Abstract
The objective of this study is to determine the prevalence of adherence to daily medications among children with sickle cell disease (SCD). Prescription records for 12 months were obtained from participants who had insurance in a Medicaid-based single health maintenance organization. Adherence was measured as a ratio between the number of expected days and the observed days between two refill periods for daily medications. A total of 93 children were studied. The average refill prescription rate was 58.4%. More formal strategies are required to identify barriers to prescription refills among children with SCD.
Keywords: Sickle cell disease, medications, adherence, children
Introduction
Sickle cell disease (SCD) is an inherited disorder of red blood cells that affects 1 in 400 African American newborns [1]. In the United States, it is mandatory to screen every newborn for a hemoglobinopathy (including SCD) in order to facilitate the start of prophylactic penicillin and anticipatory guidance prior to four months of age [2]. In addition to daily administration of penicillin until at least five years of age, children with SCD often require other daily medications such as folic acid, hydroxyurea, and oral iron chelation therapy to decrease the risk of complications [3–5]. Further, up to 50% of children with SCD also have asthma, and many require daily asthma medication [6–7].
Given the high expectation that children with SCD take daily medication to prevent complications of the disease, understanding the rate of adherence is an important component of patient care. A study on penicillin adherence in children with SCD found only 12% of the children had consistent penicillin refills over a three month period according to pharmacy records [8]. Despite the high rate of asthma among children with SCD, no data exist as to whether prescription of asthma medication is associated with a change in the adherence rate of daily-prescribed medication for SCD. Given the importance of adherence as a modifiable factor in clinical outcomes, understanding the prevalence for adherence for this population may prove to be important [9–14].
Multiple studies from our group and others demonstrate that asthma is associated with an increased rate of vaso-occlusive pain and acute chest syndrome episodes [6, 15–16]. Evidence demonstrating a decreased adherence rate to either category of medication, SCD or asthma, would be a potential explanation as to why children with SCD and asthma have a higher rate of SCD related morbidity. Further, knowledge about adherence rates to both classes of medication may facilitate patient care and improve targeted education. The primary objective of this study was to determine whether additional burden of daily asthma medication was associated with a decrease in adherence to SCD medication or whether taking daily SCD medication was associated with a decrease in adherence in daily asthma medication.
Methods
The Human Research Protection Office (HRPO) at Washington University School of Medicine approved this study. A retrospective cohort study on medication adherence was conducted in children with SCD and Medicaid insurance presenting to the St. Louis Children’s Hospital SCD Medical Treatment and Education Center at Washington University School of Medicine. Patients’ prescription records for daily medications were evaluated for 12 consecutive months. Prescription records were obtained from the Medicaid insurance company HealthCare USA. Approximately 80% of the patients presenting to the Sickle Cell Disease Medical Treatment and Education Center are on Medicaid. Among this group, 60% have HealthCare USA as their primary health insurer.
We assessed the following medication use: folic acid, hydroxyurea, penicillin, and asthma medications (Advair, Flovent, Pulmicort, Singulair). Medicines such as opioids were not measured for adherence because they are not generally taken daily. Hospital admission records were evaluated to account for the days the patient did not use prescribed medicine from the pharmacy. Patients were given as many extra days as the number of days of their hospital stay to refill their next medication on an outpatient setting since they had received hospital medications. In addition, if patients were prescribed Advair or Flovent while in the hospital, and were given the remainder of the medication at discharge, we accounted for these days by allowing as many extra days as the duration of the medication to pick up their next prescription.
Adherence was measured as the ratio of the number of expected days between refills periods (numerator) and the observed days between refill periods for the patient (denominator). For example, if a patient had 30-day supply of medication and refilled the medication in 40 days, adherence ratio would be 30:40, and multiplied by 100 to equal 75%. This would signify the patient was on time in filling the medication by 75% of the required time needed to fill the medication to be completely adherent. An average medication adherence was calculated by averaging intervals in the 12 months. This method of measurement is analogous to the validated and frequently used term medication possession ratio (MPR) which is defined as a ratio between the total days of supply of medications in a specified observation period and number of days in the observation period [17].
