Abstract
Background
Cervical and endometrial carcinoma incidentally found in the surgical specimen with high risk pathological finding or with gross residual disease.
Material and Methods
Between 2004 and 2010, 320 cervical and endometrial cancer patients were treated with EBRT and brachytherapy after having undergone total/subtotal hysterectomy. Sixty patients were lost to follow-up.
Results
Median follow-up was 21 months. Endometrial and cervical cancer with a high risk for local recurrence achieved CR 93.8 and 89 %, respectively. 56 % patients experienced CR with residual disease with cervical cancer. Median OS for endometrial and cervical cancer with residual disease was 8.5 and 24 months, respectively. Grade 3 adverse events were 5 and 3.5 % for rectum and bladder, respectively.
Conclusion
The incorporation of chemotherapy during pelvic radiotherapy followed by HDR interstitial brachytherapy for residual disease is inadequate and improves survival. We are still in learning phase of brachytherapy in post-operative gynaecological malignancy cases; expertise will be developed by practice.
Keywords: Gynaecological malignancy, Hysterectomy, Brachytherapy, Survival
Introduction
Radiotherapy is an indisputable modality of treatment in the management of gynecological cancers involving those of the cervix, endometrium, vagina, and vulva. Its use in ovarian cancer is debated. Of these, cervix cancer is one of the most common cancers seen among Indian women, and endometrial cancer ranks third in position. Brachytherapy with or without external radiation is a proven modality of treatment in both cancer cervix and cancer endometrium [1]. Following surgery, the vagina followed by the vault is the most common site of loco-regional recurrence in carcinoma endometrium, and hence the importance of irradiation in the form of brachytherapy [2]. In our day to day practice, we often come across patients of cancer cervix who have been operated on without proper staging or cases with advanced stages who have been inadvertently operated and have hence undergone incomplete surgery. Such cases require not only external radiation but also boost to the local site by means of brachytherapy to prevent local recurrence [3].
Brachytherapy is difficult to perform in such settings due to post-operative adhesions preventing bowel immobilization and causing more proximity of the bladder and rectum to the radioactive sources. Image guided delineation of the tumor and the organs at risk (OAR) by (CT scan/preferable MRI) are essential in such cases [4].
Also, delineation of the residual tumor volume (if at all present) is quite difficult as it might disappear after external radiation. Till date, there is no consensus on what thickness or length of the vagina should be irradiated in operated and externally irradiated cases of carcinoma endometrium [2]. Distorted position of the rectum, sigmoid colon, and bladder makes image guided volume delineation imperative in such cases. The dose that can be delivered by brachytherapy depends a lot on the type of applicator used. The vaginal cylinder is most commonly used, but it also has its inherent disadvantages as well. Quite often, the required dose to be delivered by brachytherapy may not be delivered due to the shape of the applicator as well as the proximity and distortion of the organs at risk. Interstitial brachytherapy in such situations enables on to achieve the desired dose delivery as well as dose distribution to the vault and vaginal mucosa [5].
In this retrospective analysis, we have presented our institutional data on the use of HDR brachytherapy in post-operative cases of cancer cervix and endometrium by means of different applicators and attempted to analyze the dose delivered and distributed and their relation to local control and adverse effects.
Aim of the Study
We have performed a retrospective analysis of the post-operative gynecological malignancy cases that had received brachytherapy following external radiation from December 2004 to February 2010 with the aim of assessing
Disease controlled rate.
Late rectal, Urinary bladder, and GI toxicities.
Overall survival.
To formulate our departmental protocol by analyzing the above results.
