Abstract
Major depressive disorder (MDD) is a common, debilitating chronic condition in the United States and worldwide. Particularly in women, depressive symptoms are often accompanied by high levels of stress and ruminations, or repetitive self-critical negative thinking. There is a research and clinical imperative to evaluate complementary therapies that are acceptable and feasible for women with depression and that target specific aspects of depression in women, such as ruminations. To begin to address this need, we conducted a randomized, controlled, mixed-methods community-based study comparing an 8-week yoga intervention with an attention-control activity in 27 women with MDD. After controlling for baseline stress, there was a decrease in depression over time in both the yoga group and the attention-control group, with the yoga group having a unique trend in decreased ruminations. Participants in the yoga group reported experiencing increased connectedness and gaining a coping strategy through yoga. The findings provide support for future large scale research to explore the effects of yoga for depressed women and the unique role of yoga in decreasing rumination.
Introduction
One of the most common and debilitating health conditions in the United States and worldwide is major depression, considered in this paper to include major depressive disorder (MDD) and dysthymia (Branchi & Schmidt, 2011; Kessler et al., 2003). Clinically, the condition presents as a persistently depressed mood with anhedonia, feelings of worthlessness, impaired cognitive abilities, altered sleep and appetite patterns, and suicidal ideations (American Psychiatric Association (APA), 2000). Epidemiological studies have demonstrated that women are disproportionately affected by depression, such that women have approximately double the prevalence rate of depression compared to men (Kessler et al., 2003). The interplay of biological and psychosocial vulnerabilities, stress, and individual personality and coping behaviors may be responsible for this increased prevalence of depression in women (Kinser, Goehler, & Taylor, 2012).
Depression is a complex disorder that can be difficult to treat successfully. Many women with depression express frustration about the usual care, citing reasons such as inadequate symptom management, unacceptable side effects, and inadequate methods for coping (Kessler et al., 2003; Lafrance & Stoppard, 2006; S. Nolen-Hoeksema & Hilt, 2009). The efficacy of the usual care for depression (pharmaceutical management and cognitive therapy) is poorer than originally thought; recent close evaluation of large-scale studies on these usual care methods has revealed large participant dropout rates and low remission rates as well as generalized reporting bias (Mathew & Charney, 2009; Pigott, Leventhal, Alter, & Boren, 2010; Turner, Matthews, Linardatos, Tell, & Rosenthal, 2008). More research is called for regarding innovative psychosocial treatments, particularly in typically under-studied populations such as women with severe depression (National Institute of Mental Health, 2005).
Although depression is characterized by a depressed mood, many women experience a variety of psychological, cognitive, and physical symptoms beyond the depressed mood (APA, 2000). For example, up to half of all women with a diagnosis of depression may experience “anxious depression,” typified by excessive ruminations (Halbreich & Kahn, 2007; Marcus et al., 2008). Rumination is a complex concept, typically defined as repetitive negative thinking about one’s depression and life situations (Smith & Alloy, 2009). Individual differences in coping patterns and ruminations play a role in the cycle of stress and depression (Hauenstein, 1996; Nolen-Hoeksema, 2006). Rumination is generally considered to be an emotion-focused coping style that is often ineffective or maladaptive because it can perpetuate stress and depressive symptoms (Lyubomirsky & Tkach, 2004; Weinstein, Brown, & Ryan, 2009). A low sense of mastery seems to contribute to brooding, a factor of rumination, when one repeatedly contemplates what’s wrong in one’s life and why it is not better (Treynor, Gonzalez, & Nolen-Hoeksema, 2003). As such, there is a research and clinical imperative to evaluate complementary therapies that are acceptable and feasible for women with depression and that target specific aspects of depression in women, such as ruminations. Yoga is a commonly practiced multifaceted mind-body modality that warrants attention for its potential use for depression (Barnes, Bloom, & Nahin, 2009; Birdee et al., 2008; Uebelacker et al., 2010).
Yoga for Depression
Findings from numerous studies suggest that various yoga interventions may help decrease psychological and physical symptoms of depression and stress in a variety of clinical and non-clinical populations (see multiple review articles: Kirkwood, Rampes, Tuffrey, Richardson, & Pilkington, 2005; Pilkington, Kirkwood, Rampes, & Richardson, 2005; Uebelacker et al., 2010). Only a small number of studies have rigorously tested the use of yoga for individuals with diagnostic levels of depression (i.e., MDD or dysthymia). Results of the few randomized controlled trials (RCTs) of yoga for MDD or dysthymia suggest that yoga may improve the mood or prevent recurrence of major depressive episodes (Broota & Dhir, 1990; Butler et al., 2008; Janakiramaiah et al., 2000; Sharma, Das, Mondal, Goswampi, & Gandhi, 2005). A recently conducted open trial of yoga for MDD found that yoga may be feasible for this population, yet the study did not evaluate adherence to the intervention or ruminations (Uebelacker, Tremont et al., 2010). Considering that brooding ruminations are associated with increased depression symptoms and suicidality in women, it is recommended that studies include ruminations as an outcome of intervention studies for depression (Lopez, Driscoll, & Kistner, 2009). Unfortunately, the limitations of research studies on yoga for depression abound, ranging from methodological issues with RCTs (Broota & Dhir, 1990; Butler et al., 2008; Janakiramaiah et al., 2000; Sharma et al., 2005) to the use of healthy participants or those with only a self-report of depressive symptoms (i.e., no confirmation of diagnosis of depression), unclear inclusion/exclusion criteria, and intervention lengths shorter than typically used in pharmaceutical treatment studies for depression (i.e., less than 8 weeks) (Pilkington et al., 2005; Uebelacker et al., 2010). Furthermore, most studies do not focus on the particular symptoms related to depression in women, such as repetitive negative thinking (ruminations) (Conway, Csank, Holm, & Blake, 2000; Morrison & O’Connor, 2008; S. Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008; Smith & Alloy, 2009).
Despite the limitations of previous studies, the preliminary evidence supports a need for a closer evaluation of the feasibility, acceptability, and mechanisms of effects of yoga for individuals with major depression. The most generally accessible form of yoga in the United States, Hatha yoga (simply called “yoga” henceforward) is a mind-body modality that combines physical practices, breathing practices, and relaxation/ meditative practices intended to enhance overall health and well-being (Desikachar, Bragdon, & Bossart, 2005; NCCAM, 2010; Uebelacker et al., 2010). Yoga may be an appropriate coping intervention for depression, as it can be self-administered, can be specifically adapted to one’s mood, and is safe for yoga-naïve individuals (NCCAM, 2010; Weintraub, 2004). The symptoms of depression often affect daily functioning and prevent women from participating in social, physical, or other self-care activities. It is these very symptoms that can potentially be reduced by a mind-body intervention such as yoga, if women with depression will accept and participate in yoga sessions. As such, the primary aim of the randomized, controlled, pilot study was to evaluate the feasibility and acceptability of an 8-week yoga intervention specifically designed for women with depression. Our secondary aim was to evaluate the effects of yoga over time as compared to an attention-control group. The study is based upon a biobehavioral paradigm focusing on the cyclic interplay of stress, stress appraisal/responses, and allostatic overload/ depression in women (see Hauenstein, 1996; Kinser, 2012; Nolen-Hoeksema, 2006). Our study provides important insights for understanding and intervening with depression in women, particularly those who have residual depressive symptoms despite treatment with the usual care.
Methods
The University of Virginia Institutional Review Board (IRB) for Health Sciences Research reviewed and approved the study protocol, recruitment plans, and guidelines for the protection of confidentiality of participants. Written informed consent was obtained from participants prior to their enrollment in the study; in addition to the written consent, verbal consent also was obtained prior to audio recording the participant interviews.
Study Design
This community-based prospective, randomized, clinical intervention pilot study was conducted in a metropolitan city on the east coast of the United States. A mixed-methods approach with an embedded design was used to provide a comprehensive view of the feasibility, acceptability, and efficacy of yoga for women with depression (Doyle, Brady, & Byrne, 2009; Sandelowski, 2000). Participants continued their usual lifestyle patterns and usual depression care.
Sampling Methods
IRB-approved materials were posted in public locations throughout the recruitment area as well as in the offices of primary care providers, women’s health providers, and mental health care providers. The recruitment materials advertised a free study on a complementary therapy for women with depression. Interested individuals contacted the investigator directly. After a short telephone screening for depressive symptoms, eligible respondents were scheduled for an in-person visit in which consent, in-depth screening, and baseline study measures were completed. Inclusion and exclusion criteria are outlined in Table 1. In order to be enrolled in the study, participants were screened for major depressive disorder with a current major depressive episode or dysthymia using the MINI-International Neuropsychiatric Interview (MINI) instrument (Sheehan et al., 1998). If a participant consented to be part of the study but then decided against participation at any point, she was offered the opportunity to provide reasons for not continuing by participating in a short semi-structured interview with the investigator. After the consent process, participants were randomized into one of two groups (yoga intervention group or attention-control group) using random numbers generated by computer.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
Intervention
Yoga group
The 8-week yoga intervention involved once-weekly group classes and daily home practice with a DVD and handouts, all of which were safe for yoga-naïve individuals. The 75-minute group gentle Hatha yoga class was taught by experienced yoga teachers familiar with teaching yoga-naïve students. To maintain treatment integrity, the teachers were trained by the investigator prior to the study. All teachers used a manual during the study with options of sequences of gentle yoga movements, breathing practices, and relaxation practices specifically designed for depression. The yoga intervention manual was developed by the investigator using relevant written materials on yoga for depression and through collaboration with expert yoga teachers and borrowed from multiple gentle styles of yoga commonly found in the United States (e.g. gentle/Hatha, Iyengar, Kripalu, LifeForce yoga) (Sparrowe & Walden, 2002; Weintraub, 2004).
