, significantly lower for elderly patients. It is possible that elderly patients in our study derived greater benefit from the ICP in terms of LOS reduction, as the aims of the ICP were to improve the efficiency of acute inpatient rehabilitation and discharge planning.
It is however debatable whether an LOS reduction can be used as a proxy for increased efficiency and hence better resource utilisation and reduced cost [19]. As LOS and cost are usually analysed as part of evaluating the effect of a multidimensional ICP, it is difficult to ascertain the effect of reduced LOS on its own. Also, many cost-effectiveness analyses of ICPs only consider in-hospital cost [6, 7] rather than the overall cost to society [3, 9]. A reduction in LOS could place a greater demand on primary care services in the community [10]. The lower DOSA rate observed in elderly THA patients is most likely to be multifactorial. The higher prevalence of comorbidity and dependence on relatives or the ambulance service for transportation may well preclude some patients from arriving at 7:00 a.m. on the day of surgery.
Gender
Our results indicate that being female is associated with a prolonged LOS for THA but not for TKA. Other authors have shown an increased LOS in female patients for both operations in acute and rehabilitation settings [17, 21, 23]. Holtzman et al. [15] demonstrated that women had a poorer functional status at the time of surgery, which partially explained postoperative differences at one-year follow-up. Vincent et al. [17] showed that for patients undergoing THA, women had a similar improvement in FIM score compared with men in a rehabilitation setting, but again at the expense of a longer LOS. Also, their absolute scores were significantly lower. A possible conclusion is that there is a gender discrepancy when patients undergo THA. Indeed, in that study, women were older than their male counterparts at the time of THA but not TKA and hence may have had more advanced osteoarthritis. The trend towards a lower DOSA rate among female patients may also be a marker of a greater disability at the time of operation. In view of this, it was to be expected that women would benefit more from the structured and efficient care under the ICP in terms of reduced LOS. However the opposite was observed in our study, which casts a degree of doubt on whether this is the mechanism for the difference in LOS reduction according to age.
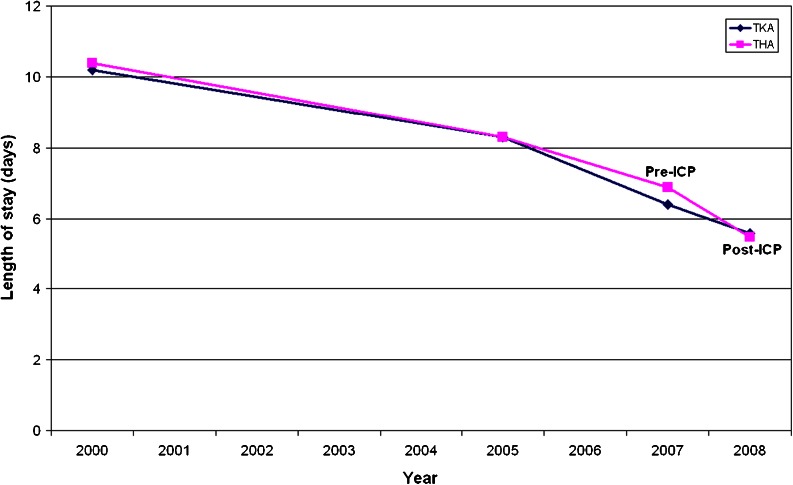
THA vs TKA
Our results show that patients undergoing THA benefitted considerably more from the introduction of the ICP compared with those undergoing TKA (1.4 vs 0.8 days of reduction in LOS). There are a number of possible explanations for this. The pathway was designed in response to the success of the fractured neck of femur pathway and hence may be better tailored towards THA. It is also possible that this is a reflection of lower DOSA rates in TKA vs. THA patients. Dy et al. [19] proposed that ICPs for procedures with a trend towards a lower LOS should be assessed on whether they produce a change in the rate of LOS reduction. Whereas we did not fully emulate their statistical analysis, Fig. 2 shows LOS at our unit over the past eight years. A change in gradient is seen for THA but not for TKA patients following introduction of the ICP.
Fig. 2.
Length of stay (LOS) following total hip (THA) and total knee (TKA) at our unit over the past 8 years
Age distribution was similar for both patient populations. There was a higher proportion of men in the TKA than the THA population (43 % vs 37 %); however as men benefitted more from the ICP than women, this does not explain the smaller LOS reduction seen in TKA patients. Finally, in the pre-ICP period, mean LOS for TKA was closer to the targeted five days than mean LOS for THA (6.4 vs 6.9 days). Introduction of the ICP largely abolished this difference (5.6 vs 5.5 days).
Study limitations were that this was a retrospective study and did not include an assessment of complication rate or a cost analysis. Outcome assessment in terms of joint function and patient-reported quality of life was beyond the scope of this study.
Conclusion
Introduction of an ICP reduced LOS by 1.4 days for THA and 0.8 days for TKA. Elderly and male patients benefitted to a greater degree. Further research is required into whether this LOS reduction has long-term effects on outcome.