Patient Characteristics
From December 2004 to February 2010, 179 endometrial cancer and 141 patients with cervical cancer after simple hysterectomy or subtotal hysterectomy with high risk surgico-pathological finding attended the Outpatient department of Radiation Oncology at the Medical College and Hospital and were included in the study. Twenty nine endometrial cancers and 31 cervical cancer patients were excluded from the analysis because of missing pertinent data or received incomplete treatment. The remaining 150 endometrial cancer and 110 patients with cervical cancer were included in this retrospective analysis. The baseline patient characteristics are shown in Table 1. Majority (57.7 %) of the patients had endometrial cancer and >60 % were above 50 years of age. Approximately 85 % of the patients had a good performance status (ECOG 0). The most common histological subtype of endometrial cancer was adenocarcinoma (98 %) and squamous cell for cervical cancer (93.6 %). Thirty patients had residual or recurrent vault disease before the start of external beam radiotherapy. Among them, 25 patients were with endometrial cancer and five patients were with cervical cancer with post-operative residual or recurrent disease at vaginal vault. Only 33 % of patients had adequate surgery, total abdominal hysterectomy with bilateral salpingo oophorectomy, and pelvic lymphadenectomy. Remaining patients were treated with simple and subtotal hysterectomy (44.6 %) or there were missing patient’s detailed operative data (21.9 %). All the patients underwent external radiation to the whole pelvis using Telecobalt machine (Theratron 780 C). Two hundred and forty eight patients had Antero-posterior portals and 12 patients were treated by four field box technique. The dose fraction varied from 1.8–2.0 Gy to a total dose of 45–50 Gy in 5–6 weeks. The median period of external radiation was 25–33 days. Sixty two percentages of the patients with cervical cancer had received concurrent chemotherapy with external beam radiotherapy, which invariably contains cisplatin (40 mg/M2).
Table 1.
Baseline patients’ characteristics that were included for statistical analysis
| Variable | Number of patients | % |
|---|---|---|
| Site | ||
| Endometrial cancer | 150 | |
| No vault residual | 145 | 96.7 |
| Vault residual/recurrence | 5 | 03.3 |
| Cervical cancer | 110 | |
| No vault residual | 85 | 77.3 |
| Vault residual/recurrence | 25 | 22.7 |
| Median age | ||
| Endometrial cancer | 61 | |
| Cervical cancer | 55 | |
| Tumor histopathology | ||
| Endometrial cancer | ||
| Adenocarcinoma | 147 | 98 |
| Squamous cell carcinoma | 2 | 1.3 |
| Clear cell carcinoma | 1 | 0.7 |
| Cervical cancer | ||
| Adenocarcinoma | 6 | 0.5 |
| Squamous cell carcinoma | 103 | 93.6 |
| Small cell carcinoma | 1 | 0.9 |
| Type of surgery | ||
| TAH and BSO and pelvic lymphadenectomy | 87 | 33.5 |
| TAH and BSO and without pelvic lymphadenectomy | 97 | 37.3 |
| Sub total hysterectomy | 19 | 7.3 |
| Missed detail operative data | 57 | 21.9 |
| Type of HDR brachytherapy | ||
| IVBT (Intravaginal brachytherapy) | 230 | 88.5 |
| ISBT (Interstitial brachytherapy) | 30 | 11.5 |
| Missing follow-up data/incomplete treatment | 60 | 18.8 |
All patients received high-dose rate (HDR) brachytherapy boost using Iridium 192 (Gamma Med and planning was done by Brachyvision Varian, Palo Alto, CA) after completion of external radiation. The applicators used were either vaginal cylinder for intravaginal brachytherapy or Martinez universal perineal template with rigid needles and obturator for interstitial brachytherapy. The dose per fraction varied from 5 to 6 Gy for healthy vault with vaginal cylinder and 7–9 Gy for residual or recurrent disease with interstitial implant. The number of fractions varied from 2 to 4. Dose was prescribed at a depth of 5 mm from the vaginal mucosal surface when cylinder was used for vault irradiation. In interstitial implant, prescribed dose was delivered to the maximum volume of disease at vault by volumetric optimization using CT image-based planning system. The organs at risk included the bladder, the sigmoid colon, and the rectum. Cumulative dose volume histogram was utilized to determine the dose to the 0.1, 0.2, 2, and 5 cc and volume of the respective OARs. Median dose to 2 cc volume to the rectum was 3–4 Gy. Median dose to 2 cc volume to the bladder was 5–6 Gy.
Follow-Up
Patients were followed up every 3 months for the 1st year, every 6 months for the 2nd and 3rd year, and then yearly. The visits included complete physical examination to detect loco-regional recurrence, toxicity grading of bladder, rectum, and vagina. Imaging (CT scan/MRI) was performed in suspected recurrence or in symptomatic cases. Toxicities were grading according to LENT SOMA criteria. Recurrence and appearance of metastatic diseases were investigated accordingly.
