Abstract
The choroid plexus is the site of the blood–cerebrospinal fluid (CSF) barrier (BCSFB) and has also been considered as a possible route for peripheral immune signals and cells to transfer to the central nervous system. Infection/inflammation stimulates innate and subsequent adaptive immune responses via Toll-like receptors (TLRs). In this study, we have investigated the mRNA expression of TLRs, cytokines, and tight junction proteins in the choroid plexus in the immature brain after systemic inflammation, as well as accumulation of immune cells into the CSF. Specific ligands for TLR-1/2, TLR-3, and TLR-4 were administered to postnatal day 8 mice and mRNA expression for the targeted genes was examined in the choroid plexus. We found that mRNA for all four TLRs was detected in the choroid plexus under control conditions. Following immune stimulation, expression of all the TLRs was upregulated by their respective ligands, except for TLR-4 mRNA, which was downregulated by Pam3CSK4 (PAM; a TLR-1/2 ligand). In addition, we investigated BCSFB regulation after TLR stimulation and found that TLR-1/2 and TLR-4 activation was associated with changes in mRNA expression of the tight junction protein occludin in the choroid plexus. PAM induced choroid plexus transcription of TNF-α and resulted in the most dramatic increase in numbers of white blood cells in the CSF. The data suggest a possible mechanism whereby systemic inflammation stimulates TLRs in the choroid plexus, which may lead to disturbances in choroid plexus barrier function, as well as infiltration of immune cells through the plexus.
Keywords: LPS, Poly I:C, Pam3CSK4, Neonatal, Brain inflammation, Cerebrospinal fluid, White blood cells
Introduction
The central nervous system (CNS) is protected from the changeable milieu (e.g., ions, solutes, pathogens, and proinflammatory cytokines) of the bloodstream through the blood–brain barrier (BBB) and the blood–cerebrospinal fluid (CSF) barrier (BCSFB) [1, 2]. The BBB and BCSFB act as barrier systems to maintain CNS homeostasis as well as transport systems providing the brain with essential nutrients. The BCSFB consists of a single layer of epithelial cells in the choroid plexus that overlay an extensive network of fenestrated capillaries. Tight junctions between adjacent barrier-forming epithelial cells form a physical barrier, thereby limiting the paracellular movement of compounds [3]. A major function of the choroid plexus is to produce CSF; however, during brain development, it has also been suggested to be a particularly important exchange interface between blood and brain (via CSF) [4]. Furthermore, the choroid plexus has been implicated in the trafficking of systemic circulating immune cells into the brain [5, 6].
Increasing evidence suggests that neonatal brain injury is associated with infection/inflammation, but the underlying mechanisms are not fully understood [7–9]. Infection/inflammation stimulates innate and subsequent adaptive immune responses via the Toll-like receptors (TLRs). We have previously shown that exposure to Pam3CSK4 (PAM) and lipopolysaccharide (LPS), specific ligands for TLR-1/2 and TLR-4, respectively, impair neonatal brain development [10, 11]. Studies have also demonstrated that polyinosinic/polycytidylic acid (Poly I:C), a specific ligand for TLR-3, exacerbates the inflammatory response and accelerates neurodegeneration in the adult brain [12] and increases the susceptibility of midbrain dopaminergic neurons to subsequent neurotoxicity [13]. Furthermore, there is evidence to show that maternal immune challenge with Poly I:C precipitates neurodevelopmental mental diseases later in life [14].
Disturbance of the BBB in association with systemic inflammation is believed to contribute to pathology in the immature brain. Studies have shown that, at the time of myelination, systemic inflammation results in increased BBB permeability to plasma proteins, specifically in white matter tracts, with a reduced amount of myelin as a result [15, 16]. Less is known about the effects of systemic inflammation on the choroid plexus. TLR-2 and TLR-4 mRNA expression has been identified in the adult choroid plexus [17] and systemic LPS exposure induced an acute phase response with upregulation of genes involved in immune-mediated cascades and downregulation of genes involved in the maintenance of barrier function [18]. Proinflammatory cytokines activate epithelial cells of the choroid plexus to increase matrix metalloproteinase secretion [19], and following hind paw inflammation, monocyte chemoattractant protein-1 expression is elevated in the choroid plexus [20]. TLR expression and regulation in the choroid plexus in the immature brain is unknown.
In this study, we hypothesized that TLRs are present in the choroid plexus in the neonatal brain and tested whether they are regulated by systemic immune challenge. As the activation of TLR-2 [21], TLR-3 (Stridh et al., unpublished), and TLR-4 [22, 23] has been shown to contribute to perinatal brain damage, we investigated these particular TLRs. We show that the mRNA for TLR-1, TLR-2, TLR-3, and TLR-4 is expressed in the choroid plexus in the normal neonatal brain and that ligand-specific regulation of expression occurs in the plexus. In addition, particularly the activation of the TLR-1/2 complex leads to an increased transcription of tumor necrosis factor-α (TNF-α) and a decreased expression of the tight junction protein occludin in the choroid plexus, while inducing a dramatic increase in the number of white blood cells in the CSF.