The fundamental aspects of the group yoga classes are as follows: (a) creation of a safe space and empowerment to adapt practice according to the mood, (b) intention setting with weekly themes, (c) pranayama (breathing practices), (d) asana (physical practices), and (e) yoga nidra (guided meditation) and savasana (relaxation). The safe space was created at the beginning of every class by the yoga teachers, who reminded participants to modify or stop any poses or activities that were uncomfortable and/or to try something new. In addition, considering that most depressed individuals experience the symptoms of depression to be neither predictable nor consistent from day to day, participants in this study were encouraged to use yogic practices in a way that best met their daily needs, which differentiates this yoga intervention from others in the literature that do not account for individual mood differences (Halbreich & Kahn, 2007; Kinser et al., 2012; Marcus et al., 2008; Weintraub, 2004). To help participants focus on key aspects of the yoga intervention, every week had a theme such as self-care, finding balance, mindfulness, and others. Pranayama, or breathing practices, taught conscious regulation of the breath, with specific patterns designed to induce a sense of calm, well-being, stress tolerance, and mental focus (Benson, 1975; Brown & Gerbarg, 2005a; Brown & Gerbarg, 2005b; Brown & Gerbarg, 2009; Taylor, Goehler, Galper, Innes, & Bourguignon, 2010; Uebelacker et al., 2010). Gentle physical poses, asanas, were introduced with simple directive language and permission to adapt as needed; the level of difficulty of the poses increased slightly over the 8-week series of classes. Every yoga class ended with yoga nidra and savasana (guided meditation and relaxation). To prevent distraction from intrusive thoughts, periods of silence were kept initially to a minimum during savasana, with slowly increasing lengths of silence over the course of the sessions.
The home practices were guided by two resources for participants: (1) a DVD designed to allow them to individually adapt their daily yoga practice according to their current mood by picking from multiple 10-minute segments from the DVD menu (Weintraub & Duncan, 2007), and (2) class handouts provided after every class with themes, quotes, pictures, and descriptions of the yoga poses practiced that week.
Attention-control group
Participants in the attention-control group engaged in a series of health education sessions titled “Health and Wellness Program.” Involving lectures and videos, each session was a 75-minute weekly group class for 8 weeks. Each week had a specific theme, such as heart health, bone health, and others; handouts that included information and additional resources on that week’s topic were provided for participants to review at home. The classes were led by registered nurses who were trained by the investigator prior to the study. To maintain treatment integrity, they used a manual developed by the investigator. As with the yoga group, these classes were comprised only of study participants, and participants were made aware of this fact during the consent process. To maintain internal validity, all efforts were made to avoid the use of lectures, videos, or handouts that overlapped the content and essence of the yoga intervention. To control for potential group-effect and interaction time with study staff, the attention-control group had the same number of class meetings (8) and amount of class time (75 minutes) as the yoga group (Beal, Stuifbergen, Volker, & Becker, 2009; Lindquist, Wyman, Talley, Findorff, & Gross, 2007; Street & Luoma, 2002).
Data Collection
For the feasibility and acceptability aim of the study, three qualitative aspects were involved: First, a semi-structured interview was conducted with eligible women who declined full participation in the study after the initial screening and with those who dropped out of the study at any point; the open-ended questions were intended to elicit their reasons for not participating. Second, semi-structured exit interviews were conducted at the completion of the study with participants in both the yoga and attention-control groups using open-ended questions on topics such as participants’ overall impressions about the following: the intervention itself, aspects of the intervention that were or were not beneficial, what made participation in the intervention difficult or easy, and individuals’ plans for future use of yoga or other methods for mood. Third, participants were invited to document their feelings about their daily yoga practice and the type of practice used (e.g., group class, DVD, class handouts, or other) in the form of a daily log. Participants’ use of yoga was quantified by totaling the number of minutes practiced over 8 weeks (time in group classes plus the minutes of yoga practice per day documented on the daily practice logs).
To evaluate the effects of group on the following outcome measures, paper and pencil instruments were completed by participants at home:
Depression severity (timepoints- baseline, 2 weeks, 4 weeks, 6 weeks, 8 weeks)
Depression severity was evaluated using the Patient Health Questionnaire (PHQ-9), a widely used instrument based on the diagnostic criteria for depressive disorders in the DSM-IV-TR; the PHQ-9 includes self-report items regarding depressive symptoms over the past 2 weeks on a 4-point Likert scale. Total scores range from 0–27, where 0–4 indicates minimal depression, 5–9 mild depression, 10–14 moderate depression, 15–19 moderately severe depression, ≥20 severe depression. The PHQ-9 includes a question on suicidal ideation, which was used for monitoring for adverse events (Kroenke, Spitzer, & Williams, 2001; Löwe, Kroenke, Herzog, & Gräfe, 2004; Spitzer, Kroenke, Williams, & and the Patient Health Questionnaire Primary Care Study Group, 1999).
Stress (timepoints- baseline, 4 weeks, 8 weeks)
The Perceived Stress Scale-10 (PSS-10), a widely used psychometrically sound instrument, was used to measure the degree to which a participant perceived stress in her life during the past month, with items ranked on a 5-point Likert scale (S. Cohen & Williamson, 1988; S. Cohen, 1994; S. Cohen, Tyrrell, & Smith, 1993; Hewitt, Flett, & Mosher, 1992; Logsdon & Hutti, 2006). Designed to measure stress from chronic conditions or situations, the PSS-10 asks respondents to report about feelings such as unpredictability, uncontrollability, and overloading of stress in their lives with items ranked on a 5-point Likert scale; scores range from 0–40 with the higher score corresponding to a higher perceived stress level (S. Cohen, 1994).
Anxiety (timepoints- baseline, 4 weeks, 8 weeks)
Current levels of anxiety (“state anxiety”) were evaluated with the State-Trait Anxiety Inventory, Form Y (STAI). The S-Anxiety portion of the STAI evaluates subjective state anxiety, measuring how an individual feels “right now, at this moment” on a 4-point Likert scale. The 10-minute self-administered STAI has good psychometric properties and is well-established in terms of feasibility and readability (Spielberger, Gorsuch, & Lushene, 1970; Spielberger, 1983; Tilton, 2008).
Rumination (timepoints- baseline, 4 weeks, 8 weeks)
Rumination, or repetitive negative thinking, was evaluated with the 10-item Ruminative Responses Scale (RRS) which was designed to evaluate the propensity to ruminate in association with sadness or depression. A psychometrically sound and commonly used instrument, the RSS asks respondents to rate how often they experience various aspects of rumination on a 4-point Likert scale (1=almost never to 4=almost always) (Treynor et al., 2003). The RRS has two factors of brooding (self-critical pondering, as in “Why can’t I handle things better?”) and reflecting (emotionally-neutral pondering or brainstorming, as in “Analyze your personality to try to understand why you are depressed”). Some researchers separate the RRS into separate brooding and reflection subscales because, in studies of adolescents and suicidal patients, high scores on the reflection items were associated with enhanced cognitive coping whereas high scores on brooding items were associated with maladaptive coping (Burwell & Shirk, 2007; Crane, Barnhofer, & Williams, 2007). However, statistical data analysis for this study did not support separating the scales.
Interpersonal sensitivity and hostility (timepoints- baseline, 4 weeks, 8 weeks)
Subscales of the Brief Symptom Inventory were used to evaluate interpersonal factors often involved in depression: interpersonal sensitivity and hostility. This feasible and valid tool was designed to measure concerns about rejection by others and the tendency to be irritable during interpersonal interactions. In the 9-item subscales for sensitivity and hostility, respondents are asked to indicate how much certain concerns have distressed or bothered them during the past month on a 5-point Likert scale (0=not at all, 4=extremely); examples of items include: “Your feelings being easily hurt” (interpersonal sensitivity) and “Feeling easily annoyed or irritated” (interpersonal hostility) (Derogatis & Melisaratos, 1983).
Statistical Analysis Plan
In order to best understand participants’ view of feasibility and acceptability of the intervention, qualitative data were analyzed using a descriptive qualitative methodology with phenomenological overtones (Sandelowski, 2000). The data collected were analyzed in the manner of a hermeneutic circle (Agar, 1986; Cohen, Kahn, & Steeves, 2000). Data from interviews with participants who completed the study or dropped out of the study were analyzed for common themes regarding feasibility, acceptability, and effects of the yoga intervention or attention-control activity.
