Abstract
Context
Previous studies have suggested that children who experience parental suicide at earlier ages are at higher risk of future hospitalization for suicide attempt. However, how the trajectories of risk differ by offspring age at the time of parental suicide is currently unknown.
Objective
To study time at risk to hospitalization for suicide attempt among offspring after experiencing parental suicide or accidental death by offspring developmental period at the time of parental death.
Design
Population-based retrospective cohort study
Setting
Sweden
Participants
26,096 offspring who experienced parental suicide and 32,395 offspring of accident decedents prior to age 25 from 1973-2003.
Main Outcome Measures
Hospitalization for suicide attempt. Parametric survival analysis was used to model the time to hospitalization for suicide attempt across offspring who lost a parent during early childhood (0-5 years old), later childhood (6-12), adolescence (13-17) and young adulthood (18-24).
Results
The risk in offspring who lost a parent during early or late childhood surpassed the other two age groups’ hazards approximately 5 years after the origin and, for the youngest group, continued to rise over the course of decades. Offspring who lost a parent during adolescence or young adulthood were at greatest risk within 1 to 2 years after parental suicide, and risk declined over time. The shape of hospitalization risk was similar among those who experienced parental fatal accident. When the shape of hospitalization for suicide attempt at each developmental period was fixed to be the same between the two groups, offspring who lost a parent to suicide had earlier risk to hospitalization for suicide attempt hospitalization than offspring who lost a parent to an accident.
Conclusion
The hospitalization risk for suicide attempt in offspring who lost a parent during their childhood is different from those who lost a parent during adolescence or young adulthood. The results suggest critical windows for careful monitoring and intervention for suicide attempt risk, especially 1-2 years after parental death for the older age groups and over decades for childhood survivors of parental death.
Introduction
Suicide affects millions of individuals worldwide and leaves a devastating impact on family members left behind, herein referred to as ‘survivors’ 1. Paralleling research on understanding the processes leading to suicide, an increasing number of studies have examined the psychosocial impact of suicide on survivors 2, 3. However, research is still needed to assess the long-term impact and evaluate interventions for bereaved individuals 4, 5.
Among survivors of suicide, young offspring who survived parental suicide have received particular research attention, as they lost a caregiver during a critical developmental period and may have higher vulnerability to suicide attempt and suicide 6-8. Several studies have shown that offspring who experience parental suicide prior to young adulthood are at increased risk for suicide and hospitalization for suicide attempt, as compared to those who experience a parent’s death by other means 9-12. Other studies have noted higher anger and depressive symptoms among offspring who experienced parental suicide during childhood 13, 14. However, some studies have suggested that offspring of suicide decedents are more similar than different from offspring of accident decedents 15.
Our research group recently reported that among offspring who lost a parent to suicide before age 25, offspring’s risk for psychiatric hospitalization and suicide was noted to vary by the developmental period when the offspring experienced parental suicide, as compared to offspring of parents who were alive, and that offspring who lost a parent to suicide before age 13 were at particularly high risk 9. Furthermore, child and adolescent offspring who lost their mother to suicide had greater risk for hospitalization for suicide attempt than offspring who lost their mother in an accident11. Although these studies have helped identify subgroups of survivors of parental suicide at particularly high risk, they do not provide information regarding how risk varies over time and if there is a critical window or period during which to carefully monitor or intervene with young survivors of parental suicide. Such information has been called for to better understand the risks associated with experiencing parental suicide and would inform intervention efforts in the wake of parental suicide 3.
Using a population-based longitudinal study from Sweden with 30 years of follow-up, we characterized the pattern of risk of hospitalization for suicide attempt among young offspring who experienced parental suicide before age 25 and examined if this pattern of risk varied by the offspring’s developmental period at the time of parental death. To examine if the trajectories of suicide risk are specific to offspring of suicide decedents or are more general to offspring who experienced sudden parental death, we also examined the trajectories of hospitalization for suicide attempt among offspring of accident decedents.
Materials and Methods
We conducted a retrospective cohort study using multiple Swedish, longitudinal national registries. Data were linked using the personal identification number (PIN) assigned to all individuals either at birth or, for immigrants, upon being granted permanent residency. The Cause of Death Register provided data for 71,595 offspring of parents who died by suicide (International Classification of Diseases (ICD) 8/9: E950-E959; ICD 10: X60-X84) during 1973-2003. Offspring who lost a parent to suicide and the surviving parent were identified from the Multi-Generation Register which indicates parent-child relations for all people born or granted permanent residency in Sweden since 1932 (currently encompassing 13 million people). Of the 71,595 offspring of suicide decedents, 27,997 were younger than 25 years of age when their parent died. We excluded 1) 673 offspring who experienced the death of the coparent prior to the suicide of a parent, 2) an additional 230 individuals who had unreliable data on the psychiatric hospitalization status of the deceased or surviving parents (e.g., a hospitalization record after the parent died), and 3) 998 offspring with hospitalizations for suicide attempt prior to parental suicide. The final sample was comprised of 26,096 offspring who experienced parental suicide prior to age 25.
Using the same data source, 236,400 offspring of parents who died from accidents (ICD 8/9: E800-E929; ICD10: V01-X59) were identified during 1973-2003, of which 34,327 experienced the death of a parent prior to age 25. After applying the same exclusion criteria, the final sample of offspring of accident decedents was 32,395.
This study was approved by the Institutional Review Boards of the Karolinska Institutet and the Johns Hopkins School of Medicine. Although consent was not obtained, the data remained anonymous and incurs minimal risk of identification.
