Abstract
Experiencing a negative consequence related to one’s health behavior, like a medical problem leading to an emergency department visit, can promote behavior change, giving rise to the popular concept of the “teachable moment.” However, the mechanisms of action underlying this process of change have received scant attention. In particular, most existing health behavior theories are limited in explaining why such events can inspire short-term change in some, and long-term change in others. Expanding on recommendations published in the 2009 Academic Emergency Medicine consensus conference on public health in emergency medicine, we propose a new method for developing conceptual models that explain how negative events, like medical emergencies, influence behavior change, called the Sentinel Event Method. The method itself is atheoretical; instead, it defines steps to guide investigations that seek to relate specific consequences or events to specific health behaviors. This method can be used to adapt existing health behavior theories to study the event-behavior change relationship, or to guide formulation of completely new conceptual models. This paper presents the tenets underlying the Sentinel Event Method, describes the steps comprising the process, and illustrates its application to emergency medicine through an example of a cardiac-related emergency department visit and tobacco use.
INTRODUCTION
For many people, health behavior change does not occur as a result of carefully considered planning; rather, it is triggered by a specific event, experience, or consequence of the risky behavior. We call this the Sentinel Event Effect. An emergency department (ED) visit can act as just such an event, with the potential to inspire behavior change far beyond the visit itself. In 2009, Academic Emergency Medicine sponsored a consensus conference on public health in emergency medicine (EM), which recommended that research into public health related questions be guided by formal conceptual models and theories.1 Developing and testing models of how the ED visit can influence behavior change is critical for the maturation of both EM and public health.
Conceptual models should seek to provide a richer understanding of how specific events or consequences of an individual’s behavior relate to the larger context of the individual’s life, explain how these factors work independently and synergistically to predict the onset of behavior change, and further examine how they relate to transitioning to long-term maintenance. This article describes the Sentinel Event Method, a process for building dynamic models aimed at better understanding how discrete negative consequences of a health behavior relate to both short- and long-term behavior change, like how an ED visit resulting from a smoking-related illness influences smoking cessation. This article will present data that support the Sentinel Event Effect, and outline the proposed steps for constructing and testing dynamic conceptual models that relate constructs associated with the event itself to background or tension factors and subsequent behavior change. Emerging trends in health behavior theory building will be incorporated throughout the process. We will illustrate the model building process and how it applies to EM using a cardiac-related ED visit and tobacco use.
THE SENTINEL EVENT EFFECT
Across many medical settings, it is quite common to observe behavior change after a triggering event, or what we call the Sentinel Event Effect. Common examples in the field of EM include tobacco cessation after a cardiac-related health problem, and reduced alcohol consumption after an intoxicated driving collision. These events are commonly referred to as teachable moments. Despite the general acknowledgement of the pattern, and the embrace of the teachable moment concept in clinical practice, surprisingly little has been published on developing conceptual models to help understand the event-behavior change relationship.1,2
As discussed by McBride and colleagues,3 several indirect lines of research converge to support the Sentinel Event Effect. First, the control groups in randomized clinical trials of patients experiencing medical emergencies, like a myocardial infarction, who typically have received only minimal interventions or a placebo, exhibit long-term cessation rates ranging from 34%4 to 59%.5 These non-intervention cessation rates exceed those found in most active treatment groups in trials of healthy participants (~25% to 35%), who typically represent a highly motivated subgroup of smokers, and far surpass the prolonged cessation rate among community-based, unassisted quitters, which is about 3% to 5% per year.6–8 This overarching trend of higher-than-expected cessation is true even for undifferentiated chest pain patients treated in an ED observation unit, most of whom do not have serious cardiac disease, and who are discharged home.9 Finally, it is not just cardiac-related events that seem to inspire smoking cessation among ED patients. Even studies using general, heterogeneous ED patient populations with a broad range of diagnoses exhibit higher-than-expected cessation rates after the visit, especially for patients with more severe illnesses, and who personally attribute their visit to a smoking-related medical problem.2,10
Although individuals suffering a negative health event are more likely to quit smoking than the general community population of smokers, the cycling trend of cessation and relapse seems to affect even severely ill patients. For many individuals, motivation to remain abstinent fades over time as the contextual, affective, and cognitive factors associated with the health event decay, leading to a return of old habits and behaviors. For example, while up to 90% of hospitalized cardiac patients stop smoking at discharge, close to 50% relapse within 12 months.4,11,12 While the long-term cessation rates of cardiac patients remain remarkably high, a large proportion are not successful in the long term. This same cyclical pattern is true for the most medically ill populations, and must factor into any attempt to model the event-behavior change relation.
