Abstract
Infertility is a problem of global proportions, affecting on an average 8-12% of couples worldwide. Low sperm count (Oligozoospermia) is one of the main causes of male infertility and it is correlated with Kshina Shukra. The fruits of Gokshura (Tribulus terrestris. Linn) are considered to act as a diuretic and aphrodisiac; they used for urolithiasis, sexual dysfunctions, and infertility. Hence, it was planned to study the effect of Gokshura in the management of Kshina Shukra (Oligozoospermia), and to evade the preconception, a double-blind, randomized, placebo-controlled study was designed. In this study, eligible subjects between the age of 21 and 50 years, with a complaint of Kshina Shukra (Oligozoospermia), were randomized to receive either Gokshura granules or placebo granules for 60 days. The primary outcome measures were percentage changes in the Pratyatmaka Lakshanas (cardinal symptoms) of Kshina Shukra, Agni bala, Deha bala, Satva bala, the semenogram, and in the Quality of the Sexual Health Questionnaire. The placebo granules showed 70.95% improvement, whereas, the Gokshura granules showed 78.11% improvement in Rogi bala (Agni bala, Deha bala, Satva bala, and the Quality of Sexual Health) and Rogabala (Semen Analysis and Pratyatmaka Lakshanas). The Gokshura granules have shown superior results in the management of Kshina Shukra, as compared to the placebo granules.
Keywords: Gokshura, Kshina Shukra, Oligozoospermia, Tribulus terrestris
Introduction
Infertility is a problem of global proportions, affecting on an average 8-12% of couples worldwide.[1] Based on the National Women's Health Information Center (NWHIC), the annual incidence of male infertility is at least two million cases. Recent studies have indicated that the prevalence of Oligozoospermia is extremely high in the metropolis as well as in the smaller towns of India.[2]
Infertility is defined as the inability to achieve pregnancy after one year of unprotected coitus.[3] Male infertility is considerably to be less complicated than female infertility, but can account for 30-40% of infertility.[4] Except for some physical defects, low sperm count (Oligozoospermia) and poor sperm quality are responsible for male infertility in more than 90% of the cases. Out of these, in about 30 to 40% the cause is unexplained, and in the rest of the cases critical illness, malnutrition, genetic abnormalities, pollution, side effects of some medicines, hormones, and chemicals play a major role.[5]
More than 190 studies on Vajikarana (Aphrodisiac therapy)[6] have been carried out in various Ayurvedic Academic Institutes in India, at the PG and PhD level, wherein, researchers have considered various aspects of the problem, like its etiology, pathogenesis, and complications of the diseases related to the reproductive system, in both Ayurvedic and Modern parlance. Out of 190 studies more than 50 studies have been carried out on Oligozoospermia. The term Oligozoospermia is correlated in the research studies with Kshina Shukra (23 studies); Alpa Shukra (1 study); Shukra Dosha (3 studies); Shukra Dushti (13 studies); Shukra Kshaya (11 studies); Shukralpata (3 studies); Kshina Retas (1 study); Bijopaghata (1 study), and Shukradhatu Vikara (3 studies). Acharya Susruta has included Kshina Shukra under Shukra Dushti. Here, Vata dosha along with Pitta undergo vitiation and create a disturbance in the normal qualities and quantity of the Shukra Dhatu.[7] Oligozoospermia is a seminal disorder in which the sperm count is below 20 million/ml.[8]
However, it is evident that several studies were conducted on this subject, but only few studies have been carried out to recognize the clinical efficacy of single herbs, in this subject. Gokshura (Tribulus terrestris) is mentioned as a Vrishya (Aphrodisiac)[9] and also used in almost all prescriptions, along with other drugs, to treat the malady Kshina Shukra. Studies have suggested that Gokshura can enhance the hormone levels to within a normal range. It can increase the testosterone by increasing the luteinizing hormone and the gonadotropin-releasing hormone.[10] This hormone is effective in building muscles as well as improving fertility and libido, and it has also been proved to be active in stimulating spermatogenesis and sertoli cell activity in rats.[11] However, to generate an evidence based on this, this clinical study has been carried out on Gokshura for the role of Vrishya (Aphrodisiac).[12]
Aim of Study
The aim of this study is to find out the effect of Gokshura in the management of Kshina Shukra (Oligozoospermia).