Material and Methods
Animals
C57BL/6J mice were bought from Charles River (Germany). Mice were housed in a 12-h light–dark cycle and bred at Laboratory for Experimental Biomedicine (University of Gothenburg, Gothenburg, Sweden) and were provided with a standard laboratory chow diet (B&K, Solna, Sweden) and drinking water ad libitum. All animal experiments were approved by the Animal Ethics Committee of Gothenburg (No. 374-09).
Administration of TLR Ligands
Postnatal day (PND) 8 mice were injected intraperitoneally (i.p.; 10 μl/g body weight) with PAM (tlrl-pms; 5 mg/kg), a TLR-1/2 ligand; Poly I:C (Poly(I:C)-LMW, InvivoGen; 10 mg/kg), a TLR-3 ligand; LPS (List Biological Laboratories, Inc., ultrapure #423; 0.3 mg/kg), a TLR-4 ligand; or vehicle (LPS free saline, S8776, Sigma-Aldrich, Sweden) and were then deeply anesthetized and sacrificed 14 h postinjection for tissue sampling. TLR agonist doses and time for sacrifice were based on our previous studies showing biological effects at these concentrations and at this particular time point. In particular, we have found that a single injection, 14 h before hypoxia–ischemia, of these ligands at the doses used in the present study, sensitizes the neonatal brain to hypoxic–ischemic damage ([22] and Stridh et al., unpublished).
Choroid Plexus Preparation
Brains were rapidly dissected out and placed in phosphate-buffered saline (PBS). Choroid plexuses from the lateral ventricles were dissected out under a microscope, snap frozen, and stored at −80 °C until analysis. To achieve enough RNA for expression analysis, choroid plexus from two animals were pooled for each sample.
Reverse Transcription-Quantitative Polymerase Chain Reaction (PCR)
Choroid plexus tissues were homogenized and total RNA was extracted using the RNeasy Micro Kit (Qiagen, Sweden) according to the manufacturer’s instructions. RNA was measured in a spectrophotometer at 260 nm absorbance. QuantiTect Reverse Transcription Kit (Qiagen, Sweden) was used to synthesize first strand cDNA according to the manufacturer’s instructions. Each PCR (20 μl) contained 2 μl cDNA, 10 μl Quanti Fast SYBR Green PCR Master Mix (Qiagen, Sweden), 2 μl PCR primer, and 6 μl H2O. The following primers were used: TLR-1 (QT00157430), TLR-2 (QT00129752), TLR-3 (QT00122983), TLR-4 (QT00259042), claudin-1 (QT00159278), occludin (QT00111055), zonula occludens-1 (ZO-1; QT00493899), interleukin-1β (IL-1β; QT01048355), TNF-α (QT00104006), monocyte chemotactic protein-1 (MCP-1; QT00167832), GAPDH (QT01658692), and YWHAZ (QT00105350), all from Qiagen, Sweden.
The amplification protocol comprised an initial 5-min denaturation at 95 °C, followed by 40 cycles of denaturation for 10 s at 95 °C and annealing/extension for 30 s at 60 °C on a LightCycler 480 (Roche, Sweden). Melting curve analysis was performed to ensure that only one PCR product was obtained. For quantification and for estimating amplification efficiency, a standard curve was generated using increasing concentrations of cDNA. The amplification transcripts were quantified with the relative standard curve and normalized against the reference genes GAPDH and YWHAZ.
Immunohistochemistry for Tight Junction Proteins
A separate group of pups were injected with TLR ligands along with saline-injected controls, as described above, and animals were killed 14 h later at PND 9 (n = 2 for each group; from two mixed litters). Pups were killed by an i.p. injection of pentobarbital and immediately transcardially perfused with cold heparinized saline for about 30 s followed by cold Histofix (Histolab, Gothenburg, Sweden) for 5 min using a syringe pump using a flow rate to minimize the risk of damaging cerebral vessels. Brains were dissected out and left in Histofix overnight in the fridge before being dehydrated and embedded in paraffin. Coronal 10-μm sections were cut from the hemisphere and two sections containing the lateral choroid plexus were used from each animal for immunohistochemistry. Paraffin on sections was removed by xylene and sections were rehydrated in decreasing ethanol concentrations. Sections were washed in PBS containing 0.1 % Tween 20, which was also used for all subsequent washes. Antigen presentation was enhanced by proteinase treatment (10 μg/ml; proteinase K, Roche Diagnostics, Germany) for 9 min. Blocking was performed by incubation in 3 % H2O2 in PBS for 10 min and serum-free protein block (Dako, Sweden) for 1 h. Rabbit anti-occludin (1:100; Invitrogen, Cat#71-1500) and anti ZO-1 (1:100, Invitrogen Cat#61-7300) were used as primary antibodies and incubated overnight (4 °C), and sections were subsequently incubated for 2 h with biotinylated secondary antibodies against the appropriate species (1:250; Vector Laboratories, USA) at room temperature. All sections were then incubated with avidin–peroxidase complex (ABC Kit PK-6100; Vector Laboratories, USA) for 1 h and developed with the DAB Kit (SK-4100, Vector Laboratories, USA). Control sections, with omission of primary antibodies, generated near to blank sections. Before coverslipping, sections were counterstained with hematoxylin (2 min).