Response and Toxicity
Results were analyzed on July 2011. The common factor among the study group of heterogeneous population was their post-operative status. Hence, results were different for each group of malignancy. Median follow-up time period was 21 months (range 2–62 months). Most cases of endometrial cancer and cervical cancer with healthy vaginal vault, but high risk for loco-regional recurrence, were on complete remission, 93.8 % (136/145) and 89 % (76/85), respectively. Only one patient presented with isolated vaginal recurrence. Seven patients with endometrial cancer had developed pelvic lymph node metastasis, malignant ascites, or liver metastasis (4.8 %). Three patients (1.3 %) died due to other co-morbid disease. Five patients with cervical cancer with suspected microscopic disease at vaginal vault had developed local site recurrence after nine months, three cases died due to both local and distant failure, and only one patient had distant metastasis only.
There were 14 (56 %) complete responses (CR) noted in the group with residual/recurrent disease at vaginal vault with cervical cancer, but none of the patients were with endometrial cancer. Four out of 25 (16 %) evaluable patients with residual cervical cancer had progressive disease (PD), whereas 80 % (4/5) of residual endometrial cancer had progressive disease even after brachytherapy.
Late rectal (radiation proctitis) and urinary bladder (radiation cystitis) toxicity were the most common adverse events noted. Thirteen patients (5 %) had developed late Grade 3 radiation-induced proctitis. Among them, five endometrial cancers and three cervical cancers with suspected microscopic disease at vaginal vault had developed late Grade 3 radiation proctitis. Grade 2 and Grade 1 radiation-induced proctitis had developed in 6.9 % (18/260) and 58 % (151/260), respectively. Late radiation-induced Bladder toxicity was noted in 27.30 % (71/260) of cases and 3.5 % (9/260) patients had experienced Grade 3 adverse events. Bladder toxicity is more in Ca-Endometrium and Ca-Cervix case with the use of Cylinder but less with use of interstitial brachytherapy. Diarrhea was the most common GI toxicity and was experienced by 24 out all 260 patients (9.5 %), and was easily managed with anti-diarrheal therapy.
Overall Survival
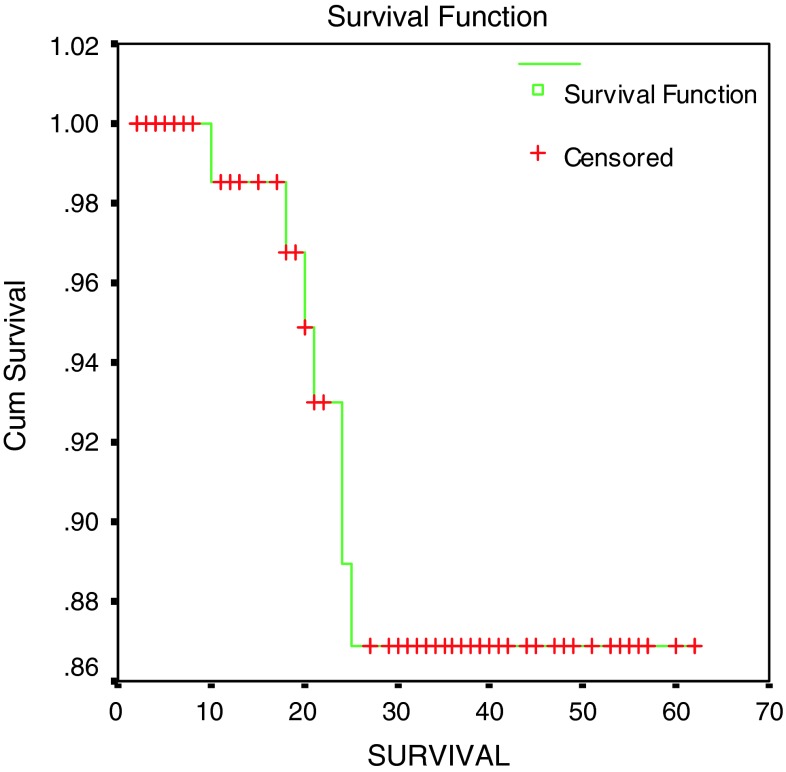
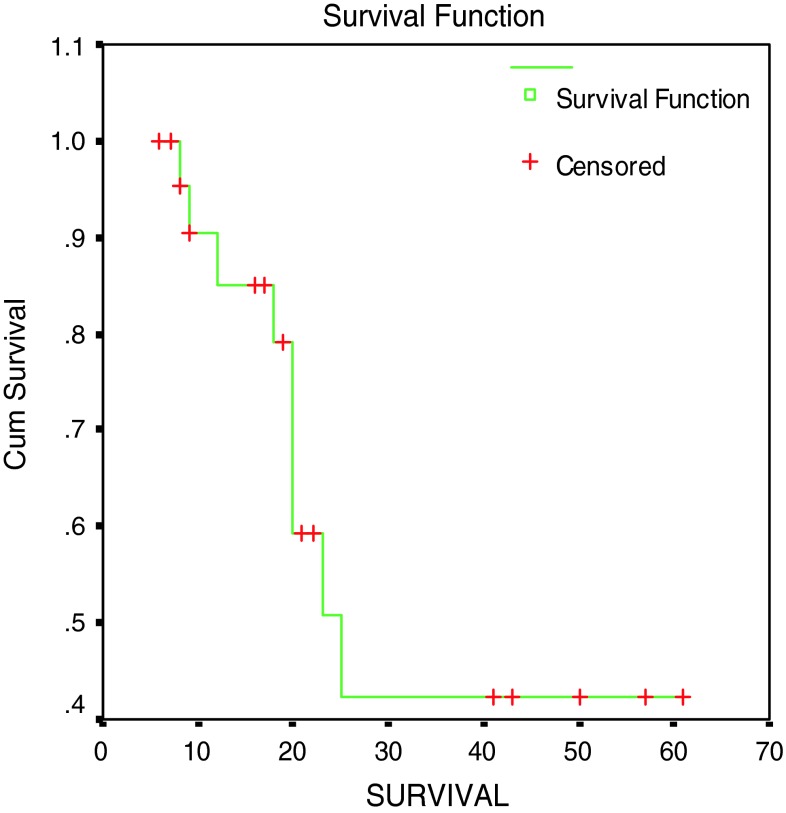
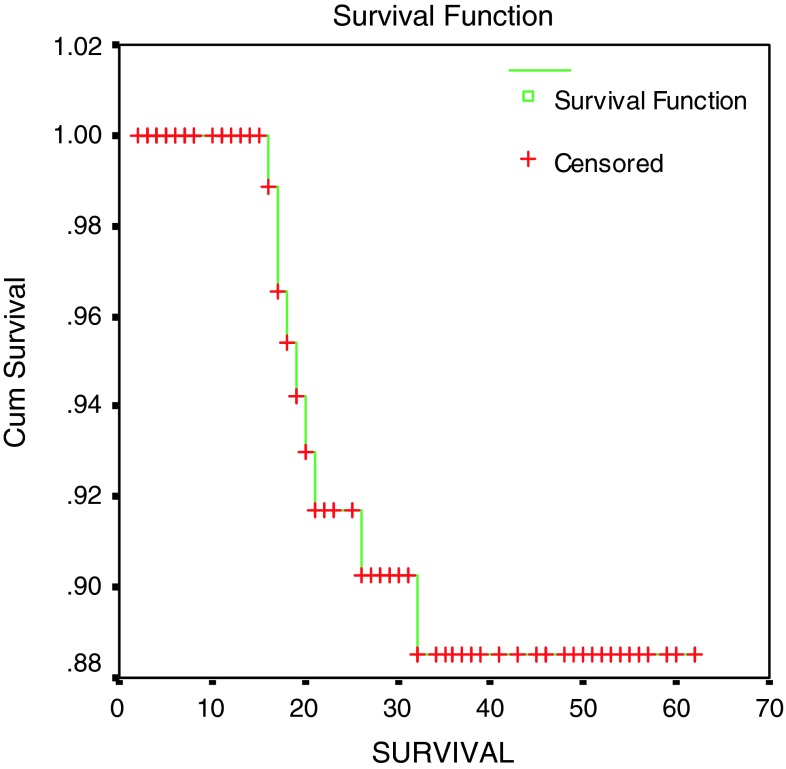
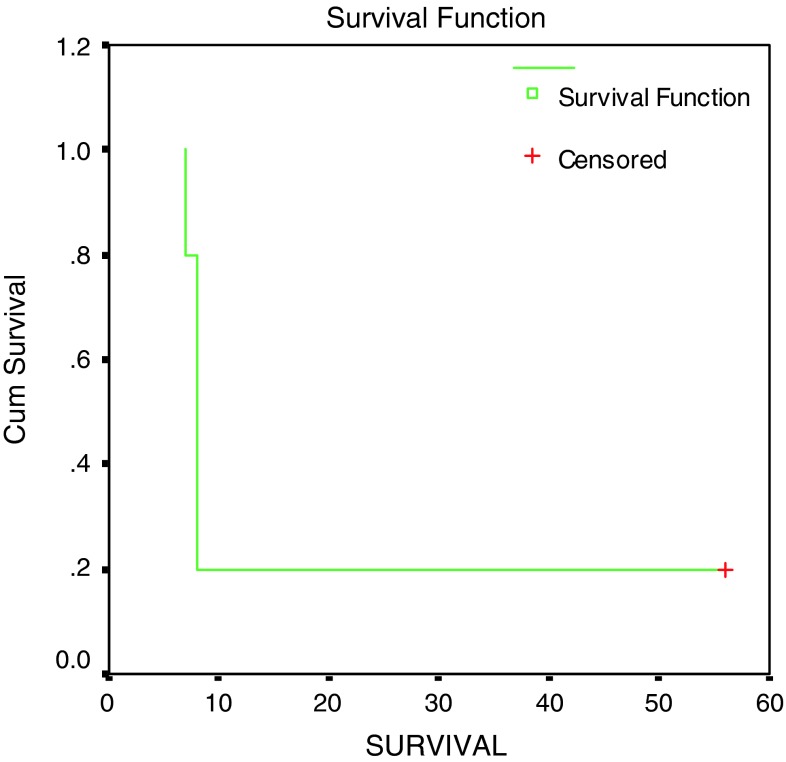
After a maximum follow-up period of 62 months, 35 out of 260 patients eventually had disease progression and died after palliative chemotherapy. Three endometrial cancer patients died due to other co-morbid condition. More than 85 % of cervical cancer and 88 % of endometrial cancer with suspected microscopic disease at vault survived in a median follow-up period of 21 months (range 2–62 months). There was a significantly longer median in overall survival in cervical cancer with residual/recurrent disease than with endometrial cancer residual/recurrent disease. The median overall survival for endometrial cancer with residual disease was 8.5 months as compared to cervical cancer with vault residual/recurrent disease 24 months (Figs. 1, 2, 3, 4).
Fig. 1.
Kaplan–Meier plot of overall survival for patients with cervical cancer with suspected microscopic residual disease at vaginal vault
Fig. 2.
Kaplan–Meier plot of overall survival for patients with cervical cancer with recurrent/residual disease at vault
Fig. 3.
Kaplan–Meier plot of overall survival for patients with endometrial cancer with suspected microscopic disease at vault
Fig. 4.
Kaplan–Meier plot of overall survival for patients with endometrial cancer with gross residual/recurrent disease at vault