Hypothesis
Gokshura is not effective in the management of Kshina Shukra as a Null Hypothesis. However, it is effective in the management of Kshina Shukra as an Alternate Hypothesis.
Materials and Methods
The methodology used for this study is explained as per the Consolidated Standards of Reporting Trials (CONSORT) Statement, 2010.[13]
A total of 72 patients with Kshina Shukra were selected from the Outpatient Department of the Institute for Postgraduate Teaching and Research Hospital, Gujarat Ayurved University, Jamnagar. The patients were divided into two groups, by following the Computer-Generated Randomization Plan. Out of them, 63 patients completed the treatment and they were divided into two groups — Group A – 31 patients and Group B – 32 patients — taking into consideration the inclusion and exclusion criteria.
Inclusion criteria
Age group between 21 to 50 years
Sperm count < 20 million/ml
Patients presenting with Pratyatmaka Lakshana (Cardinal Symptoms) of Kshina Shukra, with semen samples suggestive of Oligozoospermia, were selected.
Exclusion criteria
Age below 21 or above 50 years
Sperm count > 20 million/ml
Patients with azoospermia and aspermia
Genetic defects like Klinefelter's syndrome
Patients with diseases like varicocele, accessory sex gland infection, sexually transmitted diseases, systemic diseases like diabetes mellitus (DM), and so on, were excluded from this study.
Laboratory investigations
Routine hematological, biochemical, and urine examination, semen analysis, and Serum follicle-stimulating hormone (FSH), Serum luteinizing hormone (LH), and Serum Testosterone were carried out before and after the treatment, and a semenogram was carried out before treatment, on the thirtieth, sixtieth, and ninetieth, days of the study.
Ethical clearance