The quantitative data were analyzed using SPSS Version 19. Calculations of descriptive statistics on demographic and study variables were completed in the form of means and standard deviations (continuous variables) or frequencies and percentages (categorical variables). Baseline group differences in demographic and baseline study variables were analyzed using independent t-tests for continuous variables and chi-square tests for categorical variables; assumptions of univariate normality and homogeneity of variance were met, using Fisher’s test of skewness and Levene’s test. To determine if there were differences over time by group, separate multilevel models were used to estimate differences in the slopes between the groups for the measures of depression, stress, anxiety, rumination, and interpersonal sensitivity/hostility. Model parameters have been estimated by restricted maximum likelihood, and the within-subject variance-covariance matrix is modeled in the form determined by Akaike’s AIC criterion. Random intercepts and slopes have been estimated from the data. At Level 1 (within-subject analysis), the models estimated change for participants. At Level 2 (between-subjects analysis), the differences in average slopes for each group (yoga group vs. the attention-control group) were modeled. Testing revealed no major violations of assumptions (univariate normality, multivariate normality and linearity), other than small sample size. AIC was used to determine the appropriate model and covariance structure, and the random intercept and slope model and unstructured covariance structure were the best fit for all models. Covariates were centered to the mean. Given that this is a feasibility pilot study, an alpha = 0.05 has been used for all tests; trends are closely examined.
Results
Recruitment
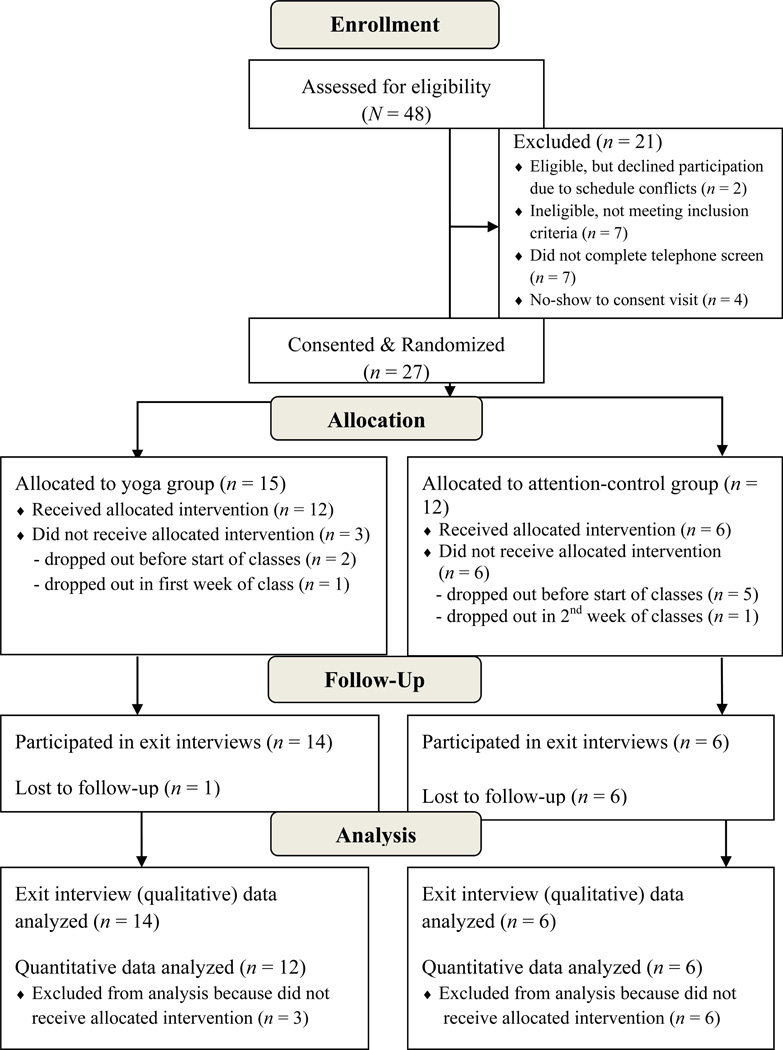
A flowchart of participant recruitment, enrollment, and completion of the study is shown in Figure 1. The 4-month recruitment period occurred from May to August 2011. A total of 48 women expressed interest in the study. Of these, 7 individuals did not complete the full telephone screening to determine eligibility, either because they could not be reached or they called after enrollment had ended. Five individuals who were eligible from the telephone screening did not show up for their in-person screening/consent visits and were lost to follow-up; their mean depression scores were 19.8 (SD = 5.6; range 10–24). Of those who did complete the telephone screenings, 7 individuals were ineligible to participate because they did not have sufficiently severe depression. Two other individuals were eligible based upon the telephone screening criteria but were unable to participate in the full study because of schedule conflicts; their mean depression scores were 16 (SD = 1.4). Twenty-seven individuals completed the in-person screening, were enrolled as participants in the study, and were randomized to the yoga group or the attention-control group. Nine individuals dropped out at some point during the study (n = 6 from attention-control group; n = 3 from yoga group). The majority of those who dropped out participated only in the screening visit and never participated in any aspect of the intervention (n = 5 in attention-control group; n = 2 in yoga group); the rest dropped out in the first few weeks of the intervention period (n = 1 in control group; n = 1 in yoga group). Most of the participants from both groups agreed to be interviewed (n = 6 in attention-control group; n = 14 in yoga group), but some were lost to follow-up before exit interview (n = 6 in attention-control group; n = 1 in yoga group).
Figure 1.
Participant Flow Diagram
Sample
Twenty-seven participants enrolled in the study. See Table 2 for group differences on the demographic characteristics of the study population, based upon independent t-tests for continuous variables and chi-square tests for categorical variables. There were no significant differences between the groups in most of the demographic variables such as age, ethnicity/race, marital status, employment status, current major depressive episode, reported recent major life changes, antidepressant/ anxiolytic use, current use of individual psychotherapy, and current participation in exercise. As demonstrated in Table 3, there were no group differences in baseline levels of the variables of interest (depression, anxiety, stress, ruminations, interpersonal sensitivity and hostility), based upon independent t-tests for these normally distributed continuous variables.
Table 2.
Group Differences on Demographic Characteristics
| Group Assignment | ||||||||
|---|---|---|---|---|---|---|---|---|
| Demographic Characteristics |
Overall (n = 27) mean (SD) or n (%) |
Yoga (n = 15) mean (SD) or n (%) |
Attention- Control (n = 12) mean (SD) or n (%) |
Statistic |
p- value |
|||
| Age | 43.26 | (15.57) | 40.93 | (15.84) | 46.17 | (15.40) | −.86 Ŧ | .40 |
| Ethnicity/Race | ||||||||
| White (non-Hispanic) | 17 | (62.96%) | 10 | (66.67%) | 7 | (58.33%) | .19 ŧ | .66 |
| Non-White | 10 | (37.04%) | 5 | (33.33%) | 5 | (41.67%) | ||
| Education | ||||||||
| <college degree | 10 | (37.04%) | 3 | (20.00%) | 7 | (58.33%) | 4.20 ŧ | .04 |
| ≥ college degree | 17 | (62.96%) | 12 | (80.00%) | 5 | (41.67%) | ||
| Marital/Partner Status | ||||||||
| Single/ divorced | 20 | (74.1%) | 11 | (73.3%) | 9 | (75.00%) | .01 ŧ | .92 |
| Married/partnered | 6 | (25.9%) | 4 | (26.7%) | 3 | (25.00%) | ||
| Employment Status | ||||||||
| Full-time | 13 | (48.15%) | 8 | (53.33%) | 5 | (41.67%) | .36 ŧ | .55 |
| Part-time/not working | 14 | (51.85%) | 7 | (46.67%) | 7 | (58.33%) | ||
| Current Major Depression | ||||||||
| (MDD or MDE) | 22 | (81.50%) | 11 | (73.33%) | 11 | (91.67%) | 1.49 ŧ | .22 |
| Reports Recent Major Life | ||||||||
| Changes | 15 | (55.56%) | 9 | (60.00%) | 6 | (50.00%) | .27 ŧ | .60 |
| Current Use of Anti-Depressant Medications | 17 | (62.96%) | 9 | (60.00%) | 8 | (66.67%) | .13 ŧ | .72 |
| Current Use of Anxiolytic | ||||||||
| Medications | 10 | (37.04%) | 6 | (40.00%) | 4 | (33.33%) | .13 ŧ | .72 |
| Currently in Individual | ||||||||
| Psychotherapy | 19 | (70.37%) | 11 | (73.33%) | 8 | (66.67%) | .14 ŧ | .71 |
| Currently Engages in | ||||||||
| Exercise (any type) | 11 | (40.74%) | 7 | (46.67%) | 4 | (33.33%) | .49 ŧ | .48 |
= t-test
ŧ = Chi-square
MDD = major depressive disorder; MDE = major depressive episode
Table 3.
