Abstract
Objective
To investigate the effect of various wheelchair tilt-in-space and recline angles on sacral skin perfusion in wheelchair users with spinal cord injury (SCI).
Design
Repeated measures, intervention and outcomes measure design.
Setting
University research laboratory.
Participants
Power wheelchair users with SCI (N=11).
Interventions
Six protocols of various wheelchair tilt-in-space and recline angles were randomly assigned to the participants, including (1) 15° tilt-in-space and 100° recline, (2) 25° tilt-in-space and 100° recline, (3) 35° tilt-in-space and 100° recline, (4) 15° tilt-in-space and 120° recline, (5) 25° tilt-in-space and 120° recline, and (6) 35° tilt-in-space and 120° recline. Each protocol consisted of a 5 min upright sitting and a 5 min tilted and reclined period.
Main Outcome Measures
Skin perfusion over the sacrum (midpoint between the right posterior superior iliac spine and adjacent spinous process) and right ischial tuberosity was measured using laser Doppler flowmetry.
Results
Sacral skin perfusion did not show a significant difference in all six protocols of various tilt-in-space and recline angles when changing from an upright to a tilted and reclined position (N.S.). However, as previously reported, skin perfusion over the ischial tuberosity showed a significant increase at 15°, 25°, and 35° tilt-in-space when combined with 120° recline and at 35° tilt-in-space when combined with 100° recline (P<.0083).
Conclusions
Our results indicate that wheelchair tilt-in-space and recline enhances skin perfusion over the ischial tuberosities without reducing sacral skin perfusion when changing from an upright to a tilted and reclined position.
Keywords: Laser-Doppler, pressure ulcer prevention, skin, spinal cord injury, wheelchair tilt-in-space, wheelchair recline
Specific combinations of wheelchair tilt-in-space and recline angles are recommended for clinically effective pressure relief to reduce risk of pressure ulcers in wheelchair users with spinal cord injury (SCI).1–3 Such clinical practices are based on evidence that wheelchair tilt-in-space and recline can reduce seating pressure.3–5 It has also been demonstrated that ischemic tissues can restore blood flow during these pressure relieving maneuvers.2, 6 Although wheelchair tilt-in-space and recline can be used to reduce risk of pressure ulcers under the ischial tuberosities,1–3 it is unclear whether such activities will increase pressure and reduce blood flow to the tissues over the sacrum, another common site of pressure ulcers.7 Additionally, the use of recline may cause shearing of tissues in the sacral area further increasing risk of tissue ischemia.4
In response to the position paper on the clinical use of wheelchair tilt-in-space and recline published by the Rehabilitation Engineering and Assistive Technology Society of North America (RESNA),1 we have designed a series of studies2, 6 to investigate the effectiveness of wheelchair tilt-in-space and recline on reducing risk of pressure ulcers in wheelchair users with SCI. In our previous study,2, 6 we demonstrated an increase in skin perfusion over the ischial tuberosity in response to wheelchair tilt-in-space and recline. In this study, we hypothesized that wheelchair tilt-in-space and recline causes an increase in skin perfusion over the ischial tuberosity with a decrease of skin perfusion over the sacrum.
METHODS
A repeated measures, intervention and outcome measures research design was used in this study.
Participants
A total of 11 wheelchair users with SCI were recruited into the study. Details of inclusion and exclusion criteria have been previously reported.2 All participants gave informed consent to this study approved by a university institutional review board. The demographic data of participants were as follows (values are mean ± standard deviation): age 37.7±14.2 years; body mass index 24.7± 2.6 kg/m2; and duration of injury 8.1±7.5 years. The 11 wheelchair users included 2 females and 9 males with traumatic SCI at the level of C4 through T5. Four participants had sensory complete injury (American Spinal Injury Association (ASIA) Impairment Scale A), 2 participants had motor complete injury (ASIA B), and 5 participants had incomplete injury (ASIA C). All participants used power wheelchair for mobility.