White Blood Cells
To investigate the recruitment of immune cells into the CSF, we determined the number of white blood cells in the blood and CSF. TLR ligands were administered at PND 8, along with saline injections, as outlined above (n = 5 per group; three mixed litters). At 14 h after injections, blood and CSF were sampled from pups. Blood was collected directly from the heart and CSF sampled from the cisterna magna with a fine glass capillary (typically 3–4 μl collected per mouse). CSF samples with suspected blood contamination were immediately discarded. Samples were mixed with methyl violet and the number of white blood cells per microliter was determined in a Bürker chamber.
Statistics
Gene expression data and cell numbers were analysed with one-way analysis of variance followed by Dunnett’s multiple comparison test. Data are presented as the mean ± standard error of the mean (SEM) and significance was set at p < 0.05. All statistical analyses were performed using GraphPad Prism 5.0 (GraphPad Software).
Results
TLR mRNA Regulation in the Choroid Plexus
Repeated neonatal exposure to TLR-2 agonist reduces myelination [10] and TLR-2 deficiency provides neuroprotection from neonatal hypoxia–ischemia [21]. Further, both TLR-3 (Stridh et al., unpublished) and TLR-4 [22] have been shown to increase the sensitivity of the neonatal brain to hypoxic–ischemic brain damage. Therefore, specific ligands for TLR-1/2, TLR-3, and TLR-4 were administered to PND 8 mice and mRNA expression for the targeted TLRs was examined in the choroid plexus.
Under control conditions, mRNA expression for TLR-1, TLR-2, TLR-3, and TLR-4 was detected in the choroid plexus (Fig. 1). Following stimulation with specific TLR agonists, all TLR mRNAs were regulated. The mRNA expression for TLR-1 was significantly upregulated after treatment with the TLR-1/2 ligand PAM (0.89 ± 0.14, n = 6, p < 0.001) and TLR-4 ligand LPS (0.56 ± 0.17, n = 6, p < 0.05) compared to saline-treated controls (0.08 ± 0.02, n = 6; Fig. 1a). TLR-2 mRNA was upregulated only after TLR-1/2 ligand PAM treatment (0.30 ± 0.05, n = 6 vs. saline 0.10 ± 0.004, n = 6, p < 0.001; Fig. 1b), and both TLR-3 ligand Poly I:C and TLR-4 ligand LPS exposure resulted in the upregulation of TLR-3 (2.01 ± 0.17, n = 6, p < 0.001 and 1.11 ± 0.07, n = 6, p < 0.05, respectively, vs. saline 0.72 ± 0.04, n = 6; Fig. 1c). TLR-4 expression was downregulated by TLR-1/2 ligand PAM exposure (PAM 0.96 ± 0.03, n = 6 vs. saline 1.25 ± 0.11, n = 6, p < 0.05; Fig. 1d).
Fig. 1.
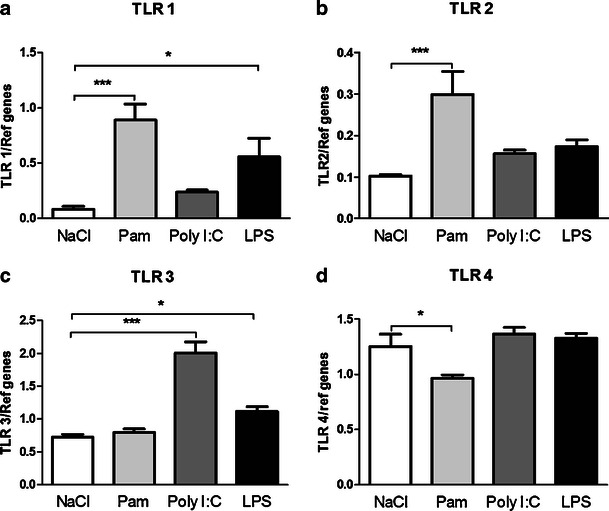
TLR mRNA regulation in the choroid plexus. TLR-specific ligands were administered and mRNA expression of TLR-1, TLR-2, TLR-3, and TLR-4 in the choroid plexus was examined 14 h postinjection. Bar graphs show the mRNA expression for TLR-1 (a), TLR-2 (b), TLR-3 (c), and TLR-4 (d) after different TLR agonist stimulation. Data are normalized against the geometric mean of the reference genes GAPDH and YWHAZ and shown as the mean ± SEM; *p ≤ 0.05, ***p ≤ 0.001, n = 6/group
Immune Response in the Choroid Plexus Following TLR Stimulation
To investigate the immune response in the choroid plexus after TLR stimulation, the gene expressions for the cytokines IL-1β and TNF-α and the chemokine MCP-1 were analyzed after administration with different TLR ligands. TNF-α gene expression was increased after PAM administration (1.67 ± 0.25, n = 6, p < 0.001 vs. saline 0.10 ± 0.05, n = 6; Fig. 2b). No differences were observed in IL-1β or MCP-1 expression after administration of the different TLR ligands (Fig. 2a, c).