Group Differences on Study Variables at Baseline
| Group Assignment | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study Variable | Overall (n= 27) mean (SD) |
Yoga (n=15) mean (SD) |
Attention- Control (n=12) mean (SD) |
t-test |
p -value |
|||
| Depression (PHQ9) | 15.44 | (5.90) | 14.67 | (4.58) | 16.42 | (7.33) | −.76 | .46 |
| Perceived Stress (PSS) | 38.26 | (5.66) | 38.47 | (4.58) | 38.00 | (6.95) | .21 | .84 |
| Anxiety (STAI) | 53.37 | (12.81) | 52.53 | (13.51) | 55.08 | (12.32) | −.51 | .62 |
| Ruminations (RSS) | 26.30 | (5.74) | 27.40 | (5.05) | 24.92 | (6.45) | 1.12 | .27 |
| Interpersonal Sensitivity & Hostility | 12.11 | (7.24) | 12.00 | (4.91) | 12.25 | (9.65) | −.08 | .93 |
Retention and Adherence
Eighteen out of the original 27 participants completed the study. Retention rates differed between the two groups, such that more participants in the yoga group (n = 12; 80%) completed the study than did those in the attention-control group (n = 6; 50%). All participants attended an average of 6.9±1.2 classes, with no significant difference between the groups in adherence to the intervention (p = .18). The recommended “dose” of the yoga intervention was a once-weekly 75-minute group class and approximately 20 minutes per day on other days (total of 195 minutes per week or 1560 minutes over 8 weeks). The mean total minutes of yoga practiced by all individuals in this group (1153.8±609.4 minutes) was less than the total recommended minutes; however, as can be seen in the standard deviation, there was a wide range in the amount of home practice across individuals. On any given week, 40–50% of participants met the recommended dosage of minutes in home yoga practice.
Completion Status
There were no statistically significant baseline differences between those who went on to complete the intervention (n = 18) and those who did not (n = 9). Similar to those who completed the study, most individuals who did not complete the study were white, single, had at least a college degree, were taking an antidepressant, were participating in individual psychotherapy, and were not exercising on a regular basis. The only trend towards significance that was identified was in the area of reported recent major life changes at baseline. More completers (n = 12; 66.67%) than non-completers (n = 3; 33.33%) reported recent major life changes (χ2=2.7; p=.051). There was no difference in baseline study variables between those who completed the study and those who did not, such that the non-completers looked very similar to the completers with regards to levels of depression, stress, anxiety, ruminations, and interpersonal factors.
Group Differences in Study Outcomes
In the first model represented in Table 4, we examined the longitudinal change by group in depression (PHQ-9) using 5 time points (baseline, 2, 4, 6, and 8 weeks). The addition of baseline stress significantly improved the model fit; thus, we will focus on this model. The baseline average depression score for those in the usual care group was 17.5 for a participant with average levels of stress at baseline (see intercept coefficient), indicating moderately severe depression (a score between 15–20 on the PHQ-9). The significant covariate of baseline stress indicated that as baseline stress increased, the baseline depression score also increased. All participants, as a whole, had decreasing levels of depression over time (indicated by the significant time coefficient). There were no significant differences in depression scores over time between the yoga and control groups (non-signficant group by time interaction).
Table 4.
Differences over Time in Depression and Rumination- Multilevel Models
| Depression | Rumination | |||
|---|---|---|---|---|
| Models | Unadjusted | Adjusted | Unadjusted | Adjusted |
| Intercept | 17.3 | 17.5* - | 25.7* | 25.9* |
| Time | −2.4* | −3.3* | 1.2* | −1.0 |
| Group | −3.1* | 2.4* | −1.5 | −1.5 |
| Group × time | −0.1 | −0.1 | −2.0** | −2.0** |
| Baseline stress | 0.5* | 0.5* | ||
| AIC | 498.5 | 489.1 | 313.8 | 310.9 |
| df | 8 | 9 | 8 | 9 |
p<.05
p<0.1 (trend)
Adjusted models: baseline stress centered to the mean is covariate
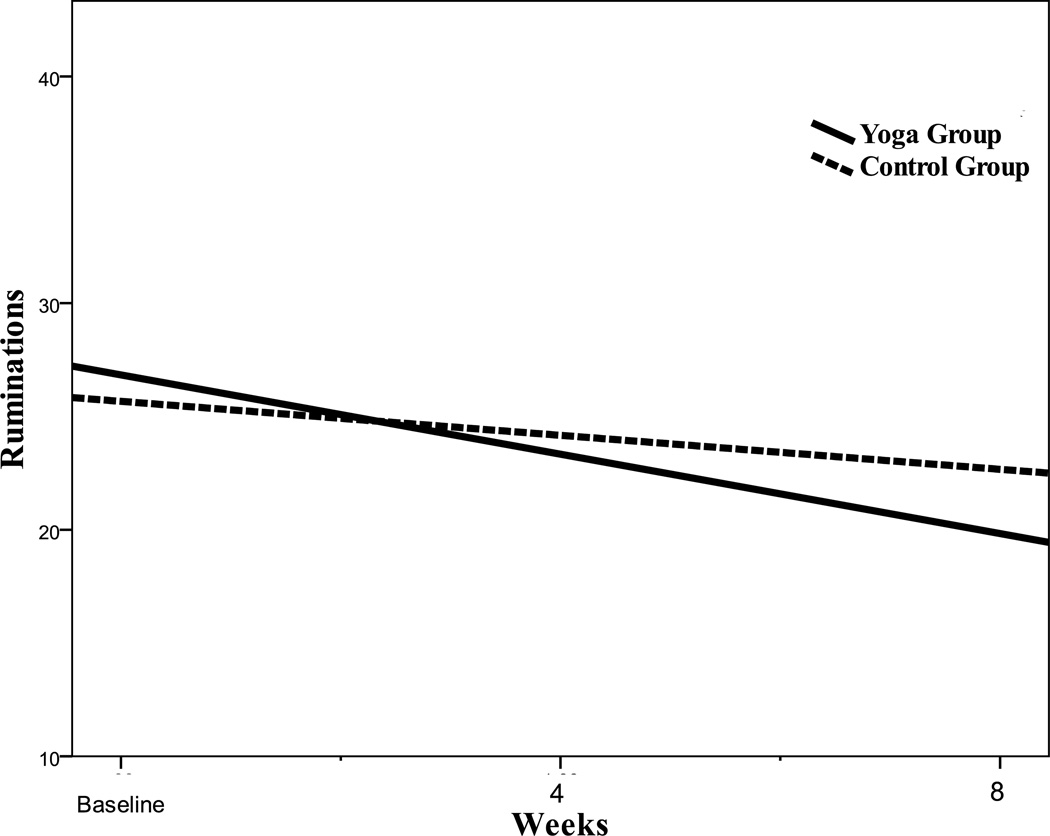
In the second model represented in Table 4, we evaluated whether or not there were group differences in ruminations over time at 3 time points (baseline, 4, and 8 weeks). The addition of baseline depression did not improve the model fit so this variable was not used as a covariate. Baseline stress was a significant covariate that did improve model fit, thus it will be included in the model for rumination. The baseline average rumination score was 25.9 for a participant in the control group. As baseline stress levels increased, baseline rumination scores also increased (indicated by a significant baseline stress coefficient). The trend in group differences over time (p = .083) indicated that the yoga group had reduced rumination scores over time compared to the control group (see Figure 2). The coefficient of time was not significant, suggesting that there was not an equivalent decrease in rumination scores in the control group.
Figure 2.
Slopes of Rumination Scores Over Time by Group
Longitudinal changes in other study variables, including anxiety, stress, and interpersonal sensitivity/ hostility, were examined with additional models not represented in the table. Results of these models revealed a significant time effect such that there was a decrease in scores in all measures in all participants over time. However, there were no differences in anxiety, stress, and interpersonal/hostility between the yoga and attention-control groups over time. In addition, the dose of yoga (total minutes of yoga practiced during the study) was evaluated, but was not a significant covariate in any model.
Feasibility and Acceptability: Qualitative Findings
Three main themes regarding feasibility and acceptability arose from the data from the semi-structured exit interviews with study participants and their daily logs. Quotes from participants are presented to support and illustrate these themes. Participants also provided general suggestions for future yoga research for depression.
Theme 1- Feasibility: Barriers to participation
The first theme reflects how scheduling difficulties related to work and life responsibilities were the main barriers to participation in and completion of the study. Of the study participants who dropped out of the study, all of them cited work and home-life responsibilities as barriers to their participation in the study. They echoed one woman’s statement about the busy nature of her life, when she stated “I am a grad student, I’ve got a pretty demanding job, and then there are other life demands … it’s just hard to do everything.” Many completers of the yoga intervention suggested that their busy, fast-paced lifestyle became a vicious cycle of contributing to stress and depression while also preventing them from participating in self-care. One participant stated that, due to her busy life, she “just didn’t have anything in me to do much of anything” on the days she was to do the home practices. However, for some women, coming to terms with their limitations was an essential part of the process of stopping the negative self-judgments typical in depression, as described by one participant: “At first, I was feeling bad that I couldn’t do the whole practice all the time… [but I learned that] it’s not about how much you didn’t do, it’s about how it helped you today… I really took that to heart.”
