Abstract
Background:
Operative intervention for thoracic trauma typically requires thoracotomy. We hypothesized that thoracoscopy may be safely and effectively utilized for the acute management of thoracic injuries.
Materials and Methods:
The Trauma Registry of a Level I trauma center was queried from 1999 through 2010 for all video-assisted thoracic procedures within 24 h of admission. Data collected included initial vital signs, operative indication, intraoperative course, and postoperative outcome.
Results:
Twenty-three patients met inclusion criteria: 3 (13%) following blunt injury and 20 (87%) after penetrating trauma. Indications for urgent thoracoscopy included diaphragmatic/esophageal injury, retained hemothorax, ongoing hemorrhage, and open/persistent pneumothorax. No conversions to thoracotomy were required and no patient required re-operation. Mean postoperative chest tube duration was 2.9 days and mean length of stay was 5.6 days.
Conclusion:
Video-assisted thoracoscopic surgery is safe and effective for managing thoracic trauma in hemodynamically stable patients within the first 24 h post-injury.
Keywords: Thoracic trauma, video-assisted thoracoscopic surgery, retained hemothorax
INTRODUCTION
Traumatic injuries are a significant cause of morbidity and mortality in the United States, contributing to 140,000 deaths annually, and are the leading cause of death in individuals younger than 40 years of age.[1] Thoracic injuries are the primary factor in approximately 35% of these deaths, one-third of which occur immediately following the injury, and are contributory in nearly 75% of trauma-related deaths.[1,2] Up to 15% of patients who sustain thoracic trauma undergo emergent thoracotomy for resuscitation, massive hemothorax, cardiac tamponade, large thoracic wounds, major thoracic vascular injuries, tracheobronchial injuries, or evidence of esophageal injury. The remaining 85-90% of patients who reach the emergency department but do not require emergent thoracotomy are initially managed with tube thoracostomy, pain control, pulmonary toilet, and observation.[3] Patients failing this management ultimately require invasive thoracotomy for further evaluation and treatment.
Video-assisted thoracoscopic surgery (VATS) has been established as safe and effective for major thoracic procedures such as pulmonary resection. VATS has also been used in the management of thoracic trauma for indications such as retained hemothorax, persistent air leak, empyema, evaluation of diaphragmatic and mediastinal injuries.[3–7]
VATS has typically been described for the management of subacute or chronic complications of thoracic trauma and there is little data regarding the use of this technique in the more acute setting. Over the last decade, VATS has been our preferred technique in the acute setting whenever feasible. We hypothesized that VATS may be safely and effectively utilized for the acute management of hemodynamically stable patients with thoracic injuries in a time period encompassing the first 24 h post-injury.
MATERIALS AND METHODS
Patients
The trauma database at a level I trauma center was queried to identify all patients who underwent VATS for acute trauma between 1999 and 2010. Patients were excluded if they had VATS procedures after 24 h of admission. Emergency department records, operative reports, inpatient progress notes, and discharge summaries were reviewed. Data collected included patient demographics, type of traumatic injury, preoperative evaluation, operation performed, blood product transfusion, and postoperative outcome. The study was approved by the institutional review board of the University of Cincinnati and the need for informed consent was waived.
Assessment and operative technique
Initial assessment, resuscitation, and stabilization were performed in the emergency department under the supervision of a multidisciplinary trauma team. Patients were evaluated by chest X-ray and further imaging modalities as indicated. Tube thoracostomy was performed based on clinical or radiological evidence of hemothorax and/or pneumothorax. Consultations were placed to other specialties, including the thoracic surgery service, when deemed appropriate by the trauma service attending surgeon.
VATS was performed only in patients who were hemodynamically stable and met criteria for undergoing urgent thoracotomy. All procedures were performed in the operating room under general anesthesia. When feasible, a double-lumen endotracheal tube was used; however, when necessary, single-lumen tubes were utilized with intermittent apnea or a bronchial blocker. VATS was performed with patients in the lateral decubitus position, typically employing three 12-millimeter ports. Postoperative pleural drainage was established with a single chest tube.