A study by West and Sohal13 provides additional conceptual support for the Sentinel Event Effect. In a large study of 918 current smokers who reported having made at least one quit attempt and 996 ex-smokers, they found that smokers often have unplanned quit attempts. These unplanned quit attempts appeared to be more successful than those that were a result of conscious forethought and planning. This finding generally runs contrary to predictions arising from many health behavior theories, like the Transtheoretical Model,14 and therapeutic models like Motivational Interviewing,15 all of which emphasize the role of forethought, preparation, and motivation building. Frequently these unplanned quit attempts appear to be triggered by specific events, and we argue that stage-based approaches, or approaches that conceptualize motivation in a linear fashion, may not capture the full picture of behavior change. We advocate a re-formulation of behavior change for substance abuse that integrates baseline tension factors pertaining to background motivation to change with specific triggers that prompt the initiation of cessation, like a medical emergency.
In sum, the extant literature suggests that 1) health events alone, including medical emergencies, can be associated with a greater likelihood of smoking cessation than would otherwise be expected, independent of tobacco treatment; 2) the behavior change brought about by such an event is temporary for some and long-lasting for others; and 3) understanding such behavior change is likely to involve an interplay between background tension and trigger factors.
The Sentinel Event Method of Model Building
In the past decade there has been a notable emergence of constructive discussions surrounding shortcomings of existing health behavior theories, including the Health Belief Model,16,17 the Transtheoretical Model,14 the Theory of Planned Behavior,18 Leventhal’s Self-Regulation Theory,19,20 and Roger’s Protection Motivation Theory.21,22 Notably, Rothman and colleagues have pointed out that traditional theories are “static” models that do not adequately incorporate the dynamic quality of behavioral change over time.21–23
Work by Miller,24 and by Resnicow et al.,25,26 have suggested a Quantum Change approach, modeled after Chaos Theory, to understanding the substantial and dynamic complexities of health behavior change. Quantum Change posits that behavior change is a complex adaptive system with multiple components, is sensitive to initial conditions, and that random events (large or small) may prompt sudden change in behaviors by influencing “key vectors along the [behavior change] pathway and may propel the individual into a dramatically different space.”26 According to Resnicow and Vaughn, “for public health, a relevant question is whether we can identify intrapsychic patterns, initial conditions or behavioral paths within and across individuals that increase the likelihood of tipping into healthy behavior.”26 The Sentinel Events Method attempts to address exactly this question.
We have incorporated many of the new paradigms of theory building into the Sentinel Event Method of model building, including 1) formal incorporation of specific triggers, cues, or motivators that may prompt behavior change efforts; 2) conceptualizing behavioral initiation as a separate process from behavioral maintenance; and 3) attending to the rich and fluid relationship between behaviors, thoughts, feelings, and social context over time. The method is not, itself, a theory or conceptual model. Rather, it is a suggestion for how to systematically develop and test theories in the context of an event as a trigger to change. The steps are outlined below.
Define the behavior and event of interest
The behavior change of interest and the event, consequence, or trigger must be clearly defined. Specificity and operationalization of the behavior and event are crucial. In the current context we are conceptualizing “events” as actual events, such as an ED visit or hospitalization, rather than subjective or internal happenings, such as “hitting bottom,” which is often mentioned as an “event” in the addictions literature. While the chronic or ambient negative consequences of one’s behavior can be very important, the Sentinel Event Method focuses on identifying and defining discrete events and measuring constructs and behavior from that particular reference point.
In our illustrative example, we will focus on smokers (behavior) experiencing chest pain or other symptoms that necessitated an acute cardiac evaluation (event). Cardiac disease is a common consequence of tobacco use, and tobacco use is a prototypical example of the pattern of cyclical change that characterizes cessation of all substance classes. A study using such a sample, therefore, would have good potential for producing a generalizable body of knowledge pertaining to health events, as a category, as well as addictive behaviors in general.
