Abstract
Objective
To test the relationship between older Americans Act (OAA) program expenditures and the prevalence of low-care residents in nursing homes (NHs).
Data Sources and Collection
Two secondary data sources: State Program Reports (state expenditure data) and NH facility-level data downloaded from http://LTCfocUS.org for 16,030 US NHs (2000–2009).
Study Design
Using a two-way fixed effects model, we examined the relationship between state spending on OAA services and the percentage of low-care residents in NHs, controlling for facility characteristics, market characteristics, and secular trends.
Principal Findings
Results indicate that increased spending on home-delivered meals was associated with fewer residents in NHs with low-care needs.
Conclusions
States that have invested in their community-based service networks, particularly home-delivered meal programs, have proportionally fewer low-care NH residents.
Many states are in the throes of transforming their financing and delivery of long-term services and supports (LTSS). Many of these efforts are aimed at increasing Medicaid funding on home and community-based services (HCBS) in an effort to delay or avoid nursing home (NH) placement, and maintaining current non-Medicaid LTSS funding for the near-poor older adults. While much effort has been geared toward evaluating the cost-effectiveness and role of Medicaid funded HCBS in preventing or postponing NH placement, little research has evaluated the value of other state funded non-Medicaid LTSS, such as The Older Americans Act (OAA) programs.
The Older Americans Act of 1965 (Pub. L. 89-73, 79 Stat. 218, July 14, 1965) was among the first federal initiatives aimed at providing comprehensive services to help older adults stay as independent as possible in their homes and communities. The major program under the OAA, Title III Grants for State and Community Programs on Aging, provides funding to State Units on Aging (SUA) and local Area Agencies on Aging (AAA) for services that include in-home assistance, home-delivered and congregate meals, respite for family caregivers, preventive health services, and legal services for older adults and their caregivers. While funding from the OAA is small compared with the major source of long-term care (LTC) funding from Medicaid, it provides a safety net for people who might otherwise not qualify for Medicaid financed LTC support. A recent national survey of OAA program participants found that more than 85 percent of those receiving homemaker services, case management, transportation, and home-delivered meals report that these programs helped them remain at home (Altshuler and Schimmel 2010). HCBS can be viewed as a substitute for institutionalization for individuals who do not require skilled 24-hour care. Without these programs, it may be that more individuals would be in NHs with low-care needs.
Previous studies have suggested that anywhere from 5 to 30 percent of NH residents have low-care needs and could perhaps be better served in the community (Ikegami, Morris, and Fries 1997; Castle 2002; Mor et al. 2007; Arling et al. 2010; Hahn et al. 2011). States vary greatly in their prevalence of low-care NH residents (Mor et al. 2007). The rates of low-care residents in NHs has been found to be related to variation in Medicaid expenditures on home and community-based services (HCBS) and availability of community alternatives (Castle 2002; Hahn et al. 2011).
Because it is believed that the availability of supportive services in the community allows older adults to remain at home and transition from the NH back to the community, we hypothesize that states that invest more money in their OAA programs will have fewer residents in NHs with low-care needs. We took into consideration other factors that have been shown to be related to a NH's proclivity to provide services to residents with low-care needs, such as the facility's occupancy rate and characteristics of NH's resident population. With regard to market characteristics, we believed that competition may influence low-care resident rates in NHs and therefore we included measures of home care capacity and supply of NH beds. In addition, we believed that states with greater investments in their Medicaid HCBS programs would have an increased awareness and ability to sustain low-care NH residents in the community. Furthermore, NHs in states with more generous Medicaid payment rates may have an incentive to have residents with low-care needs to decrease their expenditures on care while receiving a similar payment rate.
Method
Data
The OAA requires annual performance reporting by SUAs through the State Program Report (SPR). The SPR provides information on the characteristics of clients, the types and levels of service, expenditures of funds from the OAA and other sources, and administrative information about SUAs and local AAAs. These data were downloaded for years 2000–2009 from the Administration on Aging's Aging Integrated Database (AGID) from http://classic.agidnet.org/agid_help/database_helps.asp.