Outcome variable
Hospitalization for confirmed or suspected suicide attempt (ICD 8/9: E950-E959; E980-E989; ICD 10: X60-X84; Y10-Y34) was the outcome of interest and was obtained from the National Inpatient Registry. The National Inpatient Registry records ICD discharge diagnoses for all individuals admitted to any general or psychiatric hospital in Sweden for assessment or treatment. We examined the date of first hospitalization for suicide attempt after the origin, which excluded offspring who attempted suicide prior to parental death. The origin was defined as the date when a parent died from suicide or accident or the date when the offspring turned 10 years old, if parental death occurred prior to this date. These dates were obtained by linking the Cause of Death Register and Multi-Generation Register. The offspring age of 10 was selected as an origin for offspring who lost a parent before age 10, as it is rare for children younger than age 10 to carry out a suicide attempt requiring hospitalization, and a recent study used this age as a starting point to examine age to first suicide attempt 16. Individuals were censored if they died prior to December 31, 2003.
Exposure variable and covariates
The offspring were stratified into groups based on the timing of parental death: early childhood (0-5 years old), later childhood (6-12 years old), adolescence (13-17 years old) and young adulthood (18-24 years old). A similar categorization was used in a previous study 9.
In addition to the outcome and age of offspring when the parent died, we identified the following eleven covariates from the Swedish national registries: birth year and birth country of both parents (Sweden vs. non-Sweden) and offspring, deceased parent’s history of psychiatric hospitalization, surviving parent’s psychiatric hospitalization prior to parental death, gender of offspring and parents, and deceased parent’s age at the time of parental death.
Statistical Analysis
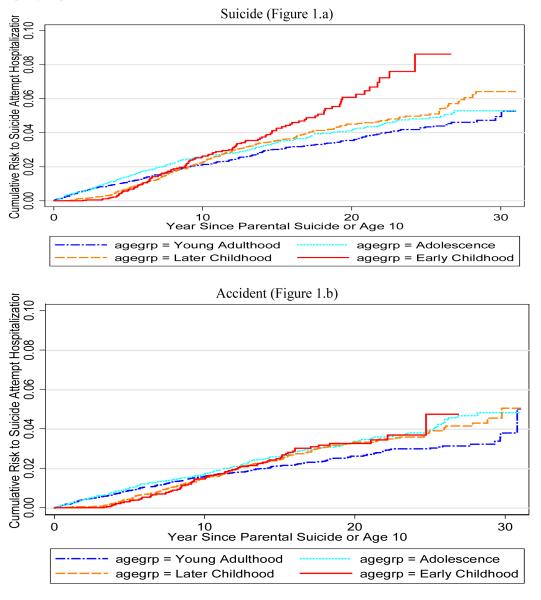
First we examined the cumulative hazard to hospitalization for suicide attempt using non-parametric Nelson-Aalen cumulative hazard curves, which are graphically depicted in Figure 1. We then conducted stratified parametric survival analysis to examine the time to hospitalization for suicide attempt across the four developmental periods during which the offspring experienced parental death. Parametric survival analysis was preferred over semi-parametric Cox regression as this technique allows for modeling the patterns of hospitalization for suicide attempt at each developmental period without constraining the pattern to be similar across periods (i.e. without imposing proportional hazards). Parametric survival analysis assumes that hospitalization for suicide attempt follows a certain hazard shape/pattern. Since we did not find any prior literature reporting the shape of such hazard among offspring survivors, we compared models across several distributions (Weibull, loglogistic, gamma and lognormal) using the Akaike Information Criteria (AIC)17 and Bayesian Information Criterion (BIC) fit indices 18. The lognormal distribution yielded the lowest AIC and BIC for the majority of developmental periods and was thus selected for further analysis.
Figure 1.
Non-parametric Nelson-Aalen Cumulative Hazard of Hospitalization for Suicide Attempt among Offspring who Lost a Parent to Suicide or Accident, Stratified by Developmental Period when the Offspring Experienced Parental Suicide.
The lognormal distribution models the log of time to hospitalization for suicide attempt and assumes an increase followed by a decrease in hazard over time. The lognormal model estimates two parameters of interest: 1) a location parameter, β, captures time to event and is the log median survival time, and 2) a scale (dispersion) parameter, σ, informs the hazard shape19-21. Lower β denotes earlier time to hospitalization for suicide attempt as the median survival time will be smaller; larger σ indicates that the peak of the hazard pattern will be closer to the origin.
We also examined if the two parameters, location and scale, were statistically different between offspring who experienced parental death in the three younger developmental periods as compared to those who experienced parental death during young adulthood (reference group). The models were adjusted for psychiatric hospitalizations in the deceased parent as well as the surviving parent prior to the index parent’s death. We conducted parametric survival analysis similarly among offspring of accident decedents and chose the lognormal distribution to characterize the trajectory patterns using the same criteria. A model that included type of parental death was estimated to test whether the location and/or scale parameters were statistically different between offspring of accident and suicide decedents within each developmental period.
To gauge whether the differential risks were more due to the environmental impact of losing a parent to suicide early in the offspring’s development, a subanalysis using a shared frailty model was conducted among siblings who experienced parental suicide at different developmental periods. The shared frailty model incorporates unobserved shared heterogeneity (i.e., the correlation induced by sharing the same parent) in hazard estimation. This approach is similar to multi-level modeling as applied to correlated survival data 22. The Weibull distribution that assumes a monotonic increase or decrease in hazard was preferred over the lognormal distribution for the sibling analysis. The selection was based on lower AIC and better concordance with results from a piecewise exponential model that allows for a more flexible hazard 21. Weibull models can be presented in hazard and accelerated time failure metrics.
