Abstract
Background
Peritoneal dialysis (PD) is the preferred dialysis modality for many end-stage renal disease (ESRD) patients in the US. However, in sharp contrast to the high rates of PD use in other industrialized countries, utilization of PD in the US is low and declining. PD availability is a necessary condition for PD utilization; however, little is known about the availability and geographic distribution of PD services. This study describes trends in the regional supply of PD services among dialysis facilities between 1995 and 2003.
Study design
Longitudinal cohort study.
Setting and participants
Non-federal outpatient dialysis facilities treating ESRD patients in the US using data from the US Renal Data System.
Predictors
Annual ESRD patient and dialysis facility composition in hospital referral regions.
Outcome
Annual proportion of dialysis facilities offering PD treatment services in hospital referral regions.
Results
The average proportion of facilities offering PD services in hospital referral regions was 56% in 1996, which declined to 47% in 2003. There was geographic variation in PD services, with greater PD availability in metropolitan cities (compared to rural regions) and the Northeast (relative to the South and Midwest). Variation in PD availability was not explained by disease trends or patient characteristics believed to be important for PD use. An increasing regional presence of chain-affiliated facilities was associated with less PD supply.
Limitations
Accuracy of patient registry data, inability to account for consolidation of PD services among chain providers, sensitivity of results to definition of regional markets.
Conclusions
The small and declining availability of PD seems counterintuitive given its demonstrated appeal to patients and payers. Further research is needed to further investigate dialysis facilities’ role in the underutilization of a potentially useful therapy.
Keywords: peritoneal dialysis, end-stage renal disease, organization and delivery of care, longitudinal trends, geographic variation
BACKGROUND
In 2006, over 500,000 Americans were treated for end-stage renal disease (ESRD) at an annual cost of $33.6 billion.1 Growth in the ESRD population and the limited availability of kidneys for transplantation have increased utilization and federal outlays for dialysis services. Although peritoneal dialysis (PD) offers an effective, convenient, and less expensive alternative to hemodialysis (HD), its use in the US has been low: PD use peaked at 14% of all incident ESRD patients in 1985, and has continuously declined since 1995 to a current rate of 6.2%.1 This rate is far below other North American, Asian, and European countries where 20–81% of ESRD patients were treated with PD.2
This low utilization of PD in the US is inconsistent with the demonstrated appeal of PD to patients, providers, and payers. Studies have demonstrated that PD is preferred by many dialysis patients.3–6 In terms of optimal clinical outcomes, cost-effectiveness and quality of life, 33–40% of nephrologists believe PD is appropriate for half their patients. Medicare, the primary payer of health care services for ESRD patients in the US, spent an average $18,562 less per PD patient than for each HD patient in 2006.1 Medicare provides financial incentives for facilities to provide PD services by reimbursing facilities the same prospective reimbursement (i.e., a composite rate) for either PD or HD treatment, even though PD is less costly for facilities.7, 8 In light of this evidence, the low and declining utilization of PD in the US is perplexing.
Much of the empirical evidence on the declining use of PD has focused on individual determinants of PD utilization and has not explained the low and declining use of PD.9–11 In spite of clinical improvements among incident PD patients, the decline in PD use has not been attributable to patient characteristics.11 Although some differences across dialysis organizations have been observed,12 little attention has been paid to the availability of PD services at dialysis facilities even though its supply may influence physicians’ and patients’ choice of treatment. Ultimately, the availability of PD services is the necessary condition from which PD utilization can occur. Earlier studies cross-sectionally examined PD supply and found a tendency for facilities offering PD to target areas with patient populations appropriate for PD therapy.13–15 Yet it is not clear where PD services are available and how this distribution of supply has changed because few studies have examined the dynamics of PD services longitudinally.16–18
In this study, we employed longitudinal and geographic methods to describe trends in the regional supply of PD services between 1995 and 2003. We also tested hypotheses of whether PD was available in areas where it may be needed most. Since many incident dialysis patients prefer PD when informed of their dialysis options,3, 4, 19 we examined trends in PD supply in relation to area characteristics with the greatest potential for PD demand such as rural locations and regions with high incidence of ESRD, as well as areas in which ESRD patients are more likely to have characteristics associated with PD use such as White, young, and employed ESRD populations.5, 20
METHODS
Study design and data
We conducted a longitudinal cohort study of all ESRD patients and dialysis facilities in the US between 1995 and 2003. The study sample included non-federal outpatient dialysis facilities located in the US and District of Columbia as well as all prevalent ESRD patients receiving any ESRD-related service during the study period. The data for this study come from multiple sources, but the principal source of information on ESRD providers and patients came from US Renal Data System (USRDS).
Dialysis facility characteristics, treatment service offerings, and operating statistics came from the Centers for Medicare and Medicaid Services Annual Facility Survey (CMS-2744, USRDS-FACILITY file). We accounted for facilities that opened and closed during the study period, and paid particular attention to facilities that were sold or purchased by other organizational entities. CMS assigns new provider identification numbers to facilities undergoing changes in ownership and, as a result, facilities that were acquired may have multiple provider identification numbers, even though their physical location and staffing remain intact. We tracked changes in ownership, obtained facility addresses and information regarding facility affiliation with any chain organization by augmenting USRDS data with information from the CMS Provider of Service file. From these merged data, we improved the accuracy and quality of our facility-level data by removing invalid or duplicate submissions and obtaining more information on chain affiliation. To retain as many facility observations as possible for analysis, missing facility survey data (< 0.50% of facilities) was imputed using the value of the preceding or subsequent year (or the average of both, if available).
