Dear Editor,
Polypoidal choroidal vasculopathy (PCV) is primarily a choroidal vascular disease, which can lead to acute severe visual loss secondary to massive submacular or vitreous hemorrhage.
Various treatment modalities, such as direct thermal laser photocoagulation, tissue plasminogen activator (t-PA) injection with gas displacement, submacular surgery and macular translocation surgery have been proposed. Photodynamic therapy (PDT) with verteporfin has shown good results for PCV, but extensive subretinal hemorrhages and exudation limits its application.[1] Favorable results have been reported with combined therapy, including PDT and intravitreal bevacizumab (IVB), to treat PCV.[2]
We evaluated nine eyes of eight patients with PCV who were treated with IVB monotherapy. We excluded patients that had any previous treatment for PCV or wet age-related macular degeneration (AMD) in the study or contralateral eye.
All participants received a comprehensive ocular examination including digital fluorescein angiography (FA), indocyanine green angiography (ICGA) and optical coherence tomography (OCT) at baseline, and at 3-monthly interval visits till last follow-up. IVB injection was performed as per standard protocol. Repeat treatment was performed every 4 weeks if the OCT showed persistent pigment epithelial detachment (PED)/subretinal fluid (SRF) or active polypoidal lesion on fundus fluorescein angiography (FFA)/ICGA.
The mean age was 60.6 years and 37.5% of the patients were female. At baseline, the median Snellen best corrected visual acuity (BCVA) was 20/2000 (range 20/30–20/10,000). The mean follow-up duration was 8.4 months (range 4–12 months).
All eyes showed resolution of subretinal hemorrhage, PED [Fig. 1] and angiographic activity [Fig. 2], but persistence of polypoidal lesion was noted in three eyes. At the last follow-up, the median Snellen BCVA was 20/100 (range 20/25–20/400). The mean log MAR BCVA showed a statistically significant improvement from 1.41 to 0.63 (P = 0.04). Seven (77.7%) eyes showed significant improvement in visual acuity, with mean number of line improvement of 6.5. The remaining two eyes maintained the baseline visual acuity till last follow-up. The mean number of injections was 2.3. The mean longest treatment-free period was 5.88 months. No significant systemic or ocular side-effects were observed in any of the eyes receiving IVB injections.
Figure 1.
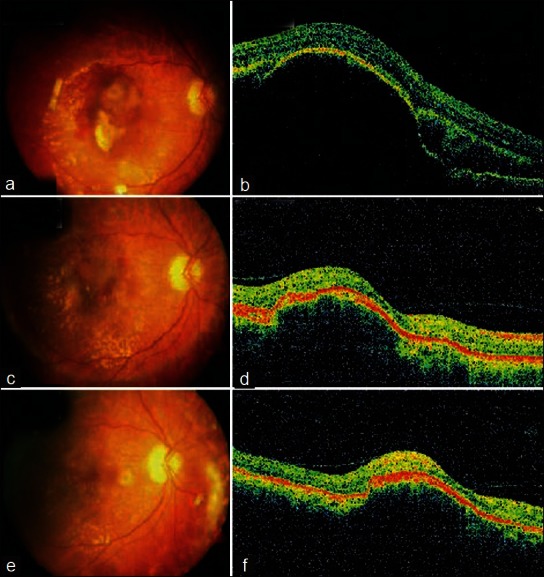
Fundus photo at baseline (a) shows hemorrhagic pigment epithelial detachment (PED) involving the fovea with subretinal hemorrhage. (b) (at 1-month follow-up) Reduction in the PED with decrease in subretinal hemorrhage. (c) (at 3-month follow-up) Disappearance of subretinal hemorrhage and PED. (d) OCT at baseline shows a PED with intraretinal cystic fluid at the edge of the PED. (e) (At 1-month follow-up) and (f) (at 3-month follow-up) Significant reduction in the height of the PED on OCT
Figure 2.
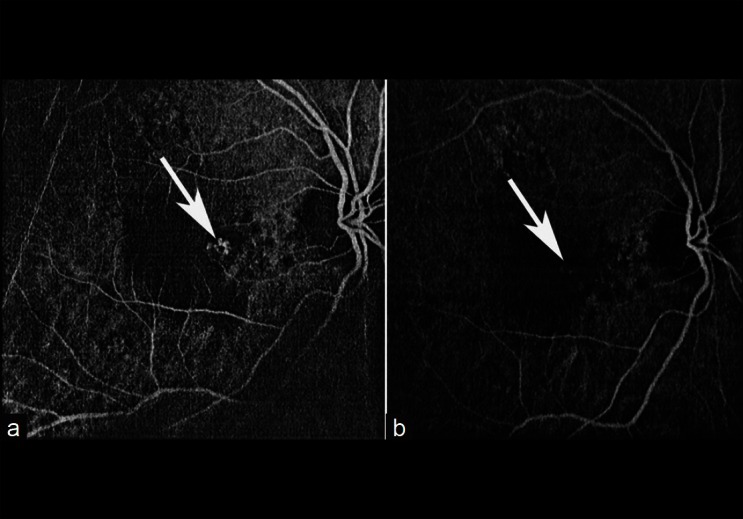
Indocyanine green angiographic images (a) before treatment and (b) 1 year after treatment, showing regression of polyps (arrows) after treatment
In our study, mean BCVA improvement of 2 or more lines was seen in 72% of the patients, and the remaining 28% showed a stabilization of visual acuity at mean follow-up of 8.4 months. Kokame et al.,[3] reported stabilization of vision at 6 months, with monthly intravitreal injection of ranibizumab in PCV.
Lai et al., reported stabilization of vision and reduction in exudative detachment with intravitreal bevacizumab, but a limited role in regression of polypoidal lesions in ICGA. Persistent lesions were treated with PDT.[4] In our study, persistent lesions were closely followed-up, which did not bleed again during the follow-up. Complete regression of polypoidal lesion in ICGA may not be the therapeutic target, but close follow-up is mandatory.
In conclusion, our study demonstrated that IVB injection helps to improve or maintain the vision in patients with symptomatic treatment-naïve PCV.
References
- 1.Chan WM, Lam DS, Lai TY, Liu DT, Li KK, Yao Y, et al. Photodynamic therapy with vertiporfin for symptomatic polypoidal choroidal vasculopathy. Ophthalmology. 2004;111:1576–84. doi: 10.1016/j.ophtha.2003.12.056. [DOI] [PubMed] [Google Scholar]
- 2.Sato T, Kishi S, Matsumoto H, Mukai R. Combined photodynamic therapy with verteporfin and intravitreal bevacizumab for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2010;149:947–54.e.1. doi: 10.1016/j.ajo.2009.12.038. [DOI] [PubMed] [Google Scholar]
- 3.Kokame GT, Yeung L, Lai JC. Continuous anti-VEGF treatment with ranibizumab for polypoidal choroidal vasculopathy: 6-month results. Br J Ophthalmol. 2010;94:297–301. doi: 10.1136/bjo.2008.150029. [DOI] [PubMed] [Google Scholar]
- 4.Lai TY, Chan WM, Liu DT, Luk FO, Lam DS. Intravitreal bevacizumab (Avastin) with or without photodynamic therapy for the treatment of polypoidal choroidal vasculopathy. Br J Ophthalmol. 2008;92:661–6. doi: 10.1136/bjo.2007.135103. [DOI] [PubMed] [Google Scholar]