Theme 2- Acceptability of yoga and health-education: Decreased depression
The second theme reflects how participants in both the yoga and attention-control group reported an improved mood during their time in the study, which supported acceptability of the intervention and control activity. In the exit interviews, participants in both the health-education (attention-control) and the yoga groups consistently reported a sense of decreased depression over the course of the study. However, the reasons cited for this perceived decrease in depression were different between the two groups. Those in the attention-control group stated they had decreased depression because they felt increased motivation to care for themselves combined with active social support. Participants in the attention-control group consistently suggested that they felt less depressed because they had started to care for themselves and that they benefitted from talking with others in the attention-control group. One participant suggested that “signing up for the study refocused my need to take care of myself,” signifying the association between self-care and decreased depression. In contrast, those in the yoga group felt yoga helped their mood because it provided a coping strategy to deal with persistent negative thoughts about stress in their lives while also increasing a sense of connectedness to themselves and to others around them. For example, one participant commented that learning how to be mindful of the breath and body through yoga helped her break patterns of self-judging thoughts: “I normally look at all the things I didn’t get done or do perfectly … but in the class I learned to focus and be pleased with just doing a little something for me.” Participants repeatedly commented that they learned through yoga to manage their thoughts, by “de-stressing” and letting “thoughts go by without obsessing.” Another participant suggested that she was “more alert” to herself, thus enhancing her personal confidence with life in general. Many participants suggested that yoga was empowering; this is elucidated in one participant’s statement that, after a few weeks of yoga practice, she had a general “feeling of being more capable” of doing yoga and other activities of daily life. Participants in the yoga group suggested that they also felt decreased depression because they gained a profound sense of “connectedness” with others in their classes. One participant expressed her feelings about the benefit of a social interaction through yoga that transcended conversation: “shared consciousness was there, when everyone was together. The shared centeredness is very powerful, it makes you feel a feeling of connectedness with everything …even by just breathing together.”
Theme 3- Feasibility and acceptability of yoga: Motivators for practice
The third theme reflects how various motivators affected the feasibility and acceptability of the yoga intervention. When questioned about their experiences with home practice in the yoga intervention and the likelihood of continuing with their yoga practice, all of the participants discussed the topic of motivation in various forms. The DVD, class handouts, and daily logs were described as partial motivators. The gained experience of an improved mood and enhanced self-confidence were also described as motivators and key factors, particularly when participants considered how to incorporate yoga into their lives after the end of the study.
As tools to facilitate home yoga practice, the DVD and weekly yoga class handouts were motivators for some, but not all. When asked about the value of these tools, participants had mixed reviews. A few loved the DVD and felt that it was very motivating for home practice during the study and could be helpful in the future. One participant reported: “Both class and DVD gave me something different… it’s wonderful to see a woman who is just a normal looking woman who is doing yoga. That was very encouraging to me.” Some participants used certain sections of the DVD that they found appealing, typically the warm-up, breathing, and meditation chapters. The majority of participants, however, preferred to use only the handouts of poses from class each week, stating that they had gained confidence with the routine that they had learned in the safety of their group class. One participant said “I stuck to the comfort zone of the exercises that I learned in class” and another suggested that “I felt like what I learned during the weekly class was the best to think about.”
With regards to the feasibility of the home yoga aspect of the intervention, many commented that the daily log acted as a motivator to help them adhere to the recommended practice. One participant stated: “Sometimes I didn’t want to get out of bed … but I would get out of bed and breathe and stretch because I knew I had to fill out that log!” Another suggested that the home practice and daily logs helped “add structure to [her] days.” This log occasionally triggered a sense of guilt in some participants who felt they had not completed their “homework.” Nonetheless, many participants stated that they appreciated the sense of responsibility that came with having a log to fill out. One participant succinctly summarized this feeling with the following statement: “[I needed] that push and that accountability to do it; that sheet of paper was there and I said ‘okay, I need to write something down.’”
When directly asked by the investigator about the most important motivation for sticking with yoga practice, the most common answer was that participants felt better after yoga practice thus reinforcing their motivation to continue with the protocol. One participant said that she would stick with her home yoga practice because she “would feel better afterwards, and that encouragement helped.” Another participant echoed this sentiment with the following comment: “Now, since I’m kind of on a roll and gotten used to doing it every day or almost every day, when I don’t do it, I feel it in my body and my emotions. That’s kind of motivation itself.”
Participants’ suggestions for feasibility of future studies
When asked by the investigator about what they liked the least in the study and for suggestions for designing future research studies, a few participants had ideas to share. First, one participant wished for a longer time-frame of the study, beyond 8 weeks, saying:
When you’re doing something consistently for a long time, it sinks in more. The first two to three weeks you’re honestly not there yet, you don’t grasp it yet. But by then, it’s like you’re at mid-way point and you’re almost done and [the routine is] not really set in stone.
Second, some participants wished for less “homework” and more frequent group classes. Despite a general dislike of having to write in a log, participants consistently stated that future research studies should continue to include the combination of group classes and home practice. One participant reflected positively about this combination, saying “it wasn’t just ‘here’s a class’ or just ‘here’s a DVD,’ but the combination of the two. I was really glad that all of that was incorporated in [the study].” Fourth and finally, a number of participants suggested that a “buddy system” or “accountability partners,” in the form of participant-to-participant communication outside of class, could have been helpful for encouraging adherence to home practice during the study as well as after the study was completed.
Discussion
This study provides support for the feasibility and acceptability of yoga as a complementary therapy for women with depression, as evidenced through examination of recruitment, retention, adherence, and the results of the quantitative and qualitative data. In addition, the findings suggest that, despite the fact that the yoga group and attention-control group had the same degree of decreased depression over time, yoga appears to be uniquely helpful for decreasing ruminations.
Recruitment, Retention, Acceptability, and Feasibility
Ease of recruitment for the study itself is an important indicator of acceptability of yoga by women with depression. Despite our initial concerns that the common depressive symptom of anhedonia would be a barrier to women volunteering for a study, we were able to garner the interest of many women with MDD and moderate to severe depressive symptoms in a 4-month time span. Referrals from psychotherapists and psychiatrists were an important aspect of the recruitment process. In addition, we were able to recruit a racially and ethnically diverse group of participants that mirrored the demographics of the recruitment area. The most effective recruitment strategies were the use of word-of-mouth and placement of brochures at healthcare provider offices. There were only two women who declined to participate in the study after the initial telephone screening, citing schedule issues. However, there were four additional women who were “no shows” to the next screening and consent visit. These women had slightly higher depression scores than those who initially declined the study. Future research is warranted to determine whether “no shows” are too depressed and anhedonic to meet the investigator for the consent visit or whether there are other factors involved.
The retention rate of the yoga group was much higher than that of the control group. Unfortunately, it is difficult to compare reasons for the differing retention rates because many of the dropouts in the control group were lost to follow-up. The only dropout from the control group who participated in an interview suggested that she could not continue due to schedule conflicts, which is consistent with the reasons in the yoga group. Attrition is often high in control groups, but the attention-control group was designed based upon the literature supporting health education sessions as reasonable for retention (Davis, Broome, & Cox, 2002; Gross et al., 2010; Innes, 2009; Lengacher et al., 2001; Mather et al., 2002; Trivedi et al., 2006; Williams et al., 2010). In an attempt to gain insight into potential mediators for this attrition, we evaluated baseline information about the dropouts. Interestingly, more study completers reported recent major stressful life changes at baseline than did those who dropped out of the study; this is the opposite scenario of what we would have expected, given that stressful life events are often associated with worsened depression and increased anhedonia (Kendler, Thornton, & Gardner, 2000). Future research with a larger sample size is warranted for evaluating differences in and the impact of retention rates. Strategies for improving retention rates, such as those that enhance how women cope with scheduling difficulties, should be evaluated in future studies.
The qualitative findings support the acceptability of the yoga intervention for depression. All of the women who participated in the yoga group reported that they enjoyed participating in the yoga classes and they felt that yoga was effective for decreasing their depression and associated symptoms. As the study progressed, participants gained the felt experience of the benefits of yoga that served as an important internal motivator for their continued participation. During the interviews and in their logs, participants reflected on an increased awareness of the enjoyable outcomes of yoga, such as feelings of physical and mental wellness (Vealey, 2007). Research suggests that personal positive experiences contribute to self-efficacy, whereby participants feel more motivated for and capable of participating in a yoga routine, thereby reinforcing future practice (Whaley, 2004).
