Abstract
Purpose
Adverse events associated with the use of bone cement for fixation of prostheses is a known complication. Due to inconclusive results in studies of hip fracture patients treated with cemented and uncemented hemiprostheses, this study was initiated.
Methods
Our study is based on data reported to the Norwegian Hip Fracture Register on 11,210 cervical hip fractures treated with hemiprostheses (8,674 cemented and 2,536 uncemented).
Results
Significantly increased mortality within the first day of surgery was found in the cemented group (relative risk 2.9, 95 % confidence interval 1.6–5.1, p=0.001). The finding was robust giving the same results after adjusting for independent risk factors such as age, sex, cognitive impairment and comorbidity [American Society of Anesthesiologists (ASA) score]. For the first post-operative day the number needed to harm was 116 (one death for every 116 cemented prosthesis). However, in the most comorbid group (ASA worse than 3), the number needed to harm was only 33.
Conclusions
We found increased mortality for the cemented hemiprosthesis the first post-operative day compared to uncemented procedures. This increased risk is closely related to patient comorbidity estimated by the patient’s ASA score.
Introduction
From the time Sir John Charnley started to treat hip osteoarthritis with a cemented prosthesis 50 years ago, cases of intraoperative haemodynamic instability, respiratory depression and deaths have been reported. For decades numerous studies have been conducted to sort out the mechanisms leading to these deleterious reactions, i.e. “the bone cement implantation syndrome” [1, 2]. During the last two decades the number of studies in this area has dropped markedly. Closer attention to pre- and perioperative monitoring in addition to improved cementing techniques and systematic anticoagulation regimens may have decreased awareness of these complications.
Several laboratory and human studies have shown neuro-depressive, vasoactive, cytotoxic and procoagulant activities directly or indirectly caused by methyl methacrylate (MMA) [3–10]. Thus, a multitude of pathological reactions have triggered cardiorespiratory and vascular instability that occasionally lead to a fatal outcome in patients with poor reserve capacity.
We have recently reported that post-operative mortality within three months in hip fracture patients was correlated with preoperative comorbidity, reduced renal function and old age. In addition, the surgical trauma caused release of intracellular enzymes such as troponin T and reduced oxygen tension, consistent with damage of heart cells and reduced pulmonary function [11].
Even though multiple case reports [12] and uncontrolled materials have pointed in the direction of bone cement as an important cofactor of the untoward side effects, it has been difficult to show convincingly in clinical studies that this was a harmful substance, but based on the precautionary principle the authorities issued a warning [12]. The main reasons for the inconclusive results of reported clinical studies may be inferior study design, lack of statistical power [13] and missing day-to-day analysis [14]. The aim of this study was to investigate the mortality in hip fracture patients treated with cemented and uncemented hemiarthroplasties. In order to include as many patients as possible, an observational study based on patients reported to the Norwegian Hip Fracture Register [15] was performed.
Materials and methods
All 53 hospitals in Norway treating hip fractures report their operations to the Norwegian Hip Fracture Register [16]. The register contains data on the patients, the fractures and the operations. Mortality data were collected from Statistics Norway and gave us date of death. This means that mortality estimates on the operation day can vary between one and 23 hours and on day one between 24 and 47 hours.