Patient characteristics were obtained from information in the Medical Evidence Report (CMS-2728). Since a new report was required for all patients beginning or re-entering ESRD service, we tracked changes in patient characteristics and residence over time. Data on ESRD patients between 1995 and 2003 was culled from two USRDS files. The PATIENTS file contains information on patients’ first date of ESRD service, demographic information, and date of death. Patient movement over time was tracked using patient zip codes from the RESIDENC file.
Demographic characteristics were obtained from several sources. County-level demographic statistics from the Area Resource File were converted to the zip code-level based on land-area weighting. Healthcare provider census data was obtained from the American Hospital Association’s Annual Hospital Survey and American Medical Association’s Physician Masterfile.
All zip code-level dialysis facility, ESRD patient, and demographic data were aggregated to generate region-level statistics based on Hospital Referral Regions (HRRs) for each year of the study period. HRRs may be a more valid measure of healthcare markets than municipal designations (e.g., counties, metropolitan statistical areas) because HRR boundaries are based on actual patient utilization, thereby reflecting the geographic extent of healthcare markets for tertiary care.21 HRRs are particularly appropriate for studies of ESRD services because ESRD patients receive a significant amount of specialized non-dialysis care in tertiary settings.22 Furthermore, the larger geographic area of HRRs better reflect PD service areas, as PD patients are likely to travel outside county boundaries for their care. Data on zip code assignments to HRRs (n=306) were obtained from geographic boundary files from the Dartmouth Atlas of Health Care.23
Measurements
Our outcome of interest was regional availability of PD services, which we defined as the annual percentage of dialysis facilities in an HRR that reported offering PD treatment services (either continuous ambulatory or continuous cyclic) in the USRDS-FACILITY file. We were unable to measure the extent of PD availability because there are no observable capacity parameters for PD as there are for HD (e.g., number of stations). For the purposes of this descriptive analysis, the proportion of facilities offering PD therapy is appropriate because it is observable; measures availability (i.e., potential utilization); and accounts for differences in the size of regions and dialysis markets.
Potential demand for PD is approximated by several patient characteristics attributed to PD use.5, 20 ESRD incidence was based on date of ESRD onset and HRR residence for a given year and calculated as the number of new ESRD patients per 10,000 general population in each HRR. The remaining patient characteristics were aggregated to the HRR level and measured as a percentage among prevalent ESRD patients. We calculated the percentages of White, African American, Asian, other non-White, and Hispanic patients to represent patient race and ethnicity. The percentage of non-elderly patients represented the proportion of ESRD patients in an HRR younger than 65 years of age. Similarly, the percentage of employed ESRD patients was based on report of either full- or part-time patient employment.
Our analysis also accounted for facility composition in regional markets, including the proportion of facilities that were freestanding units (versus hospital-based), for-profit owned, affiliated with any chain organization, experienced a change in ownership during the year, and were located in urban locations. General market characteristics, such as per capita income, healthcare provider density, and dialysis market competition, served as control variables. Healthcare provider density was operationalized using 1) the number of hospital beds and 2) full time equivalent nephrologist supply per HRR square mile. Because the two measures were highly correlated with one another (r= 0.96), we used factor analysis to construct a single, composite measure.24, 25 Dialysis market competition was calculated using the Herfindahl index, which is equal to the sum of the square of each dialysis facility’s market share (i.e., based on the number of dialysis patients unique to each facility).26 For ease of interpretation, this variable was coded in reverse such that an index value of −1 represented concentrated or monopolistic markets and values approaching 0 characterized unconcentrated, competitive dialysis markets.
Analysis
Univariate statistics were used to 1) generate maps of geographic distributions of PD availability, by HRR, and 2) compare changes in PD supply to patient and facility composition in markets. Multivariate analysis was also conducted using SAS version 9.1 (SAS Institute, www.sas.com) to examine the extent to which PD service availability was related to ESRD patient and facility compositions in the markets. We used generalized estimating equations (GEE) to account for correlations among repeated observations to yield consistent population-averaged parameter estimates.27 All covariates were lagged by one year from the dependent variable. We used Wald chi-square statistics to test the joint significance of groups of covariates in the multivariate model (e.g., patient and facility characteristics). Several additional variables (e.g., proportion of pre-ESRD erythropoietin use, average number of comorbid conditions and average BMI among ESRD patients) were considered, but dropped from the multivariate model because of their high correlations with other patient population attributes that caused multicollinearity in the analysis. The study was approved by the Institutional Review Boards of the University of North Carolina at Chapel Hill and Duke University Health System.