In terms of the feasibility of the home practice aspect of the yoga intervention, daily life stresses, in the form of family, work and/or school responsibilities, were a barrier to adherence to the full recommended dose of yoga. This is consistent with the literature that suggests that these responsibilities often strain depressed women’s abilities to prioritize self-care activities such as yoga and may affect well-being (Cotter & Lachman, 2010; Keita, 2007; Nolen-Hoeksema, 2006). Although several participants felt that it was difficult to find time for themselves to practice yoga at home, many reported that they learned to have realistic goals and expectations of themselves for their yoga practice; these realistic goals seemed to translate into a realistic view of their ability to deal with the world around them, which may be beneficial for their long-term engagement in self-care (Son, Kerstetter, Mowen, & Payne, 2009). Any psychosocial intervention requires time and effort on the part of the individual, which may continue to be a challenge in the use of yoga for depression. Nonetheless, the dose of home yoga practice received by participants in this study was not a significant covariate in our data analysis. In other words, individuals with more time in home practice did not necessarily have a greater decrease in depression or ruminations. This finding is interesting, particularly because it is unknown what the minimum effective “dose” of yoga may be and whether it includes home practice versus group classes (Uebelacker et al., 2010). Participants in our study consistently stated that they felt the most noteworthy benefit from the group classes and experienced more barriers to home practice, so future researchers may wish to study these factors more fully in a long-term study. In addition, as suggested by multiple participants, future researchers may wish to evaluate the role of a “buddy system” for long-term adherence, which is a social approach for relapse prevention (Lox, Martin, & Petruzzello, 2006).
The findings from the qualitative data supported the use of behavioral strategies to facilitate adherence to the home yoga practice (i.e., the class handouts, the DVD, daily logs). The majority of the yoga group participants reported using class handouts rather than the DVD to guide their home practice, citing an enhanced sense of confidence about and competence with yoga. It is not surprising that participants tended to choose a home practice that mirrored their group class practice because a sense of confidence and competence has been shown to help individuals maintain consistency with an intervention, particularly when combined with a positive social environment and the reinforcement with positive affective states (Whaley, 2004). The participants also cited the daily yoga logs as a motivator for regular practice during the study itself. The use of logs may have contributed to the foundational skill of self-awareness. This tool for gaining awareness of thoughts and feelings about mood and participation in an intervention has been shown to enhance self-regulation and adherence to interventions (Vealey, 2007). Although participants did not always fully complete the logs and many participants expressed frustration with keeping up with them, the logs may have been a relevant self-monitoring strategy. The literature suggests that, even if a log is incomplete, it can be helpful for providing an avenue for self-evaluation and for reinforcing consistency with the intervention (Lox et al., 2006). By writing in the column in the log about her mood, the participant may have been able to see clearly whether or not participating in yoga was beneficial. Considering this, future researchers may wish to continue to use logs, or a similar method, to help participants adhere to an intervention.
Unique Effect of Yoga: Trend in Decreased Rumination
The study supports the need for continued large-scale research studies to evaluate the effects of yoga on depression as compared to an active control group. Participants in both groups had a significant decrease in depression scores over time, such that the mean depression score decreased from a “moderately severe” level to a “minimal” level of depression in 8 weeks. Although the attention-control group had a similar decrease in depression over time, the yoga group had a unique trend towards decreased ruminations, when controlling for baseline stress. At each time point during the study, the yoga group had a greater reduction in rumination scores compared to the control, as seen in Figure 2. This suggests that, perhaps given more time in the intervention, the yoga group may have ultimately had a more significantly decreased rumination score. Data from the qualitative interviews support this, as many participants verbalized a desire for the intervention to be a bit longer to help them fully establish yoga in their routine and feel more confident with their yoga abilities.
The quantitative and qualitative findings suggest that there may be a few reasons that account for decreased depression in the attention-control group without a decrease in ruminations. The yoga and the attention-control groups shared a few similar aspects, in that they both required women to voluntarily engage in an activity requiring participants to get out of the house, that involved social support, and that encouraged self-care. These factors may have been important enough to enact change in all participants’ perception of depression but not necessarily ruminations in the attention-control group. First, volunteer bias may have played an important role in decreasing depression because, as many participants in the attention-control group reported, simply volunteering for a research study was a motivator for self-care. Second, the simple act of bringing women with depression together may be an intervention in itself. Studies suggest that the social environment plays a key role in mental health (Curley, Jensen, Mashoodh, & Champagne, 2011; Luyten, Blatt, Van Houdenhove, & Corveleyn, 2006). Indeed, many of the women in the attention-control group reported that they benefitted from talking with others in the group and hearing about others’ experiences, conceivably similar to the value of therapeutic group modalities (Cuijpers et al., 2010). This may be a key difference between the groups, however, because the participants in the yoga group often discussed how connectedness occurred transcendent of dialogue. In fact, connectedness, or a general sense of self in the world, has been shown to be a more powerful and enduring mediator for decreasing depression than direct social support (Deary, Roche, Plotkin, & Zahourek, 2011; Segrin & Rynes, 2009; Uebelacker, Tremont et al., 2010; Williams & Renee, 2006). Future researchers may wish to include measures of social connectedness to more closely evaluate this potential difference. Third, two women in the attention-control group encouraged each other to join a gym; physical activity has been shown to significantly improve the mood, so this simple change in lifestyle in two out of the six women in the attention-control group may be partly responsible for the change in depression level (Mead et al., 2009). We can only speculate about the impact of these factors on our results; to increase power to detect changes between groups, future large-scale studies should evaluate these factors with a larger sample size.
Study Limitations
Generalizability of this study is limited for a number of reasons. First, the nature of a pilot study is a small sample size, which places limits upon quantitative methodologies and generalizability. Second, as with any study that requires volunteer participation, volunteer bias may have occurred due to convenience sampling, such that the sample may include those who already intended to enact changes for self-care and mental wellness. Third, attrition rates were relatively high in the attention-control group as compared to the yoga group, despite multiple strategies to retain participants such as weekly telephone calls to address barriers to participation. We were unable to include dropouts in the quantitative analysis because most dropped out before receiving any of the intervention and completing any study instruments beyond baseline. Finally, beyond the exit interview, we did not engage in long-term follow-up of participants, which may have provided additional information about the feasibility and acceptability of long-term yoga practice for women with depression. Previous studies have found multiple barriers to long-term continuation of yoga (Alexander, Taylor, Innes, Kulbok, & Selfe, 2008; Atkinson & Permuth-Levine, 2009). A longer study with depressed women would be beneficial for evaluating what strategies for maintenance of yoga practice are most helpful and whether the positive benefits of yoga practice are sustained over time.
Conclusion
The results of this study suggest that yoga is acceptable to and feasible for this population. Despite the small sample size, there was a trend towards decreased ruminations in the yoga group only, which may provide insight into one possible mechanism for yoga’s effect on depression. Further research is warranted to evaluate if, given enough time and with a larger sample size, the effect of the decreased ruminations could cause a more significant decrease in depression in the yoga group. Qualitative findings provide support for the feasibility, acceptability, and benefits of the use of yoga with depressed women. This pilot study was designed carefully to address multiple methodological limitations of previous studies of yoga for depression and supports the need for replication in future large-scale research into yoga as a complementary therapy for women with depression.