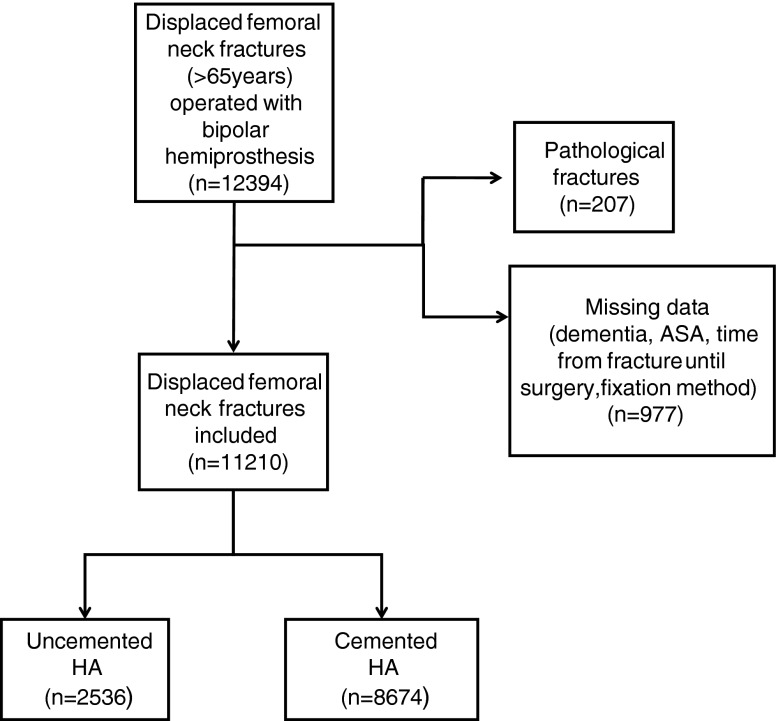
Information on cognitive impairment [19], comorbidities [American Society of Anesthesiologists (ASA) score] [18] and time from fracture to surgery was reported to the registry. In this study, patients registered from January 2005 to December 2010 more than 65 years of age with femoral neck fractures [17] treated with a cemented or uncemented bipolar hemiprosthesis were included. A total of 12,394 patients were extracted from the register; 1,184 patients had missing data of interest for this study, leaving 11,210 patients available for statistical analysis (Fig. 1).
Fig. 1.
Flow chart of patient selection
Statistical analysis
All statistical analyses were conducted using PASW version 18 (IBM, Armonk, NY, USA). Baseline characteristics between the two groups were tested with the chi-square test for categorical data or two-sample t test for continuous data. We used Poisson regression to estimate risk ratio (RR) at the day of operation and Cox regression to estimate RR of mortality during follow-up for patients with cemented versus uncemented prostheses. Adjustments were done for potential confounders such as comorbidity (ASA score), age, sex, dementia and time interval from fracture to surgery (intervals zero–six, six–12, 12–24 and 24–48 hours) in univariable and multivariable models. A p value ≤ 0.05 was considered statistically significant. We found the risk factors influencing mortality to be different the day of surgery (day 0) and the first post-operative day (day 1) as compared to the rest of the follow-up period. Due to this difference, the mortality estimates were done separately for these periods. The number needed to harm (NNH) is the number of cemented prostheses implanted in order to experience one fatality caused by the cementation alone. The NNH was estimated according to different ASA scores.
Results
Baseline characteristics are given in Table 1. The groups were well balanced, although more patients with cognitive impairment and operations within 12 hours of fracture were found in the uncemented group. These two factors did not influence mortality.
Table 1.