Ethical clearance was obtained from the Institutional Ethics Committee of IPGT and RA Jamnagar; Vide Ref-PGT/7/Ethics/2009-2010/3494/15 Dated: 8 February, 2010, before starting the study, and this study was registered in the Clinical Trial Registry of India, vide CTRI/2011/07/001907.[14]
Blinding
The prepared drugs were blinded and labeled as Group A and Group B by the Department of Rasa Shastra as the study was designed as a Double-blind Randomized Placebo-controlled study.
Method of allocation concealment
Both drugs in granule form were given, 6 g twice daily, before food, in the morning and night, with warm water, for 60 days.
Before dispensing the medicine, Koshtha Shuddhi (bowel cleansing therapy) was carried out with 20 ml of Eranda Taila (oil of Ricinus communis), in both the groups. After Koshtha Shuddhi (bowel cleansing therapy), a light diet was advised on the same day. The following day onwards the patients were given medicine and also allowed to take a normal diet.
Follow-up
The patients were advised to visit the hospital every fortnight during the treatment and for one month after the treatment for follow-up.
Criteria for assessment
The improvement in the patients was assessed mainly on the basis of relief in the signs and symptoms of Kshina Shukra (Oligozoospermia), improvement in the semenogram, especially in the total sperm count, and also in the serum FSH, LH, and testosterone level, improvement in Deha Bala, Chetasa Bala and Agni Bala, and improvement in the Quality of Sexual Life Questionnaire.[15]
Arbitration of criteria considered for assessment in the interpretation of results was as follows;
Roga Bala: 70% – Semen Analysis – 50%; Lakshanas – 20%
Rogi Bala: 30% – Agni Bala – 5%; Deha Bala – 5%; Chetsa Bala – 5%; Sexual Quality of Life (QoL) – 15%
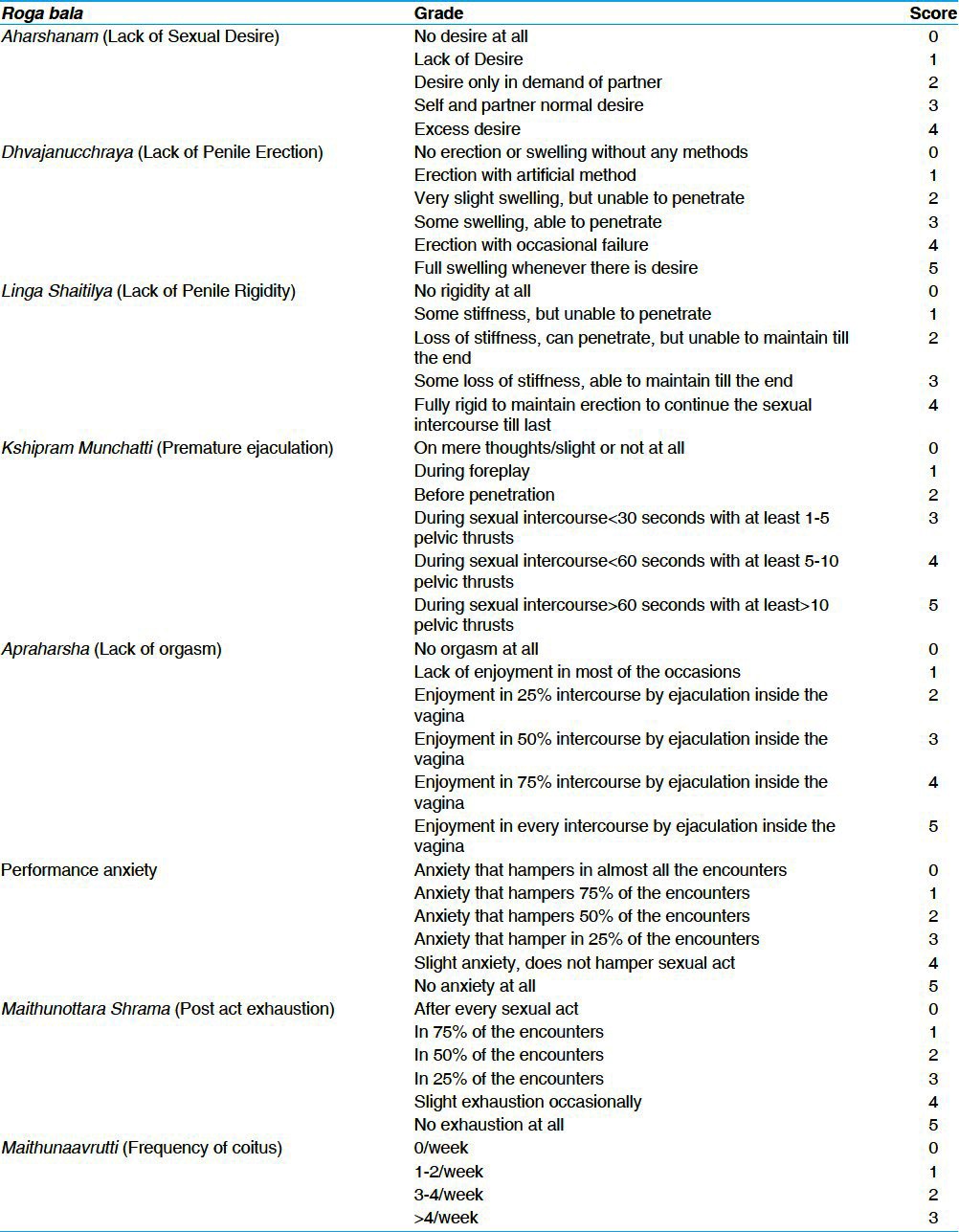
A. Roga Bala: Roga Bala was used to assess the signs and symptoms of Kshina Shukra. The details of the scoring pattern adopted for the assessment of the clinical signs and symptoms are given in Table 1.
Table 1.