Results
Adherence to medication prescribed on a daily basis was measured in 93 children with SCD for a full year. In this cohort, 48.4% (n=45) had SCD-SS, 36.6% (n=34) had SCD-SC disease, 9.7% (n=9) had SCD-S Beta thalassemia plus disease, 4.3% (n=4) had SCD- S beta thalassemia zero disease, and 1.1% (n=1) had SCD-S/Hereditary Persistence. The percentage of male was 59.1% (n=55). The mean age was 7 years with the youngest being 6 months and the oldest being 20 years. In regards to the medications prescribed, 62 patients had penicillin, 28 daily asthma medications (Advair: n=2, Flovent: n=22, Pulmicort: n=6, Singulair: n=8), 4 hydroxyurea, and 80 folic acid. Furthermore, 73% of the children were prescribed two or more scheduled medications.
Adherence rates for each drug were: penicillin 54.9% (n=62), all asthma medications 59.3 % (n=28) (Advair 62.7% (n=2), Flovent 61.2 (n=22), Pulmicort 53.9 (n=6), Singulair 67.2% (n=8)), hydroxyurea 60.5% (n=4), and folic acid 61.3% (n=80). The overall adherence was a mean of 58.4%, with a median of 59.0% and the 25%tile of 36.6% and the 75%tile of 79.6%. Moreover, average adherence for patients who took asthma medications in addition to SCD medications was 61% while it was 56% for those who did not take asthma medications (2 sided t-test p = 0.45).
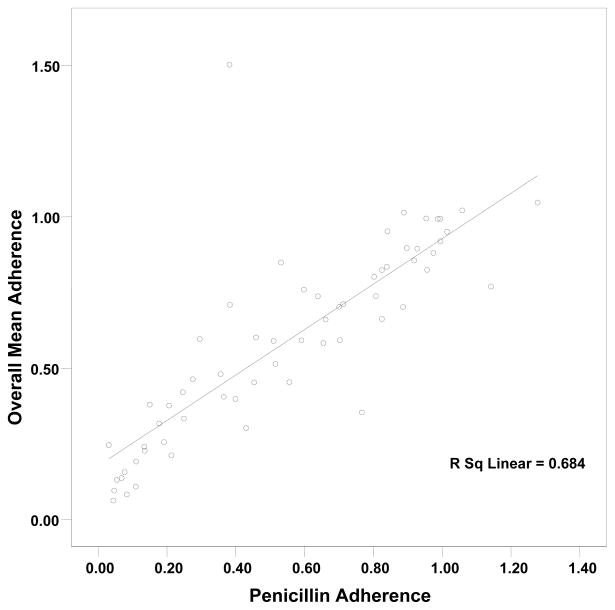
We evaluated whether adherence to one drug was associated with adherence to a second drug. When patients were adherent to one therapy, they were generally adherent to all of the therapies. The correlation coefficient between adherence to penicillin and overall adherence was 0.827 (P= < 0.001) (figure 1). Similarly, this pattern was observed with folic acid and Flovent, a daily asthma medication, with a correlation coefficient of 0.824 (P = <0.001) and 0.644 (p = 0.001), respectively.
Figure 1. Correlation of adherence to penicillin to overall adherence in 62 children with SCD.
The vertical axis represents average medication adherence to all scheduled daily medications in patients with sickle cell disease of the course of 12 months, and the horizontal axis represents adherence to penicillin. The prescription refill rate was measured as a ratio of the number of days that the medicine intended to supply and the difference in days between two refill periods for the patient. Pearson’s correlation coefficient indicated a strong positive relationship between the two with a coefficient of 0.827 (P = <0.001).