Fig. 2.
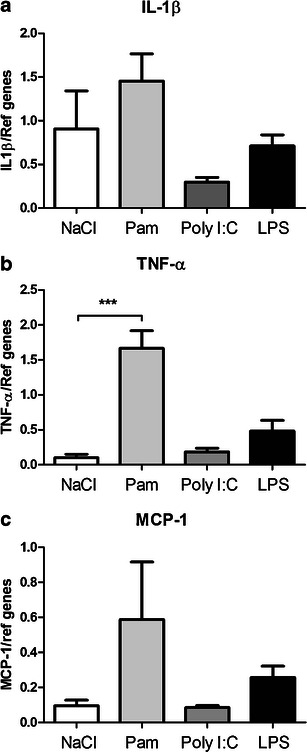
Regulation of the immune response in the choroid plexus following TLR stimulation. TLR-specific ligands were administered and mRNA expression of the cytokines IL-1β and TNF-α and the chemokine MCP-1 in the choroid plexus was examined 14 h postinjection. The expression of TNF-α was upregulated after PAM (b). No changes were found in IL-1β or MCP-1 expression after the administration of the different ligands (a, c). Data are normalized against the geometric mean of the reference genes GAPDH and YWHAZ and shown as the mean ± SEM; ***p ≤ 0.001, n = 6/group
Regulation of Barrier Proteins Following TLR Stimulation
To investigate barrier regulation in the immature brain after TLR stimulation, the gene expression for the tight junction proteins occludin, ZO-1, and claudin-1 were analyzed after administration with different TLR ligands. Occludin gene expression was decreased by TLR-1/2 ligand PAM and TLR-4 ligand LPS (1.63 ± 0.07, n = 6, p < 0.001 and 1.80 ± 0.08, n = 6, p < 0.05, respectively, vs. saline 2.07 ± 0.06, n = 6; Fig. 3b). No differences were observed in ZO-1 or claudin-1 expression after the administration of the different TLR ligands (Fig. 3a, c).
Fig. 3.
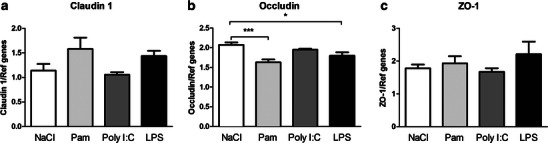
Regulation of barrier proteins in the choroid plexus following TLR stimulation. TLR-specific ligands were administered and mRNA expression of several barrier proteins in the choroid plexus was examined 14 h postinjection. The expression of occludin was downregulated after PAM and LPS exposure (b). No changes were found in ZO-1 or claudin-1 expression after the administration of the different ligands (a, c). Data are normalized against the geometric mean of the reference genes GAPDH and YWHAZ and shown as the mean ± SEM; *p ≤ 0.05, ***p ≤ 0.001, n = 5–6/group
Immunohistochemical Expression of Tight Junction Proteins
Immunoreactivity against one tight junction transmembrane protein (occludin) and one anchoring protein (ZO-1) was examined in sections from TLR ligand-treated and saline-treated animals. In brains, these proteins were only associated to brain barrier-forming cells (cerebral vessels and choroidal epithelial cells) and no immunoreactivity was visible in brain parenchyma. In the choroid plexus, the staining pattern for both proteins was very similar with positive staining towards the CSF side (apical) of epithelial cells when cells were sectioned so both apical and basolateral membranes were visible (Fig. 4). In other cross-sections of epithelial cells, positive staining girthed the whole cells. There was no obvious difference in staining pattern of either occludin or ZO-1 in any of the TLR ligand-treated animals from saline-injected animals (only PAM-injected and saline-injected animals illustrated).
Fig. 4.