Apparatus
Laser Doppler flowmetry (LDF)a was used to measure sacral skin perfusion in perfusion unit (or loosely defined as skin blood flow in clinical usage).2, 7 Two thin LDF probesb were placed on the skin over the sacrum (midpoint between the right posterior superior iliac spine (PSIS) and adjacent sacral vertebrae spinous process, or sacral ridge) and right ischial tuberosity, respectively. A power wheelchairc with tilt-in-space and recline functions was used in this study. The seat width was 0.48 m (19 inches) and a standard wheelchair seat cushion and back supportd configured with the wheelchair was used in this study. Two angle gaugese were used to measure the angles of wheelchair seat and back support during the tilt-in-space and recline maneuvers.
Procedure
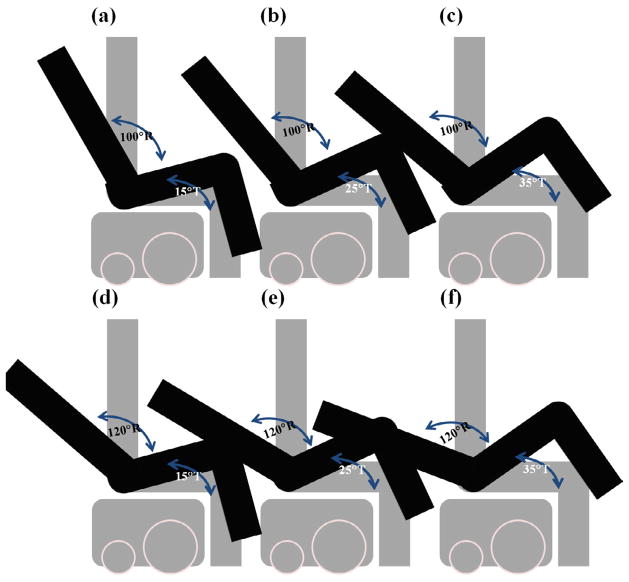
The descriptions of procedures for participant preparation are discussed in Jan et al. (2010).2 Each protocol consisted of a 5 min baseline sitting at no tilt/recline and a 5 min tilted and recline position in one of 6 positions including (1) 15° tilt-in-space and 100° recline, (2) 25° tilt-in-space and 100° recline, (3) 35° tilt-in-space and 100° recline, (4) 15° tilt-in-space and 120° recline, (5) 25° tilt-in-space and 120° recline, and (6) 35° tilt-in-space and 120° recline. A 5 min washout period (at 35° tilt-in-space and 120° recline) was allowed between protocols. The rational of selecting these 6 protocols are discussed in our previous article.2 The configuration of 6 wheelchair tilt-in-space and recline angles are shown in Fig. 1.
Fig 1.
Configurations of 6 combinations of wheelchair tilt-in-space (T) and recline (R) angles. (a) 15° tilt-in-space combined with 100° recline. (b) 25° tilt-in-space combined with 100° recline. (c) 35° tilt-in-space combined with 100° recline. (d) 15° tilt-in-space combined with 120° recline. (e) 25° tilt-in-space combined with 120° recline. (f) 35° tilt-in-space combined with 120° recline.