Statistics
Results are expressed as mean ± standard deviation or median (range).
RESULTS
Patient characteristics
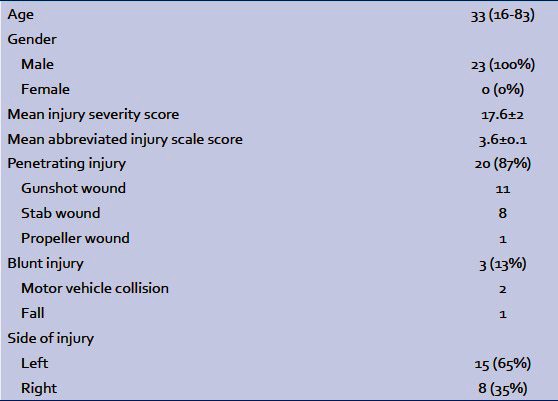
From 1999 through 2010, the trauma service averaged 2142 admissions per year. Of these patients, 23 underwent VATS procedures for acute thoracic trauma within 24 h of admission. Patient demographics and injury causes are shown in Table 1. All patients underwent chest X-ray in the emergency room and 11 patients underwent further imaging with a chest computed tomography (CT) scan. Preoperative chest tubes were placed in 17 patients. Mean preoperative chest tube output was 964 ± 141 milliliters (mL). Almost half of the patients (11/23) sustained additional extra-thoracic injuries, with four requiring abdominal operation.
Table 1.
Patient characteristics
Perioperative details
Indications for urgent VATS were: 6 (26%) for suspected diaphragmatic or esophageal injuries, 16 (70%) for bleeding, and 1 (4%) for open/persistent pneumothorax. Mean time from arrival in the emergency room to initiation of operation was 353 ± 88 min (range 15 min to 23 h). Six patients (26%) were in the operating room within one hour of arrival in the emergency room, and another six (26%) within two hours. Eight (35%) of the operations were performed in conjunction with a thoracic surgeon. The other 15 were performed by trauma surgeons. Mean total operating time for the VATS procedures was 116 ± 16 min (range 47 to 381 min, with concomitant abdominal operations). Eleven (48%) patients underwent evacuation of a hemothorax only, and were not found to have active bleeding requiring intervention. Six (26%) patients underwent pulmonary wedge resections for lung lacerations. One patient had a chest wall wound evaluated and repaired. Two patients underwent diaphragm repair – one via thoracic and one via abdominal approach. The final three patients underwent VATS for evaluation for potential mediastinal and diaphragmatic injuries, with no repair required. No conversions to thoracotomy were required and no patient required re-operation.
Overall mean estimated blood loss from all procedures combined with VATS and including any evacuated pleural hematoma was 433 ± 70 mL. Nine (39%) patients received blood product transfusions intraoperatively, resulting in a mean transfusion of 1 unit of packed red blood cells per patient. Two (9%) patients received fresh frozen plasma as well.
Postoperatively, mean total chest tube output was 564 ± 194 mL over a mean duration of pleural drainage of 2.9 ± 0.3 days (range 1 to 7 days). Mean total postoperative length of stay (LOS) was 5.6 ± 0.9 days.
There was one postoperative death in a patient who developed abdominal compartment syndrome following a thoracoabdominal gunshot wound. One patient who underwent VATS for retained hemothorax after a fall, redeveloped a hemothorax after chest tube removal and was successfully treated with directed pleural pigtail catheter placement and infusion of tissue plasminogen activator.
DISCUSSION
While the role of VATS in the management of thoracic injuries and their sequelae is expanding, its defined use in the acute setting is not as well established. Up to 30% of patients sustaining thoracic injuries require urgent exploration which is typically done via thoracotomy. Our institutional experience suggests that VATS can be successfully performed within the first 24 h following thoracic trauma with minimal morbidity, obviating the need for thoracotomy.