Discussion
This retrospective analysis for evaluating the role of adjuvant or salvage radiotherapy of post-operative gynecological malignancy and also evaluating the results of our institutional practice is comparable to other major studies. The most important principles in the management of cancer patient are the overall survival and quality of life. The surgical gynecologic oncologist and radiation oncologist both have agreed that single modality of treatment is preferable than a combination modality of therapeutic intervention regarding patients' quality of life and also survival. However, for patients with invasive carcinoma of the cervix and endometrium, who were incidentally found in the surgical specimen after simple hysterectomy with high risk surgical pathological finding and patients under gone inadvertent surgery with gross residual disease or vault recurrence, it is critical that all received whole pelvic radiotherapy and HDR intravaginal or HDR interstitial using Martinez universal perineal template. Although carcinoma of the uterine cervix is the most common gynecologic malignancy in India, the women have not been well educated about this endemic malignancy nor do they understand the importance of screening. Occasionally, because of inadequate preoperative work-ups, simple hysterectomies are performed and invasive carcinomas of the cervix are found incidentally in the surgical specimens and some times gross residual disease left in the vaginal vault.
In this study, the patients with cervical carcinoma and subclinical disease at vaginal vault, the actuarial survival (AS), were comparable with those of other series [6, 7], and the majority of treatment-related sequelae of rectum and bladder were categorized as LENT SOMA Grade 1–2 minor complications.