We examined the differences in patterns between daughters and sons at each developmental period among offspring of suicide decedents by using stratified lognormal models. A model was estimated to test whether the location and scale parameters were statistically different between daughters and sons within each developmental period. Model fit was assessed using the Cox-Snell goodness of fit test. Analyses used robust standard errors to account for the dependence between observations due to clustering of siblings within families (77% of the observations were siblings). All analyses were conducted using Stata version 10 23.
Results
Among the 26,096 offspring who experienced parental suicide prior to age 25, 3,534 (13%) occurred during 0-5 years of age (early childhood), 7,147 (27%) occurred during 6-12 years of age (later childhood), 6,401 (25%) during 13-17 (adolescence) and 9,014 (35%) during ages 18-24 (young adulthood). Table 1 describes the characteristics of the offspring of suicide decedents and their parents (deceased and surviving). Psychiatric hospitalization rates of the deceased parent ranged anywhere between 44-48% across all age groups. Parental psychiatric hospitalizations were least frequent among the group of offspring who lost their parent to suicide during their early childhood. Any psychiatric hospitalization of the surviving parent prior to the death of their spouse ranged from 7-8%. Among 32,395 offspring who experienced parental fatal accident prior to age 25, 4,058 (13%) occurred during early childhood, 7,444 (23%) during later childhood, 7,241 (22%) during adolescence and 13,652 (42%) during young adulthood. The characteristics of the offspring of accident decedents, as well as their parents are provided online (eTable 1).
Table 1.
Characteristics of Offspring, Suicide Decedents and Surviving Parents by the Developmental Period of Offspring at the Time Parental Suicide Occurred, Identified from Swedish Population-based Registries, 1973-2003
|
Early childhood (Ages 0-5) (n=3,534) |
Later Childhood (Ages 6-12) (n=7,147) |
Adolescence (Ages 13-17) (n=6,401) |
Young Adulthood (Ages 18-24) (n=9,014) |
p-value | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Offspring | N | % | N | % | N | % | N | % | |
| Country of Birth: Sweden | 3,489 | 99 | 6,953 | 97 | 6,159 | 96 | 8,722 | 97 | 0.001 |
| Offspring Female | 1,674 | 47 | 3,474 | 49 | 3,110 | 49 | 4,333 | 48 | 0.60 |
| Year of Birth (Mean±SD) | 1981 | 7.1 | 1976 | 8.9 | 1971 | 8.8 | 1965 | 8.7 | 0.001 |
| Any Psychiatric Hospitalization prior to parental death |
1 | 0.03 | 12 | 0.2 | 65 | 1.0 | 195 | 2.2 | p<0.001 |
| Deceased Parent | |||||||||
| Country of Birth: Sweden | 2,984 | 85 | 6,142 | 86 | 5,563 | 87 | 7,980 | 89 | 0.001 |
| Year of Birth (Mean±SD) | 1951 | 9.0 | 1947 | 10.6 | 1942 | 10.9 | 1936 | 11.1 | 0.001 |
| Any Psychiatric Hospitalization |
1,548 | 44 | 3,392 | 47 | 3,075 | 48 | 4,268 | 47 | 0.001 |
| Age of Parent at Death (Mean±SD) |
33.1 | 6.7 | 38.8 | 6.9 | 44.3 | 6.5 | 49.8 | 6.6 | 0.001 |
| Parent Mother | 741 | 21 | 1,702 | 24 | 1,617 | 25 | 2,556 | 28 | 0.001 |
| Surviving Parent | |||||||||
| Country of Birth: Sweden | 3,045 | 87 | 6,190 | 87 | 5,529 | 87 | 7,819 | 88 | 0.21 |
| Year of Birth (Mean±SD) | 1953 | 8.7 | 1949 | 10.2 | 1943 | 10.5 | 1938 | 10.7 | 0.001 |
| Any Psychiatric Hospitalization Prior to Spouse Death |
280 | 8 | 509 | 7 | 450 | 7 | 630 | 7 | 0.30 |
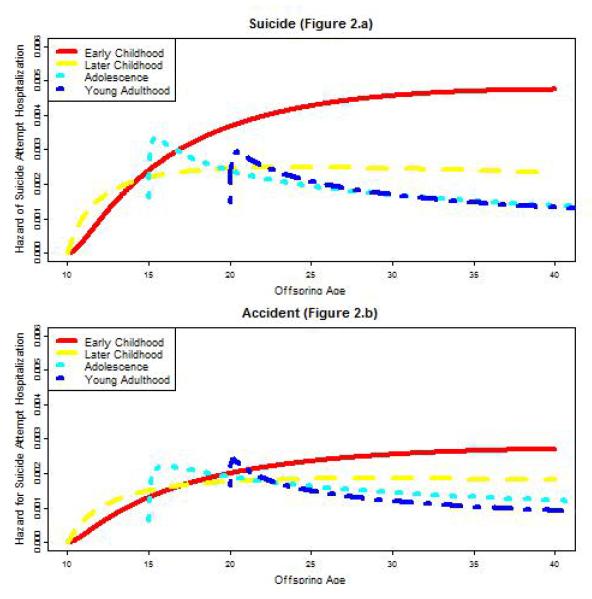
Table 2 reports the parameter estimates that characterize time to hospitalization for suicide attempt for each age group, as well as by whether the offspring lost a parent to suicide or a fatal accident. The models adjusted for psychiatric hospitalization of the parent and spouse prior to parental death. Figure 1 shows the non-parametric cumulative hazard to hospitalization for suicide attempt. Figures 2a and 2b graphically depict the hazard shape of hospitalization for suicide attempt predicted from the model parameters. Table 2 (left portion) and Figure 2a suggest that the pattern of suicide attempt hospitalization is different across offspring who experienced parental suicide during different developmental periods. Although the absolute hazard is relatively small, offspring who experienced parental suicide during early childhood surpassed all other offspring’s hazards approximately 5 years after the origin, and their hazard continued to rise until it leveled off two decades later. Similarly, those who lost a parent to suicide during later childhood had increased hazard of hospitalization for suicide attempt relative to young adult offspring, although the hazard did not increase approximately 5 years after the origin. In contrast, the hazard of hospitalization for suicide attempt for offspring who experienced parental suicide during adolescence or young adulthood was highest in the first two years after parental suicide but then decreased over time. No significant differences were noted in either time or shape parameters between offspring who experienced parental suicide during young adulthood versus adolescence (Table 2 left portion).