Patient characteristics according to fixation method
| Subgroups | Uncemented | Cemented | Total | p valuea | |
|---|---|---|---|---|---|
| ASA score | 1 | 3.5 % (90) | 4.5 % (393) | 4.3 % (483) | 0.212 |
| 2 | 36 % (912) | 35 % (3,014) | 35.0 % (3,926) | ||
| 3 | 55 % (1,390) | 55 % (4,750) | 54.8 % (6,145) | ||
| 4 | 5.6 % (142) | 5.9 % (508) | 5.8 % (650) | ||
| 5 | 0.1 % (2) | 0.0 % (4) | 0.1 % (6) | ||
| Age, years | 83.3 | 83.0 | 83.0 (SD 6.7) | ||
| Sex | Male | 26.1 % (661) | 25.4 % (2,199) | 25.5 % (2,860) | 0.47 |
| Female | 73.9 % (1,875) | 74.6 % (6,475) | 74.5 % (8,350) | ||
| Dementia | No dementia | 60.8 % (1,541) | 63.1 % (5,475) | 62.6 % (7,016) | 0.035 |
| Dementia | 28.5 % (706) | 25.5 % (2,183) | 26.2 % (2,889) | ||
| Unsure | 11.1 % (282) | 11.3 % (982) | 11.3 % (1,264) | ||
| Time from fracture to operation | 0–6 h | 4.2 % (106) | 3.0 % (258) | 3.2 % (364) | <0.001 |
| 6–12 h | 15.6 % (395) | 10.5 % (911) | 11.7 % (1,306) | ||
| 12–24 h | 35.3 % (894) | 34.2 % (2,963) | 34.4 % (3,857) | ||
| 24–48 h | 27.2 % (691) | 30.4 % (2,634) | 29.7 % (3,325) | ||
| >48 h | 17.7 % (450) | 22.0 % (1,908) | 21.0 % (2,358) |
No. of patients shown in parentheses
ap value for difference between patient subgroups of cemented and uncemented hemiarthroplasties
When estimating the immediate perioperative period (within the first post-operative day) compared to the entire following post-operative period (Table 2) we found cement to be an independent risk factor for mortality (adjusted analysis), but not so for the period from post-operative day 2 and thereafter. Cognitive impairment, sex and time from fracture to operation did not represent any increased mortality risk within the first post-operative day, while comorbidity (ASA score) and age were highly significant risk factors for mortality. When using multivariable analyses to evaluate the post-operative period (from the second post-operative day to the end of follow-up) we found comorbidity (ASA score), age, male sex, cognitive impairment and time from fracture to surgery to be independent and significant risk factors for mortality.
Table 2.
Risk and hazard rates at day 0 and day 1 combined and from post-operative day 2 to end of follow-up, respectively
| Day 0 and day 1 combined | From post-operative day 2 to end of follow-up | |||
|---|---|---|---|---|
| Parameter | Unadjusted | Adjusteda | Unadjusted | Adjusteda |
| RR (95 % CI) p value | RR (95 % CI) p value | RR (95 % CI) p value | RR (95 % CI) p value | |
| Fixation, uncemented | Ref. | Ref. | Ref. | Ref. |
| Cemented | 2.8 (1.6–5.1) 0.001 | 2.9 (1.6–5.2) 0.001 | 0.93 (0.87–1.0) 0.053 | 0.96 (0.89–1.03) 0.267 |
| ASA (per 1 unit increase) | 3.6 (2.7–4.8) <0.001 | 3.2 (2.4–4.4) <0.001 | 1.9 (1.7–1.9) <0.001 | 1.58 (1.50–1.66) <0.001 |
| Age (per 1 unit increase) | 1.1 (1.1–1.2) <0.001 | 1.1 (1.1–1.2) <0.001 | 1.06 (1.06–1.07) <0.001 | 1.05 (1.05–1.06) <0.001 |
| Sex, male | Ref. | Ref. | Ref. | Ref. |
| Female | 0.9 (0.6–1.3) 0.635 | 0.9 (0.6–1.4) 0.676 | 0.61 (0.57–0.61) <0.001 | 0.59 (0.55–0.63) <0.001 |
| Dementia, no | Ref. | Ref. | Ref. | Ref. |
| Unsure | 1.5 (1.0–2.2) 0.045 | 1.0 (0.7–1.5) 0.979 | 2.0 (1.8–2.2) <0.001 | 1.63 (1.48–1.78) <0.001 |
| Dementia | 2.1 (1.3–3.3) 0.002 | 1.3 (0.8–2.2) 0.225 | 2.8 (2.6–3.0) <0.001 | 2.35 (2.20–2.51) <0.001 |
| Time from fracture to operation (per 6 h increase) | 1.2 (1.0–1.4) 0.032 | 1.1 (0.9–1.3) 0.303 | 1.1 (1.0–1.1) <0.001 | 1.03 (1.00–1.06) 0.026 |
Cox regression analyses of data from post-operative day 2 to the end of follow-up; it was statistically estimated as hazard ratio
RR risk ratio, CI confidence interval
aValues adjusted for other risk factors (age, sex, cementation, ASA score, dementia and time from fracture to surgery)
The NNH due to cement impaction was 116 operated per death in the total population independent of additive risk factors. The harmed number (fatalities) was more severe with increasing comorbidity (Table 3). In this cohort with 8,674 cemented procedures approximately 74 fatalities the first post-operative day could therefore have been related to the cementation and consequently been avoided using an uncemented procedure if there is a causal relationship between cemented procedure and increased risk of death. With increasing ASA class the NNH decreased, i.e. cementing as an attributed mortality risk increased for each ASA class. The NNH was 811 for ASA scores 1 and 2 as opposed to 33 for ASA scores 4 and 5.