When defining the event, it is important to consider the range or spectrum of illnesses to include. The seriousness of the illness is likely to be an important predictor of behavior change. In our example, then, it would be important to include individuals at the more severe end of the disease spectrum, such as those with a myocardial infarction necessitating coronary artery bypass graft surgery, as well as those on the less severe end of the spectrum, such as patients with chest pain who receive a cardiac work-up but who did not actually have an infarction (false alarm). This is likely to result in reasonable homogeneity of the event (cardiac symptoms prompting an acute evaluation) while studying a population that is likely to have ample heterogeneity in the event-related constructs of interest, such as illness severity.
Define the cognitive, affective, environmental, and social constructs believed to be directly relevant to how the event can inspire change in the behavior of interest
Constructs to be tested may be novel or derived from existing theories. In either case, the investigator should consider including cognitive, affective, environmental, and social domains.
For the sake of our illustration, we used Leventhal’s Self-Regulation Theory, also known as the Common Sense Model,19,20 to help identify constructs. A strong advantage of this theory is its inclusion of both cognitive and affective elements to explain a person’s ability to cope with illness. Self-Regulation Theory posits that an individual crafts mental representations of his or her medical problems, and this can guide future coping behaviors and various outcomes.19,20 A patient constructs beliefs around his or her symptoms, the duration of the illness, perceived causes, perceived impact, and treatment effectiveness. Using Self-Regulation Theory, three primary event-related constructs were identified: 1) perceived event severity, 2) event-related emotional reactions, and 3) smoking-related causal attributions. Perceived event severity is defined as the patient’s perception of the seriousness of his or her current health problem. Event-related emotional reactions include any emotional reaction experienced during the event, like anxiety, fear, sadness, or even relief, such as when reassured that one’s chest pain is not an infarction. Both perceived severity and emotional reactions can be very volatile or state-dependent, arguing for multiple assessments over time. Causal attribution is defined as an individual’s understanding of why he or she has developed the illness in question. In the context of our example, we would be particularly interested in the patient’s perception of whether the medical problem triggering the ED visit is caused or made worse by smoking. All three of these constructs enjoy theoretical prominence, empirical support, alignment with clinical observations, and potential to inform intervention development, which are all factors relevant in choosing specific constructs to study.
Consider non-event related factors that could be important, including background or tension factors
Negative events and behavioral change do not occur in a vacuum, but rather, within the context of an individual’s larger life circumstances. Many behavior change theories take into account the potential influence of the individual’s social and physical environment. Social Cognitive Theory27 includes both personal and environmental/social factors in accounting for behavior change. Other theories, like the Theory of Planned Behavior,18 and the Transtheoretical Model,14 also suggest that behavior change is facilitated in the context of an enabling or supportive environment. These non-event related factors, which are known as background or tension factors because they are present before the event, can persist or change during and after the event as well.
In our example, we have chosen to include several background or tension factors, including demographics, general negative affect, nicotine dependence, actual event severity, and pre-event intention to quit. The model could have contained many more predictors; the list of candidate constructs is very long. However, it is important to design a model that is testable and not overly complex, so we decided to focus on those we deemed most important and most readily measured. Once our specific model is tested, if there are large amounts of variance unaccounted for in smoking behavior, future explorations could examine integrating other variables.
Identify how the event-related and background variables relate to each other and to short- and long-term behavior change
The researcher should specify the anticipated effect of each background factor on the constructs central to the event, and how all constructs, both background and those central to the event, influence the behavior milestones of interest. Because some factors may have an influence on the initiation of a behavior that is quite different from their roles in the long-term maintenance of that behavior, explicit hypotheses pertaining to these transitions should be made. The posited influence of any particular variable need not be conceptualized as having a linear relationship with the behavioral outcome of interest. Non-linear relationships and interaction effects between predictors should be considered and included in the conceptual model, when appropriate.
Although most traditional behavior theories have assumed behavioral change will be maintained over time, the two processes of behavioral initiation and behavioral maintenance most likely differ qualitatively.21–23 That is, the factors that prompt a person to embark on a change in health behavior are not necessarily the same factors that assist individuals in maintaining those changes. For example, an individual may tend to focus on the future when making a decision about initiating a behavioral change, but will focus on an evaluation of success, consequences, and satisfaction since making the initial change when considering maintaining the change.21,22,28 While the majority of existing theories have attended to initiation of behavior change with the assumption that those changes will continue, in reality most behavior change is not maintained over time. The appreciation for the distinction between initiation and maintenance is an impetus behind dynamic model building. In dynamic model building, a set of theoretical constructs are identified and researchers specify how they relate to outcomes at each behavior change milestone, from decision-making to behavior initiation to prolonged change.23
Figures 1 and 2 specify not only the direction of the relations in our hypothetical model but their relative strengths, key interactions, and how the constructs relate to both short- and long-term change. This particular model is currently being tested in a prospective cohort study funded by the National Institute of Drug Abuse (R01DA023170).