Table 2.
Parameter Estimates and Standard Errors obtained from the Lognormal Regression Models after Parental Death or Age 10 (for those who experienced Parental Death prior to Age 10) after Adjusting for Psychiatric Hospitalization of Spouse and Parent prior to Parental Death, Identified from Swedish Population-based Registries, 1973-2003.
| Offspring of Suicide Decedents | Offspring of Accident Decedents | Suicide vs. Accident | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| # of attempt |
IR1 | Parental Suicide (n=26,096) |
Difference from young adults |
# of attempt |
IR1 | Parental Accident (n=32,395) |
Difference from young adults |
Unconstrained Model2 |
Constrained Model3 |
|||
|
| ||||||||||||
| Age when Parent Died | β | SE | p-value | β | SE | p-value | p-value | p-value | ||||
| Early childhood (0-5 years) | 116 | 2.74 | 5.23 | 0.17 | <0.001 | 75 | 1.52 | 5.82 | 0.23 | <0.001 | 0.06 | 0.001 |
| Later childhood (6-12 years) | 248 | 2.16 | 6.42 | 0.18 | <0.001 | 180 | 1.54 | 6.70 | 0.25 | <0.001 | 0.58 | 0.02 |
| Adolescence (13-17 years) | 222 | 2.09 | 8.44 | 0.34 | 0.629 | 195 | 1.70 | 8.39 | 0.40 | 0.08 | 0.69 | 0.07 |
| Young Adulthood (18-24 years) | 274 | 1.83 | 8.81 | 0.36 | Reference | 283 | 1.37 | 9.70 | 0.41 | Reference | 0.35 | 0.04 |
| σ | SE | p-value | σ | SE | p-value | p-value | p-value | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Early childhood (0-5 years) | 1.38 | 0.08 | <0.001 | 1.51 | 0.10 | <0.001 | 0.37 | NA | ||||
| Later Childhood (6-12 years) | 1.91 | 0.08 | <0.001 | 1.89 | 0.12 | <0.001 | 0.91 | NA | ||||
| Adolescence (13-17 years) | 2.99 | 0.17 | 0.928 | 2.81 | 0.19 | 0.180 | 0.38 | NA | ||||
| Young Adulthood (18-24 years) | 3.03 | 0.17 | Reference | 3.25 | 0.19 | Reference | 0.66 | NA |
IR = incident rates (per 1000 person-years)
These p-values report the comparison of offspring who lost a parent to suicide versus an accident for each parameter in the same age group.
These p-values report the comparison of offspring who lost a parent to suicide versus an accident for the location parameter in the same age group after the shape (pattern) are constrained to be the same
β: refers to the location parameter, which informs the median log survival time
σ: refers to the dispersion parameter, which informs the shape of the hazard
Figure 2.
Predicted Hazard of Hospitalization for Suicide Attempt among Offspring who Lost a Parent by Suicide or Accident, Stratified by Developmental Period when the Offspring Experienced Parental Death.a,b
a For offspring who lost a parent during early childhood (before 5 years old), hazard was predicted from the later origin at age 10
b Hazard was predicted for offspring who experienced parental suicide during later childhood at age 10, during adolescence at age 15 and during young adulthood at age 20
A similar analysis was conducted to examine trajectories of hospitalization for suicide attempt among offspring of accident decedents (Figure 2b). Time to hospitalization for suicide attempt was similar between the two groups when both shape and time to event was allowed to vary (Table 2 Unconstrained Model). However, since the shape parameter was not significantly different between the suicide and accident groups, a more parsimonious model that fixes the shape to be the same between the suicide and accident groups and only allows the time parameter to vary was conducted. This more parsimonious model suggested that offspring who lost a parent to suicide in early childhood, later childhood and young adulthood had significantly earlier onset of hospitalization for suicide attempt than offspring who lost a parent in an accident during the same developmental periods (p=0.001, p=0.02 and p=0.04, respectively) (Table 2 Constrained Model).
Subanalysis was conducted among siblings who experienced parental suicide during different developmental periods. There were 14,289 (55%) offspring who had at least one sibling in another developmental period under investigation when parental suicide occurred. Siblings who experienced parental suicide in early childhood had statistically increased risk for suicide attempt hospitalization over the course of the follow-up period [Hazard Ratio = 1.50; 95%CI=1.09, 2.07; β=6.06; SE=0.20; p-value=0.01], as compared to siblings who experienced parental suicide during young adulthood. No significant differences were noted between siblings who experienced parental suicide during later childhood or adolescence, as compared to their young adult siblings.