Table 3.
Number needed to treat with a cemented prosthesis in order to cause one fatality due to the cementation (NNH) day 0–1, according to ASA score
| ASA score | Dead | Total | Risk | RD (cem−uncem) | NNHa | 95 % CI | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| 1 + 2 | Uncemented | 2 | 1,002 | 0.002 | ||||
| Cemented | 11 | 3,407 | 0.003 | 0.0012 | 811 | 218 | ∞ | |
| 3 | Uncemented | 7 | 1,390 | 0.005 | ||||
| Cemented | 79 | 4,755 | 0.017 | 0.0116 | 86 | 59 | 157 | |
| 4 + 5 | Uncemented | 3 | 144 | 0.021 | ||||
| Cemented | 26 | 512 | 0.051 | 0.0299 | 33 | 17 | ∞ | |
| 1–5 | Uncemented | 12 | 2,536 | 0.005 | ||||
| Cemented | 116 | 8,674 | 0.013 | 0.0086 | 116 | 82 | 199 | |
CI confidence interval
aNumber of patients treated with a cemented implant in order to cause one fatality because of cementation compared to an uncemented implant if there is a direct causal effect. The NNH was calculated as an inverse value of the risk difference (RD) between the methods [1/(risk cemented − risk uncemented)]
Discussion
This register study of more than 11,000 patients showed significantly increased mortality on the day of surgery and the first post-operative day in hip fracture patients treated with a hemiprosthesis fixed with bone cement compared to patients with uncemented implants. This initial mortality risk was increased even when adjusting for the most common risk factors for mortality: male sex, age, comorbidity (ASA score), cognitive impairment (dementia/possible dementia) and time from fracture to surgery. Long-term follow-up for six years revealed no difference in mortality related to anchoring of the femoral component.
Our study confirms earlier reports describing the relation between impaction of bone cement and surgically-induced mortality [12, 13]. An Australian register study also indicated similar findings and reported increased mortality on the first post-operative day in patients with cemented prostheses [20]. A similar UK study did not confirm these results, but the calculations were based on discharge figures and not by day-to-day estimates [14]. The Swedish Hip Arthroplasty Register [21] recently reported no difference in mortality according to femoral fixation method at one year post-operatively for a similar group of patients.
In this study, as in most studies on hip fractures, patients had comorbid conditions, with more than 60 % of the patients having an ASA score of 3 or worse. In addition the average age was 83 years and more than every fourth patient was cognitively impaired. This group of patients may accordingly lack the reserve capacity often necessary to cope with a double trauma of hip fracture and surgery. Other studies have described comorbidity, age, male sex, delayed surgery and cognitive impairment as some of the most important risk factors for mortality [22–26]. Time from fracture to surgery is the only factor we can influence; our aim has been to identify other preventable factors that increase mortality risk. This study identifies cementation as another independent risk factor for mortality for this group of patients.
NNH, i.e. the number of patients treated with a cemented implant in order to cause one fatality because of cementation compared to an uncemented implant, was 116 which indicates that approximately 75 patients in this cohort could possibly have died as a consequence of the cementing procedure alone compared to an uncemented alternative (8,674 patients with cemented prosthesis/116) (Table 3). However, in patients with preoperative symptomatic comorbidity, i.e. ASA 3 and 4, the NNH was 88 and 33, respectively. The most comorbid patients are at even higher risk of a fatal outcome when cemented procedures are used. This information indicates that comorbidity should be a factor worth considering when selecting the method of fixation.