Acknowledgments
Conflict of interests
None
References
- 1.Hospital Episodes Statistics Online (2009) Hospital Episode Statistics. http://www.hesonline.nhs.uk :Accessed 14 Februay 2012
- 2.HM Treasury (2010) Budget 2010: Securing the recovery. http://www.hm-treasury.gov.uk/budget2010.htm :Accessed 14 February 2012
- 3.Brunenberg DE, Van Steyn MJ, Sluimer JC, Bekebrede LL, Bulstra SK, Joore MA. Joint recovery programme versus usual care: an economic evaluation of a clinical pathway for joint replacement surgery. Med Care. 2005;43:1018–1026. doi: 10.1097/01.mlr.0000178266.75744.35. [DOI] [PubMed] [Google Scholar]
- 4.Dowsey MM, Kilgour ML, Santamaria NM, Choong PF. Clinical pathways in hip and knee arthroplasty: a prospective randomised controlled study. Med J Aust. 1999;170:59–62. doi: 10.5694/j.1326-5377.1999.tb126882.x. [DOI] [PubMed] [Google Scholar]
- 5.Husni ME, Losina E, Fossel AH, Solomon DH, Mahomed NN, Katz JN. Decreasing medical complications for total knee arthroplasty: effect of critical pathways on outcomes. BMC Musculoskelet Disord. 2010;11:160. doi: 10.1186/1471-2474-11-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macario A, Horne M, Goodman S, Vitez T, Dexter F, Heinen R, Brown B. The effect of a perioperative clinical pathway for knee replacement surgery on hospital costs. Anesth Analg. 1998;86:978–984. doi: 10.1097/00000539-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Scranton PE. The cost effectiveness of streamlined care pathways and product standardization in total knee arthroplasty. J Arthroplast. 1999;14:182–186. doi: 10.1016/S0883-5403(99)90123-7. [DOI] [PubMed] [Google Scholar]
- 8.Vanhaecht K, Sermeus W, Tuerlinckx G, Witters I, Vandenneucker H, Bellemans J. Development of a clinical pathway for total knee arthroplasty and the effect on length of stay and in-hospital functional outcome. Acta Orthop Belg. 2005;71:439–444. [PubMed] [Google Scholar]
- 9.Larsen K, Hansen TB, Thomsen PB, Christiansen T, Søballe K. Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. J Bone Joint Surg Am. 2009;91:761–772. doi: 10.2106/JBJS.G.01472. [DOI] [PubMed] [Google Scholar]
- 10.Rotter T, Kinsman L, James E, Machotta A, Gothe H, Willis J, Snow P, Kugler J (2010) Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev (3):CD006632 [DOI] [PubMed]
- 11.Barbieri A, Vanhaecht K, Van Herck P, Sermeus W, Faggiano F, Marchisio S, Panella M. Effects of clinical pathways in the joint replacement: a meta-analysis. BMC Med. 2009;7:32. doi: 10.1186/1741-7015-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rotter T, Kugler J, Koch R, Gothe H, Twork S, Van Oostrum JM, Steyerberg EW. A systematic review and meta-analysis of the effects of clinical pathways on length of stay, hospital costs and patient outcomes. BMC Health Serv Res. 2008;8:265. doi: 10.1186/1472-6963-8-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthr Cartil. 2005;13:769–781. doi: 10.1016/j.joca.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 14.Katz JN, Wright EA, Guadagnoli E, Liang MH, Karlson EW, Cleary PD. Differences between men and women undergoing major orthopedic surgery for degenerative arthritis. Arthritis Rheum. 1994;37:687–694. doi: 10.1002/art.1780370512. [DOI] [PubMed] [Google Scholar]
- 15.Holtzman J, Saleh K, Kane R. Gender differences in functional status and pain in a Medicare population undergoing elective total hip arthroplasty. Med Care. 2002;40:461–470. doi: 10.1097/00005650-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Vincent KR, Vincent HK, Lee LW, Alfano AP. Outcomes in total knee arthroplasty patients after inpatient rehabilitation: influence of age and gender. Am J Phys Med Rehabil. 2006;85:482–489. doi: 10.1097/01.phm.0000219151.18749.50. [DOI] [PubMed] [Google Scholar]
- 17.Vincent HK, Alfano AP, Lee L, Vincent KR. Sex and age effects on outcomes of total hip arthroplasty after inpatient rehabilitation. Arch Phys Med Rehabil. 2006;87:461–467. doi: 10.1016/j.apmr.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Khan F, Ng L, Gonzalez S, Hale T, Turner-Stokes L (2008) Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy. Cochrane Database Syst Rev (2):CD004957 [DOI] [PMC free article] [PubMed]
- 19.Dy SM, Garg PP, Nyberg D, Dawson PB, Pronovost PJ, Morlock L, Rubin HR, Diener-West M, Wu AW. Are critical pathways effective for reducing postoperative length of stay? Med Care. 2003;41:637–648. doi: 10.1097/01.MLR.0000062552.92534.BE. [DOI] [PubMed] [Google Scholar]
- 20.Cook JR, Warren M, Ganley KJ, Prefontaine P, Wylie JW. A comprehensive joint replacement program for total knee arthroplasty: a descriptive study. BMC Musculoskelet Disord. 2008;9:154. doi: 10.1186/1471-2474-9-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008;79:168–173. doi: 10.1080/17453670710014941. [DOI] [PubMed] [Google Scholar]
- 22.Forrest G, Fuchs M, Gutierrez A, Girardy J. Factors affecting length of stay and need for rehabilitation after hip and knee arthroplasty. J Arthroplast. 1998;13:186–190. doi: 10.1016/S0883-5403(98)90097-3. [DOI] [PubMed] [Google Scholar]
- 23.Dall GF, Ohly NE, Ballantyne JA, Brenkel IJ. The influence of pre-operative factors on the length of in-patient stay following primary total hip replacement for osteoarthritis: a multivariate analysis of 2302 patients. J Bone Joint Surg Br. 2009;91:434–440. doi: 10.1302/0301-620X.91B4.21505. [DOI] [PubMed] [Google Scholar]
- 24.Foote J, Panchoo K, Blair P, Bannister G. Length of stay following primary total hip replacement. Ann R Coll Surg Engl. 2009;91:500–504. doi: 10.1308/003588409X432356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. The effect of age on pain, function, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001;161:454–460. doi: 10.1001/archinte.161.3.454. [DOI] [PubMed] [Google Scholar]