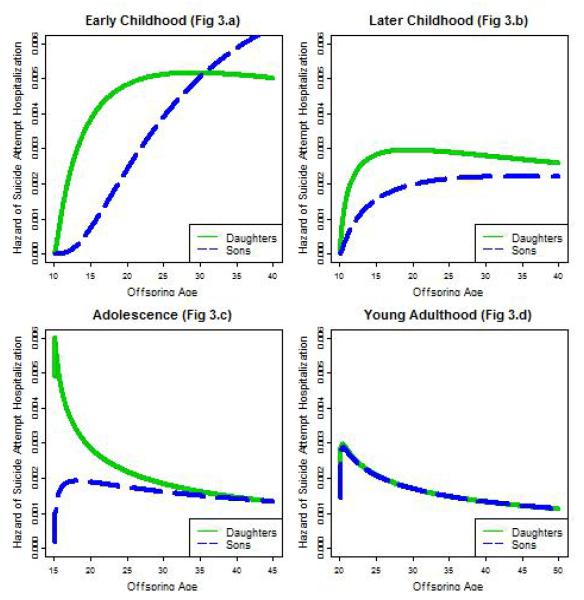
We further examined if the pattern of hospitalization for suicide attempt differed between daughters and sons who experienced parental suicide during the same developmental period. The parameter estimates for sons and daughters and the significance level of the difference for each parameter are reported in Table 3. The predicted hazards are graphically depicted in Figure 3. For offspring who experienced parental suicide during early childhood (Figure 3a) or adolescence (Figure 3c), daughters were at greater risk of hospitalization for suicide attempt than sons directly following parental suicide. This difference became minimal approximately 20 years later for offspring who experienced parental suicide during early childhood and 10 years after the origin for those who experienced parental suicide during adolescence. In both developmental periods, the shape parameters were significant, but the time parameters were not, suggesting that the shape of the hazard significantly differed between daughters and sons, but time to hospitalization for suicide attempt was not shorter in daughters than sons. Time to hospitalization for suicide attempt did not significantly differ between daughters and sons who experienced parental suicide during later childhood or young adulthood (Figure 3d). The hazard pattern for offspring’s hospitalization for suicide attempt did not differ significantly between offspring who lost their mother to suicide, as compared to offspring who lost their father [results not shown].
Table 3.
Gender differences in the Parameter Estimates and Standard Errors obtained from the Lognormal Regression Models after Parental Suicide or Age 10 (for those who experienced Parental Suicide prior to Age 10), Identified from Swedish Population-based Registries, 1973-2003
| Daughters (n=12,591) |
Sons (n=13,505) |
Gender differences1 |
|||
|---|---|---|---|---|---|
|
| |||||
| Age when Parent Died from Suicide | β | SE | β | SE | p-value |
| Early childhood (0-5 years) | 5.24 | 0.21 | 4.73 | 0.22 | 0.14 |
| Later childhood (6-12 years) | 6.39 | 0.22 | 6.30 | 0.29 | 0,91 |
| Adolescence (13-17 years) | 8.66 | 0.45 | 7.85 | 0.49 | 0.31 |
| Young Adulthood (18-24 years) | 9.02 | 0.56 | 8.63 | 0.45 | 0.71 |
| σ | SE | σ | SE | p-value | |
|---|---|---|---|---|---|
| Early childhood (0-5 years) | 1.54 | 0.10 | 0.97 | 0.10 | 0.001 |
| Later Childhood (6-12 years) | 1.98 | 0.11 | 1.76 | 0.14 | 0.263 |
| Adolescence (13-17 years) | 3.26 | 0.22 | 2.55 | 0.23 | 0.05 |
| Young Adulthood (18-24 years) | 3.01 | 0.26 | 3.04 | 0.21 | 0.69 |
These p-values report the comparison of daughters versus son for each parameter in the same age group.
β: refers to the location parameter, which informs the median log survival time
σ: refers to the dispersion parameter, which informs the shape of the hazard
Figure 3.
Predicted Hazard of Hospitalization for Suicide Attempt among Offspring who Lost a Parent to Suicide, Stratified by Offspring Gender and Developmental Period when the Offspring Experienced Parental Suicide. a,b
a For offspring who lost a parent during early childhood (before 5 years old), hazard was predicted from the later origin at age 10
b Hazard was predicted for offspring who experienced parental suicide during later childhood at age 10, during adolescence at age 15 and during young adulthood at age 20
Discussion
This study offers a novel approach to examine the time to hospitalization for suicide attempt among offspring who experienced parental suicide prior to age 25. We found that risk of hospitalization for suicide attempt in childhood survivors of parental suicide differs in duration and persistence of risk,from those who lost a parent later in their lives. The hospitalization risk for suicide attempt continued to rise for decades among offspring who experienced parental suicide during early childhood. For those who experienced parental suicide during adolescence and young adulthood, hospitalization risk for suicide attempt peaked immediately following parental death and decreased as years progressed. The trajectory shapes were very similar for offspring of accident decedents. When the shape was fixed to be the same, offspring who lost a parent to suicide generally had earlier risk to hospitalization for suicide attempt than offspring who lost a parent to an accident. Younger siblings who lost a parent to suicide during early childhood had an increased long-term risk of hospitalization for suicide attempt, as compared to their elder siblings who lost a parent during young adulthood, implying a more detrimental impact of parental suicide during early development. Differences were not evident between siblings who experienced parental suicide during later childhood or adolescence, as compared to siblings who were young adults at the time of parental suicide. We also found that daughters had higher risk of hospitalization for suicide attempt than sons who lost a parent during their early childhood and adolescence; however, this gender difference was not evident in offspring who lost a parent during later childhood or young adulthood. The risk trajectories did not differ between offspring who lost a mother or father to suicide.