The use of thoracoscopy in the setting of trauma has gained increasing support in the literature and in practice over the last several decades. Branco first described thoracoscopy to aid in the diagnosis and treatment of patients with penetrating chest injuries in 1946.[8] VATS was then subsequently described by Jackson and Ferreira in 1976 to diagnose diaphragmatic injuries incurred by penetrating trauma to the left lower chest.[9] In 1981, Jones, et al., reported the performance of emergency thoracoscopy with local anesthetic in patients with ongoing bleeding following tube thoracostomy placement for traumatic hemothoraces.[10] Despite these early reports, VATS did not become more established in the management of thoracic trauma until recently. The use of thoracoscopy in the trauma setting has followed the expansion of VATS in elective thoracic procedures. VATS has been associated with decreased postoperative wound and pulmonary complications, reduced pleural drainage duration and hospital length of stay, and improved pain control and postoperative quality of life. Recent reports evaluating the use of VATS for chest trauma management have demonstrated similar benefits.[3,4,7,11]
Most of the published experience with VATS following trauma has been in a more chronic setting, usually days or weeks after the initial injury. Indications for subacute thoracoscopy following trauma include empyema, treatment of thoracic duct injury, and removal of symptomatic foreign bodies. VATS in these situations is not much different than that performed for non-traumatic situations such as spontaneous pneumothorax, non-traumatic retained hemothorax or parapneumonic empyema.
Over the last several years, we have evolved our use of VATS following trauma to include hemodynamically stable patients who have an indication for urgent thoracic exploration within 24 h following presentation. The most common urgent use of VATS following trauma is the drainage of residual hemothoraces greater than 500 mL or collections that result in the opacification of one-third of a hemithorax.[12] Many patients with thoracic trauma can be initially managed with a chest tube alone; however, retained hemothorax may be found in up to 18% of patients, with nearly 40% of these undrained hemothoraces resulting in fibrothorax.[13] In addition, up to 23% of pneumothoraces will have a persistent air-leak.[14] Indications for thoracoscopy within 24 h post-injury include the evaluation and treatment of persistent hemo- and pneumothoraces as well as other injuries such as diaphragmatic tears, esophageal injuries, and other mediastinal wounds.
Much of the literature regarding the use of post-injury VATS does not distinguish between the acute and chronic setting. Our study is one of the larger studies of VATS in the first 24 h of injury. We demonstrated that this approach is safe and effective in acutely injured and appropriately selected trauma patients as none of our patients required conversion to thoracotomy or re-operation. The mean chest tube duration was under three days and the mean length of stay under six days despite the fact that the patients had significant injuries. These outcomes are similar to those reported by Meyer, et al., in a study in which patients who failed non-operative management with tube thoracostomy were randomized to VATS or thoracotomy at 72 h after injury.[15] Patients undergoing VATS in this study had significantly shorter postoperative length of stay and chest tube duration compared to patients undergoing thoracotomy. Contraindications to the use of VATS should include: Hemodynamic instability, inability to tolerate single-lung ventilation or a lateral decubitus position, suspected injuries to the heart or great vessels, and severe adhesions due to prior thoracic procedures or conditions.