Delay of surgery more than 48 hours after the fracture has been associated with increased mortality [27, 28] but mostly for a delay exceeding 48 hours after the fracture.
This study indicates that patients should be treated without delay once admitted in order to limit time from fracture to surgery. However, delay from fracture to the operation is an independent and significant risk factor (adjusted) only from the second post-operative day and onward. According to the results of this study delayed surgery does seem to have less impact on early post-operative mortality (within the first post-operative day) compared to ASA score, age and cementation. We also found that dementia and sex behave in a similar fashion as risk factors for mortality. This shows that risk factors have different impact according to different peri- and post-operative periods. A possible explanation could be that physiological demands and challenges differ peri- and post-operatively. The physiological implications and changes leading to death are probably not the same during the initial peri- and post-operative period as compared to the post-operative follow-up. The rate ratio is therefore likely to vary between these periods, and consequently the immediate perioperative period should be analysed separately when it comes to mortality studies. These analyses would demand exact data on time of death for the immediate post-operative period which was not available in this study.
Multivariable Cox regression analyses showed that dementia was not a risk factor [RR 1.3, 95 % confidence interval (CI) 0.8–2.2, p=0.225] for the immediate mortality induced by surgery, but the risk was significantly increased because of dementia/cognitive impairment (RR 2.35, 95 % CI 2.20–2.51, p<0.001) from the second post-operative day through the six-year observation period. This delayed risk is in line with other recent reports and might be related to subsequent adverse clinical events and upcoming diseases [29, 30]. Patients suffering cognitive impairment are less likely to follow post-operative procedures and guidelines outlined to facilitate fast recovery without complications.
In epidemiological data mainly derived from orthopaedic patients, the highest death rate and frequency of myocardial infarction have been reported to be the day of surgery [31, 32]. We have earlier found elevated levels of plasma troponin T that correlated with the three-month fatal outcome [11]. In the same population, we showed that affection of the liver, lung and kidney functions in comorbid elderly patients also correlated with fatal outcome [22]. About 30 % of the population has a patent foramen ovale [33, 34]. During major orthopaedic surgery, this opening could allow procoagulant cell conjugates and fragments to pass directly from the venous to the arterial blood. This favours blood cell aggregation at cites of loci minoris resistentiae, e.g. in an abnormal post-stenotic flow, micro-ruptured plaque, and contributes to the explanation of the rate of immediate intraoperative and post-surgical severe events that may be fatal. This potential risk factor for mortality has to our knowledge not been investigated for this group of patients.
The findings in this study are based on register data and cannot be interpreted as a randomised study [35]. This applies even though the baseline characteristics are similar between the groups and the cohort is large. Another important consideration is that this study only deals with mortality. Morbidity, functional outcome, pain, quality of life and reoperations were not investigated and should certainly also be accounted for when considering treatment options and follow-up regimens for these patients. Several studies evaluating the significance of these factors have been published lately. A Cochrane review from 2010, by Parker et al. [36], reported lower reduction of mobility and lower pain scores for patients treated with cemented hemiarthroplasties compared to uncemented procedures. The reoperation rate seems to be higher for uncemented implants [37] and bipolar implants might also increase the risk for reoperation [21]. These are factors reducing the function of the patient and possibly increasing the mortality risk due to inactivity, additional surgery and reduced independency. Some of these factors might even reduce the potential primary benefit from using an uncemented implant.
We found a correlation between cement fixation of the prosthesis and perioperative mortality, more so for patients with increased comorbidity. Register studies are hypothesis generating and our data do not account for rigorous conclusions or change of guidelines. However, the use of uncemented prostheses should be considered for the most debilitated patients suffering a hip fracture in order to eliminate factors that possibly increase the mortality risk such as bone cement. For the same reason, delay of surgery should also be avoided, unless this is due to a preoperative optimalisation of the patient improving the likelihood of survival of the surgical procedure.