Scoring pattern of Roga Bala
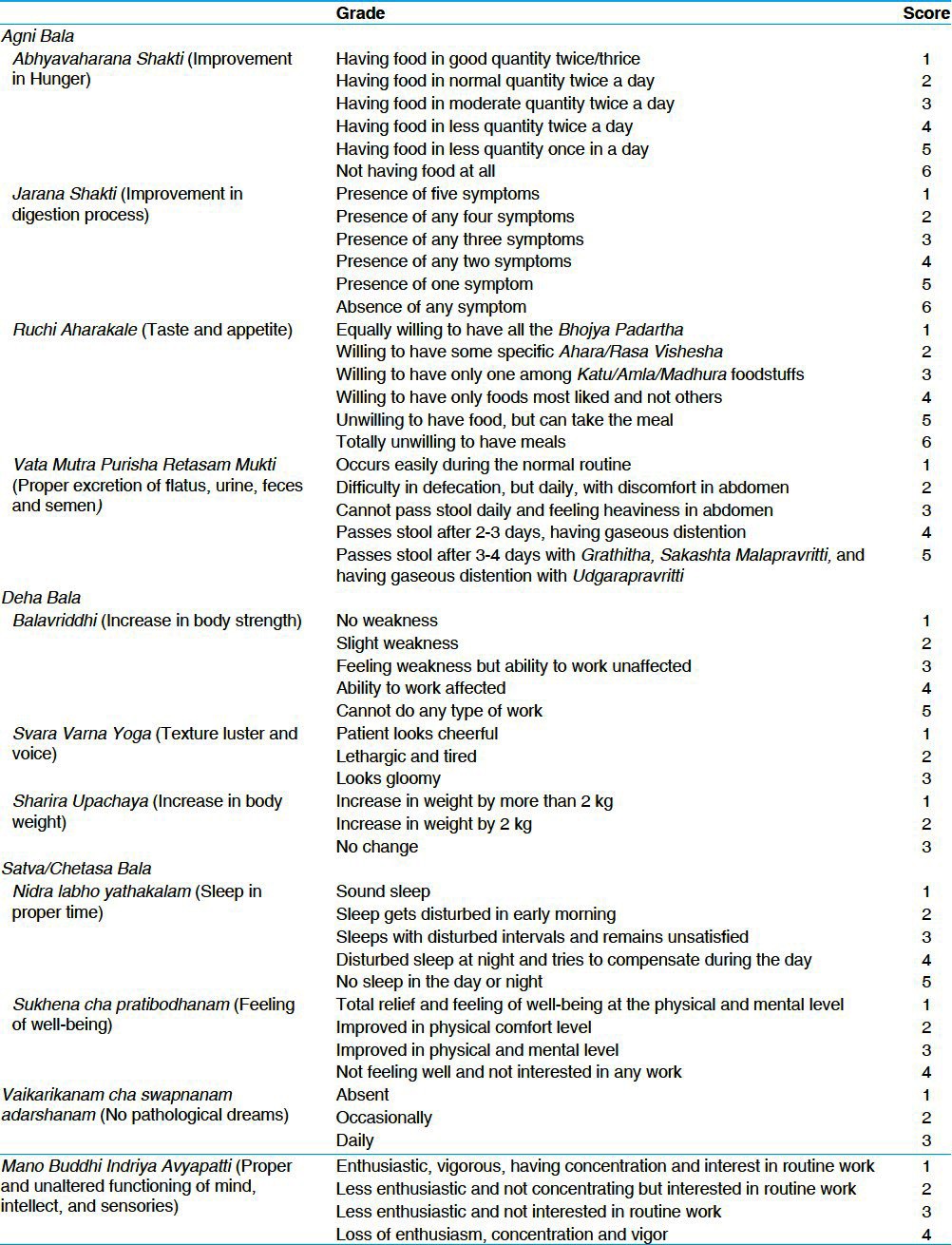
B. Rogi bala: Rogi bala, was assessed for any improvement in the Sexual QoL and in the symptoms of Agni Bala, Deha Bala, as well as Chetasa Bala, and the scoring patterns adopted are given in [Table 2].
Table 2.
Scoring pattern of Rogi Bala
Statistical analysis
The data generated in the clinical study was analyzed by applying the student's ‘t’ test[16] in the subjective and objective criteria of a single group, and to compare the effect of the therapy on the two groups. The obtained results were interpreted as:
Not significant (NS) : P > 0.05
Significant (S) : P < 0.05 or P < 0.01
Highly significant (HS) : P ≤ 0.001
Observations
The following flowchart depicts the figures of the clinical study. One hundred and fifty-two patients were screened during this study. Among them 80 patients were excluded, as they did not fulfill the eligibility criteria. Seventy-two patients fulfilling the eligibility criteria were randomly allocated by, using the Computerized Randomization Plan, into two groups, Group A with 37 patients and Group B with 35 patients, and were given intervention.