Acknowledgments
This publication was made possible by grant number 5-T32-AT000052 from the National Center for Complementary and Alternative Medicine (NCCAM). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCCAM. The authors thank all of the members of the study team, particularly Mindy Loiselle and Robert Goldschmidt (certified yoga teachers), Debbie Seegers, Karyn Schultz, and Kalay Naidoo (registered nurses), and Joan Plotkin-Han (on-call psychiatrist). We thank Amy Weintraub for the use of her LifeForce Yoga DVD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agar M. Speaking of ethnography. Thousand Oaks, CA: Sage Publications, Inc; 1986. [Google Scholar]
- Alexander GK, Taylor AG, Innes KE, Kulbok P, Selfe TK. Contextualizing the effects of yoga therapy on diabetes management: A review of the social determinants of physical activity. Family & Community Health. 2008;31(3):228–239. doi: 10.1097/01.FCH.0000324480.40459.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: Fourth edition, text revision (DSM-IV-TR) 4th ed. Arlington, VA: American Psychiatric Association; 2000. [Google Scholar]
- Atkinson NL, Permuth-Levine R. Benefits, barriers, and cues to action of yoga practice: A focus group approach. American Journal of Health Behavior. 2009;33(1):3–14. doi: 10.5993/ajhb.33.1.1. [DOI] [PubMed] [Google Scholar]
- Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United states, 2007. National Health Statistics Reports. 2009;(12):1–23. [PubMed] [Google Scholar]
- Beal CC, Stuifbergen A, Volker D, Becker H. Women's experiences as members of attention control and experimental intervention groups in a randomized controlled trial. Canadian Journal of Nursing Research. 2009;41(4):16–31. [PubMed] [Google Scholar]
- Bennett S, Weintraub A, Khalsa S. Initial evaluation of the LifeForce yoga program as a therapeutic intervention for depression. International Journal of Yoga Therapy. 2008;28:49–57. [Google Scholar]
- Benson H. The relaxation response. New York: Avon Books; 1975. [Google Scholar]
- Birdee GS, Legedza AT, Saper RB, Bertisch SM, Eisenberg DM, Phillips RS. Characteristics of yoga users: Results of a national survey. Journal of General Internal Medicine. 2008;23(10):1653–1658. doi: 10.1007/s11606-008-0735-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branchi I, Schmidt M. In search of the biological basis of mood disorders: Exploring out of the mainstream. Psychoneuroendocrinology. 2011;36(3):305–307. doi: 10.1016/j.psyneuen.2010.12.013. [DOI] [PubMed] [Google Scholar]
- Broota A, Dhir R. Efficacy of two relaxation techniques in depression. India: Journal of Personality and Clinical Studies; 1990. [Google Scholar]
- Brown RP, Gerbarg PL. Sudarshan kriya yogic breathing in the treatment of stress, anxiety, and depression. part II--clinical applications and guidelines. Journal of Alternative & Complementary Medicine. 2005a;11(4):711–717. doi: 10.1089/acm.2005.11.711. [DOI] [PubMed] [Google Scholar]
- Brown RP, Gerbarg PL. Sudarshan kriya yogic breathing in the treatment of stress, anxiety, and depression: Part I-neurophysiologic model.[erratum appears in J altern complement med. 2005 apr;11(2):383–4] Journal of Alternative & Complementary Medicine. 2005b;11(1):189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- Brown RP, Gerbarg PL. Yoga breathing, meditation, and longevity. Annals of the New York Academy of Sciences. 2009;1172:54–62. doi: 10.1111/j.1749-6632.2009.04394.x. [DOI] [PubMed] [Google Scholar]
- Burwell RA, Shirk SR. Subtypes of rumination in adolescence: Associations between brooding, reflection, depressive symptoms, and coping. Journal of Clinical Child and Adolescent Psychology : The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53. 2007;36(1):56–65. doi: 10.1080/15374410709336568. [DOI] [PubMed] [Google Scholar]
- Butler LD, Waelde LC, Hastings TA, Chen XH, Symons B, Marshall J, Spiegel D. Meditation with yoga, group therapy with hypnosis, and psychoeducation for long-term depressed mood: A randomized pilot trial. Journal of Clinical Psychology. 2008;64(7):806–820. doi: 10.1002/jclp.20496. [DOI] [PubMed] [Google Scholar]
- Cohen M, Kahn D, Steeves R. Hermeneutic phenomenological research: A practical guide for nurse researchers. Thousand Oaks, CA: Sage Publications, Inc; 2000. [Google Scholar]
- Cohen S. Perceived stress scale. 1994 Retrieved February 2, 2010, from www.mindgarden.com/docs/PerceivedStressScale.pdf.
- Cohen S, Williamson G. Perceived stress in a probability sample of the united states. In: Oskamp S, Spacapan S, editors. The social psychology of health. Thousand Oaks, CA: Sage Publications, Inc; 1988. pp. 31–67. [Google Scholar]
- Cohen S, Tyrrell DA, Smith AP. Negative life events, perceived stress, negative affect, and susceptibility to the common cold. Journal of Personality and Social Psychology. 1993;64(1):131–140. doi: 10.1037//0022-3514.64.1.131. [DOI] [PubMed] [Google Scholar]
- Conway M, Csank PAR, Holm SL, Blake CK. On assessing individual differences in rumination on sadness. Journal of Personality Assessment. 2000;75(3):404–425. doi: 10.1207/S15327752JPA7503_04. [DOI] [PubMed] [Google Scholar]
- Cotter KA, Lachman ME. No strain, no gain: Psychosocial predictors of physical activity across the adult lifespan. Journal of Physical Activity and Health. 2010;(7):584–594. doi: 10.1123/jpah.7.5.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane C, Barnhofer T, Williams JM. Reflection, brooding, and suicidality: A preliminary study of different types of rumination in individuals with a history of major depression. British Journal of Clinical Psychology. 2007;46:497–504. doi: 10.1348/014466507X230895. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, Schuurmans J, van Oppen P, Hollon SD, Andersson G. Psychotherapy for chronic major depression and dysthymia: A meta-analysis. Clinical Psychology Review. 2010;30(1):51–62. doi: 10.1016/j.cpr.2009.09.003. [DOI] [PubMed] [Google Scholar]
- Curley JP, Jensen CL, Mashoodh R, Champagne FA. Social influences on neurobiology and behavior: Epigenetic effects during development. Psychoneuroendocrinology. 2011;36(3):352–371. doi: 10.1016/j.psyneuen.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis L, Broome M, Cox R. Maximizing retention in community-based clinical trials. Journal of Nursing Scholarship. 2002;34(1):47–53. doi: 10.1111/j.1547-5069.2002.00047.x. [DOI] [PubMed] [Google Scholar]
- Deary L, Roche J, Plotkin K, Zahourek R. Intentionality and hatha yoga: An exploration of the theory of intentionality, the matrix of healing- a growth model. Holistic Nursing Practice. 2011;25(5):246–253. doi: 10.1097/HNP.0b013e31822a02e0. [DOI] [PubMed] [Google Scholar]
- Derogatis L, Melisaratos N. The brief symptom inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Desikachar K, Bragdon L, Bossart C. The yoga of healing: Exploring yoga's holistic model for health and well-being. International Journal of Yoga Therapy. 2005;15:17–39. [Google Scholar]
- Doyle L, Brady A, Byrne G. An overview of mixed-methods research. Journal of Nursing Research. 2009;14(2):175–185. [Google Scholar]
- Weintraub A, Duncan D. LifeForce yoga to beat the blues: Level 1. Pennsauken, NJ: Disc Makers; 2007. (Producer) (Director) [Video/DVD] [Google Scholar]
- Gross CR, Kreitzer MJ, Thomas W, Reilly-Spong M, Cramer-Bornemann M, Nyman JA, Ibrahim HN. Mindfulness-based stress reduction for solid organ transplant recipients: A randomized controlled trial. Alternative Therapies in Health & Medicine. 2010;16(5):30–38. [PMC free article] [PubMed] [Google Scholar]
- Halbreich U, Kahn LS. Atypical depression, somatic depression and anxious depression in women: Are they gender-preferred phenotypes? Journal of Affective Disorders. 2007;102(1–3):245–258. doi: 10.1016/j.jad.2006.09.023. [DOI] [PubMed] [Google Scholar]
- Hauenstein EJ. A nursing practice paradigm for depressed rural women: Theoretical basis. Archives of Psychiatric Nursing. 1996;10(5):283–292. doi: 10.1016/s0883-9417(96)80037-9. [DOI] [PubMed] [Google Scholar]
- Hewitt PL, Flett GL, Mosher SW. The perceived stress scale: Factor structure and relation to depression symptoms in a psychiatric sample. Journal of Psychopathology and Behavioral Assessment. 1992;14(3):247–257. [Google Scholar]
- Innes KE. Abstracts from the North American Research Conference on Complementary and Integrative Medicine. May 12–15, 2009; Minneapolis, MN. Journal of Alternative and Complementary Medicine (New York, N.Y.); 2009. pp. 446–458. [DOI] [PubMed] [Google Scholar]
- Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of sudarshan kriya yoga (SKY) in melancholia: A randomized comparison with electroconvulsive therapy (ECT) and imipramine. Journal of Affective Disorders. 2000;57(1–3):255–259. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]
- Keita GP. Psychosocial and cultural contributions to depression in women: Considerations for women midlife and beyond. Journal of Managed Care Pharmacy: JMCP. 2007;13(9):S12–S15. doi: 10.18553/jmcp.2007.13.9-a.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Gardner CO. Stressful life events and previous episodes in the etiology of major depression in women: An evaluation of the "kindling" hypothesis. The American Journal of Psychiatry. 2000;157(8):1243–1251. doi: 10.1176/appi.ajp.157.8.1243. [DOI] [PubMed] [Google Scholar]