We merged these data with an internal file of the http://LTCfocUS.org, a product of the Shaping Long-Term Care in America Project being conducted at the Brown University Center for Gerontology and Healthcare Research and supported, in part, by the National Institute on Aging (http://www.ltcfocus.org). This dataset includes information for years 2000–2009 and combines variables from the Online Survey Certification and Reporting (OSCAR) data (administrative data collected by state survey agencies during nursing facility annual certification inspections); the Minimum Data Set (MDS) (resident-level data related to resident clinical and functional status); the Area Resource File (ARF) (a national county-level health resources database maintained by the Health Resources and Services Administration that contains data about the health professionals and facilities in each county); and the Residential History File, a data resource developed at the Brown University Center for Gerontology and Healthcare Research built using Medicare Enrollment data, Medicare claims data, and MDS data to track individuals as they move through the long-term care system (Intrator et al. 2011).
Sample
The sample includes a total of 145,649 facility-year observations from 16,030 free-standing certified NHs in the continental United States. Facilities that were hospital-based were excluded from the analyses because they are very different in terms of resident severity, structure, and care practice (Stearns et al. 2006). The facility had to be operating at least one full year for inclusion in the study.
Outcome Variable
Consistent with previous research (Buttar, Blaum, and Fries 2001; Mor et al. 2007; Hahn et al. 2011), estimates of the percentage of low-care residents were identified using RUG-III and activities of daily living (ADLs) classifications. Specifically, individuals were identified as low-care if they required no physical assistance in any of the four late-loss ADLs (bed mobility, toileting, transferring, and eating) and if they were not classified in the two lowest functioning RUG-III classifications (“special rehab” or “clinically complex”). Data were then aggregated to the facility level to derive prevalence estimates of low-care residents in each facility on the first Thursday in April of each year.
Main Independent Variables
The main independent variables were state-specific OAA registered service expenditures (Personal Care, Homemaker, Chore, Home-Delivered Meals, Adult Day Care/Health, Case Management) for each year, 2000–2009. All payment rates were adjusted to 2009 dollars using the annual Consumer Price Index, and rates were adjusted for the number of older adults aged 65+ in the state.
Control Variables
Several facility-level, annualized time-varying covariates were included based on their relationship with low-care status or the provision of care in NHs found in other studies: proportion of days paid for under the Medicare skilled nursing (SNF) benefit; proportion of Medicaid residents; occupancy rate; and percent of admissions paid for under an HMO. At the market level, defined by county boundaries, we controlled for home care capacity using the number of home health agencies per 1,000 people aged 65+ in the county (Hahn et al. 2011) and supply using the total number of NH beds in the county (Hahn et al. 2011). At the state level, we controlled for the percent of Medicaid spending on HCBS as it is a proxy for states' orientation toward HCBS (Mor et al. 2007; Muramatsu et al. 2007, 2008; Houser, Fox-Grage, and Gibson 2009) and the Medicaid payment rate adjusted to 2009 dollars.
Analyses
Using the XTREG procedure in STATA 11.0 (StataCorp 2009), we estimated a facility fixed effects model to examine the relationship between OAA expenditures on Title III services and the proportion of low-care NH residents from 2000 to 2009. In addition to potential confounders, we controlled for time trends using a set of year dummy variables. Huber-White robust variance estimators were applied to adjust for within-state clustering over time and the facility-year is the unit of analysis.
Results
Over time, there has been an increase in states' expenditures on OAA Title III registered services and the percentage of Medicaid dollars going toward HCBS (see Figure 1 and Table 1). Accompanying these increases in funding for HCBS, there has been a decrease in the proportion of low-care residents of NHs from 17.9 percent in 2000 to 12.6 percent in 2009 (see Table 1).
Figure 1.
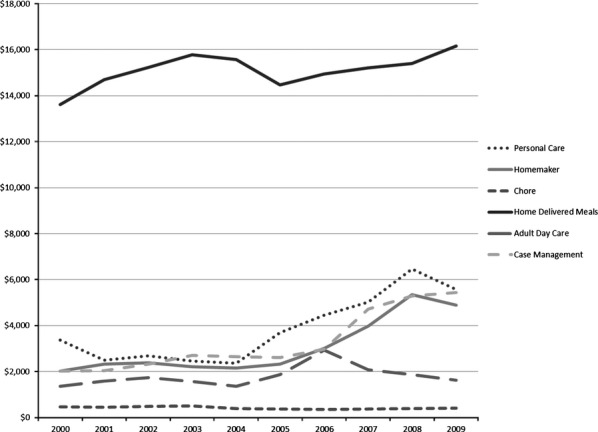
Average Expenditures on Title III Personal Care, Homemaker, Chores, Home-Delivered Meals, Adult Day Care, and Case Management Services per 1,000 65+ (2000–2009)
Table 1.