RESULTS
Changes in the supply of PD services over time
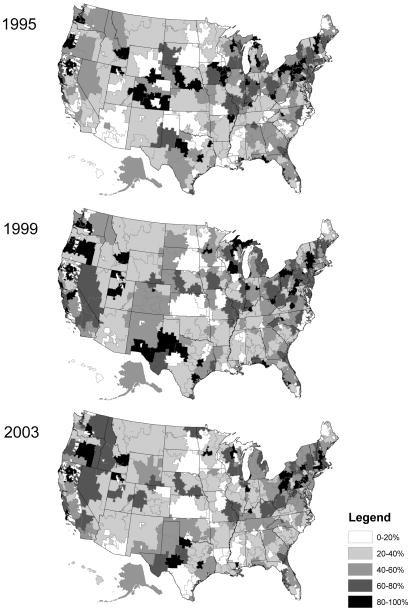
The supply of PD services varied over time and by geographic region. Temporally, the proportion of dialysis facilities offering PD services averaged 51–56% between 1995 and 1999, but declined to 47% in 2003 (Figure 1). Although the total numbers of facilities offering PD services increased over time, PD growth was not proportional to the overall growth of the dialysis industry. The observed downward trend in regional PD availability was due to a more rapid increase in the total number of dialysis facilities entering the dialysis market throughout the study period (not shown). Geographically, PD supply was generally greater in metropolitan cities and the Northeast, and less available in rural regions and in the South and Midwest. Exceptions to these geographic trends over time appear in HRRs in Texas, which experienced growth of PD, and the North Central states, where the proportion of facilities offering PD therapies diminished throughout the study period (not shown).
Figure 1.
Percent of Dialysis Facilities Offering Peritoneal Dialysis Service, by Hospital Referral Region: 1995, 1999, 2003
Association between changes in PD supply and demand for dialysis services
Although there was wide variation in regional markets’ ESRD patient composition (Table 1), overall HRR-level ESRD prevalence and patient demographic trends favorable for PD use were either stable or increased as PD supply declined. The inverse relationships found in unadjusted annual trends (Table 2) suggests that PD supply did not appear responsive to characteristics known to favor PD use among ESRD patients.
Table 1.
Descriptive Statistics of Regional PD Supply and Hospital Referral Region Composition, 1995–2003
| N= 2,754 HRR-years | Mean ± SD | Range |
|---|---|---|
| % Facilities with any PD service | 51.0 ± 26.4 | (0, 100) |
| ESRD patient composition | ||
| Incidence (per 10,000 pop) | 3.4 ± 1.57 | (0.7, 17.2) |
| Prevalence (per 10,000 pop) | 18.3 ± 8.0 | (3.4, 80.9) |
| Race | ||
| % White | 71.7 ± 20.7 | (14.4, 99.6) |
| % African American | 23.4 ± 21.3 | (0, 79.7) |
| % Asian | 2.4 ± 5.9 | (0, 83.0) |
| % Other race | 2.5 ± 5.0 | (0, 42.1) |
| % Hispanic ethnicity | 5.0 ± 8.9 | (0, 73.3) |
| % Non-elderly | 59.2 ± 5.7 | (29.5, 75.1) |
| % Employed | 7.0 ± 3.9 | (0, 20.7) |
| Dialysis facility composition | ||
| % For profit-owned | 68.7 ± 31.3 | (0, 100) |
| % Chain affiliation | 60.4 ± 32.7 | (0, 100) |
| % Freestanding | 74.5 ± 30.2 | (0, 100) |
| % Urban | 70.0 ± 30.7 | (0, 100) |
| % ownership change | 4.7 ± 13.5 | (0, 100) |
| Other regional characteristics | ||
| Per capita income (1,000s) | 21.7 ± 4.7 | (8.7, 47.8) |
| Healthcare provider density | −0.1 ± 0.5 | (−0.2, 7.0) |
| Hospital density (beds) | 2.0 ± 10.0 | (0.002, 146.3) |
| Nephrologist density | 0.02 ± 0.1 | (0, 1.6) |
| Dialysis market competition | −0.3 ± 0.3 | (−1.0, −0.01) |
Notes:
- Incidence and prevalence defined as ESRD patients per 10,000 general population in each HRR throughout the year (i.e., period incidence).
- Healthcare provider density is a composite measure of regional supply of hospital beds and nephrologists per square mile.
Table 2.