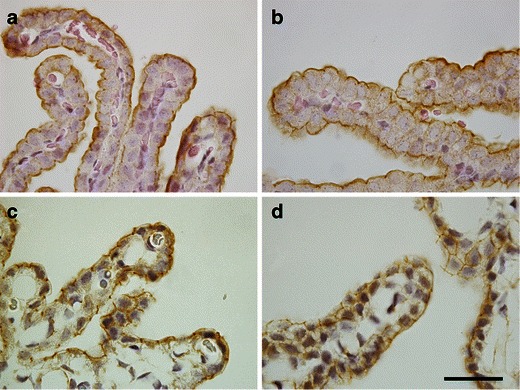
Tight junction proteins in the choroid plexus following PAM stimulation. Immunoreactivity for the tight junction proteins occludin and ZO-1 in saline-exposed and PAM-exposed animals. Occludin and ZO-1 are present towards the apical side of the epithelial cells of control animals (a, c, respectively) and this staining pattern does not appear to change after PAM treatment (b, c, respectively). Scale bar is 25 μm
White Blood Cells in Blood/CSF
The number of white blood cells in the blood and CSF after TLR stimulation is presented in Fig. 5. There was increased number of cells in the blood after TLR-1/2 stimulation (PAM, 2,347 ± 205 cells/μl) compared with saline-injected pups (saline, 1,458 ± 177 cells/μl; p < 0.05). The number of cells was 1,864 ± 135 cells/μl after LPS injections and 1,400 ± 377 cells/μl after Poly I:C, which was not significantly different from saline-treated animals (p > 0.05). In the CSF, the number of cells was close to zero in saline-injected control animals (8 ± 2 cells/μl). The number of cells was increased to 51 ± 13 cells/μl in LPS-treated animals (p < 0.05) to 52 ± 8 in Poly I:C-injected animals (p < 0.05) and to 2,525 ± 575 cells/μl after PAM exposure (p < 0.001).
Fig. 5.
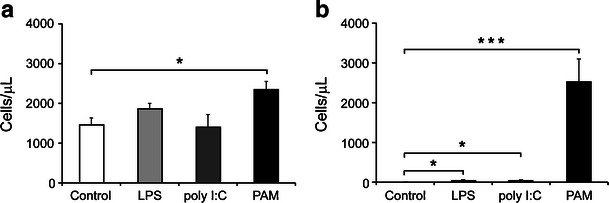
White blood cells after TLR stimulation. The number of white blood cells was counted in the blood (a) and CSF (b) 14 h after the administration of TLR ligands at PND 8. In the blood, there was a significant increase in cell numbers only after TLR-1/2 stimulation (PAM) with around a 60 % increase compared to saline-injected controls. In the CSF, all ligand treatments resulted in significantly increased numbers of cells with around 50 cells/μl after LPS and Poly I:C treatments and 2,500 cells/μl after PAM treatment compared to 8 cells/μl in controls. Data are shown as mean ± SEM; *p ≤ 0.05, ***p ≤ 0.001, n = 5/group
Discussion
In the present study, we demonstrate the presence of TLR-1, TLR-2, TLR-3, and TLR-4 mRNA in the choroid plexus in the normal neonatal brain and that the mRNA expression is regulated after systemic inflammatory stimuli. Furthermore, activation of the TLR-1/2 complex or TLR-4 leads to decreased mRNA expression of the tight junction protein occludin in the choroid plexus. The most striking immune responses were seen following the activation of the TLR-1/2 complex, which resulted in an increased transcription of TNF-α and a dramatic increase in the number of white blood cells in the CSF.
For most of the TLRs, we found ligand-specific upregulation of gene transcription after stimuli with their respective ligands. These findings correspond well with previous studies of the BBB, which have demonstrated increased expression of TLR-2 and TLR-3 on endothelial cells after stimuli with TLR-1/2 ligand PAM and TLR-3 ligand Poly I:C [24, 25]. In the adult brain, TLR-4 mRNA is highly expressed, particularly in the choroid plexus [26]. Our results confirm the presence of TLR-4 mRNA expression in these CNS structures. However, TLR-4 mRNA expression did not change after TLR-4 ligand LPS administration. Similarly, we have previously noted a lack of TLR-4 gene expression regulation in the CNS in response to systemic LPS in neonatal rats [23]. Although TLR-4 mRNA was not regulated after LPS exposure, TLR-4 mRNA was reduced in the choroid plexus following TLR-1/2 ligand PAM administration in the present study. These results suggest that there may be interactions between the TLR-2 and TLR-4 receptors, which may be similar to what have been previously reported in the adult brain [27]. We also found an upregulation of TLR-1 and TLR-3 mRNA transcription after LPS exposure. To our knowledge, there are no previous studies showing this pattern of mRNA expression in the choroid plexus. However, TLR-3 mRNA has been found to be upregulated after LPS exposure in human peripheral blood monocytes, which appears to be dependent on a TLR-4–MyD88–NF-κB signaling pathway [28]. Also, LPS derived from Helicobacter pylori or Porphyromonas gingivalis has been shown to require the formation of heterotypic receptor complexes comprising both TLR-1 and TLR-2 [29, 30]. Further investigation is needed to determine whether such complex TLR regulation also occurs in the choroid plexus.