In Group A, out of 37 patients, six discontinued and in Group B, three patients discontinued out of 35; due to various reasons. Finally, the statistical analysis was completed on 63 patients, of which 31 patients belonged to Group A and 32 patients belonged to Group B.
In this study, the maximum number of patients belonged to the 21-30 years age group (46.25%), belonging to the Hindu religion (93.05%). They belonged to the lower middle class (45.83%), had primary level education (27.7%), were laborers (43.06%), and were exposed to occupational heat (59.72%). The maximum number of patients had Mandagni (43.05%) and Kapha Vata Prakruti (54.17%). All the patients of this study wer e found with a well-developed secondary character and they had a good relationship with their respective partners (94.44%).
The maximum number of patients were habituated to tobacco (58.33%) and most of the patients wore cotton undergarments (80.77%), tight underwear (67.31%), had a habit of warm water bath (37.5%), were mentally depressed (30.56%), were unaware of the fertility period (38.89%); and practiced Vegadharana (Suppression of urges) (83.33%).
It was observed that the maximum number of patients had primary infertility (66.67%) with severe oligozoospermic conditions (26.39%) for one to three years of chronicity (43.75%). With respect to symptoms of Kshina Shukra reported by the patients, they were Daurbalya (weakness), 52.78% Mukha Sosha (Dryness of Mouth), 47.22% Linga Shaithilya (Loss of Penile rigidity), and 45.83% Klaibya (Erectile dysfunction).
Results
Effect of therapy on symptoms
Group A: The granules provided a highly and statistically significant (P < 0.001) result in the case of Daurbalya (weakness) (48.14%), and significant (P < 0.05) results in cases of loss of penile erection (6.03%), loss of penile rigidity (9.41%), premature ejaculation (6.12%), lack of orgasm (9.76%), and performance anxiety (8.69%). The results were insignificant (P > 0.05) in the case of post-act exhaustion (1.33%), frequency of coitus (2.08%), Mukha Sosha (dryness of mouth) (6.66%), and depression (22.22%). However, Group B granules provided a highly and statistically significant (P < 0.001) result in Daurbalya (weakness) (78.26%), loss of penile erection (9.44%), loss of penile rigidity (17.02%), premature ejaculation (10.68%), lack of orgasm (13.54%), and post-act exhaustion (13.33%). Significant (P < 0.05) results were observed in frequency of coitus (18.36%) and performance anxiety (10.81%) and insignificant (P > 0.05) results in Mukha Sosha (Dryness of mouth) (18.75%) and depression (15.38%).
Effect of therapy in Agni bala, Deha bala, and Satva bala
Group A granules provided a highly statistically significant (P < 0.001) result giving Abhyavaharana Shakti (20.45%), Jarana Shakti (21.92%), Ruchi Hi Aharakale (12.05%), Balavriddhi (15.38%), Svaravarna Yoga (19.18%), a significant (P < 0.05) result in Sukhena Cha Pratibodhanam (8.57%), and Mano Buddhi Indriya Avyapatti (8.82%); and an insignificant (P > 0.05) result in Vata Mutra Purisha Retasam Mukti (7.5%), Sharira Upachaya (1.09%), and Nidra Labho yathakalam (5.56%). However, Group B Granules provided a highly statistically (P < 0.001) significant result giving Abhyavaharana Shakti (32.29%), Jarana Shakti (20.51%), Ruchi Hi Aharakale (19.04%), Balavriddhi (25.67%), Svaravarna Yoga (22.53%), a significant (P < 0.05) result in Vata Mutra Purisha Retasam Mukti (13.63%), Sukhena cha Pratibodhanam (7.57%), and Mano Buddhi Indriya Avyapatti (8.82%); and an insignificant (P > 0.05) result in Sharira Upachaya (1.11%) and Nidra Labho Yathakalam (7.84%).
Effect of therapy in hematological and biochemical parameters
There were no statistically significant changes (P > 0.05) in all hematological parameters like Hemoglobin, total red blood cell (RBC) count, total leukocyte count, and in the differential count in both the granules, as well as, in the biochemical parameters like fasting blood sugar (FBS), S. Cholesterol, S. Triglycerides, serum glutamic oxaloacetic transaminase (SGOT), serum glutamic pyruvic transaminase (SGPT), Total Protein, and so on. However, there was a change from the pre-test to post-test mean values of the above parameters, which was within the physiological limits. There was a statistically insignificant difference found in all of these parameters (P > 0.05). The difference found between the two groups was statistically insignificant. This proves that there was no adverse effect of the treatment.