Unadjusted Trends in Regional PD Supply, ESRD Patient and Facility Composition, by year
| N=306 HRRs | 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 |
|---|---|---|---|---|---|---|---|---|---|
| % Facilities with any PD service | 50.8 | 55.9 | 54.1 | 52.8 | 52.8 | 49.9 | 48.1 | 47.3 | 47.4 |
| ESRD patient composition | |||||||||
| Incidence (per 10,000 pop) | 3.3 | 3.0 | 3.2 | 3.4 | 3.4 | 3.5 | 3.6 | 3.6 | 3.3 |
| Prevalence (per 10,000 pop) | 14.7 | 15.7 | 16.7 | 17.8 | 18.7 | 19.2 | 20.0 | 20.7 | 21.0 |
| Race / ethnicity | |||||||||
| % White | 72.3 | 72.1 | 72.0 | 71.8 | 71.7 | 71.6 | 71.4 | 71.3 | 71.1 |
| % African American | 23.4 | 23.4 | 23.4 | 23.4 | 23.4 | 23.4 | 23.4 | 23.4 | 23.5 |
| % Asian | 2.1 | 2.2 | 2.2 | 2.3 | 2.4 | 2.5 | 2.5 | 2.6 | 2.6 |
| % Other race | 2.2 | 2.3 | 2.4 | 2.4 | 2.5 | 2.6 | 2.6 | 2.7 | 2.8 |
| % Hispanic ethnicity | 1.9 | 3.0 | 3.9 | 4.6 | 5.2 | 6.1 | 6.5 | 6.8 | 7.3 |
| % Non-elderly | 61.1 | 60.3 | 59.7 | 59.2 | 58.9 | 58.7 | 58.5 | 58.2 | 58.3 |
| % Employed | 1.6 | 3.4 | 4.9 | 6.3 | 7.5 | 8.5 | 9.5 | 10.3 | 11.2 |
| Dialysis facility composition | |||||||||
| % For profit-owned | 57.0 | 60.8 | 65.2 | 69.8 | 71.9 | 73.1 | 74.8 | 72.5 | 73.0 |
| % Chain affiliation | 29.5 | 41.1 | 53.5 | 61.7 | 67.1 | 68.2 | 71.5 | 73.7 | 77.6 |
| % Freestanding | 64.3 | 69.4 | 71.5 | 73.4 | 75.2 | 76.5 | 78.3 | 80.4 | 81.4 |
| % Urban | 71.9 | 71.6 | 70.8 | 70.1 | 69.5 | 68.8 | 69.0 | 69.0 | 69.2 |
| % ownership change | 4.7 | 7.2 | 6.3 | 6.2 | 4.6 | 6.1 | 4.1 | 2.3 | 1.0 |
Note:
- Incidence and prevalence defined as ESRD patients per 10,000 general population in each HRR throughout the year (i.e., period incidence).
PD service availability appeared to be more associated with organizational characteristics of dialysis facilities. The steady decline of PD service availability occurred at a time of marked increases in the proportions of for-profit, chain-affiliated, and freestanding (non-hospital based) dialysis facilities across HRRs. These trends reflected a period of growth of freestanding facilities and changes in facility ownership to for-profit and chain-affiliated entities.
In terms of the association between PD service availability and ESRD patient and provider characteristics (Table 3), PD was less available in HRRs with a greater representation of non-White ESRD patients. Compared to HRRs with a higher proportion of White ESRD patients, a 10 percentage point increase in African American ESRD patients within HRRs was associated with 2.6% fewer dialysis facilities with PD services in HRRs (β= −0.26; p= 0.0001) and 6.2% among “other non-White” ESRD patients (β= −0.62; p= 0.004). A 10 percentage point increased presence of chain-affiliated facilities in HRRs was associated with 0.4% less PD service availability (β= −0.04; p= 0.08). However, a similar increase among dialysis facilities in urban settings was associated with 1.1% more PD availability in HRRs (β= 0.11; p= 0.0006).
Table 3.
GEE Results: Effects of Regional Patient and Dialysis Facility Composition on Percent of Dialysis Facilities Offering Peritoneal Dialysis Service, 1995–2003
| N = 2,448 HRR-years | β | (95% CI) | P | χ2 | P |
|---|---|---|---|---|---|
|
|
|
||||
| ESRD patient composition | 36.42 | <0.0001 | |||
| Incidence (per 10,000 pop) | −0.90 | (−2.07, 0.28) | 0.1 | ||
| Race / ethnicity (ref: White) | |||||
| % African American | −0.26 | (−0.39, −0.13) | 0.0001 | ||
| % Asian | −0.26 | (−0.57, 0.05) | 0.1 | ||
| % Other race | −0.62 | (−1.05, −0.20) | 0.004 | ||
| % Hispanic ethnicity | −0.16 | (−0.39, 0.07) | 0.2 | ||
| % Non-elderly | −0.14 | (−0.55, 0.28) | 0.5 | ||
| % Employed | −0.49 | (−1.18, 0.19) | 0.2 | ||
| Dialysis facility composition | 15.09 | 0.01 | |||
| % For-profit owned | −0.002 | (−0.06, 0.05) | 0.9 | ||
| % Chain-affiliated | −0.04 | (−0.07, 0.004) | 0.08 | ||
| % Freestanding | 0.02 | (−0.05, 0.08) | 0.6 | ||
| % Urban location | 0.11 | (0.05, 0.17) | 0.0006 | ||
| % Ownership change | −0.02 | (−0.05, 0.02) | 0.4 | ||
| Other regional characteristics | 22.53 | <0.0001 | |||
| Per capita income | 0.76 | (0.26, 1.27) | 0.003 | ||
| Healthcare provider density | 2.82 | (−1.47, 7.12) | 0.2 | ||
| Dialysis market competition | −15.96 | (−25.23, −6.69) | 0.0007 | ||
Notes:
- Covariates in the multivariate model are lagged by one year of the dependent variable.
- The statistical model also controlled for year indicators (not shown).
- ESRD incidence is modeled because PD may be more appropriate for early dialysis patients or those with residual renal function. However, modeling ESRD prevalence (in lieu of incidence) on PD supply yielded similar results.
- To test groups of variables (e.g., patient composition, facility composition), we conducted Wald tests. Results of the Chi-square statistics and p-values are reported here.