Several study limitations should be noted. This study focused on suicide attempt hospitalizations which only captured a portion of individuals who attempted suicide, as many attempters do not come to medical attention. Misclassification of suicide to accident is also possible as accidents could be hidden suicides. This study excluded offspring who had been hospitalized for suicide attempt prior to parental suicide, as well as those who experienced the death of their other parent prior to parental suicide, which may have made our results more conservative as these subgroups may be at particularly high risk for subsequent suicide attempt. The trajectory pattern may depend on the choice of hazard, however, comparison of other models using model diagnostics should have minimized model misspecification. Generalizability may be limited to the Western world, since the Swedish population is primarily Caucasian with relatively high socioeconomic status and universal access to health care. Suicide was relatively rare in this sample of offspring survivors and could not be examined separately as an outcome. Notwithstanding these limitations, this study offers several major strengths such as the use of the population-based Swedish registry, which identified over 20,000 people who lost a parent to suicide before age 25, with close to 30 years of follow-up. We also used parametric survival analysis that provided a robust approach to elucidate the risk pattern for suicide attempt hospitalizations. Hospitalization for suicide attempt was recorded by clinicians and was not biased by self-report.
This study showed that offspring’s trajectories for suicide attempt hospitalization differed by the developmental timing of parental death. The differences in the risk of hospitalization for suicide attempt may in part be due to different psychiatric profiles of parents who die by suicide at an early versus later age. Although we did not find that suicide and accident decedents with younger offspring had higher rates of psychiatric hospitalizations than parents of older offspring, previous studies have suggested that parents who had died suddenly earlier in the offspring’s lives were more likely to have severe mental illnesses 24. Psychological autopsy studies have noted differences in the psychiatric profiles of individuals who died by suicide at younger ages 25-27, suggesting that losing a parent during childhood may be a marker of higher familial and environmental vulnerability to suicidal behavior and/or psychiatric disorder.
Parental suicide may have a different meaning and consequences to offspring at different developmental stages. Although adolescence and young adult survivors experienced parental suicide during the developmental periods in which the rate of suicide attempt is generally higher than those who are younger, survivors who lost a parent during early childhood had the highest cumulative risk for hospitalization for suicide attempt over the course of the thirty year follow-up. In bereavement studies that have examined the impact of parental death on offspring outcomes, the moderating effect of child’s age at the time of death on psychosocial outcomes has been suggested, although empirical evidence is scarce and with conflicting results 28. For adolescents and young adults, the loss of a parent could be a precipitating/proximal factor for suicide attempt hospitalization following parental death, especially as the risk for onset of psychiatric disorders and suicide attempt increases during these periods. However, among survivors of childhood parental suicide, loss of a parent may indicate a distal risk factor for suicide attempt in offspring, potentially due to the interaction of genetic, epigenetic and environmental vulnerability. According to attachment theory parental death can result in a permanent disruption of attachment29, 30. The severed attachment by parental death has been suggested to have a long-term impact on the mental well-being of the child 31, but this may also depend on the quality of attachment before the loss. The sibling analyses provides some evidence for an environmental impact of losing a parent very early in the course of development, as this analysis compared offspring with similar genetic vulnerability and shared environmental influences blame, anger, responsibility, guilt, and abandonment.
This study builds on the work of prior studies using the same data source that found that offspring of suicide decedents have increased hospitalization risk for suicide attempt, compared to offspring of alive parents and accident decedents. However, when both shape and time to hospitalization for attempt was allowed to vary, pattern of risk for offspring of suicide decedents was more similar than different from offspring who experienced a parental fatal accident, which has been suggested by other studies 15. When the model examined only the differences in time and assumed that the shape was similar between the two groups, offspring of suicide decedents generally had an earlier onset of hospitalization for suicide attempt than offspring of accident decedents. Although the pattern of risk was quantitatively similar between the two groups, it is important to consider that this study cannot elucidate potential qualitative differences before and after parental death between these two groups. Two reviews have suggested that there are unique themes in the bereavement process which differ as suicide survivors often experience intense anger, guilt, responsibility and may feel a profound sense of abandonment 32,2. A recent review noted that the bereavement process differs between offspring of suicide decedents and offspring survivors of other causes of parental death by family functioning before and after the loss; however the review emphasized the need for more longitudinal studies that examine the bereavement process33.
This study also suggested that daughters are more likely to be hospitalized for suicide attempt than sons among those who lost a parent to suicide during early childhood or adolescence; however, no gender differences were noted among offspring who lost a parent to suicide during later childhood. This study could not distinguish whether this gender difference was due to differences in the prevalence of psychiatric disorders such as depression between males and females at a younger age. Although gender differences may also be due to the higher likelihood of females to attempt suicide than males (males are however more likely to die by suicide) 34, 35, future studies should examine this evidence more closely. Previous studies have suggested that offspring of maternal suicide decedents had higher risk for suicide attempt hospitalization than offspring of maternal fatal accident 11. However, in the present analyses when offspring of maternal suicide decedents were directly compared with offspring of paternal suicide decedents, we did not find a significant difference in the hazard pattern of hospitalization for suicide attempt. The finding suggests that although losing a mother to suicide and to accident may be vastly different, parental gender may not have a significant impact on the risk trajectory for hospitalization for suicide attempt in offspring survivors of parental suicide. This study was underpowered to double stratify by both the gender of the parent and offspring to examine whether female offspring who lost their mother to suicide or males who lost their father to suicide had differing risk trajectories.