According to the results of this study risk factors seem to differ in different post-operative time periods. Some factors do apply primarily (ASA score, age and cementation), while other factors (sex, cognitive impairment and time from fracture to surgery) have a significant impact on mortality, but mainly from post-operative day 2 in this study. This might imply that several risk factors for mortality play different roles in the perioperative period and therefore should be accounted for differently according to the individual patient. We believe that more research is needed in order to evaluate the impact of independent risk factors in the perioperative period; emphasis should be on patient surveillance during and shortly after the surgery. In addition we encourage a focus on identifying vulnerable subgroups of patients and other possible risk factors for mortality, which could supply additional tools in order to customise treatment and reduce hazards from the surgical trauma. We find it crucial to study the immediate perioperative period separately when mortality is an issue. This is due to critical physiological challenges possibly applying only to the perioperative period.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation syndrome. Br J Anaesth. 2009;102:12–22. doi: 10.1093/bja/aen328. [DOI] [PubMed] [Google Scholar]
- 2.Dahl OE. Cardiorespiratory and vascular dysfunction related to major reconstructive orthopedic surgery. Acta Orthop Scand. 1997;68:607–614. doi: 10.3109/17453679708999038. [DOI] [PubMed] [Google Scholar]
- 3.Giercksky KE, Bjorklid E, Prydz H. The effect of intravenous injection of purified human tissue thromboplastin in rats. Scand J Haematol. 1976;16:300–310. doi: 10.1111/j.1600-0609.1976.tb01155.x. [DOI] [PubMed] [Google Scholar]
- 4.Modig J, Busch C, Olerud S, Saldeen T. Pulmonary microembolism during intramedullary orthopaedic trauma. Acta Anaesthesiol Scand. 1974;18:133–143. doi: 10.1111/j.1399-6576.1974.tb00852.x. [DOI] [PubMed] [Google Scholar]
- 5.Ereth MH, Weber JG, Abel MD, Lennon RL, Lewallen DG, Ilstrup DM, Rehder K. Cemented versus noncemented total hip arthroplasty–embolism, hemodynamics, and intrapulmonary shunting. Mayo Clin Proc. 1992;67:1066–1074. doi: 10.1016/S0025-6196(12)61121-5. [DOI] [PubMed] [Google Scholar]
- 6.Engesaeter LB, Strand T, Raugstad TS, Husebø S, Langeland N. Effects of a distal venting hole in the femur during total hip replacement. Arch Orthop Trauma Surg. 1984;103:328–331. doi: 10.1007/BF00432420. [DOI] [PubMed] [Google Scholar]
- 7.Dahl OE, Johnsen H, Kierulf P, Molnar I, Rø JS, Vinje A, Mowinckel P. Intrapulmonary thrombin generation and its relation to monomethylmethacrylate plasma levels during hip arthroplasty. Acta Anaesthesiol Scand. 1992;36:331–335. doi: 10.1111/j.1399-6576.1992.tb03477.x. [DOI] [PubMed] [Google Scholar]
- 8.Schlag G, Schliep HJ, Dingeldein E, Grieben A, Ringsdorf W. Does methylmethacrylate induce cardiovascular complications during alloarthroplastic surgery of the hip joint (in German)? Anaesthesist. 1976;25:60–67. [PubMed] [Google Scholar]
- 9.Dahl OE, Westvik AB, Kierulf P, Lyberg T. Effect of monomethylmethacrylate on procoagulant activities of human monocytes and umbilical vein endothelial cells in vitro. Thromb Res. 1994;74:377–387. doi: 10.1016/0049-3848(94)90153-8. [DOI] [PubMed] [Google Scholar]
- 10.Linder LG, Harthon L, Kullberg L (1976) Monomer leakage from polymerizing acrylic bone cement. An in vitro study on the influence of speed and duration of mixing, cement volume and surface area. Clin Orthop Relat Res 119:242–249 [PubMed]
