Abstract
Background:
To review a single-surgeon series of 616 athletic patients with anterior cruciate ligament reconstructions in order to evaluate the relationship between the timing of the reconstruction and the incidence of meniscal and chondral injuries.
Methods:
Six group of patients were categorized based on the time interval from their injury to surgery in the following manner: <3 months, 3-6 months, 6-9 months, 9-18 months, 18-36 months, and >36 months. The presence of meniscal tears was documented and chondral pathology was scored based on the Outerbridge classification.
Results:
Incidence of medial meniscus tear was significantly higher in patients undergoing reconstruction after 3 months from their injury (P = 0.032). The opportunity of patients with chondral pathology was recorded to be significantly higher in the groups operated on after 6 months from their injuries time (P = 0.008).
Conclusions:
Considering the effect of time on the rate of having meniscus injury and chondral pathology, reducing the time between the injury and surgery could improve the long-term health outcomes in this population.
Keywords: Chondral injury, ligament reconstruction, meniscal
INTRODUCTION
Every year, a large number of athletes experience knee trauma during training session and competitions. The anterior cruciate ligament (ACL) is the most commonly injured ligament of the knee, which mainly affects patients between 15 and 45 years of age.[1] ACL tear can be secondary to contact or non-contact traumatic situation. However, non-contact condition is more prevalent.[1–4] The ACL rupture can occur not only as a sole event but also in association with the rupture of meniscus and other ligaments.[5–7]
While the reconstruction of an injured ACL is considered as one of the most important procedures in sport injury, the optimal timing for the operation remains uncertain.[8] The safety and efficacy of the timing of the operation is controversial.[9] It appears that some consensus has been achieved on this issue with more surgeons waiting for the resolution of the acute hemarthrosis and the restoration of normal gait and range of movement before performing the surgery. It has also been suggested that any undue delay in surgery may lead to an increase in meniscal pathology such as experiencing recurrent episodes of giving ways, which could damage the articular surface.[10] The timing of surgery is of importance in counseling patients regarding the outcome of surgery and could be of particular interest while treating patients within a healthcare system with limited resources. It may also help surgeons to set priorities to their waiting list.
Recent long-term clinical researches have pointed out the increased risk of secondary meniscal damage and chondral lesion in patients with chronic ACL deficiency.[11–13] The present study, therefore, was designed to evaluate the association between ACL deficiency and its impact on meniscal and articular cartilage injury among groups of professional Iranian athletes and also to determine whether there is a correlation between the timing of reconstruction and these types of injuries.
METHODS
The present retrospective study was conducted on the medical records of 616 consecutive professional athletes gathered from referral hospitals between 1995 and 2009. Based on these records, the studied athletes had visited a single orthopedic surgeon (M.R.) because of knee injury and they were diagnosed with ACL tear, which was confirmed by magnetic resonance imaging (MRI) and arthroscopy. Athletes who were injured through a non-exercise mechanism such as experiencing a car accident, those experiencing concomitant ACL tear and tibia or fibula fracture, and those with a positive history of meniscal tear in the same leg were excluded.
The demographic information of the athletes including their age, gender, the injured leg, the sport in which they were involved, the duration between the time of injury and the surgery, and the injured ligaments was recorded in a questionnaire. The sport in which the athletes were involved consisted of soccer, wrestling, ball games (handball, volleyball, and basketball), martial arts, and others (ski, tennis, table tennis, running, badminton, skating, etc.). The duration between the time of injury and that of surgery was classified as <3 months (Group A), 3-6 months (Group B), 6-9 months (Group C), 9-18 months (Group D), 18-36 months (Group E), and >36 months (Group F). In cases with meniscal tear, the data on individuals with total meniscus injury regardless of their grade were entered and those with partial tears were excluded. Chondral lesion was graded based on the Outerbridge classification. Severity of chondral pathology was divided into two groups: Low graded groups (type 1 and 2) and high grade groups (type 3 and 4).
The data gathered from 616 athletes were entered and then analyzed using SPSS.[14] Chi-square test was used to evaluate the correlation between the presence of the meniscal tear, chondral damage, and the duration between the time of injury and that of surgery.