Descriptive Characteristics of Sample at Baseline (2000) and End of Study (2009)
| 2000 (N = 14,747) | 2009 (N = 14,385) | |||||
|---|---|---|---|---|---|---|
| Mean (SD) | Range | Mean (SD) | Range | |||
| Facility characteristics | ||||||
| Percent of residents classified “low care” | 17.85 | (13.16) | (0–100) | 12.58 | (11.70) | (0–100) |
| Percent medicaid | 61.98 | (26.67) | (0–100) | 60.39 | (23.13) | (0–100) |
| Occupancy rate | 84.33 | (15.47) | (1–100) | 83.44 | (14.82) | (1–100) |
| Percent of NH days that are SNF | 7.26 | (10.01) | (0–99) | 14.38 | (16.00) | (0–99) |
| Percent of admissions that are HMO | 7.76 | (11.28) | (0–100) | 13.15 | (12.03) | (0–100) |
| Market characteristics | ||||||
| No. of HHAs per 1,000 65+ | 0.51 | (0.55) | (0–5) | 0.38 | (0.42) | (0–4) |
| No. of NH beds in the county | 426.09 | (1143.45) | (15–40,916) | 439.18 | (1272.15) | (12–38,962) |
| State characteristics | ||||||
| %Medicaid $ on HCBS | 18.19 | (10.00) | (1–48) | 32.19 | (13.57) | (9–69) |
| Adjusted Medicaid payment rate | 130.17 | (26.44) | (83–200) | 159.64 | (29.39) | (114–229) |
Note. HCBS, home and community-based services; HHA, home health agencies; HMO, health maintenance organization; NH, nursing home; SNF, skilled nursing facility.
Results of our multivariate analyses indicate that increased spending on home-delivered meals was associated with fewer residents in NHs with low-care needs. Specifically, every additional $25 states spend on home-delivered meals per year, per person aged 65+ in the state, is associated with a decrease in the low-care NH population of 1 percent point. For example, Washington, over the study period, spent approximately $8.10 per capita aged 65+ on home-delivered meals and Wyoming spent $82.46. Using the coefficients generated from this model, states that spend, on average, the same amount as Washington would have an average low-care population of 16.8 percent, while states that spend similar to Wyoming would have an average low-care population of 13.8 percent in their NHs.
A number of facility characteristics were related to the prevalence of low-care residents. A higher occupancy rate and a higher percentage of residents funded by Medicaid were associated with a higher prevalence of low-care residents in the facility (see Table 2). In addition, NHs with a smaller proportion of NH days covered under the SNF benefit, and a smaller proportion of admissions covered by a Medicare HMO plan, were associated with a higher prevalence of low-care residents.
Table 2.
Results from Two-Way Fixed Effects Model (2000–2009)
| Coef. | Std. Err. | p > t | |
|---|---|---|---|
| OAA Title III services | |||
| Personal care | −0.001 | 0.012 | .905 |
| Homemaker | −0.003 | 0.010 | .793 |
| Chores | 0.225 | 0.214 | .300 |
| Home-delivered meals | −0.038 | 0.018 | .036 |
| Adult day care | 0.016 | 0.010 | .126 |
| Case management | 0.009 | 0.011 | .410 |
| Facility characteristics | |||
| Percent Medicaid | 0.024 | 0.003 | .000 |
| Occupancy rate | 0.030 | 0.004 | .000 |
| Percent of NH days that are SNF | −0.076 | 0.010 | .000 |
| Percent of admissions that are HMO | −0.037 | 0.009 | .000 |
| Market characteristics | |||
| No. of HHAs per 1,000 65+ | −0.025 | 0.101 | .807 |
| No. of 100 NH beds in the county | 0.001 | 0.000 | .713 |
| State characteristics | |||
| %Medicaid $ on HCBS | 0.016 | 0.020 | .431 |
| Adjusted Medicaid payment rate | −0.002 | 0.008 | .766 |
Note. N = 16,030 NHs and 145,649 facility-year observations.