In order to test whether stimulation of TLRs leads to changes in BCSFB properties, we also investigated the gene expression of several tight junction proteins. In epithelial cells of the choroid plexus, there was a significant downregulation of occludin both after PAM and LPS exposure. The tight junctions are made up of a range of proteins where occludin and claudins are transmembrane components and ZO-1 is one of the principal anchoring proteins of occludin inside the cell membrane. The claudins differ somewhat between tight junctions throughout the body and claudin-1 is found together with claudin-2 and claudin-11 in the epithelial cells of the choroid plexus [31]. At this time, we still have an unclear picture of the exact molecular function of these different tight junction proteins and how they interact. However, studies of claudin-5 knockout animals have shown that it can have a direct effect on BBB permeability [32]. There are also many studies showing that changes to barrier permeability are often associated with alterations of both occludin and ZO-1 [33–35]. The expected pivotal role of occludin in tight junction function, the first tight junction transmembrane protein to be discovered, was somewhat lessened when it was discovered that occludin-deficient mice still could assemble normal tight junctions [36]. However, later studies have shown that it appears that tight junction function can be modulated by phosphorylation of Tyr/Ser/Thr residues on occludin [37] and also that occludin-deficient mice have altered epithelial secretion function [38].
The reduced gene expression of occludin was not reflected by any apparent changes in immunoreactivity for occludin and ZO-1 proteins. It has previously been shown that, despite no structural changes in the BCSFB following immune challenge in vitro, the efficiency of the choroidal epithelium to clear the CSF from deleterious compounds was reduced [19]. We have recently demonstrated that systemic LPS exposure downregulates the inducible antioxidant system in the choroid plexus in the immature brain, even though choroid epithelial cells are not structurally damaged [39]. It remains to be determined whether the changed occludin mRNA expression in the present study affects choroid plexus function.
The investigation into the inflammatory response in the choroid plexus showed specific regulation of TNF-α following administration with the TLR-1/2 ligand PAM. To the best of our knowledge, this is the first study to examine the cytokine response in the choroid plexus following stimulation of the TLR-1/2 complex. Others have previously shown, by in situ hybridization, that IL-1β and TNF-α mRNA expression is increased in the choroid plexus and circumventricular organs following peripheral LPS injection in adult rats [40, 41]. These results differ from ours where we found no significant change in any of the cytokines or chemokine studied after either Poly I:C or LPS. The diverse results between the studies may be due to measurements that were made at different time points or that the developmental stage of the brain affects the cytokine profile.
In support of our findings that peripheral injection with the TLR-1/2 agonist PAM resulted in the most pronounced upregulation of TNF-α and downregulation of the tight junction protein occludin in the choroid plexus, we further demonstrated a dramatic increase in white blood cells in the CSF following PAM injection. These results suggest that systemically circulating ligands for the TLR-1/2 complex may have strong proinflammatory effects on the immature BCSFB. Thus, the BCSFB may provide an immunomodulatory target with the potential to reduce leukocyte accumulation, which has been shown to be beneficial in experimental models of meningitis [42].
In summary, this study shows for the first time that several TLRs are expressed in the choroid plexus in the immature brain, both under physiological conditions and after inflammatory stimuli. Activation by specific TLR ligands resulted in differential upregulation of most of their respective receptors at the BCSFB. In particular, systemic inflammation induced by TLR-1/2 activation stimulated an inflammatory response in the neonatal choroid plexus, downregulated tight junction protein gene transcription, and increased the number of inflammatory cells in the CSF. Such alterations in the choroid plexus and CSF may mediate mechanisms to reduce barrier function that could put the CNS at risk of injury.
Acknowledgments
This research received financial assistance from the Swedish Medical Research Council (VR 2009-2630), a government grant to a researcher in Public Health Service at the Sahlgrenska University Hospital (ALFGBG-142881), European Union grant FP7 (Neurobid, HEALTH-F2-2009-241778), the Leducq Foundation (DSRR_P34404), Åhlén-stiftelsen, and Wilhelm and Martina Lundgren Foundation.
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Linnea Stridh and C. Joakim Ek contributed equally to this work.