This study further solidified evidence showing that child survivors of parental death are at increased risk for suicide attempt hospitalization that persists for decades and that this risk trajectory differs from older offspring survivors of parental death. The study findings have implications for clinicians and parents to monitor risk for suicide attempt that may vary depending on when the child experienced parental death and by offspring gender. An emphasis may be placed on more immediate support for adolescent and young adult offspring who lost a parent. However, the cumulative risk in young offspring survivors suggests the importance of providing proactive long-term support. Although the relative risk for hospitalization for suicide attempt was higher among those who experienced parental death in childhood than older survivors, hospitalization for suicide attempt was a rare event. The shape of risk was similar between offspring of suicide and accident decedents, although there was some evidence that it occurs earlier in childhood survivors of parental suicide. Future studies could examine if the pattern is similar for other outcomes such as the onset of Major Depression. Future studies should identify malleable factors that could protect and build resilience in young survivors of parental death such as the surviving parent’s health and psychological well-being and support provided by grandparents and other extended family members.
Supplementary Material
eTable 1 Characteristics of Offspring, Suicide Decedents and Surviving Parents by the Developmental Period of Offspring at the Time Parental Fatal Accident Occurred, Identified from Swedish Population-based Registries, 1973-2003
Acknowledgements
The authors wish to acknowledge the National Institute of Drug Abuse for a training award to S. Janet Kuramoto (1F31DA0263182) and NARSAD for a Young Investigator Award to Dr. Holly C. Wilcox. We also thank Dr. Annette Erlangsen for valuable input regarding the study findings. The authors would also like to acknowledge Professor Alvaro Munoz and Christopher Cox from the Department of Epidemiology of the Johns Hopkins Bloomberg School of Public Health for providing consultation in parametric survival analysis (statepi.jhsph.edu).This study was funded by a NARSAD Young Investigator Award to Dr. Holly C. Wilcox and National Institute of Drug Abuse for training support of S. Janet Kuramoto (1F31DA0263182).
Footnotes
All authors report no competing interests.
Previous Presentation. The European Symposium on Suicide and Suicidal Behaviour, Rome, Italy, September 8, 2010.
References
- 1.Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R. World report on violence and health. World Health Organization; Geneva: 2002. [Google Scholar]
- 2.Jordan JR. Is suicide bereavement different? A reassessment of the literature. Suicide and Life-Threatening Behavior. 2001;31(1):91–102. doi: 10.1521/suli.31.1.91.21310. [DOI] [PubMed] [Google Scholar]
- 3.Cerel J, Jordan JR, Duberstein PR. The impact of suicide on the family. Crisis. 2008;29(1):38–44. doi: 10.1027/0227-5910.29.1.38. [DOI] [PubMed] [Google Scholar]
- 4.Cerel J, Padgett JH, Conwell Y, Reed GA. A call for research: the need to better understand the impact of support groups for suicide survivors. Suicide and Life-Threatening Behavior. 2009 Jun;39(3):269–281. doi: 10.1521/suli.2009.39.3.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McMenamy JM, Jordan JR, Mitchell AM. What do suicide survivors tell us they need? Results of a pilot study. Suicide Life Threat Behav. 2008 Aug;38(4):375–389. doi: 10.1521/suli.2008.38.4.375. [DOI] [PubMed] [Google Scholar]
- 6.Brent DA, Oquendo m, Birmaher B, et al. Familial Pathways to Early-Onset Suicide Attempt. Archives of General Psychiatry. 2002;59:801. doi: 10.1001/archpsyc.59.9.801. [DOI] [PubMed] [Google Scholar]
- 7.Kuramoto SJ, Brent DA, Wilcox HC. The impact of parental suicide on child and adolescent offspring. Suicide and Life-Threatening Behavior. 2009 Apr;39(2):137–151. doi: 10.1521/suli.2009.39.2.137. [DOI] [PubMed] [Google Scholar]
- 8.Hung NC, Rabin LA. Comprehending childhood bereavement by parental suicide: a critical review of research on outcomes, grief processes, and interventions. Death Studies. 2009 Sep;33(9):781–814. doi: 10.1080/07481180903142357. [DOI] [PubMed] [Google Scholar]
- 9.Wilcox HC, Kuramoto SJ, Lichtenstein P, Langstrom N, Brent DA, Runeson B. Psychiatric morbidity, violent crime, and suicide among children and adolescents exposed to parental death. Journal of American Academy of Child and Adolescent Psychiatry. 2010 May;49(5):514–523. doi: 10.1097/00004583-201005000-00012. quiz 530. [DOI] [PubMed] [Google Scholar]
- 10.Runeson B, Asberg M. Family history of suicide among suicide victims. American Journal of Psychiatry. 2003 Aug 1;160(8):1525–1526. doi: 10.1176/appi.ajp.160.8.1525. 2003. [DOI] [PubMed] [Google Scholar]