Discussion
Among a cohort of children with SCD, we assessed medication refill records for one year. An overall 58.4% refill rate indicates that patients were only partially adherent to their medication regimen and did not receive the full benefit from these medications.
An expected finding in this study was the strong correlation between patient’s adherence to one medication and patient’s adherence to all other medications. This observation suggests, but does not confirm that adherence is more patient specific than drug specific. Increasing overall adherence may involve multiple factors such as better education, monitoring, access to pharmacy, support from family, and/or relationship to healthcare providers. Given that poor adherence can contribute to substantial worsening of disease, death, and increased health care costs, greater efforts are necessary to identify specific patients at increased risk for non-adherence [9–14].
A major finding from our study was that use of daily asthma medication was not associated with a lower rate of adherence of medication used for prophylaxis of SCD-related morbidity. To our knowledge, this is the first study in SCD to evaluate the adherence rate of rate of multiple medications, including asthma medication in children with SCD. Previous studies have focused on adherence of a single agent, typically penicillin [8] or more recently hydroxyurea [18]. However, none of the studies have evaluated whether the burden of taking daily medications for asthma influenced the adherence rate of the single agent of interests. Given the high prevalence of asthma among children with SCD, these findings are relevant to health care providers of children with SCD who have asthma.
As would be anticipated, several limitations are inherent in our study design. Measure of adherence was not a direct measure because we did not observe patients’ intake of medications. Therefore, medication adherence could be lower than what we documented by prescription refills. In addition to patients’ compliance with medications refills, appropriate dosing and administration of the medication at the prescribed interval is important to bring about the desired effect. However, it is important to note that neither the dose at which the patients took their medication nor the interval at which they took the medication was assessed. Despite the limitation of pharmacy refill records as an indirect measure of adherence, prior studies demonstrate adherence data from pharmacy refill records are correlated with clinical outcomes [19–20]. Further, adherence was only measured in medications that were prescribed to be taken daily. Despite these limitations, we believe our results provide reasonable estimates of daily prescription refill rates in children with SCD.
In summary, children with SCD refill their daily medications approximately 58% of the time; and those who refill one daily medication are likely to refill the other daily medications, including daily asthma medication. Our findings emphasize the evaluation of adherence on a routine basis in clinical practice. Future investigation is warranted to determine the opportunities for improving adherence in this population.
Acknowledgments
Grant sponsor: NIH (6/12/08–7/30/08); Grant number: TL1RR024995; Grant sponsor: NHLBI; Grant number: RO1HL079937; Grant sponsor: Burroughs Wellcome Foundation; Grant number: 1006671.
The Clinical and Translational Science Award provides support to establish the Washington University Institute of Clinical and Translational Sciences (ICTS). The Clinical Research Training Center—Predoctoral Program (TL1), component of ICTS, provides career development for medical and allied healthcare students through didactic coursework, mentored training, work-in-progress research discussions, and journal clubs and conferences.