Robust standard errors adjusted for clustering within facility. Year and facility dummy variables not shown. The first year, 2000, was the reference.
HCBS, home and community-based services; HHA, home health agency; HMO, health maintenance organization; NH, nursing home; OAA, older Americans Act; SNF, skilled nursing facility.
To test the robustness of our findings, we also modeled the relationship between OAA spending and the proportion of long-stay residents who at any time during the year appeared as low care on their MDS assessment. Results were consistent with our first Thursday in April estimate and, therefore, confirm that this relationship exists even with a more refined definition of the prevalence rate.
Discussion
Results from our study suggest that the decreasing prevalence of low-care residents in NHs was associated with increased spending on OAA programs and Medicaid HCBS programs over time. Up and above these temporal trends, our results suggest that increased state expenditures on home-delivered meal services were related to a decreased prevalence of low-care residents.
The home-delivered meals program is designed to address problems of food insecurity, promote socialization, and promote the health and well-being of older persons through nutrition and nutrition-related services (Colello 2011). Home-delivered meals are often the first in-home service that older adults receive and can often serve as a primary access point for other HCBS (Administration on Aging 2012). Home-delivered meals also provide an essential service to caregivers, by helping them maintain their own health and well-being. In addition, home-delivered meal services provide more than just food to recipients (Choi 1999). Drivers are often the eyes and ears who serve as a “safety check” and report changing health or needs of home-bound older adults. In addition, any unanswered delivery is reported and investigated. Oftentimes, those who deliver food also provide companionship to people who otherwise might be alone all day. Investment in home-delivered meals may be one of the mechanisms that help to keep low-care individuals out of the NH.
Predictors of NH entry include demographic characteristics, socioeconomic status, health status and physical functioning, living arrangements and family structure, and availability of support (Miller and Weissert 2000; Gaugler et al. 2007). A 2009 survey of home-delivered meals recipients found that 70 percent were age 75 and older, 56 percent lived alone, 25 percent had an annual income of $10,000 or less, and 59 percent said that the home-delivered meals program provided at least one-half of their daily food intake (Altshuler and Schimmel 2010). This survey also found that 4 of 10 home-delivered meals recipients reported needing help with one or more of the ADLs and 85 percent reported needing help with one or more instrumental ADLs (Altshuler and Schimmel 2010). This suggests that these individuals are particularly vulnerable and receiving meals may allow them to be maintained in the community.
While the home-delivered meals program is the largest of the OAA programs, it does not reach all of those in need. It is reported that nearly 4.5 million older adults living in the community need long-term care (Rogers and Komisar 2003). Among people 65 and older, estimates are that 14 percent need long-term care while among people age 85+, half need some long-term care. In fiscal year 2010, the home-delivered meals program through the OAA provided meals to 868,076 participants (Administration on Aging 2012). There are also many who are on waiting lists to receive these services (Day 2012). Therefore, expanding the funding and targeting services to reach these millions of older adults who need assistance may decrease the proportion of low-care residents in NHs.
The United States has made significant progress toward expanding HCBS, mainly through Medicaid HCBS waiver programs. However, our study indicated that the proportion of Medicaid spending going toward HCBS did not have a differential effect on the prevalence of low-care residents over time. Because low-care residents in this study could either be Medicaid eligible, Medicaid LTC eligible, or non-Medicaid eligible, the lack of association between increased Medicaid HCBS investment and decreased prevalence of low-care residents could likely be because some low-care residents are not Medicaid eligible. Future research should seek to determine whether the level of generosity of Medicaid eligibility levels may have an effect on the proportion of low-care residents in NHs. In particular, there is considerable variability in the eligibility levels for the medically needy program from state to state. It may be the case that in states with the most stringent requirements, frail, older individuals who are not quite eligible for Medicaid are not eligible for Medicaid HCBS and so enter NHs since they will rapidly become eligible for Medicaid residing there.