Statistical Analysis
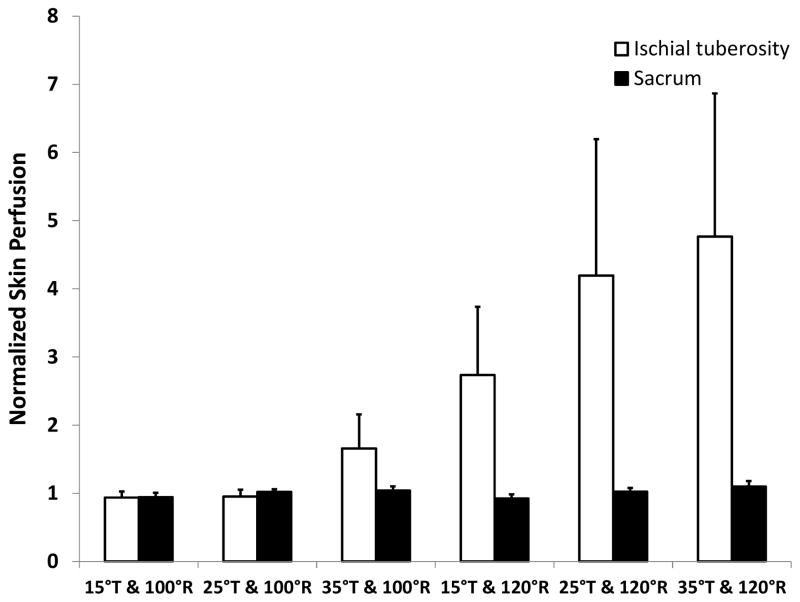
Skin perfusion over the sacrum during a 5 min upright sitting was averaged to establish the baseline perfusion value for each participant. The change of skin perfusion over the sacrum in response to changes in body positions caused by performing wheelchair tilt-in-space and recline was normalized to each participant’s baseline perfusion. A one-way analysis of variances (ANOVA) with repeated measures design was used to examine the effect of wheelchair tilt-in-space and recline on skin perfusion. Paired t tests with Bonferroni corrections were used for post-hoc analysis. All statistical tests were performed at an alpha level of.05 and were adjusted to.0083 for multiple comparisons. All data were analyzed by using SPSS.f Skin perfusion over the right ischial tuberosity in response to wheelchair tilt-in-space and recline reported in our previous publication2 is shown in Fig. 2 for a reference to compare the difference of skin perfusion at the ischial tuberosity and sacrum in response to wheelchair tilt-in-space and recline.
Fig 2.
Comparison of normalized sacral skin perfusion in response to wheelchair tilt-in-space (T: 15°, 25°, 35°) in combination with recline (R: 100°, 120°). Normalized sacral skin perfusion did not show any significant difference between six conditions (N.S.). However, normalized skin perfusion over the ischial tuberosity showed a significant increase at 4 conditions (15°, 25°, and 35° tilt-in-space combined with 120° recline and 35° tilt-in-space combined with 100° recline) (P<.0083). Data shown as mean ± SE.
RESULTS
Sacral skin perfusion did not show a significant difference in all six protocols of various tilt-in-space and recline angles when changing from an upright to a tilted and reclined position (P>.05, N.S.) (Fig. 2). However, as previously reported,2 skin perfusion over the ischial tuberosity showed a significant increase at 15°, 25°, and 35° tilt-in-space when combined with 120° recline (P<.01) and a significant increase at 35° tilt-in-space when combined with 100° recline (P<.0083) (Fig. 2).
DISCUSSION
Although preliminary in nature, our results did not support our hypothesis and showed no indication that sacral skin perfusion decreases during the designated wheelchair tilt-in-space and recline positioning. This result may provide a useful preliminary answer to a clinical problem whether wheelchair tilt-in-space and recline enhances skin perfusion over the ischial tuberosity at the price of causing skin ischemia over the sacrum when a person moves from an upright to a tilted and reclined position.
The selection of skin perfusion as an index to evaluate the efficacy of wheelchair pressure relieving function on tissue viability is based on the consensus of prolonged tissue ischemia as the most important causative factor of pressure ulcers.2, 6, 7 Along with our previous work2, 6 and results from this study, we further showed that wheelchair tilt-in-space and recline may not decrease skin perfusion over the sacrum. According to the principle of skin blood flow response to mechanical stress,7 we conclude that wheelchair tilt-in-space and recline did not increase interface pressure over the sacrum (midpoint between right PSIS and spinous process) because skin perfusion over the sacrum did not show an obvious change when changing from an upright to a tilted and recline position. This may first sound inconsistent with the general seating biomechanics.5, 8 However, based on our results, more weight may transfer to the thoracic and lumbar areas, rather than to the sacrum. If this is true, it represents a positive finding as these areas of the torso are at a relatively lower risk of developing pressure ulcers.9
Study Limitations
We only recruited 11 wheelchair users with SCI into this study. Because this was a feasibility study, we intended to examine whether our protocols could be used to assess the efficacy of wheelchair tilt-in-space and recline on reducing risk of pressure ulcers.2, 6 A larger sample size using this protocol should be conducted to verify our results. Although we used one wheelchair in this study, the dimensions of the seating system fit all participants. Future studies may need to recruit participants with various body sizes and incorporate different wheelchair seat sizes.