CONCLUSION
Our study demonstrates that VATS is safe and effective for managing acute thoracic trauma within the first 24 h of injury in hemodynamically stable patients. VATS should be considered for the management of patients who meet criteria for urgent thoracotomy following traumatic injury and may be used successfully in the early diagnosis and treatment of thoracic injuries.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Meredith JW, Hoth JJ. Thoracic trauma: When and how to intervene. Surg Clin North Am. 2007;87:95–118. doi: 10.1016/j.suc.2006.09.014. vii. [DOI] [PubMed] [Google Scholar]
- 2.Manlulu AV, Lee TW, Thung KH, Wong R, Yim AP. Current indications and results of VATS in the evaluation and management of hemodynamically stable thoracic injuries. Eur J Cardiothorac Surg. 2004;25:1048–53. doi: 10.1016/j.ejcts.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 3.Cetindag IB, Neideen T, Hazelrigg SR. Video-assisted thoracic surgical applications in thoracic trauma. Thorac Surg Clin. 2007;17:73–9. doi: 10.1016/j.thorsurg.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Ahmed N, Jones D. Video-assisted thoracic surgery: State of the art in trauma care. Injury. 2004;35:479–89. doi: 10.1016/S0020-1383(03)00289-4. [DOI] [PubMed] [Google Scholar]
- 5.Abolhoda A, Livingston DH, Donahoo JS, Allen K. Diagnostic and therapeutic video assisted thoracic surgery (VATS) following chest trauma. Eur J Cardiothorac Surg. 1997;12:356–60. doi: 10.1016/s1010-7940(97)00192-9. [DOI] [PubMed] [Google Scholar]
- 6.Lang-Lazdunski L, Mouroux J, Pons F, Grosdidier G, Martinod E, Elkaïm D, et al. Role of videothoracoscopy in chest trauma. Ann Thorac Surg. 1997;63:327–33. doi: 10.1016/s0003-4975(96)00960-5. [DOI] [PubMed] [Google Scholar]
- 7.Hazelrigg SR, Cetindag IB, Fullerton J. Acute and chronic pain syndromes after thoracic surgery. Surg Clin North Am. 2002;82:849–65. doi: 10.1016/s0039-6109(02)00031-2. [DOI] [PubMed] [Google Scholar]
- 8.Branco J. Thoracoscopy as a method of exploration in penetrating injuries of the chest. Diseases Chest. 1946;12:330–5. doi: 10.1378/chest.12.4.330. [DOI] [PubMed] [Google Scholar]
- 9.Jackson AM, Ferreira AA. Thoracoscopy as an aid to the diagnosis of diaphragmatic injury in penetrating wounds of the left lower chest: A preliminary report. Injury. 1976;7:213–7. doi: 10.1016/0020-1383(76)90216-3. [DOI] [PubMed] [Google Scholar]
- 10.Jones JW, Kitahama A, Webb WR, McSwain N. Emergency thoracoscopy: A logical approach to chest trauma management. J Trauma. 1981;21:280–4. [PubMed] [Google Scholar]
- 11.Smith JW, Franklin GA, Harbrecht BG, Richardson JD. Early VATS for blunt chest trauma: A management technique underutilized by acute care surgeons. J Trauma. 2011;71:102–7. doi: 10.1097/TA.0b013e3182223080. [DOI] [PubMed] [Google Scholar]
- 12.Heniford BT, Carrillo EH, Spain DA, Sosa JL, Fulton RL, Richardson JD. The role of thoracoscopy in the management of retained thoracic collections after trauma. Ann Thorac Surg. 1997;63:940–3. doi: 10.1016/s0003-4975(97)00173-2. [DOI] [PubMed] [Google Scholar]
- 13.Helling TS, Gyles NR, 3r rd, Eisenstein CL, Soracco CA. Complications following blunt and penetrating injuries in 216 victims of chest trauma requiring tube thoracostomy. J Trauma. 1989;29:1367–70. doi: 10.1097/00005373-198910000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Carrillo EH, Schmacht DC, Gable DR, Spain DA, Richardson JD. Thoracoscopy in the management of posttraumatic persistent pneumothorax. J Am Coll Surg. 1998;186:636–9. doi: 10.1016/s1072-7515(98)00093-3. discussion 639-40. [DOI] [PubMed] [Google Scholar]
- 15.Meyer DM, Jessen ME, Wait MA, Estrera AS. Early evacuation of traumatic retained hemothoraces using thoracoscopy: A prospective, randomized trial. Ann Thorac Surg. 1997;64:1396–400. doi: 10.1016/S0003-4975(97)00899-0. [DOI] [PubMed] [Google Scholar]