- 11.Talsnes O, Hjelmstedt F, Dahl OE, Pripp AH, Reikerås O. Clinical and biochemical prediction of early fatal outcome following hip fracture in the elderly. Int Orthop. 2010;35:903–907. doi: 10.1007/s00264-010-1149-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duncan JA. Intra-operative collapse or death related to the use of acrylic cement in hip surgery. Anaesthesia. 1989;44:149–153. doi: 10.1111/j.1365-2044.1989.tb11168.x. [DOI] [PubMed] [Google Scholar]
- 13.Lennox IA, McLauchlan J. Comparing the mortality and morbidity of cemented and uncemented hemiarthroplasties. Injury. 1993;24:185–186. doi: 10.1016/0020-1383(93)90290-M. [DOI] [PubMed] [Google Scholar]
- 14.Costa ML, Griffin XL, Pendleton N, Pearson M, Parsons N. Does cementing the femoral component increase the risk of peri-operative mortality for patients having replacement surgery for a fracture of the neck of femur? Data from the National Hip Fracture Database. J Bone Joint Surg Br. 2011;93:1405–1410. doi: 10.1302/0301-620X.93B10.26690. [DOI] [PubMed] [Google Scholar]
- 15.Norwegian Arthroplasty Register (2012) Http//:www.haukeland.no/nrl. Last accessed 17 Apr 2012
- 16.Gjertsen J-E, Engesaeter LB, Furnes O, Havelin LI, Steindal K, Vinje T, Fevang JM. The Norwegian Hip Fracture Register: experiences after the first 2 years and 15,576 reported operations. Acta Orthop. 2008;79:583–593. doi: 10.1080/17453670810016588. [DOI] [PubMed] [Google Scholar]
- 17.Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961;43-B:647–663. [Google Scholar]
- 18.No authors listed (1963) American Society of Anesthesiology new classification of physical status. Anesthesiology 24:111
- 19.Shulman KI. Clock-drawing: is it the ideal cognitive screening test? Int J Geriatr Psychiatry. 2000;15:548–561. doi: 10.1002/1099-1166(200006)15:6<548::AID-GPS242>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 20.Costain DJ, Whitehouse SL, Pratt NL, Graves SE, Ryan P, Crawford RW. Perioperative mortality after hemiarthroplasty related to fixation method. Acta Orthop. 2011;82:275–281. doi: 10.3109/17453674.2011.584208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leonardsson O, Kärrholm J, Åkesson K, Garellick G, Rogmark C. Higher risk of reoperation for bipolar and uncemented hemiarthroplasty. Acta Orthop. 2012;83:459–466. doi: 10.3109/17453674.2012.727076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Talsnes O, Hjelmstedt F, Dahl OE, Pripp AH, Reikerås O. Biochemical lung, liver and kidney markers and early death among elderly following hip fracture. Arch Orthop Trauma Surg. 2012;132:1753–1758. doi: 10.1007/s00402-012-1611-7. [DOI] [PubMed] [Google Scholar]
- 23.Holvik K, Ranhoff AH, Martinsen MI, Solheim LF. Predictors of mortality in older hip fracture inpatients admitted to an orthogeriatric unit in Oslo, Norway. J Aging Health. 2010;22:1114–1131. doi: 10.1177/0898264310378040. [DOI] [PubMed] [Google Scholar]
- 24.Juliebø V, Krogseth M, Skovlund E, Engedal K, Wyller TB. Medical treatment predicts mortality after hip fracture. J Gerontol A Biol Sci Med Sci. 2010;65:442–449. doi: 10.1093/gerona/glp199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petersen MB, Jørgensen HL, Hansen K, Duus BR. Factors affecting postoperative mortality of patients with displaced femoral neck fracture. Injury. 2006;37:705–711. doi: 10.1016/j.injury.2006.02.046. [DOI] [PubMed] [Google Scholar]