References
- 1.White DA, Salorio CF, Schatz J, et al. Preliminary study of working memory in children with stroke related to sickle cell disease. J Clin Exp Neuropsychol. 2000;22(2):257–264. doi: 10.1076/1380-3395(200004)22:2;1-1;FT257. [DOI] [PubMed] [Google Scholar]
- 2.Screening for sickle cell disease in newborns: recommendation statement. Am Fam Physician. 2008;77(9):1300–1302. [PubMed] [Google Scholar]
- 3.Van der Dijs FP, Schnog JJ, Brouwer DA, et al. Elevated homocysteine levels indicate suboptimal folate status in pediatric sickle cell patients. Am J Hematol. 1998;59(3):192–198. doi: 10.1002/(sici)1096-8652(199811)59:3<192::aid-ajh3>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 4.Platt OS. Hydroxyurea for the treatment of sickle cell anemia. N Engl J Med. 2008;358(13):1362–1369. doi: 10.1056/NEJMct0708272. [DOI] [PubMed] [Google Scholar]
- 5.Raphael JL, Bernhardt MB, Mahoney DH, et al. Oral iron chelation and the treatment of iron overload in a pediatric hematology center. Pediatr Blood Cancer. 2009;52:616–620. doi: 10.1002/pbc.21929. [DOI] [PubMed] [Google Scholar]
- 6.Boyd JH, Macklin EA, Strunk RC, et al. Asthma is associated with acute chest syndrome and pain in children with sickle cell anemia. Blood. 2006;108(9):2923–2927. doi: 10.1182/blood-2006-01-011072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Knight-Madden JM, Forrester TS, Lewis NA, et al. Asthma in children with sickle cell disease and its association with acute chest syndrome. Thorax. 2005;60:206–210. doi: 10.1136/thx.2004.029165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elliott V, Morgan S, Day S, et al. Parental health beliefs and compliance with prophylactic penicillin administration in children with sickle cell disease. J Pediatr Hematol Oncol. 2001;23(2):112–116. doi: 10.1097/00043426-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Aday LA, Begley CE, Lairson DR, et al. A framework for assessing the effectiveness, efficiency, and equity of behavioral healthcare. Am J Manag Care. 1999;5(Spec No):SP25–44. [PubMed] [Google Scholar]
- 10.Gardiner P, Dvorkin L. Promoting medication adherence in children. Am Fam Physician. 2006;74(5):793–798. [PubMed] [Google Scholar]
- 11.Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;(2):CD000011. doi: 10.1002/14651858.CD000011.pub3. [DOI] [PubMed] [Google Scholar]
- 12.Julius RJ, Novitsky MA, Jr, Dubin WR. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34–44. doi: 10.1097/01.pra.0000344917.43780.77. [DOI] [PubMed] [Google Scholar]
- 13.Lehane E, McCarthy G. Medication non-adherence--exploring the conceptual mire. Int J Nurs Pract. 2009;15(1):25–31. doi: 10.1111/j.1440-172X.2008.01722.x. [DOI] [PubMed] [Google Scholar]
- 14.Wamboldt FS, Wamboldt MZ, Gavin LA, et al. Parental criticism and treatment outcome in adolescents hospitalized for severe, chronic asthma. J Psychosom Res. 1995;39(8):995–1005. doi: 10.1016/0022-3999(95)00507-2. [DOI] [PubMed] [Google Scholar]
- 15.Morris CR. Asthma management: Reinventing the wheel in sickle cell disease. Am J Hematol. 2009;84:234–241. doi: 10.1002/ajh.21359. [DOI] [PubMed] [Google Scholar]
- 16.Boyd JH, Macklin EA, Strunk RC, et al. Asthma is associated with increased mortality in individuals with sickle cell anemia. Haematologica. 2007;92(8):1115–1118. doi: 10.3324/haematol.11213. [DOI] [PubMed] [Google Scholar]
- 17.Andrade SE, Kahler KH, Frech F, et al. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15:565–574. doi: 10.1002/pds.1230. discussion 575–567. [DOI] [PubMed] [Google Scholar]
- 18.Thornburg CD, Calatroni A, Telen M, et al. Adherence to hydroxyurea therapy in children with sickle cell anemia. J Pediatr. 2010;156:415–419. doi: 10.1016/j.jpeds.2009.09.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weiden PJ, Kozma C, Grogg A, et al. Partial compliance and risk of rehospitalization among california medicaid patients with schizophrenia. Psychiatr Serv. 2004;55:886–891. doi: 10.1176/appi.ps.55.8.886. [DOI] [PubMed] [Google Scholar]
- 20.Grossberg R, Zhang Y, Gross R. A time-to-prescription-refill measure of antiretroviral adherence predicted changes in viral load in hiv. J Clin Epidemiol. 2004;57:1107–1110. doi: 10.1016/j.jclinepi.2004.04.002. [DOI] [PubMed] [Google Scholar]