RESULTS
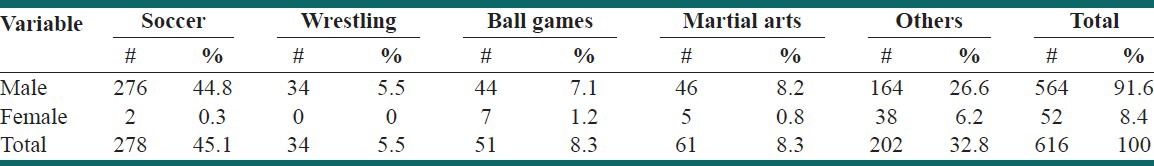
Overall, 564 (91.6%) out of a total of 616 athletes with ACL tear enrolled in this study were male. The mean age was 27.6 years, ranging from 13 to 60 years. Table 1 outlines the gender distribution and the sports in which the athletes were involved.
Table 1.
The frequency of athletes involved in different sports
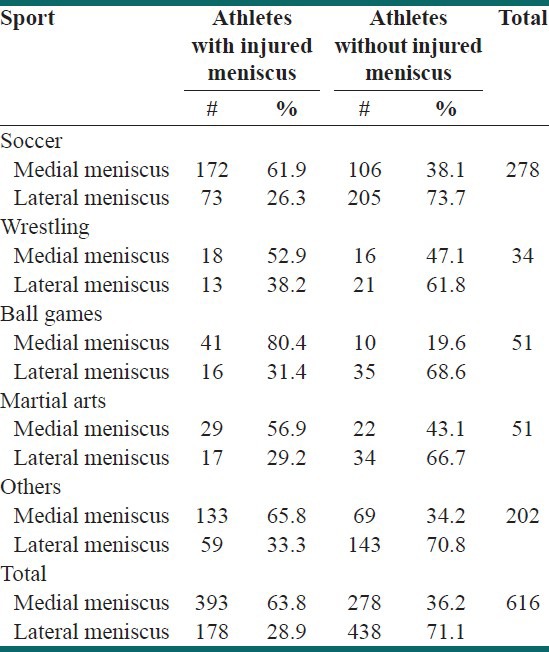
The single ACL injury was reported in 103 (16.7%) of the athletes. Table 2 shows the prevalence of meniscal damage in different sports. Medial meniscus injuries were more prevalent than lateral meniscus injuries among our professional athletes.
Table 2.
The incidence of medial and lateral meniscus injury in different sports
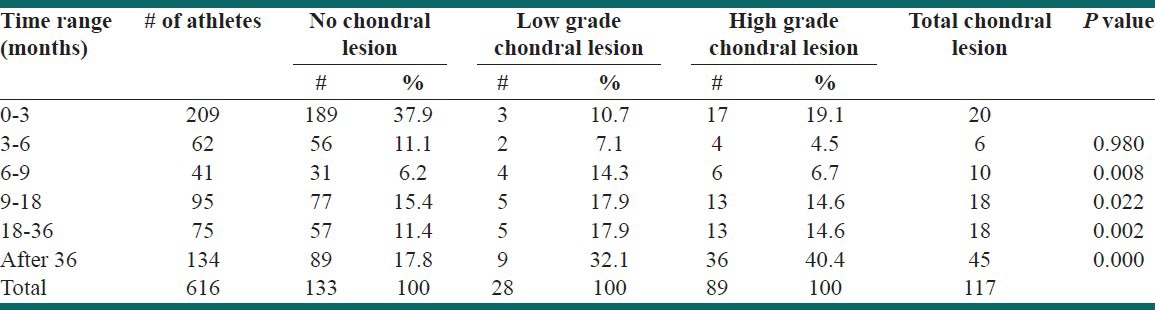
Also, 115 (18.7%) of athletes had chondral lesions. Among them, 104 (90%) athletes were male and 11 (9%) were female. There was no significant association between chondral pathology and sex of the athletes (Pv > 0.05). After an interval of 6 months, there was a significant increase in the prevalence of chondral lesions (Chi square test, P = 0.008) [Table 3].
Table 3.
The incidence and severity of chondral injuries among 6 groups
Based on what was reported and identification by MRI and arthroscopic findings, medial femoral condyl showed more prevalent chondral injuries (58.11%) than lateral side due to ACL deficiency.