Perkins et al. [8] reported good outcomes for 32 patients who received AP/PA whole pelvis irradiation following simple hysterectomy and noted that there were no demonstrable advantages in adding transvaginal brachytherapy. However, vaginal relapse was reported in 50 % (6/12) of their recurrent patients. When compared with our results, showing that some of the recurrent disease was noted in the vaginal stump only, it is risky to completely omit intravaginal brachytherapy.
Ampil et al. [9] described results in 44 patients who received post-operative irradiation after hysterectomy for stage IB or IIA cervical cancer (15 patients were treated with radical hysterectomy). They suggested that the combination of external radiation with additional vaginal cuff irradiation is recommended for patients treated with simple hysterectomy. The results confirm that our current irradiation strategy is acceptable for patients with invasive cervical cancer following inadvertent treatment with a simple hysterectomy.
For patients with advanced pathological findings and gross residual or recurrent disease at vaginal vault, the AS was not satisfactory. Therefore, concurrent chemotherapy with the combination of external beam irradiation and brachytherapy are not adequate to control the disease. However, since the patient number in cervical cancer with residual disease at vault was relatively small, we cannot conclude the actuarial survival of these patients.
For patients with gross residual or recurrent disease, 15 patients (60 %) died of disease and median survival 23 months 48 % (12/25) of these patients developed LENT SOMA Grade 2–3 rectal complications, it is reasonable to reduce the treatment-related morbidity by reducing the irradiation dose or changing the treatment strategy to improve the outcome.
There might be three approaches to optimize the radiation strategy in our retrospective study. The first was to reduce the external radiation dose and volume. In our series, the median external radiation dose to the true pelvis was 50 Gy, which was higher than that used in other series. Therefore, it is advisable to reduce the dosage to reduce the probability of late morbidity.
The second approach was to modify the prescribed dose of HDR intravaginal brachytherapy. Despite the questionable radiobiological disadvantages, high-dose-rate brachytherapy has been widely used in India and Europe, and HDR intravaginal brachytherapy for additional vaginal stump irradiation might narrow the therapeutic window. Since the radiation dose of the anterior rectal wall was estimated to be 4–5 Gy on each insertion, the cumulative dose to the anterior rectal wall would be ~64 Gy. As the rectum is a late-reacting tissue, a α/β of three was used in the calculations. The calculated cumulative rectal biologically equivalent dose (adding the biological effective doses of external radiation and HDR intravaginal brachytherapy together) was 107 Gy3, calculated by the linear-quadratic formula as described in Fowler’s review [10].
In comparison with the other studies, the cutoff value for the development of rectal complications was either the cumulative rectal dose of 70 Gy or the cumulative biologically equivalent dose of 110 Gy3. Therefore, it is imperative to lower the prescribed dose of HDR intravaginal brachytherapy to decrease the risk of rectal complications.
Finally, close surveillance for selected patients might be feasible. Smith et al. [11] reported that 272 patients with early invasive adenocarcinoma of the cervix (FIGO IA1 and IA2) had an excellent prognosis and simple hysterectomy might be appropriate. Schorge et al. [12] suggested that for patients with micro-invasive carcinoma who met the criteria for FIGO stage IA1 cervical cancer and had disease limited to the cervix, simple hysterectomy might offer a definitive treatment.
Endometrial carcinoma is one of the common gynecologic malignancy and the fourth most common cancer in women. Approximately 75 % of patients have uterus-confined [International Federation of Gynecology and Obstetrics (FIGO) Stage I] disease at diagnosis. The current standard treatment for Stage I disease is the surgical removal of the uterus, fallopian tubes, and ovaries followed by with or without adjuvant radiotherapy (RT).
Adjuvant RT is recommended based on the perceived risk of disease recurrence in the pelvic lymph nodes and/or vagina. Surgical-pathologic studies have shown that the risk of pelvic nodal disease increases mainly with increasing depth of myometrial invasion and greater pathologic grade. In Creasman, the pelvic nodal risk ranged from 0 %, for low-grade tumors not invading the myometrium, to 34 %, for high-grade tumors invading more than half of the myometrium.
Gynecologic Oncology Group (GOG)-99 study and Post-Operative Radiation Therapy in Endometrial Carcinoma (PORTEC) study revealed that most pelvic recurrence after radical surgery and pelvic radiotherapy are located in vagina. GOG 99 Published data have shown that pelvic radiotherapy reduced the risk of any recurrence by 58 %. Substitution of whole pelvic radiotherapy with vaginal vault brachytherapy or adding vaginal vault brachytherapy might result in a similar or more reduction in recurrence [2].