- Kessler R, Berglund P, Demler O, Jin R, Koretz D, Merikangas K, Wang P. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) Journal of the American Medical Association. 2003;289(3):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kinser PA, Goehler LE, Taylor AG. How might yoga help depression? A neurobiological perspective. EXPLORE: The Journal of Science and Healing. 2012;8(2):118–126. doi: 10.1016/j.explore.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkwood G, Rampes H, Tuffrey V, Richardson J, Pilkington K. Yoga for anxiety: A systematic review of the research evidence. British Journal of Sports Medicine. 2005;39(12):884–891. doi: 10.1136/bjsm.2005.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer L, Williams J. MOS short-form general health survey. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafrance MN, Stoppard JM. Constructing a non-depressed self: Women's accounts of recovery from depression. Feminism & Psychology. 2006;16(3):307–325. doi: [Google Scholar]
- Lengacher CA, Gonzalez LL, Giuliano R, Bennett MP, Cox CE, Reintgen DS. The process of clinical trials: A model for successful clinical trial participation. Oncology Nursing Forum. 2001;28:1115–1120. [PubMed] [Google Scholar]
- Lindquist R, Wyman JF, Talley K, Findorff MJ, Gross CR. Design of control-group conditions in clinical trials of behavioral interventions. Journal of Nursing Scholarship. 2007;39(3):214–221. doi: 10.1111/j.1547-5069.2007.00171.x. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Hutti MH. Readability: An important issue impacting healthcare for women with postpartum depression. MCN: The American Journal of Maternal Child Nursing. 2006;31(6):350–355. doi: 10.1097/00005721-200611000-00004. [DOI] [PubMed] [Google Scholar]
- Lopez CM, Driscoll KA, Kistner JA. Sex differences and response styles: Subtypes of rumination and associations with depressive symptoms. Journal of Clinical Child and Adolescent Psychology : The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53. 2009;38(1):27–35. doi: 10.1080/15374410802575412. [DOI] [PubMed] [Google Scholar]
- Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: Sensitivity to change of the patient health questionnaire (PHQ-9) Journal of Affective Disorders. 2004;81(1):61–66. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- Lox CL, Martin KA, Petruzzello SJ. The psychology of exercise: Integrating theory and practice. 2nd ed. Scottsdale, AZ: Holcomb Hathaway; 2006. Physical activity interventions. pp. 147-18. [Google Scholar]
- Luyten P, Blatt SJ, Van Houdenhove B, Corveleyn J. Depression research and treatment: Are we skating to where the puck is going to be? Clinical Psychology Review. 2006;26(8):985–999. doi: 10.1016/j.cpr.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, Tkach C. The consequences of dysphoric rumination. In: Papageorgiou C, Wells A, editors. Depressive rumination: Nature, theory, and treatment () Chicester, England: John Wiley & Sons Ltd; 2004. [Google Scholar]
- Marcus SM, Kerber KB, Rush AJ, Wisniewski SR, Nierenberg A, Balasubramani GK, Trivedi MH. Sex differences in depression symptoms in treatment-seeking adults: Confirmatory analyses from the sequenced treatment alternatives to relieve depression study. Comprehensive Psychiatry. 2008;49(3):238–246. doi: 10.1016/j.comppsych.2007.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mather A, Rodriguez C, Guthrie M, McHarg A, Reid I, McMurdo M. Effects of exercise on depressive symptoms in older adults with poorly responsive depressive disorder: Randomised controlled trial. The British Journal of Psychiatry. 2002;180(5):411–415. doi: 10.1192/bjp.180.5.411. [DOI] [PubMed] [Google Scholar]
- Mathew SJ, Charney DS. Publication bias and the efficacy of antidepressants. American Journal of Psychiatry. 2009;166(2):140–145. doi: 10.1176/appi.ajp.2008.08071102. [DOI] [PubMed] [Google Scholar]
- Mead G, Morley W, Campbell P, Greig C, McMurdo M, Lawlor D. Exercise for depression. Cochrane Database of Systematic Reviews. 2009;3 doi: 10.1002/14651858.CD004366.pub4. CD004366. [DOI] [PubMed] [Google Scholar]
- Morrison R, O'Connor R. A systematic review of the relationship between rumination and suicidality. Suicide and Life-Threatening Behavior. 2008;38:523–538. doi: 10.1521/suli.2008.38.5.523. [DOI] [PubMed] [Google Scholar]
- National Center for Complementary and Alternative Medicine (NCCAM) About yoga. 2010 Retrieved 9/26, 2010, from http://nccam.nih.gov/health/yoga/
- Nolen-Hoeksema S. The etiology of gender differences in depression. In: Keita GP, editor. Understanding depression in women: Applying empirical research to practice and policy. Washington, DC US: American Psychological Association; 2006. pp. 9–43. [Google Scholar]
- Nolen-Hoeksema S, Hilt LM. Gender differences in depression. In: Hammen CL, editor. Handbook of depression. 2nd ed. New York, NY US: Guilford Press; 2009. pp. 386–404. [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3(5):400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Pigott H, Leventhal A, Alter G, Boren J. Efficay and effectiveness of antidepressants: Current status of research. Psychotherapy and Psychosomatics. 2010;79:267–279. doi: 10.1159/000318293. [DOI] [PubMed] [Google Scholar]
- Pilkington K, Kirkwood G, Rampes H, Richardson J. Yoga for depression: The research evidence. Journal of Affective Disorders. 2005;89(1–3):13–24. doi: 10.1016/j.jad.2005.08.013. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Whatever happened to qualitative description? Research in Nursing and Health. 2000;23:334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Segrin C, Rynes KN. The mediating role of positive relations with others in associations between depressive symptoms, social skills, and perceived stress. Journal of Research in Personality. 2009;43(6):962–971. [Google Scholar]
- Sharma VK, Das S, Mondal S, Goswampi U, Gandhi A. Effect of sahaj yoga on depressive disorders. Indian Journal of Physiology & Pharmacology. 2005;49(4):462–468. [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- Smith JM, Alloy LB. A roadmap to rumination: A review of the definition, assessment, and conceptualization of this multifaceted construct. Clinical Psychology Review. 2009;29(2):116–128. doi: 10.1016/j.cpr.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son J, Kerstetter D, Mowen A, Payne L. Global self-regulation and outcome expectations: Influences on constraint self-regulation and physical activity. Journal of Aging and Physical Activity. 2009;17:307–326. doi: 10.1123/japa.17.3.307. [DOI] [PubMed] [Google Scholar]
- Sparrowe L, Walden P. The woman's book of yoga and health: A lifelong guide to wellness. Boston, MA: Shambala; 2002. [Google Scholar]
- Spielberger C, Gorsuch R, Lushene R. State-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Spielberger CD. State-trait anxiety inventory (STAI.) Menlo Park, CA: Mind Garden; 1983. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, and the Patient Health Questionnaire Primary Care Study Group Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA: The Journal of the American Medical Association. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Street LL, Luoma JB. Control groups in psychosocial intervention research: Ethical and methodological issues. Ethics & behavior. 2002;12(1):1–30. doi: 10.1207/S15327019EB1201_1. [DOI] [PubMed] [Google Scholar]
- Taylor A, Goehler L, Galper D, Innes K, Bourguignon C. Top-down and bottom-up mechanisms in mind-body medicine: Development of an integrative framework for psychophysiological research. Explore. 2010;6:29–41. doi: 10.1016/j.explore.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilton SR. Review of the state-trait anxiety inventory (STAI) NewsNotes. 2008;48(2) June 2, 2010. [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27(3):247–259. [Google Scholar]
- Trivedi MH, Greer TL, Grannemann BD, Church TS, Galper DI, Sunderajan P, Carmody TJ. TREAD: Treatment with exercise augmentation for depression: Study rationale and design. Clinical Trials. 2006;3(3):291–305. doi: 10.1191/1740774506cn151oa. [DOI] [PubMed] [Google Scholar]
- Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med. 2008;358(3):252–260. doi: 10.1056/NEJMsa065779. [DOI] [PubMed] [Google Scholar]
- Uebelacker LA, Epstein-Lubow G, Gaudiano BA, Tremont G, Battle CL, Miller IW. Hatha yoga for depression: Critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. Journal of Psychiatric Practice. 2010;16(1):22–33. doi: 10.1097/01.pra.0000367775.88388.96. [DOI] [PubMed] [Google Scholar]
- Uebelacker LA, Tremont G, Epstein-Lubow G, Gaudiano BA, Gillette T, Kalibatseva Z, Miller IW. Open trial of vinyasa yoga for persistently depressed individuals: Evidence of feasibility and acceptability. Behavior Modification. 2010;34(3):247–264. doi: 10.1177/0145445510368845. [DOI] [PubMed] [Google Scholar]
- Vealey RS. Mental skills training in sport. In: Tenenbaum G, Eklund RC, editors. Handbook of sport psychology. 3rd ed. Hoboken, NJ: John Wiley & Sons; 2007. pp. 287–309. [Google Scholar]
- Weinstein N, Brown KW, Ryan RM. A multi-method examination of the effects of mindfulness on stress attribution, coping, and emotional well-being. Journal of Research in Personality. 2009;43(3):374–385. [Google Scholar]
- Weintraub A. Yoga for depression: A compassionate guide to relieve suffering through yoga. New York, NY: Broadway Books; 2004. [Google Scholar]
- Whaley DE. Seeing isn't always believing: Self-perceptions and physical activity behaviors in adults. In: Weiss MR, editor. Developmental sport and exercise psychology: A lifespan perspective. Morgantown, WV: Fitness Information Technology; 2004. pp. 289–311. [Google Scholar]
- Williams KLG, Renee V. Predicting depression and self-esteem from social connectedness, support, and competence. Journal of Social & Clinical Psychology. 2006;25(8):855–874. [Google Scholar]
- Williams JM, Russell IT, Crane C, Russell D, Whitaker CJ, Duggan DS, Silverton S. Staying well after depression: Trial design and protocol. BMC Psychiatry. 2010;10:23–23. doi: 10.1186/1471-244X-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]