- 26.Shoda N, Yasunaga H, Huriguchi H, Matsuda S, Ohe K, Kadono Y, Tanaka S (2012) Risk factors affecting inhospital mortality after hip fracture: retrospective analysis using the Japanese Diagnosis Procedure Combination Database. BMJ Open. doi:10.1136/bmjopen-2011-000416 [DOI] [PMC free article] [PubMed]
- 27.Vidán MT, Sánchez E, Gracia Y, Marañón E, Vaquero J, Serra JA. Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med. 2011;155:226–233. doi: 10.7326/0003-4819-155-4-201108160-00006. [DOI] [PubMed] [Google Scholar]
- 28.Smektala R, Endres HG, Dasch B, Maier C, Trampisch HJ, Bonnaire F, Pientka L. The effect of time-to-surgery on outcome in elderly patients with proximal femoral fractures. BMC Musculoskelet Disord. 2008;9:171. doi: 10.1186/1471-2474-9-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duckworth AD, Phillips SA, Stone O, Moran M, Breusch SJ, Biant LC. Deep infection after hip fracture surgery: predictors of early mortality. Injury. 2012;43:1182–1186. doi: 10.1016/j.injury.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 30.Marengoni A, Corrao S, Nobili A, Tettamanti M, Pasina L, Salerno F, Iorio A, Marcucci M, Bonometti F, Mannucci PM, et al. In-hospital death according to dementia diagnosis in acutely ill elderly patients: the REPOSI study. Int J Geriatr Psychiatry. 2011;26:930–936. doi: 10.1002/gps.2627. [DOI] [PubMed] [Google Scholar]
- 31.Kikura M, Oikawa F, Yamamoto K, Iwamoto T, Tanaka KA, Sato S, Landesberg G. Myocardial infarction and cerebrovascular accident following non-cardiac surgery: differences in postoperative temporal distribution and risk factors. J Thromb Haemost. 2008;6:742–748. doi: 10.1111/j.1538-7836.2008.02948.x. [DOI] [PubMed] [Google Scholar]
- 32.Lie SA, Engesaeter LB, Havelin LI, Furnes O, Vollset SE. Early postoperative mortality after 67,548 total hip replacements: causes of death and thromboprophylaxis in 68 hospitals in Norway from 1987 to 1999. Acta Orthop Scand. 2002;73:392–399. doi: 10.1080/00016470216312. [DOI] [PubMed] [Google Scholar]
- 33.Honĕk J, Honĕk T, Januška J, Sebesta P, Novotný S, Sefc L, Fiedler J, Srámek M, Horváth M, Parobková M (2012) Patent foramen ovale and the risk of paradoxical embolization of venous bubbles in divers - cave for foam sclerotization of varicose veins (in Czech). Article. Rozhl Chir 91:378–380 [PubMed]
- 34.Marriott K, Manins V, Forshaw A, Wright J, Pascoe R. Detection of right-to-left atrial communication using agitated saline contrast imaging: experience with 1162 patients and recommendations for echocardiography. J Am Soc Echocardiogr. 2013;26:96–102. doi: 10.1016/j.echo.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 35.Labek G, Janda W, Agreiter M, Schuh R, Böhler N. Organisation, data evaluation, interpretation and effect of arthroplasty register data on the outcome in terms of revision rate in total hip arthroplasty. Int Orthop. 2011;35:157–163. doi: 10.1007/s00264-010-1131-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parker MJ, Gurusamy KS, Azegami S (2010) Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev 6:CD001706. doi:10.1002/14651858.CD001706.pub4 [DOI] [PMC free article] [PubMed]
- 37.Gjertsen JE, Lie SA, Vinje T, Engesæter LB, Hallan G, Matre K, Furnes O. More re-operations after uncemented than cemented hemiarthroplasty used in the treatment of displaced fractures of the femoral neck: an observational study of 11,116 hemiarthroplasties from a national register. J Bone Joint Surg Br. 2012;94(8):1113–1119. doi: 10.1302/0301-620X.94B8.29155. [DOI] [PubMed] [Google Scholar]