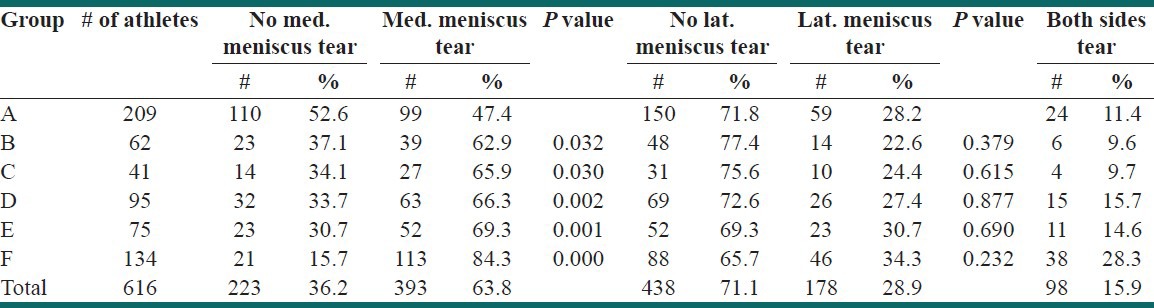
The prevalence of medial and lateral menisci tears within the groups is presented in Table 4. Considering the gathered information, the severity of tears in the medial meniscus increases over time since the injury.
Table 4.
Incidence of meniscal tears in the 6 groups
DISCUSSION
The present study was conducted on 616 athletes involved in different sports diagnosed with ACL tear based on the findings of clinical examination, MRI, and arthroscopy. The first strength of our study lies in the ability of examining a large group of patients by a single surgeon (M.R.). This is of great importance since the identification of pathology during knee arthroscopy has been shown to be related to the observer's capability.[15,16] About 16.7% of the studied population had ACL tear alone. We found an increased incidence of medial meniscal tears if the interval between the injury and reconstruction process was >3 months. A significant reduction was also found in the number of patients with normal articular surfaces after a delay of 6 months in the time of operation.
Prade et al., reported a relatively higher prevalence (44%) of single ACL tear among patients with acute knee injuries accompanied with hemarthrosis over a 90-days period.[14] Similarly, Frobell et al., reported the prevalence of ACL rupture in the general population to be about 30%, which was higher than previously described.[17] The difference between the diagnostic methods was considered as the main reason contributing to the discrepancies reported in these studies. In other words, while MRI was used to detect ACL tear in the abovementioned studies, our patients were diagnosed by clinical examination, MRI, and arthroscopic evaluations. The higher accuracy of the diagnostic procedures in our study accounts for the reduced number of single ACL tear and increased rate of combined meniscal and/or chondral injuries. The other possibility for having differences of the prevalence of single ACL tear in our population is on the basis of late referral of athletes to orthopedic surgeon. Some of athletes prefer to continue playing without considered their injury. It can extend their knee complications and decrease the rate of single ACL tear.
Based on our findings, there was an association between delayed reconstruction and an increased incidence of medial meniscus tear and chondral pathology after 3 and 6 months, respectively, which is clinically important.
To our knowledge, few studies have investigated the relationship between a delay in reconstruction and the incidence of secondary pathologies. In line with the results published by Papastergiou et al., our finding showed the association between ACL tear and meniscus injury 3 months after the events. It could be concluded that the rate of secondary meniscus injury increases over time and, therefore, the operation should be performed within 3 months of the injury.[18] While Rocha et al., described similar findings, they noted a higher rate of lateral meniscus injury within the first 3 months of ACL tear.[19] Papastergiou et al., studied 451 patients who had been undertaken reconstructive operation.[18] They examined the incidence of meniscal tears based on the interval between the injury and operation, but failed to assess the possible changes in the articular surface. They found an increased incidence of both medial and lateral meniscal tears when the operation was postponed beyond 3 months. Due to the fact that most of the elite players are expected to continue their participation in competitions of the league despite of their injury, serious rehabilitation will be achieved for their recovery. Therefore, after rehabilitation process and reducing their pain and effusion, pseudo well-being and self confidence will occur. These athletes believed that the recovery of ACL tearing was completed and they could continue their playing without any treatment for their knee. But, unfortunately, this type of estimation will increase the chance of severe injury, especially meniscal tear.
The incidence of chondral lesion among our population increased as the interval between injury and reconstruction was >6 months. Church and Keating[10] reviewed 187 patients and found a significant increase in degenerative changes of grade 1 to 4 (31.3% vs 10.7%) and also in the overall incidence of meniscal tears among those who had undergone late reconstruction (after >12 months of injury). Based on our findings, significant changes in the articular surface of the injured knee starts in less than a year.
It has been suggested that patients with ACL deficiency dispose to the development of chondral injuries in weight bearing activities due to excessive anterior tibial translation and rotational instability in their injured knee.