The results of our study have confirmed previous findings and added to the body of literature showing the high efficacy and low morbidity of adjuvant pelvic external radiotherapy and HDR intravaginal brachytherapy for endometrial cancer.
The recent Dutch PORTEC trial included an analysis of survival after vaginal relapse of endometrial carcinoma and showed that, after vaginal recurrence, the 5-year survival rate was only 65 % when relapsed patients were treated curatively with RT and/or surgery [13]. GOG-99 found that 5 (38 %) of 13 patients with vaginal recurrence after surgery (in the no-radiation arm) died as a result of their endometrial cancer. However, since the patient number in endometrial cancer with residual or recurrent disease at vault was relatively small, we cannot conclude the actuarial survival of these patients.
On the basis of these results, it seems preferable to treat selected patients initially with adjuvant radiotherapy, given its minimal morbidity and high efficacy, rather than observe and attempt salvage therapy when vaginal recurrence occurs.
In our series and others, the vaginal isolated vaginal recurrence rate adjuvant radiotherapy was <1 % (1), loco-regional and distant recurrence was 3.5 % (5), and only distant recurrence was 1 % (2). Salvage RT (pelvic EBRT with brachytherapy) for residual or recurrent disease is associated with significantly more morbidity than adjuvant radiotherapy, given the need for greater radiation doses and larger treatment volumes of treatment.
The most common side effects of HDR intravaginal brachytherapy (IVBT) were vaginal changes seen on follow-up pelvic examinations (i.e., mucosal telangiectasia, atrophy, stricture, or adhesions). Dyspareunia was occasionally bothersome and may have improved with regular use of a vaginal dilator. About 20 % of patients had temporary vaginal discharge and/or mild bleeding after brachytherapy.
The long-term side effects were urinary bladder, rectal, and other gastro intestinal toxicities. The radiation dose distribution is more localized with HDR brachytherapy conforming to the shape of the vagina. Also, the rectal dose is kept below a threshold to avoid long-term rectal complications. This retrospective study has shown 10.3 % (15) patients developed late Grade 2–3 rectal and 11 % (16) patients developed late Grade 2–3 bladder toxicity which is comparable to other studies.
Multiple single institution studies have shown pelvic and vaginal recurrence rate after adjuvant whole pelvis EBRT and HDRIVBT to be 0–4 % and 0–2 %, respectively, which is comparable to our series. Only one isolated vaginal recurrence has been reported (<1 %) with adjuvant whole pelvis EBRT and HDR IVBT. In addition, only five pelvic (3.5 %) and vaginal and two isolated distant recurrence (1 %) occurred.
A recent survey of radiation oncologists revealed that only 5 % treat the entire vagina with HDR IVBT in the adjuvant setting and 95 % treat either the upper third or half of the vagina. It has been our practice to treat the upper half of vagina. Given the minimal vaginal morbidity seen in our patients treated with HDR brachytherapy without compromising vaginal recurrence, it may be disadvantageous to treat the entire length of vagina because of post-intra vaginal brachytherapy vaginal stenosis and dyspareunia.
Our results may not be directly applicable to the patient with extensive pelvic nodal dissection along with abdominal hysterectomy and bilateral salpingo-oophorectomy. It can be assumed that these patients were at a high risk of developing an extravaginal pelvic recurrence. These patients have not undergone complete surgical staging and have significant risk of pelvic nodal involvement and treated with whole pelvic radiotherapy along with HDR IVBT as in the GOG study.
At our institution, patients with early stage endometrial cancer were inadvertently treated with simple hysterectomy and infrequently undergone complete pelvic and paraaortic lymph node dissection. Assuming that patients with negative nodes after surgery may be at a very low risk of extravaginal pelvic recurrence, vaginal HDR brachytherapy without pelvic EBRT may be an option for properly staged node negative Stage I endometrial carcinoma.
Conclusion
For patients with cervical and endometrial cancer following inadvertent simple hysterectomy, radiotherapy with EBRT combined with one or two fractions of intravaginal brachytherapy could achieve satisfactory disease control. The incorporation of chemotherapy during whole pelvic radiotherapy followed by HDR perineal interstitial brachytherapy for high-risk patients with gross residual disease at vaginal stump are inadequate and improves survival rates.