DISCUSSION
To the best of our knowledge, this is the first study to describe temporal trends in PD service availability in dialysis facilities. In contrast to prior studies, we examined the underutilization of PD by exploring the availability of PD services, which is a precondition of PD utilization and observed outcomes. The data presented here fills a gap in the literature by exploring trends in PD service offerings among dialysis facilities over time, the extent of geographic variation in PD service availability, and the factors related to the availability of PD services.
We found that there has been a low and declining proportion of dialysis facilities offering PD services over time and that the availability of PD services has varied by geography. We also found that variations in PD service availability did not appear to be explained by disease incidence or patient characteristics associated with increased PD utilization. This finding is consistent with prior patient-level analyses of PD utilization in that declines in either PD availability or utilization could not be fully explained by other patient factors over time.11 The negative association we found between the percentages of non-White ESRD patients and PD supply aligns with our expectations. However, the negative associations we found between ESRD incidence, non-elderly, and employed patient populations on PD availability were surprising because it suggests that PD services may not be available to patients who have been known to use and benefit from it.
Given Medicare’s equal payment for dialysis treatments and lower facility costs associated with PD, we expected the potential profitability of PD to increase its availability, especially among for-profit, chain-affiliated, and freestanding facilities that dominate the US dialysis industry. However, the only significant relationship was between increasing proportions of chain-affiliated facilities and less regional PD supply. This finding is consistent with extant literature13 that suggests that consolidation and increased market share of chain organizations in the dialysis industry contributed to the decline in PD services. Although we did not find ownership change to be related to PD service availability, it is still possible that chains have standardized service modalities across affiliated sites or consolidated their PD service lines into a few units that take on a large number of PD patients,28 especially in regions with a high density of dialysis facilities. The negative correlation we found between the percentage of chain-affiliated dialysis facilities and PD supply (r= −0.20, not shown) suggests that this may be the case. However, due to the lack of reliable information needed to formally examine the extent of PD consolidation, these claims remain untested.29 Future research, incorporating detailed data on facilities’ affiliation with specific chain organizations, may elucidate our understanding of the provision of PD services among chain dialysis providers.
Our study has several limitations. First, although our study showed that a smaller percentage of dialysis facilities offered PD services during the study period, facilities may have increased their capacity for PD therapy. However, the possibility of increased capacity could not be assessed using our data. In view of the declining rate of PD use among ESRD patients, we suspect that the likelihood of capacity increase was small and that, if it occurred, the increase would be limited to a small number of dialysis facilities. Second, it is also possible that chain organizations have consolidated PD programs, reducing the number of facilities offering PD without affecting PD availability. Sole use of USRDS chain-specific affiliation, which identifies only the nine largest chain organizations, ignores the potential significance of smaller or regional chains that may bias our findings. Combining USRD and CMS data allowed us to determine affiliation with any chain organization, but did not allow for reliable assessment of chain-specific effects or PD consolidation over time. Third, the accuracy of reported data and data collection methods may affect the results of our analysis. For example, because facilities and physicians are required to submit patient documentation only when a patient begins a new treatment modality or transfers to a new facility, changes in patients’ employment or comorbidities may not always be accurate. However, the USRDS patient registry data is the best known source of comprehensive data on ESRD patients at the national level. Fourth, our findings may be sensitive to the definition of regional markets. Because counties and hospital services areas do not adequately reflect health service use, particularly for PD services, we chose HRRs to better reflect cross-county travel to dialysis facilities’ PD services. Although HRRs may be too large, PD-specific geographic markets do not exist. Finally, there are myriad factors contributing to the declining supply of PD services that were not examined. For example, the availability of clinicians (e.g., nephrologists, nurses, and surgeons) with PD training and experience could not be readily measured, but are important factors in dialysis facilities’ decision to provide PD services.30–32
Despite these limitations, our study contributes to the literature on the low use of PD in the US. Our evidence of geographic variations and declining regional supply of PD therapy seems counterintuitive to the evidence on the clinical and individual factors driving PD preference and use. The trends presented here are also particularly timely and raise concerns about costs, quality, and patient access to ESRD care. The diminishing supply of PD therapies across regions suggests possible missed opportunities in achieving cost savings in the Medicare ESRD program, the primary payer for over 90% of the nation’s ESRD care.1 Medicare’s overall ESRD costs are generally lower in regions where PD is more prevalent than where PD is less common.22 PD is less expensive and more cost-effective than HD in terms of dialysis costs and, after including hospitalizations due to dialysis, overall Medicare ESRD costs.7, 33–35 These cost savings persist even among patients who begin PD in the first year of dialysis and later switch to HD.36 Recent analysis conservatively estimated that an increase in PD use from 8% to 15% would save Medicare over $1.1 billion in Medicare over five years.37
The declining availability of PD services may limit quality of ESRD care. There is evidence that 1) PD patients report better quality of life and fewer negative aspects of life than HD patients;19, 38, 39 2) up to 40% of nephrologists believe PD is an appropriate and cost-effective modality for half of their ESRD patients;40, 41 and 3) when informed of all their treatment options, many pre-ESRD and dialysis patients prefer PD.3, 4, 19 However, only one quarter of patients ever recall the option of PD being discussed when dialysis was initiated.42 Even when pre-ESRD is detected early enough to allow physicians and patients time to develop a treatment plan, the limited availability of PD services may adversely affect modality choice43 and inhibit the alignment of ESRD care with patient preferences.