Figure 1.
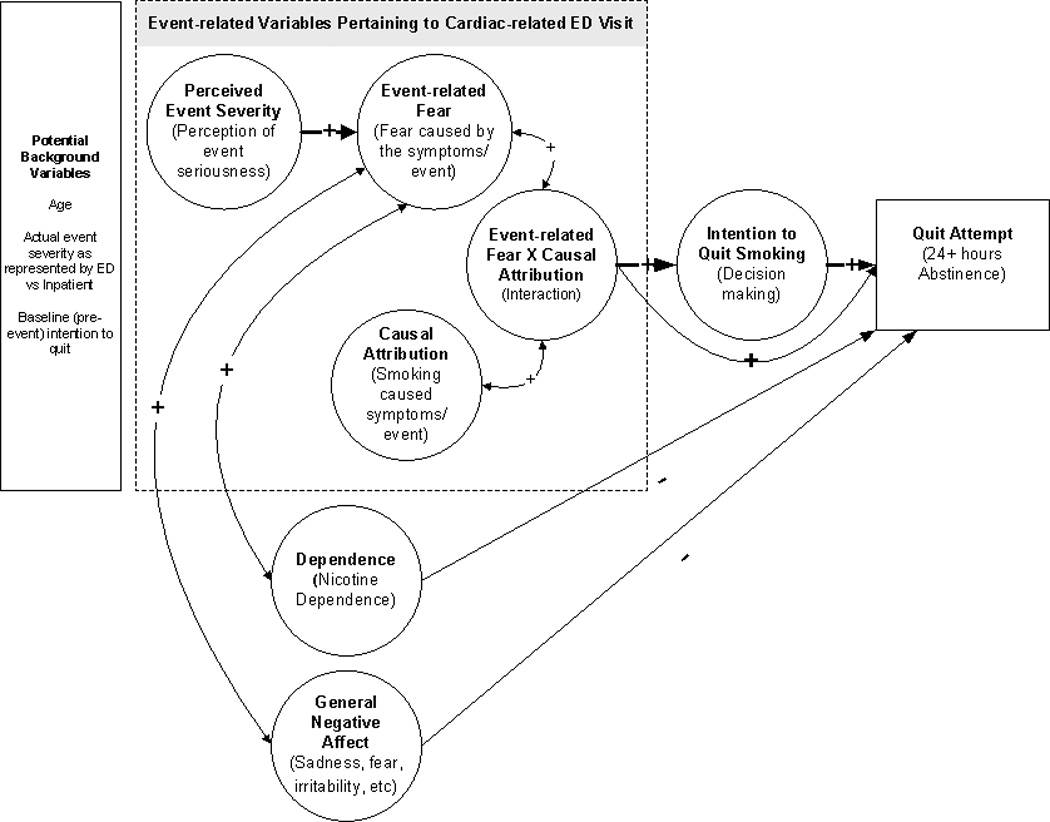
Hypothetical Model of a Sentinel Health Event, Decision-making, and a Quit Attempt
Figure 2.