In a similar study conducted by Murell et al.,[20] the injuries to the medial condyl of femur were more prevalent than other parts of condyls.
It is believed that the increased shear stresses on the meniscus and the application of greater weight-bearing loads on the articular surface (unconditioned cartilage region), which was not previously functionally loaded, may account for the abnormal translation and rotational motions following ACL injury.[21,22] Moreover, opposite to the constantly changing, contact points of the tibio–femoral articulation in a normal knee (rollback), the femur in an ACL-deficient knee may remain in contact with a section of the articular surface of tibia, resulting in point-loading with non-physiological loads, leading to degeneration process and chondral damage.[23] Andriacchi et al., in their finite element analysis of the kinematic changes related to ACL deficiency, confirmed this hypothesis.[22] Barker et al.,[1] found that the relative internal rotation of the tibia secondary to ACL injury results in an increased cartilage loss especially in the medial compartment of the injured knee. This finding is believed to be secondary to a shift of load bearing to the thinner regions of articular cartilage.
Despite the increased risk of chondral injuries secondary to a delay of >6 months in the time of surgery, there was a peak of high-grade chondral lesion among athletes operated in the first 3 months. This could be contributed to the severity of injuries at the time of damage. Acute chondral injuries have been reported in 20% of ACL tears; however, many authors believe that the common pattern of bone bruise, known as post-truamatic bone marrow lesions, represent occult damage to the cartilage secondary to the compressive force imposed on the joint surface at the time of the ACL tear.[24–26]
One of our limitations include low number of female athletes in the study. As the number of professional female athletes is lower than in some other countries, there are not many high-level competitions; similarly, international competition is subject to considerable limitation. Therefore, we could not compare our results about women's sports to that in other studies.
CONCLUSION
In conclusion, based on our findings, in order to reduce the chance of the occurrence of instability induced medial meniscal tears and chondral lesions, reconstruction should be performed before 6 months after injury. It is recommended that surgical reconstruction should be performed instantaneously after conduction of intensive rehabilitation program, psychological preparation, and economical support. Due to the fact that the return to play is one of the most imperative and challenging subjects in sports medicine field, identifying the best time for reconstruction of ACL deficiency is of high importance. It seems that time preparation to improve patients' compliance to surgery takes between 3 weeks to 3 months.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Strauss EJ, Barker JU, Bach BR. Osteoarthritis in the anterior cruciate ligament-deficient knee-Epidemiology, biomechanics, and effects on the meniscus and articular cartilage. US Musculoskelet Rev. 2010;5:65–9. [Google Scholar]
- 2.Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J Sci Med Sport. 2009;12:622–7. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Rochcongar P, Laboute E, Jan J, Carling C. Ruptures of the anterior cruciate ligament in soccer. Int J Sports Med. 2009;30:372–8. doi: 10.1055/s-0028-1105947. [DOI] [PubMed] [Google Scholar]
- 4.Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, Garrett WE, et al. Noncontact anterior cruciate ligament injuries: Risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Tandogan RN, Taser O, Kayaalp A, Taskiran E, Pinar H, Alparslan B, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc. 2004;12:262–70. doi: 10.1007/s00167-003-0398-z. [DOI] [PubMed] [Google Scholar]
- 6.Stevens KJ, Dragoo JL. Anterior cruciate ligament tears and associated injuries. Top Magn Reson Imaging. 2006;17:347–62. doi: 10.1097/RMR.0b013e3180421cc2. [DOI] [PubMed] [Google Scholar]
- 7.Pookarnjanamorakot C, Korsantirat T, Woratanarat P. Meniscal lesions in the anterior cruciate insufficient knee: The accuracy of clinical evaluation. J Med Assoc Thai. 2004;87:618–23. [PubMed] [Google Scholar]