CONCLUSION
Our results indicate that wheelchair tilt-in-space and recline enhances skin perfusion over the ischial tuberosity without reducing sacral skin perfusion when changing from an upright to a tilted and reclined position.
Acknowledgments
Supported by the National Institutes of Health (grant no. R03HD060751).
List of Abbreviations
- ASIA
American Spinal Injury Association
- LDF
Laser Doppler Flowmetry
- PSIS
Posterior Superior Iliac Spine
- SCI
Spinal Cord Injury
Footnotes
PeriFlux System 5000 and LDF module 5010, Perimed, Inc, 44 W Lancaster Ave, Ste 220, Ardmore, PA 19003.
Probe PR415, Perimed, Inc, 44 W Lancaster Ave, Ste 220, Ardmore, PA 19003.
Power wheelchair C300 Corpus, Permobil, Inc, 6961 Eastgate Blvd, Lebanon, TN 37090.
Corpus seating system, Permobil, Inc, 6961 Eastgate Blvd, Lebanon, TN 37090.
Digital Angle Gauge, Wixey, available at: http://www.wixey.com.
SPSS 20, SPSS Inc., 233 S Wacker Dr, 11th Fl, Chicago, IL 60606.
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organizations with which the authors are associated.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dicianno BE, Arva J, Lieberman JM, Schmeler MR, Souza A, Philips K, et al. RESNA position on the application of tilt, recline, and elevating legrests for wheelchairs. Assistive Technology. 2009;21:13–22. doi: 10.1080/10400430902945769. [DOI] [PubMed] [Google Scholar]
- 2.Jan YK, Jones MA, Rabadi MH, Foreman RD, Thiessen A. Effect of wheelchair tilt-in-space and recline angles on skin perfusion over the ischial tuberosity in people with spinal cord injury. Arch Phys Med Rehabil. 2010;91(11):1758–64. doi: 10.1016/j.apmr.2010.07.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Michael SM, Porter D, Pountney TE. Tilted seat position for non-ambulant individuals with neurological and neuromuscular impairment: a systematic review. Clin Rehabil. 2007;21(12):1063–74. doi: 10.1177/0269215507082338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hobson DA. Comparative effects of posture on pressure and shear at the body-seat interface. J Rehabil Res Dev. 1992;29(4):21–31. doi: 10.1682/jrrd.1992.10.0021. [DOI] [PubMed] [Google Scholar]
- 5.Sprigle S, Maurer C, Soneblum SE. Load redistribution in variable position wheelchairs in people with spinal cord injury. J Spinal Cord Med. 2010;33(1):58–64. doi: 10.1080/10790268.2010.11689674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jan YK, Liao F, Jones MA, Rice LA, Tisdell T. Effect of durations of wheelchair tilt-in-space and recline on skin perfusion over the ischial tuberosity in people with spinal cord injury. Arch Phys Med Rehabil. 2013;94 doi: 10.1016/j.apmr.2012.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jan YK, Brienza DM, Boninger ML, Brenes G. Comparison of skin perfusion response with alternating and constant pressures in people with spinal cord injury. Spinal Cord. 2011;49(1):136–41. doi: 10.1038/sc.2010.58. [DOI] [PubMed] [Google Scholar]
- 8.Aissaoui R, Lacoste M, Dansereau J. Analysis of sliding and pressure distribution during a repositioning of persons in a simulator chair. IEEE Trans Neural Syst Rehabil Eng. 2001;9(2):215–24. doi: 10.1109/7333.928581. [DOI] [PubMed] [Google Scholar]
- 9.Ding D, Leister E, Cooper RA, Cooper R, Kelleher A, Fitzgerald SG, et al. Usage of tilt-in-space, recline, and elevation seating functions in natural environment of wheelchair users. J Rehabil Res Dev. 2008;45(7):973–83. doi: 10.1682/jrrd.2007.11.0178. [DOI] [PubMed] [Google Scholar]