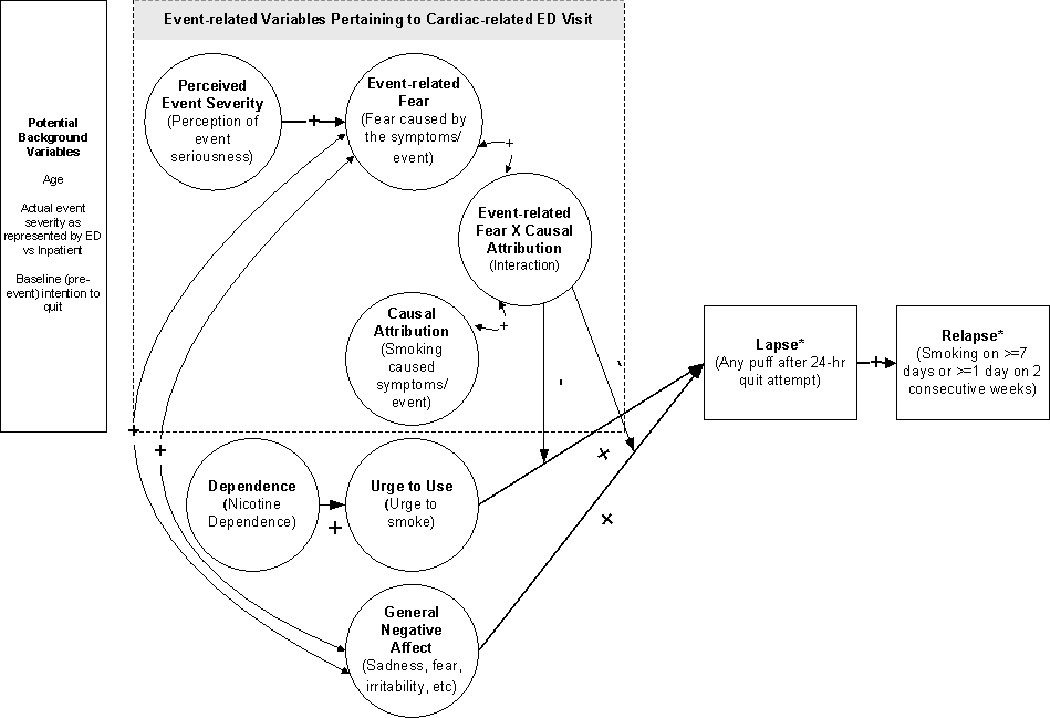
Structural Model of a Sentinel Event, Lapse, and Relapse among Quitters
Develop psychometrically sound measures of all predictors and outcomes in the model, or find existing measures, if available
If the construct is not readily measured by existing assessment instruments, currently validated measures may need to be adapted, or a new instrument may need to be constructed in order to properly assess the constructs of interest in the model.
In our example, we would have to develop and validate measures of perceived severity, emotional reactions, causal attribution, and intentions to quit, because existing measures do not provide the specificity we need. For example, most measures of perceived illness severity refer to the prospect of future illness, while we are more interested in perceptions of an existing condition. A particularly important consideration in event-behavior change studies is developing measures that can be completed across several different time anchors, because, as mentioned earlier, many of these constructs are likely to change over time. An individual may arrive at the ED afraid that he is having a myocardial infarction but leave reassured that he simply has gastritis. Measures that assess constructs in aggregate are likely to miss important variability in the constructs. We do not yet know, for example, if perceptions experienced during the beginning of the ED visit are more (or less) important than those experienced after the ED visit is over.
Test predictions, and modify model accordingly
Ideally, to test predictions pertaining to the effect an event has on behavior change, a cohort that has not yet experienced the event would need to be identified and tracked through the event and beyond, providing a true pre-event baseline against which to compare hypothesized changes in the constructs and behaviors being considered. However, this is not typically feasible, especially when considering a medical emergency. A more practical, although admittedly limited, method is to capture people during or immediately after the event, such as during their ED visits or hospitalizations, then follow them over time. This should permit accurate assessment of constructs from the point of contact forward. Data collected about pre-event constructs or states, such as pre-event motivational readiness, must necessarily rely on recall. While not ideal because of the possible biases introduced by recollection, in most situations this is the only method available to obtain data on potential predictors prior to experiencing the event, unless the event is known ahead of time, such as a study of the effects elective surgery on subsequent health behaviors. Strategies should be considered that help avoid or account for recall biases. For example, in addition to pre-event motivation to change the target behavior, investigators can assess pre-event motivation to change other behaviors that are not theoretically linked to the event. In the case of tobacco and an ED visit, for example, one could assess motivation to change sun screen or seat belt use. This can help to detect the presence of a general contrast effect bias that results in higher ratings of motivation across all behaviors when faced with a pre-post rating task.