Effect of therapy in hormones
S. Testosterone and S. FSH had decreased from 555.613 to 530.457 (4.53%↓), and 8.401 to 6.937 (17.42%↓), respectively, and S. LH had increased from 5.554 to 6.314 (13.7%↑) after treatment, in the Group A granules. However, the Group B granules had increased S. Testosterone from 515.69 to 599.81 (16.3%↑) and decreased S. FSH and S.LH from 10.812 to 6.998 (35.3%↓) and 6.673 to 4.444 (33.4%↓), respectively. There was a statistically insignificant difference found in all of these parameters (P > 0.05). On comparing the two groups on the effect of therapy on the hormones, it showed that it was statistically insignificant (P > 0.05) [Figure 1].
Figure 1.
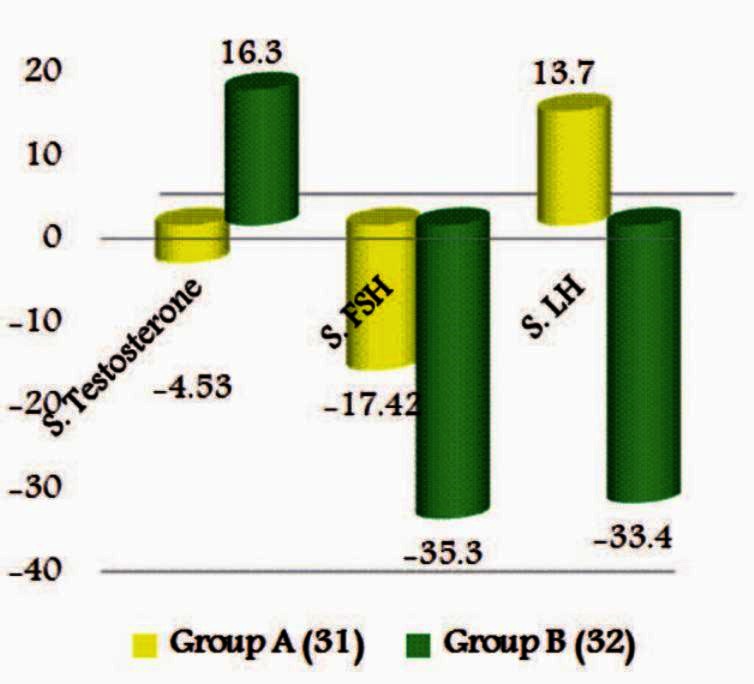
Effect of therapy on hormone
Effect of therapy in seminal parameter
The percentage of relief in Seminal Parameters like Sperm total count was 104.2%, and 25.42% in abnormal forms. Although Motility, RLP (Rapid Linear progressive), SLP (Slow Linear progressive), and NP (Non-progressive) had decreased, they were 12.05, 14.83, 16.55, and 18.45%, respectively. When subjected to statistical analysis, The total sperm count was found to be statistically significant, that is, P < 0.01. The remaining parameters were statistically insignificant in the Group A granules, whereas, in the Group B granules, percentage of relief in Seminal Parameters like Liquefaction time, volume, sperm total count, motility, RLP, SLP, NP, and abnormal forms was 3.32, 12.9, 86.31, 7.89, 20.1, 3.33, 7.53, and 12.25%, respectively. After subjecting the data to statistical analysis, the total sperm count and abnormal forms were found to be statistically highly significant (P ≤ 0.001). RLP was observed to be statistically significant, that is, P < 0.05 [Figure 2].
Figure 2.