References
- 1.Wolburg H, Paulus W. Choroid plexus: biology and pathology. Acta Neuropathol. 2010;119(1):75–88. doi: 10.1007/s00401-009-0627-8. [DOI] [PubMed] [Google Scholar]
- 2.Saunders NR, et al. Barriers in the brain: a renaissance? Trends Neurosci. 2008;31(6):279–286. doi: 10.1016/j.tins.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Coisne C, Engelhardt B. Tight junctions in brain barriers during central nervous system inflammation. Antioxid Redox Signal. 2011;15(5):1285–1303. doi: 10.1089/ars.2011.3929. [DOI] [PubMed] [Google Scholar]
- 4.Saunders NR, Liddelow SA, Dziegielewska KM. Barrier mechanisms in the developing brain. Front Pharmacol. 2012;3:46. doi: 10.3389/fphar.2012.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Engelhardt B, Ransohoff RM. Capture, crawl, cross: the T cell code to breach the blood–brain barriers. Trends Immunol. 2012;33(12):579–589. doi: 10.1016/j.it.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Kivisakk P, et al. Human cerebrospinal fluid central memory CD4+ T cells: evidence for trafficking through choroid plexus and meninges via P-selectin. Proc Natl Acad Sci U S A. 2003;100(14):8389–8394. doi: 10.1073/pnas.1433000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dammann O, Leviton A. Maternal intrauterine infection, cytokines, and brain damage in the preterm newborn. Pediatr Res. 1997;42(1):1–8. doi: 10.1203/00006450-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Wolfberg AJ, Dammann O, Gressens P. Anti-inflammatory and immunomodulatory strategies to protect the perinatal brain. Semin Fetal Neonatal Med. 2007;12(4):296–302. doi: 10.1016/j.siny.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 9.Volpe JJ. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 2009;8(1):110–124. doi: 10.1016/S1474-4422(08)70294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Du X, et al. Systemic stimulation of TLR2 impairs neonatal mouse brain development. PLoS One. 2011;6(5):e19583. doi: 10.1371/journal.pone.0019583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang X, et al. White matter damage after chronic subclinical inflammation in newborn mice. J Child Neurol. 2009;24(9):1171–1178. doi: 10.1177/0883073809338068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Field R, et al. Systemic challenge with the TLR3 agonist poly I:C induces amplified IFN[alpha]/[beta] and IL-1[beta] responses in the diseased brain and exacerbates chronic neurodegeneration. Brain Behav Immun. 2010;24(6):996–1007. doi: 10.1016/j.bbi.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deleidi M, et al. The Toll-like receptor-3 agonist polyinosinic:polycytidylic acid triggers nigrostriatal dopaminergic degeneration. J Neurosci. 2010;30(48):16091–16101. doi: 10.1523/JNEUROSCI.2400-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer U, et al. Immunological stress at the maternal–foetal interface: a link between neurodevelopment and adult psychopathology. Brain Behav Immun. 2006;20(4):378–388. doi: 10.1016/j.bbi.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Stolp HB, et al. Breakdown of the blood–brain barrier to proteins in white matter of the developing brain following systemic inflammation. Cell Tissue Res. 2005;320(3):369–378. doi: 10.1007/s00441-005-1088-6. [DOI] [PubMed] [Google Scholar]
- 16.Stolp HB, et al. Long-term changes in blood–brain barrier permeability and white matter following prolonged systemic inflammation in early development in the rat. Eur J Neurosci. 2005;22(11):2805–2816. doi: 10.1111/j.1460-9568.2005.04483.x. [DOI] [PubMed] [Google Scholar]
- 17.Laflamme N, Rivest S. Toll-like receptor 4: the missing link of the cerebral innate immune response triggered by circulating gram-negative bacterial cell wall components. FASEB J. 2001;15(1):155–163. doi: 10.1096/fj.00-0339com. [DOI] [PubMed] [Google Scholar]
- 18.Marques F, et al. Kinetic profile of the transcriptome changes induced in the choroid plexus by peripheral inflammation. J Cereb Blood Flow Metab. 2009;29(5):921–932. doi: 10.1038/jcbfm.2009.15. [DOI] [PubMed] [Google Scholar]
- 19.Strazielle N, et al. Pro-inflammatory cytokines modulate matrix metalloproteinase secretion and organic anion transport at the blood–cerebrospinal fluid barrier. J Neuropathol Exp Neurol. 2003;62(12):1254–1264. doi: 10.1093/jnen/62.12.1254. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell K, et al. Monocyte chemoattractant protein-1 in the choroid plexus: a potential link between vascular pro-inflammatory mediators and the CNS during peripheral tissue inflammation. Neuroscience. 2009;158(2):885–895. doi: 10.1016/j.neuroscience.2008.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stridh L, et al. Regulation of Toll-like receptor 1 and -2 in neonatal mouse brain after hypoxia–ischemia. J Neuroinflammation. 2011;8(1):45. doi: 10.1186/1742-2094-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang X, et al. Lipopolysaccharide sensitizes neonatal hypoxic–ischemic brain injury in a MyD88-dependent manner. J Immunol. 2009;183(11):7471–7477. doi: 10.4049/jimmunol.0900762. [DOI] [PubMed] [Google Scholar]