In our hypothetical model, we could test all of the various predictions depicted in Figures 1 and 2. We would want to make sure that we choose an analytic strategy that is appropriate for the model and study design. In this case, a particularly appropriate statistical strategy might be structural equation modeling, considering the ability of such analyses to quantify complex relations between many different variables.29
Health Behavior Intervention Development for Emergency Medicine
The field of EM has wrestled with its role in public health and health behavior interventions. On the one hand, there are cultural and logistical barriers that prevent implementation, including the perception of providers that such public health interventions are not within their realm of expertise, and pernicious time and resource constraints. On the other hand, the ED visit may represent an optimal time to intervene because of heightened motivation to change. Moreover, the ED provides much primary care, and if patients do not get behavioral health interventions in the ED, many may not get them at all. The Sentinel Event Method may help to design interventions that are practical and can be tested in emergency care settings, helping to overcome some of the resistance to such interventions.
In many cases, particularly after a model has been tested and refined in observational cohort studies, it can be used to develop an intervention that is designed to influence one or more of the model’s constructs and tested in randomized clinical trials. Such experimental trials are particularly powerful in testing whether hypothetical constructs truly represent mechanisms of action, or whether they are simply correlates or epiphenomenon.
Using our example, if we found support for the role of causal attribution, we could design ED-initiated interventions that target improving the individual’s knowledge and understanding of how smoking is related to chest pain. This might include helping to augment standard provider-based counseling strategies in terms of their emphasis on the relationship between smoking and cardiac disease. Also, it could be used to tailor interactive computer programs that provide targeted health messages to an individual based on his or her particular causal attributions. Finally, biomarker feedback strategies could be used to increase the salience of the effects of a health behavior in real time, such as administering exhaled carbon monoxide testing, and providing feedback pertaining to the results. As the Sentinel Events Method explicitly espouses, factors that influence initiation of behavior change may be different from those that maintain it. Consequently, any intervention initiated during the ED visit will likely require integration with interventions occurring after the visit to promote maximum success.
CONCLUSIONS
The Sentinel Event Method is a process for building dynamic models to help explain both short- and long-term behavior changes that arise from negative health events. By formalizing the specification of trigger events, conceptualizing behavioral initiation as separate from maintenance, and attending to the relationship between behaviors, thoughts, feelings, and social context over time, the Sentinel Event Method can help us advance the clinical notion of “teachable moments” into usable theoretical models. Such models could provide the basis of better, more targeted interventions and aid us in maximally leveraging ED visits to assist patients in initiating and sustaining healthier lifestyles.
Acknowledgments
The project described was supported by Award Number R01DA0231701 from the National Institute on Drug Abuse.
Footnotes
Disclosures: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health. None of the authors have financial conflicts of interest to disclose.
Presentations: none
Contributor Information
Edwin D. Boudreaux, Departments of Emergency Medicine, Psychiatry, and Quantitative Health Sciences, University of Massachusetts Medical School, (EDB) Worcester, MA.
Beth Bock, Centers for Behavioral and Preventive Medicine, Brown University, (BB) Providence, RI.
Erin O’Hea, Department of Psychiatry, University of Massachusetts Medical School, Worcester, MA, and Department of Psychology, Stonehill University, (EO) Easton, MA.
References
- 1.Boudreaux ED, Cydulka R, Bock B, Borrelli B, Bernstein S. Conceptual models of health behavior: research in emergency care settings. Acad Emerg Med. 2009;16:1120–1123. doi: 10.1111/j.1553-2712.2009.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boudreaux ED, Moon S, Baumann BM, Camargo CA, Jr, O’Hea EL, Ziedonis D. Intentions to quit smoking: causal attribution, perceived illness severity, and event related fear during an acute health event. Ann Behav Med. 2010;40:350–355. doi: 10.1007/s12160-010-9227-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18:156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 4.Dornelas EA, Sampson RA, Gray JF, Waters D, Thompson PD. A randomized controlled trial of smoking cessation counseling after myocardial infarction. Prev Med. 2000;30:261–268. doi: 10.1006/pmed.2000.0644. [DOI] [PubMed] [Google Scholar]