We are still in the learning phase of brachytherapy in post-operative gynecological malignancy cases; expertise will be developed by practice and acquiring knowledge on dosimetry. Very meticulous implant procedure and critical planning are needed for reducing toxicity and improve survival.
References
- 1.Chen SW, Liang JA, Yang SN. Postoperative radiotherapy for patients with invasive cervical cancer following treatment with simple hysterectomy. Jpn J Clin Oncol. 2003;33(9):477–481. doi: 10.1093/jjco/hyg086. [DOI] [PubMed] [Google Scholar]
- 2.Jolly S, Vargas C, Kumar T. Vaginal brachytherapy alone: an alternative to adjuvant whole pelvis radiation for early stage endometrial cancer. Gynecol Oncol. 2005;97(3):887–892. doi: 10.1016/j.ygyno.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 3.Igboeli P, Kapp DS, Lawrence R. Carcinoma of the cervical stump: comparison of radiation therapy factors, survival and patterns of failure with carcinoma of the intact uterus. Int J Radiat Oncol Biol Phys. 1983;9(2):153–159. doi: 10.1016/0360-3016(83)90092-5. [DOI] [PubMed] [Google Scholar]
- 4.Das RK, Patel R, Shah H. 3D CT-based high-dose-rate breast brachytherapy implants: treatment planning and quality assurance. Int J Radiat Oncol Biol Phys. 2004;59(4):1224. doi: 10.1016/j.ijrobp.2004.03.030. [DOI] [PubMed] [Google Scholar]
- 5.Nandwani PK, Vyas RK, Neema JP. Retrospective analysis of role of interstitial brachytherapy using template (MUPIT) in locally advanced gynecological malignancies. J Cancer Res Ther. 2007;3(2):111–115. doi: 10.4103/0973-1482.34692. [DOI] [PubMed] [Google Scholar]
- 6.Liu MT, Hsu JC, Liu WS. Prognostic factors affecting the outcome of early cervical cancer treated with radical hysterectomy and post-operative adjuvant therapy. Eur J Cancer Care (Engl) 2008;17(2):174–181. doi: 10.1111/j.1365-2354.2007.00831.x. [DOI] [PubMed] [Google Scholar]
- 7.Hart K, Han I, Deppe G. Postoperative radiation for cervical cancer with pathologic risk factors. Int J Radiat Oncol Biol Phys. 1997;37(4):833–838. doi: 10.1016/S0360-3016(96)00560-3. [DOI] [PubMed] [Google Scholar]
- 8.Perkins PL, Chu AM, Jose B. Posthysterectomy megavoltage irradiation in the treatment of cervical carcinoma. Gynecol Oncol. 1984;17(3):340–348. doi: 10.1016/0090-8258(84)90219-1. [DOI] [PubMed] [Google Scholar]
- 9.Ampil F, Datta R, Datta S. Elective postoperative external radiotherapy after hysterectomy in early-stage carcinoma of the cervix. Is additional vaginal cuff irradiation necessary? Cancer. 1987;60(3):280–288. doi: 10.1002/1097-0142(19870801)60:3<280::AID-CNCR2820600303>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 10.Fowler JF. The linear-quadratic formula and progress in fractionated radiotherapy. Br J Radiol. 1989;62(740):679–694. doi: 10.1259/0007-1285-62-740-679. [DOI] [PubMed] [Google Scholar]
- 11.Smith HO, Qualls CR, Romero AA. Is there a difference in survival for IA1 and IA2 adenocarcinoma of the uterine cervix? Gynecol Oncol. 2002;85(2):229–241. doi: 10.1006/gyno.2002.6635. [DOI] [PubMed] [Google Scholar]
- 12.Schorge JO, Lee KR, Flynn CE. Stage IA1 cervical adenocarcinoma: definition and treatment. Obstet Gynecol. 1999;93(2):219–222. doi: 10.1016/S0029-7844(98)00371-8. [DOI] [PubMed] [Google Scholar]
- 13.Scholten AN, van Putten WL, Beerman H. PORTEC Study Group. Postoperative radiotherapy for Stage 1 endometrial carcinoma: long-term outcome of the randomized PORTEC trial with central pathology review. Int J Radiat Oncol Biol Phys. 2005;63(3):834–838. doi: 10.1016/j.ijrobp.2005.03.007. [DOI] [PubMed] [Google Scholar]