Lastly, the declining supply of PD therapies raises concern about disparities in access to PD. One advantage of PD is less frequent travel for dialysis maintenance, which may appeal to patients lacking adequate transportation or living long distances from dialysis facilities. Consistent with prior research, we found less PD supply in rural regions.14 It is possible that distance to facilities may not be a significant barrier to PD use, since the required monthly visits may not prevent rural ESRD patients from receiving PD treatment in urban locales. However, we also found 25 HRRs (8.2% of all HRRs), in regions largely characterized as rural, with small (if any) metropolitan cities, lacked any facility offering PD service in any given year. Although urbanicity was a constant predictor of PD availability, the lack of PD service offerings in rural regions is problematic. Approximately 75% of dialysis facilities in all time periods of the study were located in metropolitan locations. The dearth of PD service may compromise access for ESRD patients for whom PD is appropriate, such as patients lacking adequate vascular access or those intending to preserve vascular access for later use.44, 45 Considering the increasing rates of ESRD incidence among non-elderly patients and minority patients with diabetes,1 it was surprising to find lower PD supply in markets with higher proportions of these potentially PD-appropriate ESRD subpopulations. Additional analysis (not shown) revealed that high ESRD prevalent regions with more non-White ESRD patients had lower PD supply. While PD may not be appropriate for all ESRD patients, it should be an available treatment option.46–48 To address these concerns and inform efforts to improve patients’ access to PD treatment, further study with patient-level data could explore the extents to which modality choice is available and PD services are accessible to various subgroups of ESRD patients. Since ESRD patient characteristics do not seem to adequately explain regional PD supply, it will be important to further examine the forces contributing to the declining availability and utilization of a potentially beneficial therapy.
Acknowledgments
Funding/Support: This research was supported by the National Research Service Award Pre-Doctoral Traineeship from the Agency for Healthcare Research and Quality, sponsored by the Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, Grant No. T32-HS000032 (VW); a Post-Doctoral Fellowship in Health Services Research, sponsored by the US Department of Veteran Affairs (VW); and NIH Grant No. K23-DK075929 (UDP).
The authors thank Matthew Maciejewski, Courtney van Houtven, and Hayden Bosworth for helpful comments on earlier drafts of this work.
Footnotes
Disclaimer: Preliminary results of this study were presented at the American Society of Nephrology 2007 Annual Meeting in San Francisco, CA. The views expressed in this article are those of the authors and do not necessarily reflect the views of the National Institutes of Diabetes and Digestive and Kidney Diseases, US Renal Data System, Department of Veteran Affairs, University of North Carolina at Chapel Hill, or Duke University Health System.
References
- 1.US Renal Data System. USRDS 2008 Annual Data Report: Atlas of End-stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2008. [Google Scholar]
- 2.Dor A, Pauly MV, Eichleay MA, Held PJ. End-stage renal disease and economic incentives: the International Study of Health Care Organization and Financing (ISHCOF) Int J Health Care Finance Econ. 2007 Sep;7(2–3):73–111. doi: 10.1007/s10754-007-9024-9. [DOI] [PubMed] [Google Scholar]
- 3.Ahlmen J, Carlsson L, Schonborg C. Well-informed patients with end-stage renal disease prefer peritoneal dialysis to hemodialysis. Perit Dial Int. 1993;13( Suppl 2):S196–198. [PubMed] [Google Scholar]
- 4.Schreiber M, Ilamathi E, Wolfson M, Fender D, Mueller S, Baudoin M. Preliminary findings from the National Pre-ESRD Education Initiative. Nephrol News Issues. 2000 Nov;14(12):44–46. [PubMed] [Google Scholar]
- 5.Stack AG. Determinants of modality selection among incident US dialysis patients: results from a national study. J Am Soc Nephrol. 2002 May;13(5):1279–1287. doi: 10.1681/ASN.V1351279. [DOI] [PubMed] [Google Scholar]
- 6.Thodis E, Passadakis P, Vargemezis V, Oreopoulos DG. Peritoneal dialysis: better than, equal to, or worse than hemodialysis? Data worth knowing before choosing a dialysis modality. Perit Dial Int. 2001 Jan-Feb;21(1):25–35. [PubMed] [Google Scholar]