- 11.Kuramoto SJ, Stuart EA, Runeson B, Lichtenstein P, Langstrom N, Wilcox HC. Maternal or paternal suicide and offspring’s psychiatric and suicide-attempt hospitalization risk. Pediatrics. 2010 Oct 18; doi: 10.1542/peds.2010-0974. 2010:peds.2010-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agerbo E, Nordentoft M, Mortensen PB. Familial, psychiatric, and socioeconomic risk factors for suicide in young people: Nested case-control study. British Medical Journal. 2002;325(7355):74–77. doi: 10.1136/bmj.325.7355.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pfeffer CR, Karus D, Siegel K, Jiang H. Child survivors of parental death from cancer or suicide: depressive and behavioral outcomes. Psychooncology. 2000 Jan-Feb;9(1):1–10. doi: 10.1002/(sici)1099-1611(200001/02)9:1<1::aid-pon430>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 14.Cerel J, Fristad MA, Weller EB, Weller RA. Suicide-bereaved children and adolescents: A controlled longitudinal examination. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(6):672–679. doi: 10.1097/00004583-199906000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Brown AC, Sandler IN, Tein JY, Liu X, Haine RA. Implications of parental suicide and violent death for promotion of resilience of parentally-bereaved children. Death Studies. 2007;31(4):301–335. doi: 10.1080/07481180601187092. [DOI] [PubMed] [Google Scholar]
- 16.Slama F, Courtet P, Golmard JL, et al. Admixture analysis of age at first suicide attempt. Journal of Psychiatric Research. 2009 Jul;43(10):895–900. doi: 10.1016/j.jpsychires.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 17.Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–723. [Google Scholar]
- 18.Schwarz G. Estimating the Dimension of a Model. The Annals of Statistics. 1978;6(2):461–464. [Google Scholar]
- 19.Schneider MF, Gange SJ, Williams CM, et al. Patterns of the hazard of death after AIDS through the evolution of antiretroviral therapy: 1984-2004. AIDS. 2005;19(17):2009–2018. doi: 10.1097/01.aids.0000189864.90053.22. [DOI] [PubMed] [Google Scholar]
- 20.Cox C, Chu H, Schneider MF, Muñoz A. Parametric survival analysis and taxonomy of hazard functions for the generalized gamma distribution. Statistics in Medicine. 2007;26(23):4352–4374. doi: 10.1002/sim.2836. [DOI] [PubMed] [Google Scholar]
- 21.Cleves MA, Gould WW, Gutierrez RG, Marchenko YU. An introduction to survival analysis using Stata. 2nd ed A Stata Press Publication; College Station, TX: 2008. [Google Scholar]
- 22.Kelly PJ. A Review of Software Packages for Analyzing Correlated Survival Data. The American Statistician. 2004;58(4):337–342. [Google Scholar]
- 23.Stata Statistical Software: Release 10.0 [computer program] Stata Corporation; College Station, TX: 2007. Version. [Google Scholar]
- 24.Melhem NM, Walker M, Moritz G, Brent DA. Antecedents and sequelae of sudden parental death in offspring and surviving caregivers. Archives of Pediatrics Adolescent Medicine. 2008 May 1;162(5):403–410. doi: 10.1001/archpedi.162.5.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. American Journal of Psychiatry. 1996 Aug;153(8):1001–1008. doi: 10.1176/ajp.153.8.1001. [DOI] [PubMed] [Google Scholar]
- 26.Runeson B. Psychoactive substance use disorder in youth suicide. Alcohol and Alcoholism. 1990 Jan 1;25(5):561–568. 1990. [PubMed] [Google Scholar]
- 27.Rich CL, Young D, Fowler RC. San Diego Suicide Study: I. Young vs Old Subjects. Archives of General Psychiatry. 1986 Jun 1;43(6):577–582. doi: 10.1001/archpsyc.1986.01800060071009. 1986. [DOI] [PubMed] [Google Scholar]
- 28.Dowdney L. Childhood bereavement following parental death. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2000;41(7):819–830. 10// [PubMed] [Google Scholar]
- 29.Bowlby J. Attachment and loss: Retrospect and prospect. 1983. [DOI] [PubMed]
- 30.Bowlby J. The making and breaking of affectional bonds. I. Aetiology and psychopathology in the light of attachment theory. An expanded version of the Fiftieth Maudsley Lecture, delivered before the Royal College of Psychiatrists, 19 November 1976. The British journal of psychiatry; the journal of mental science. 1977;130:201–210. doi: 10.1192/bjp.130.3.201. 03// [DOI] [PubMed] [Google Scholar]
- 31.Mack KY. Childhood family disruptions and adult well-being: The differential effects of divorce and parental death. Death studies. 2001;25(5):419–443. doi: 10.1080/074811801750257527. [DOI] [PubMed] [Google Scholar]
- 32.Bailley SE, Kral MJ, Dunham K. Survivors of suicide do grieve differently: empirical support for a common sense proposition. Suicide Life Threat.Behav. 1999;29(3):256–271. [PubMed] [Google Scholar]
- 33.Hung NC, Rabin LA. Comprehending childhood bereavement by parental suicide: A critical review of research on outcomes, grief processes, and interventions. Death Studies. 2009;33:781–814. doi: 10.1080/07481180903142357. [DOI] [PubMed] [Google Scholar]
- 34.Canetto SS, Sakinofsky I. The gender paradox in suicide. Suicide and Life-Threatening Behavior. 1998 Spring;28(1):1–23. [PubMed] [Google Scholar]
- 35.Beautrais A. Suicide and serious suicide attempts in youth: a multiple-group comparison study. American Journal of Psychiatry. 2003;2003(160):1093–1099. doi: 10.1176/appi.ajp.160.6.1093. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1 Characteristics of Offspring, Suicide Decedents and Surviving Parents by the Developmental Period of Offspring at the Time Parental Fatal Accident Occurred, Identified from Swedish Population-based Registries, 1973-2003