A major strength of this study lies in the use of a 10-year longitudinal multilevel dataset, which allowed examination of state HCBS spending on the prevalence of low-care residents that occurred over years. Obviously, we are not in a position to state unequivocally that increased OAA investment prevents NH admission among low-care individuals since these are observational data. Nonetheless, we controlled for national trends, Medicaid spending, and tested for the effect of changes in OAA investments over time, thereby addressing history and some state endogeneity. Use of a fixed effect model meant that real changes in facilities' proportion of low-care residents were independent of facility and market characteristics, all suggesting that these findings are more robust than many earlier studies that have examined these issues using cross-sectional data.
Nonetheless, it is also necessary to note the study's limitations. Our study is predicated upon the validity of the MDS functional assessment data and the assumption that residents who do not require skilled clinical services or assistance meeting their ADLs could be sustained in the community. Also, the lack of a specific level of cognitive functioning as an exclusion criterion for low care in this and previous research warrants further examination. While older adults diagnosed with dementia may be more likely in need of NH placement than older adults without (Temple, Andel, and Dobbs 2010), research (Buttar, Blaum, and Fries 2001) that has examined the cognitive status of low-care residents suggests that, in general, low-care residents have significantly better cognitive functioning compared with other NH residents (73 percent of the low-care residents in that study had either little or no cognitive impairment). Although some individuals identified as low-care residents under the present criteria may also have cognitive impairment, we believe that substantial cognitive impairment would be reflected in the ability to perform ADLs. In addition, we did not distinguish between the types of low-care residents by Medicaid eligibility. Increased investment in OAA is more likely to affect the general population of older adults while increased investments in Medicaid funded HCBS are likely to only decrease the prevalence of low-care residents in NHs who are Medicaid or Medicaid LTC eligible.
The use of state reported expenditure data does leave us to question the validity and consistency of the data from state to state. However, because we chose programs that require extensive client information to receive services, we believe that the record keeping and reporting would be more standardized from state to state. These data have been used in previous research and government reports; therefore, we deem them appropriate for this study question (Kitchener et al. 2007; Colello 2011; United States Government Accountability Office 2011). Another potential limitation is the use of older adults aged 65+ to adjust for OAA spending rather than the number of older adults aged 60+, for whom the federal dollars are allocated. However, census data only report projections for the aggregate numbers of 65+ in each year and OAA requires Title III programs to target or make it a priority to serve older adults with the greatest economic and social need. Therefore, we believe adjusting for the number of older adults aged 65+ in the state is appropriate and has been done elsewhere to present these data (United States Government Accountability Office 2011).
As the United States prepares for an aging population and the demand for health and social services necessary to assist older adults to live independently in the community increases, ensuring access to HCBS will likely continue to be an issue for policy makers. This article reveals that despite efforts to rebalance LTC, there are still many NH residents who have the functional capacity to live in a less restrictive environment. States that have invested in their community-based service networks, particularly home-delivered meals, have proportionally fewer of these people than do those states that have not. The challenge for states and CMS will be to build and invest in systems and programs that divert unnecessary NH placement for individuals who can be sustained in the community.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by the National Institute on Aging (P01AG027296) and the Agency for Healthcare Research and Quality (5T32HS000011).
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
References
- Administration on Aging. 2012. “Nutrition Services (OAA Title IIIC)” [accessed on July 25, 2012]. Available at http://www.aoa.gov/AoA_programs/HCLTC/Nutrition_Services/index.aspx.
- Altshuler N, Schimmel J. Aging in Place: Do Older Americans Act Title III Services Reach Those Most Likely to Enter Nursing Homes. Washington, DC: Mathematica Policy Research; 2010. [Google Scholar]
- Arling G, Kane RL, Cooke V, Lewis T. “Targeting Residents for Transitions from Nursing Home to Community”. Health Services Research. 2010;45:691–711. doi: 10.1111/j.1475-6773.2010.01105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttar A, Blaum C, Fries BE. “Clinical Characteristics and Six-Month Outcomes of Nursing Home Residents with Low Activities of Daily Living Dependency”. Journals of Gerontology: Medical Sciences. 2001;56A:M292–7. doi: 10.1093/gerona/56.5.m292. [DOI] [PubMed] [Google Scholar]
- Castle NG. “Low-Care Residents in Nursing Homes”. Journal of Health & Social Policy. 2002;14:41–58. doi: 10.1300/J045v14n03_03. [DOI] [PubMed] [Google Scholar]
- Choi NG. “Determinants of Frail Elders' Lengths of Stay in Meals on Wheels”. The Gerontologist. 1999;39(4):397–405. doi: 10.1093/geront/39.4.397. [DOI] [PubMed] [Google Scholar]
- Colello KJ. Older Americans Act: Title III Nutrition Services Program. Washington, DC: Congressional Research Service; 2011. [Google Scholar]
- Day T. 2012. “About the National Aging Network” [accessed on July 25, 2012]. Available at http://www.longtermcarelink.net/eldercare/area_agencies_on_aging.htm.