- 8.Kennedy J, Jackson MP, O'Kelly P, Moran R. Timing of reconstruction of the anterior cruciate ligament in athletes and the incidence of secondary pathology within the knee. J Bone Joint Surg Br. 2010;92:362–6. doi: 10.1302/0301-620X.92B3.22424. [DOI] [PubMed] [Google Scholar]
- 9.Bottoni CR, Liddell TR, Trainor TJ, Freccero DM, Lindell KK. Postoperative range of motion following anterior cruciate ligament reconstruction using autograft hamstrings: A prospective, randomized clinical trial of early versus delayed reconstructions. Am J Sports Med. 2008;36:656–62. doi: 10.1177/0363546507312164. [DOI] [PubMed] [Google Scholar]
- 10.Church S, Keating JF. Reconstruction of the anterior cruciate ligament: Timing of surgery and theincidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005;87:1639–42. doi: 10.1302/0301-620X.87B12.16916. [DOI] [PubMed] [Google Scholar]
- 11.Nebelung W, Wuschech H. Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy. 2005;21:696–702. doi: 10.1016/j.arthro.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 12.Irvine GB, Glasgow MM. The natural history of the meniscus in anterior cruciate insufficiency. Arthroscopic analysis. J Bone Joint Surg Br. 1992;74:403–5. doi: 10.1302/0301-620X.74B3.1587888. [DOI] [PubMed] [Google Scholar]
- 13.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22:632–44. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade RF, Wentorf FA, Fritts H, Gundry C, Hightower CD. A prospective magnetic resonance imaging study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthroscopy. 2007;23:1341–7. doi: 10.1016/j.arthro.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 15.Javed A, Siddique M, Vaghela M, Hui AC. Interobserver variations in intra-articular evaluation during arthroscopy of the knee. J Bone Joint Surg Br. 2002;84:48–9. doi: 10.1302/0301-620x.84b1.12168. [DOI] [PubMed] [Google Scholar]
- 16.Brismar BH, Wredmark T, Movin T, Leandersson J, Svensson O. Observer reliability in the arthroscopic classification of osteoarthritis of the knee. J Bone Joint Surg Br. 2002;84:42–7. doi: 10.1302/0301-620x.84b1.11660. [DOI] [PubMed] [Google Scholar]
- 17.Frobell RB, Lohmander LS, Roos HP. Acute rotational trauma to the knee: Poor agreement between clinical assessment and magnetic resonance imaging findings. Scand J Med Sci Sports. 2007;17:109–14. doi: 10.1111/j.1600-0838.2006.00559.x. [DOI] [PubMed] [Google Scholar]
- 18.Papastergiou SG, Koukoulias NE, Mikalef P, Ziogas E, Voulgaropoulos H. Meniscal tears in the ACL-deficient knee: Correlation between meniscal tears and the timing of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15:1438–44. doi: 10.1007/s00167-007-0414-9. [DOI] [PubMed] [Google Scholar]
- 19.Rocha ID, Moraes TM, Rezende MU, Pécora JR. Progress assessment of injuries associated to anterior cruciate ligament injuries. Acta Ortop Bras. 2007;15:105–8. [Google Scholar]
- 20.Murrell GA, Maddali S, Horovitz L, Oakley SP, Warren RF. The effects of time course after anterior cruciate ligament injury in correlation with meniscal and cartilage loss. Am J Sports Med. 2001;29:9–14. doi: 10.1177/03635465010290012001. [DOI] [PubMed] [Google Scholar]
- 21.Stergiou N, Ristanis S, Moraiti C, Georgoulis AD. Tibial rotation in anterior cruciate ligament (ACL)-deficient and ACL-reconstructed knees: A theoretical proposition for the development of osteoarthritis. Sports Med. 2007;37:601–3. doi: 10.2165/00007256-200737070-00004. [DOI] [PubMed] [Google Scholar]
- 22.Andriacchi TP, Briant PL, Bevill SL, Koo S. Rotational changes at the knee after ACL injury cause cartilage thinning. Clin Orthop Relat Res. 2006;442:39–44. doi: 10.1097/01.blo.0000197079.26600.09. [DOI] [PubMed] [Google Scholar]
- 23.Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med. 1999;27:143–56. doi: 10.2165/00007256-199927030-00001. [DOI] [PubMed] [Google Scholar]
- 24.Palmer WE. Magnetic resonance imaging of knee trauma: Biomechanical approach. Top Magn Reson Imaging. 2003;14:161–78. doi: 10.1097/00002142-200304000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Hayes CW, Brigido MK, Jamadar DA, Propeck T. Mechanism-based pattern approach to classification of complex injuries of the knee depicted at MR imaging. Radiographics. 2000;(Spec No. 20):S121–34. doi: 10.1148/radiographics.20.suppl_1.g00oc21s121. [DOI] [PubMed] [Google Scholar]
- 26.Yu JS, Cook PA. Magnetic resonance imaging (MRI) of the knee: A pattern approach for evaluating bone marrow edema. Crit Rev Diagn Imaging. 1996;37:261–303. [PubMed] [Google Scholar]