- 7.Lee H, Manns B, Taub K, et al. Cost analysis of ongoing care of patients with end-stage renal disease: the impact of dialysis modality and dialysis access. Am J Kidney Dis. 2002 Sep;40(3):611–622. doi: 10.1053/ajkd.2002.34924. [DOI] [PubMed] [Google Scholar]
- 8.McMurray SD, Miller J. Impact of capitation on free-standing dialysis facilities: can you survive? Am J Kidney Dis. 1997 Oct;30(4):542–548. doi: 10.1016/s0272-6386(97)90314-0. [DOI] [PubMed] [Google Scholar]
- 9.Blake PG, Finkelstein FO. Why is the proportion of patients doing peritoneal dialysis declining in North America? Perit Dial Int. 2001 Mar-Apr;21(2):107–114. [PubMed] [Google Scholar]
- 10.Khawar O, Kalantar-Zadeh K, Lo WK, Johnson D, Mehrotra R. Is the declining use of long-term peritoneal dialysis justified by outcome data? Clin J Am Soc Nephrol. 2007 Nov;2(6):1317–1328. doi: 10.2215/CJN.02550607. [DOI] [PubMed] [Google Scholar]
- 11.Mehrotra R, Kermah D, Fried L, et al. Chronic peritoneal dialysis in the United States: declining utilization despite improving outcomes. J Am Soc Nephrol. 2007 Oct;18(10):2781–2788. doi: 10.1681/ASN.2006101130. [DOI] [PubMed] [Google Scholar]
- 12.Mehrotra R, Khawar O, Duong U, et al. Ownership patterns of dialysis units and peritoneal dialysis in the United States: utilization and outcomes. Am J Kidney Dis. 2009 Aug;54(2):289–298. doi: 10.1053/j.ajkd.2009.01.262. [DOI] [PubMed] [Google Scholar]
- 13.Kendix M. Provision of home dialysis by freestanding renal dialysis facilities. Health Care Financ Rev. 1995 Winter;17(2):105–122. [PMC free article] [PubMed] [Google Scholar]
- 14.O’Hare AM, Johansen KL, Rodriguez RA. Dialysis and kidney transplantation among patients living in rural areas of the United States. Kidney Int. 2006 Jan;69(2):343–349. doi: 10.1038/sj.ki.5000044. [DOI] [PubMed] [Google Scholar]
- 15.Schlesinger M, Cleary PD, Blumenthal D. The ownership of health facilities and clinical decisionmaking. The case of the ESRD industry. Med Care. 1989 Mar;27(3):244–258. doi: 10.1097/00005650-198903000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Collins AJ, Hao W, Xia H, et al. Mortality risks of peritoneal dialysis and hemodialysis. Am J Kidney Dis. 1999 Dec;34(6):1065–1074. doi: 10.1016/S0272-6386(99)70012-0. [DOI] [PubMed] [Google Scholar]
- 17.Garg PP, Frick KD, Diener-West M, Powe NR. Effect of the ownership of dialysis facilities on patients’ survival and referral for transplantation. N Engl J Med. 1999 Nov 25;341(22):1653–1660. doi: 10.1056/NEJM199911253412205. [DOI] [PubMed] [Google Scholar]
- 18.Ozgen H, Ozcan YA. A national study of efficiency for dialysis centers: an examination of market competition and facility characteristics for production of multiple dialysis outputs. Health Serv Res. 2002 Jun;37(3):711–732. doi: 10.1111/1475-6773.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rubin HR, Fink NE, Plantinga LC, Sadler JH, Kliger AS, Powe NR. Patient ratings of dialysis care with peritoneal dialysis vs hemodialysis. Jama. 2004 Feb 11;291(6):697–703. doi: 10.1001/jama.291.6.697. [DOI] [PubMed] [Google Scholar]
- 20.Miskulin DC, Meyer KB, Athienites NV, et al. Comorbidity and other factors associated with modality selection in incident dialysis patients: the CHOICE Study. Choices for Healthy Outcomes in Caring for End-Stage Renal Disease. Am J Kidney Dis. 2002 Feb;39(2):324–336. doi: 10.1053/ajkd.2002.30552. [DOI] [PubMed] [Google Scholar]
- 21.Dartmouth Atlas of Health Care Working Group. The Dartmouth Atlas of Health Care in the United States. Chicago, IL: American Hospital Association; 1999. [Google Scholar]
- 22.Hirth RA, Tedeschi PJ, Wheeler JR. Extent and sources of geographic variation in Medicare end-stage renal disease expenditures. Am J Kidney Dis. 2001 Oct;38(4):824–831. doi: 10.1053/ajkd.2001.27702. [DOI] [PubMed] [Google Scholar]
- 23.Dartmouth Atlas of Health Care Working Group. Geographic Boundary Files: Hospital Referral Region. Lebanon, NH: Center for the Evaluative Clinical Sciences; 2003. [Google Scholar]
- 24.DeVellis RF. Scale Development: Theory and Application. 2. Vol. 26. Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]
- 25.Kennedy P. A Guide to Econometrics. 4. Cambridge, MA: MIT Press; 1998. [Google Scholar]
- 26.Folland S, Goodman AC, et al. The Economics of Health and Health Care. 3. Upper Saddle River, NJ: Prentice-Hall, Inc; 2001. [Google Scholar]
- 27.Zeger SL, Liang KY. An overview of methods for the analysis of longitudinal data. Stat Med. 1992 Oct-Nov;11(14–15):1825–1839. doi: 10.1002/sim.4780111406. [DOI] [PubMed] [Google Scholar]