- Gaugler JE, Duval S, Anderson KA, Kane RL. “Predicting Nursing Home Admission in the U.S.: A Meta-Analysis”. BMC Geriatrics. 2007;7(13):1–14. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn EA, Thomas KS, Hyer K, Andel R, Meng H. “Predictors of Low-Care Prevalence in Florida Nursing Homes: The Role of Medicaid Waiver Programs”. The Gerontologist. 2011;51:495–503. doi: 10.1093/geront/gnr020. [DOI] [PubMed] [Google Scholar]
- Houser AN, Fox-Grage W, Gibson MJ. Across the States 2009: Profiles of Long-Term Care and Independent Living. Washington, DC: AARP Public Policy Institute; 2009. [Google Scholar]
- Ikegami N, Morris JN, Fries BE. “Low-Care Cases in Long-Term Care Settings: Variation among Nations”. Age and Ageing. 1997;26:67–71. doi: 10.1093/ageing/26.suppl_2.67. [DOI] [PubMed] [Google Scholar]
- Intrator O, Hiris J, Berg K, Miller SC, Mor V. “The Residential History File: Studying Nursing Home Residents' Long-Term Care Histories”. Health Services Research. 2011;46(1):120–37. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitchener M, Ng T, Carrillo H, Miller N, Harrington C. “Developing Personal Care Programs: National Trends and Interstate Variation”. Inquiry. 2007;44(1):69–87. doi: 10.5034/inquiryjrnl_44.1.69. [DOI] [PubMed] [Google Scholar]
- Miller EA, Weissert WG. “Predicting Elderly People's Risk for Nursing Home Placement, Hospitalization, Functional Impairment, and Mortality: A Synthesis”. Medical Care Research and Review. 2000;5(3):259–97. doi: 10.1177/107755870005700301. [DOI] [PubMed] [Google Scholar]
- Mor V, Zinn J, Gozalo P, Feng Z, Intrator O, Grabowski D. “Prospects for Transferring Nursing Home Residents to the Community”. Health Affairs. 2007;26:1762–71. doi: 10.1377/hlthaff.26.6.1762. [DOI] [PubMed] [Google Scholar]
- Muramatsu N, Yin H, Campbell RT, Hoyem RL, Jacob MA, Ross CO. “Risk of Nursing Home Admission among Older Americans: Does States' Spending on Home and Community-Based Services Matter?”. Journals of Gerontology Series B: Psychological and Social Sciences. 2007;62:S169–78. doi: 10.1093/geronb/62.3.s169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muramatsu N, Hoyem RL, Yin H, Campbell RT. “Place of Death among Older Americans: Does State Spending on Home- and Community-Based Services Promote Home Death?”. Medical Care. 2008;46(8):829–38. doi: 10.1097/MLR.0b013e3181791a79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers S, Komisar H. Who Needs Long-Term Care? [Fact Sheet] Washington, DC: Health Policy Institute, Georgetown University; 2003. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 11 Release. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- Stearns SC, Dalton K, Holmes GM, Seagrave SM. “Using Propensity Stratification to Compare Patient Outcomes in Hospital-Based versus Freestanding Skilled-Nursing Facilities”. Medical Care Research and Review. 2006;63(5):599–622. doi: 10.1177/1077558706290944. [DOI] [PubMed] [Google Scholar]
- Temple A, Andel R, Dobbs D. “Setting of Care Modifies Risk of Nursing Home Placement for Older Adults with Dementia”. International Journal of Geriatric Psychiatry. 2010;25(3):275–81. doi: 10.1002/gps.2333. [DOI] [PubMed] [Google Scholar]
- United States Government Accountability Office. Older Americans Act: More Should Be Done to Measure the Extent of Unmet Need for Services. Washington, DC: GAO; 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