- 5.Rigotti NA, McKool KM, Shiffman S. Predictors of smoking cessation after coronary artery bypass graft surgery. Results of a randomized trial with 5-year follow-up. Ann Intern Med. 1994;120:287–293. doi: 10.7326/0003-4819-120-4-199402150-00005. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Smoking cessation during previous year among adults--United States, 1990 and 1991. MMWR Morb Mortal Wkly Rep. 1993;42(26):504–507. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Cigarette smoking among adults---United States 2000. MMWR Morb Mort Wkly Rep. 2002;51(29):642–645. [PubMed] [Google Scholar]
- 8.Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99:29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- 9.Bock BC, Becker BM, Niaura RS, Partridge R, Fava JL, Trask P. Smoking cessation among patients in an emergency chest pain observation unit: outcomes of the Chest Pain Smoking Study (CPSS) Nicotine Tob Res. 2008;10:1523–1531. doi: 10.1080/14622200802326343. [DOI] [PubMed] [Google Scholar]
- 10.Boudreaux ED, Baumann BM, Camargo CA, Jr, O’Hea E, Ziedonis DM. Changes in smoking associated with an acute health event: theoretical and practical implications. Ann Behav Med. 2007;33:189–199. doi: 10.1007/BF02879900. [DOI] [PubMed] [Google Scholar]
- 11.Taylor CB, Houston-Miller N, Killen JD, DeBusk RF. Smoking cessation after acute myocardial infarction: effects of a nurse-managed intervention. Ann Intern Med. 1990;113:118–223. doi: 10.7326/0003-4819-113-2-118. [DOI] [PubMed] [Google Scholar]
- 12.Rosal MC, Ockene JK, Ma Y, et al. Coronary Artery Smoking Intervention Study (CASIS): 5-year follow-up. Health Psychol. 1998;17:476–478. doi: 10.1037//0278-6133.17.5.476. [DOI] [PubMed] [Google Scholar]
- 13.West R, Sohal T. "Catastrophic" pathways to smoking cessation: findings from national survey. BMJ. 2006;332:458–460. doi: 10.1136/bmj.38723.573866.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 15.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, NY: Guilford Press; 1991. [Google Scholar]
- 16.Rosenstock IM. Historical origins of the health belief model. Health Educ Mon. 1974;2:328–335. [Google Scholar]
- 17.Rosenstock IM. The Health Belief Model: explaining health behavior through expectancies. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: theory, research, and practice. San Francisco, CA: Jossey-Bass; 1990. pp. 39–62. [Google Scholar]
- 18.Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckman J, editors. Action-control: from cognition to behavior. Heidelberg, Germany: Springer; 1985. pp. 11–31. [Google Scholar]
- 19.Leventhal H, Nerenz D, Steele D. Baum A, Revernson T, Singer J. Handbook of psychology and health, Vol IV. Hillsdale NJ: Erlbaum; 1984. Illness representations and coping with health threats; pp. 219–252. [Google Scholar]
- 20.Leventhal H, Benyamini Y, Brownlee S, et al. Illness representations: theoretical foundations. In: Petrie K, Weinman J, editors. Perceptions of health and illness: current research and applications. Amsterdam: Harwood Academic Publishers; 1997. pp. 19–45. [Google Scholar]
- 21.Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychol. 2000;19:64–69. doi: 10.1037/0278-6133.19.suppl1.64. [DOI] [PubMed] [Google Scholar]
- 22.Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol Int Rev. 2008;57:1–29. [Google Scholar]
- 23.Rothman AJ, Baldwin AS, Hertel AW, Fuglestad PT. Self-regulation and behavior change: disentangling behavioral initiation and behavioral maintenance. In: Kathleen D, Baumeister RF, editors. Handbook of self-regulation: research, theory, and applications. New York, NY: Guilford Press; 2011. pp. 106–122. [Google Scholar]
- 24.Miller W. The phenomenon of quantum change. J Clin Psychol. 2004;60:453–460. doi: 10.1002/jclp.20000. [DOI] [PubMed] [Google Scholar]
- 25.Resnicow K, Page SE. Embracing chaos and complexity: a quantum change for public health. Am J Public Health. 2008;98:1382–1389. doi: 10.2105/AJPH.2007.129460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Resnicow K, Vaughan R. A chaotic view of behavior change: a quantum leap for health promotion. Int J Behav Nutr Phys Act. 2006;3:e25. doi: 10.1186/1479-5868-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 28.Baldwin AS, Rothman AJ, Hertel AW, et al. Specifying the determinants of the initiation and maintenance of behavior change: an examination of self-efficacy, satisfaction, and smoking cessation. Health Psychol. 2006;25:626–634. doi: 10.1037/0278-6133.25.5.626. [DOI] [PubMed] [Google Scholar]
- 29.Anderson JC, Gerbing DW. Structural equation modeling in practice: a review and recommended two-step approach. Psychol Bull. 1988;103:411–423. [Google Scholar]