- 23.Eklind S, et al. Bacterial endotoxin sensitizes the immature brain to hypoxic–ischaemic injury. Eur J Neurosci. 2001;13(6):1101–1106. doi: 10.1046/j.0953-816x.2001.01474.x. [DOI] [PubMed] [Google Scholar]
- 24.Shin HS, et al. Bacterial lipoprotein TLR2 agonists broadly modulate endothelial function and coagulation pathways in vitro and in vivo. J Immunol. 2011;186(2):1119–1130. doi: 10.4049/jimmunol.1001647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zimmer S, et al. Activation of endothelial toll-like receptor 3 impairs endothelial function. Circ Res. 2011;108(11):1358–1366. doi: 10.1161/CIRCRESAHA.111.243246. [DOI] [PubMed] [Google Scholar]
- 26.Chakravarty S, Herkenham M. Toll-like receptor 4 on nonhematopoietic cells sustains CNS inflammation during endotoxemia, independent of systemic cytokines. J Neurosci. 2005;25(7):1788–1796. doi: 10.1523/JNEUROSCI.4268-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laflamme N, et al. Cooperation between Toll-like receptor 2 and 4 in the brain of mice challenged with cell wall components derived from gram-negative and gram-positive bacteria. Eur J Immunol. 2003;33(4):1127–1138. doi: 10.1002/eji.200323821. [DOI] [PubMed] [Google Scholar]
- 28.Pan ZK, et al. Bacterial LPS up-regulated TLR3 expression is critical for antiviral response in human monocytes: evidence for negative regulation by CYLD. Int Immunol. 2011;23(6):357–364. doi: 10.1093/intimm/dxr019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Triantafilou M, et al. Lipopolysaccharides from atherosclerosis-associated bacteria antagonize TLR4, induce formation of TLR2/1/CD36 complexes in lipid rafts and trigger TLR2-induced inflammatory responses in human vascular endothelial cells. Cell Microbiol. 2007;9(8):2030–2039. doi: 10.1111/j.1462-5822.2007.00935.x. [DOI] [PubMed] [Google Scholar]
- 30.Yokota S, et al. Highly-purified Helicobacter pylori LPS preparations induce weak inflammatory reactions and utilize Toll-like receptor 2 complex but not Toll-like receptor 4 complex. FEMS Immunol Med Microbiol. 2007;51(1):140–148. doi: 10.1111/j.1574-695X.2007.00288.x. [DOI] [PubMed] [Google Scholar]
- 31.Wolburg H, et al. Claudin-1, claudin-2 and claudin-11 are present in tight junctions of choroid plexus epithelium of the mouse. Neurosci Lett. 2001;307(2):77–80. doi: 10.1016/S0304-3940(01)01927-9. [DOI] [PubMed] [Google Scholar]
- 32.Nitta T, et al. Size-selective loosening of the blood–brain barrier in claudin-5-deficient mice. J Cell Biol. 2003;161(3):653–660. doi: 10.1083/jcb.200302070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bauer AT, et al. Matrix metalloproteinase-9 mediates hypoxia-induced vascular leakage in the brain via tight junction rearrangement. J Cereb Blood Flow Metab. 2010;30(4):837–848. doi: 10.1038/jcbfm.2009.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brooks TA, et al. Chronic inflammatory pain leads to increased blood–brain barrier permeability and tight junction protein alterations. Am J Physiol Heart Circ Physiol. 2005;289(2):H738–H743. doi: 10.1152/ajpheart.01288.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reuss B, Dono R, Unsicker K. Functions of fibroblast growth factor (FGF)-2 and FGF-5 in astroglial differentiation and blood–brain barrier permeability: evidence from mouse mutants. J Neurosci. 2003;23(16):6404–6412. doi: 10.1523/JNEUROSCI.23-16-06404.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saitou M, et al. Occludin-deficient embryonic stem cells can differentiate into polarized epithelial cells bearing tight junctions. J Cell Biol. 1998;141(2):397–408. doi: 10.1083/jcb.141.2.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rao R. Occludin phosphorylation in regulation of epithelial tight junctions. Ann N Y Acad Sci. 2009;1165:62–68. doi: 10.1111/j.1749-6632.2009.04054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schulzke JD, et al. Epithelial transport and barrier function in occludin-deficient mice. Biochim Biophys Acta. 2005;1669(1):34–42. doi: 10.1016/j.bbamem.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 39.D’Angelo B, Ek CJ, Sandberg M, et al., Expression of the Nrf2-system at the blood–CSF barrier is modulated by neonatal inflammation and hypoxia–ischemia. J Inherit Metab Dis. 2012. doi:10.1007/10545-012-9551-5. [DOI] [PMC free article] [PubMed]
- 40.Nadeau S, Rivest S. Regulation of the gene encoding tumor necrosis factor alpha (TNF-alpha) in the rat brain and pituitary in response in different models of systemic immune challenge. J Neuropathol Exp Neurol. 1999;58(1):61–77. doi: 10.1097/00005072-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 41.Quan N, et al. Induction of pro-inflammatory cytokine mRNAs in the brain after peripheral injection of subseptic doses of lipopolysaccharide in the rat. J Neuroimmunol. 1999;93(1–2):72–80. doi: 10.1016/S0165-5728(98)00193-3. [DOI] [PubMed] [Google Scholar]
- 42.Tuomanen EI, et al. Reduction of inflammation, tissue damage, and mortality in bacterial meningitis in rabbits treated with monoclonal antibodies against adhesion-promoting receptors of leukocytes. J Exp Med. 1989;170(3):959–969. doi: 10.1084/jem.170.3.959. [DOI] [PMC free article] [PubMed] [Google Scholar]