- 28.US Renal Data System. USRDS 2009 Annual Data Report: Atlas of End-stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2009. [Google Scholar]
- 29.Pulliam J, Hakim R, Lazarus M. Peritoneal dialysis in large dialysis chains. Perit Dial Int. 2006 Jul-Aug;26(4):435–437. [PubMed] [Google Scholar]
- 30.Furth SL, Hwang W, Yang C, Neu AM, Fivush BA, Powe NR. Relation between pediatric experience and treatment recommendations for children and adolescents with kidney failure. Jama. 2001 Feb 28;285(8):1027–1033. doi: 10.1001/jama.285.8.1027. [DOI] [PubMed] [Google Scholar]
- 31.Mehrotra R, Blake P, Berman N, Nolph KD. An analysis of dialysis training in the United States and Canada. Am J Kidney Dis. 2002 Jul;40(1):152–160. doi: 10.1053/ajkd.2002.33924. [DOI] [PubMed] [Google Scholar]
- 32.Thamer M, Hwang W, Fink NE, et al. US nephrologists’ recommendation of dialysis modality: results of a national survey. Am J Kidney Dis. 2000 Dec;36(6):1155–1165. doi: 10.1053/ajkd.2000.19829. [DOI] [PubMed] [Google Scholar]
- 33.Bruns FJ, Seddon P, Saul M, Zeidel ML. The cost of caring for end-stage kidney disease patients: an analysis based on hospital financial transaction records. J Am Soc Nephrol. 1998 May;9(5):884–890. doi: 10.1681/ASN.V95884. [DOI] [PubMed] [Google Scholar]
- 34.Nissenson AR. Health-care economics and peritoneal dialysis. Perit Dial Int. 1996;16( Suppl 1):S373–377. [PubMed] [Google Scholar]
- 35.Just PM, Riella MC, Tschosik EA, Noe LL, Bhattacharyya SK, de Charro F. Economic evaluations of dialysis treatment modalities. Health Policy. 2008 May;86(2–3):163–180. doi: 10.1016/j.healthpol.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 36.Shih YC, Guo A, Just PM, Mujais S. Impact of initial dialysis modality and modality switches on Medicare expenditures of end-stage renal disease patients. Kidney Int. 2005 Jul;68(1):319–329. doi: 10.1111/j.1523-1755.2005.00413.x. [DOI] [PubMed] [Google Scholar]
- 37.Neil N, Guest S, Wong L, et al. The financial implications for medicare of greater use of peritoneal dialysis. Clin Ther. 2009 Apr;31(4):880–888. doi: 10.1016/j.clinthera.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 38.Bass EB, Wills S, Fink NE, et al. How strong are patients’ preferences in choices between dialysis modalities and doses? Am J Kidney Dis. 2004 Oct;44(4):695–705. [PubMed] [Google Scholar]
- 39.Kutner NG, Zhang R, Barnhart H, Collins AJ. Health status and quality of life reported by incident patients after 1 year on haemodialysis or peritoneal dialysis. Nephrol Dial Transplant. 2005 Oct;20(10):2159–2167. doi: 10.1093/ndt/gfh973. [DOI] [PubMed] [Google Scholar]
- 40.Charest AF, Mendelssohn DC. Are North American nephrologists biased against peritoneal dialysis? Perit Dial Int. 2001 Jul-Aug;21(4):335–337. [PubMed] [Google Scholar]
- 41.Mendelssohn DC, Mullaney SR, Jung B, Blake PG, Mehta RL. What do American nephrologists think about dialysis modality selection? Am J Kidney Dis. 2001 Jan;37(1):22–29. doi: 10.1053/ajkd.2001.20635. [DOI] [PubMed] [Google Scholar]
- 42.Mehrotra R, Marsh D, Vonesh E, Peters V, Nissenson A. Patient education and access of ESRD patients to renal replacement therapies beyond in-center hemodialysis. Kidney Int. 2005 Jul;68(1):378–390. doi: 10.1111/j.1523-1755.2005.00453.x. [DOI] [PubMed] [Google Scholar]
- 43.Diaz-Buxo JA, Crawford-Bonadio T. The continuum home program concept. Clin Nephrol. 2008 May;69(5):326–330. doi: 10.5414/cnp69326. [DOI] [PubMed] [Google Scholar]
- 44.Coles GA, Williams JD. What is the place of peritoneal dialysis in the integrated treatment of renal failure? Kidney Int. 1998 Dec;54(6):2234–2240. doi: 10.1046/j.1523-1755.1998.00183.x. [DOI] [PubMed] [Google Scholar]
- 45.Gokal R. Peritoneal dialysis, B: Techniques, indications, and complications of peritoneal dialysis. In: Massry SG, Glassock RJ, editors. Massry & Glassock’s Textbook of Nephrology. 4. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 46.Farias MG, Soucie JM, McClellan W, Mitch WE. Race and the risk of peritonitis: an analysis of factors associated with the initial episode. Kidney Int. 1994 Nov;46(5):1392–1396. doi: 10.1038/ki.1994.410. [DOI] [PubMed] [Google Scholar]
- 47.Kim GC, Vonesh EF, Korbet SM. The effect of technique failure on outcome in black patients on continuous ambulatory peritoneal dialysis. Perit Dial Int. 2002 Jan-Feb;22(1):53–59. [PubMed] [Google Scholar]
- 48.Tanna MM, Vonesh EF, Korbet SM. Patient survival among incident peritoneal dialysis and hemodialysis patients in an urban setting. Am J Kidney Dis. 2000 Dec;36(6):1175–1182. doi: 10.1053/ajkd.2000.19832. [DOI] [PubMed] [Google Scholar]