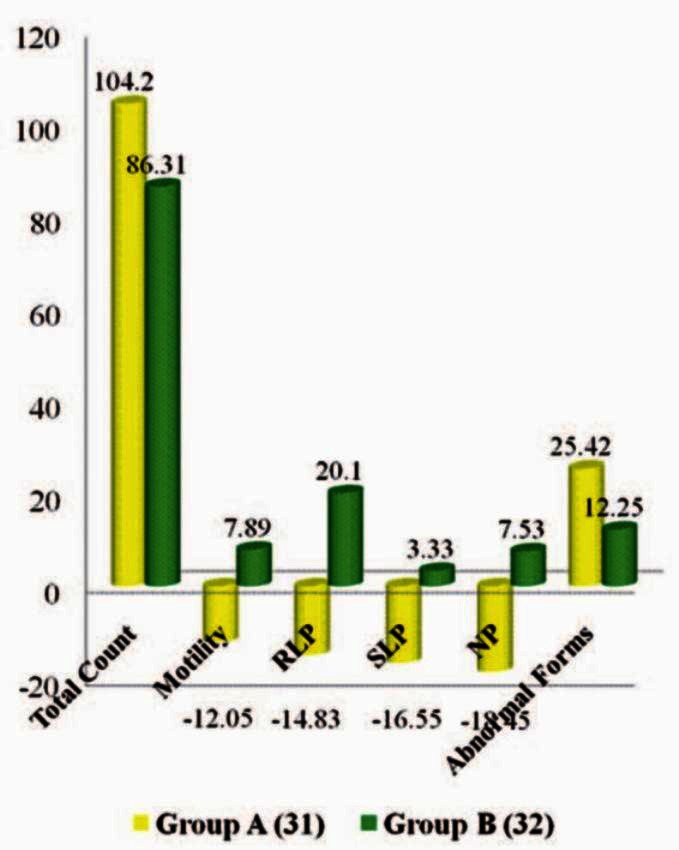
Effect of therapy on seminal parameters
In both groups, the total sperm count was recorded before treatment, at the end of the first, second, and third month, it was analyzed by the Kruskal-Wallis One Way Analysis of Variance on the Ranks test and it was observed that there was a statistically significant difference in both the groups, i.e. (P < 0.01). Even though, both the drugs increased the total sperm count on comparing the effect of therapy between the two groups, there was no statistically significant difference found (P > 0.05).
Effect of therapy on quality of sexual health
Group A granules provided 27.80% improvement and in Group B granules, 49.38% improvement was observed, which was highly significant (P ≤ 0.001). On comparing, there was a statistically significant difference found (P < 0.05) between both groups in the domain of sexual life, psychosexual, and Global index [Figure 3].
Figure 3.
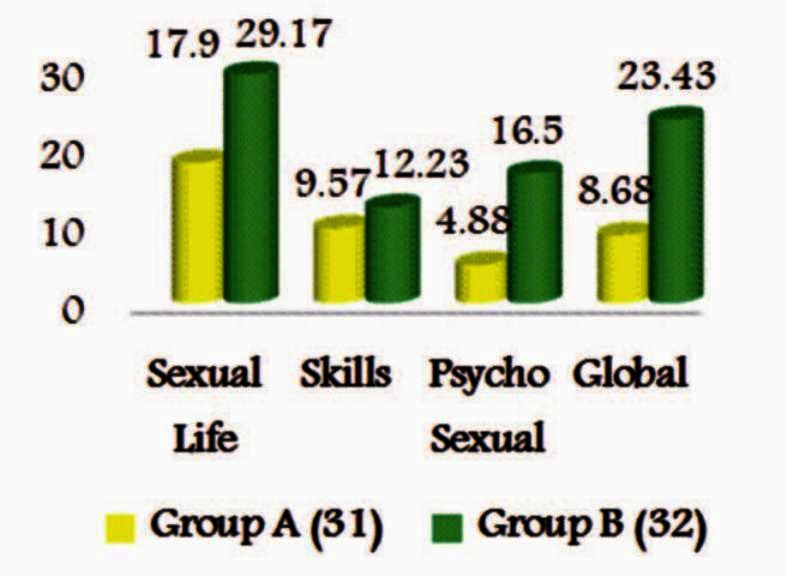
Effect of therapy on quality of sexual life
Overall effect of the therapy
Group A granules, showed 70.95% improvement and Group B Granules showed 78.11% improvement in Rogi bala (Agni bala, Deha bala, Satva bala, and Sexual QoL) and Rogabala (Semen Analysis and Lakshanas). One patient having Group A granules and two patients having Group B granules were able to impregnate their partners in the second month of treatment [Figure 4].
Figure 4.
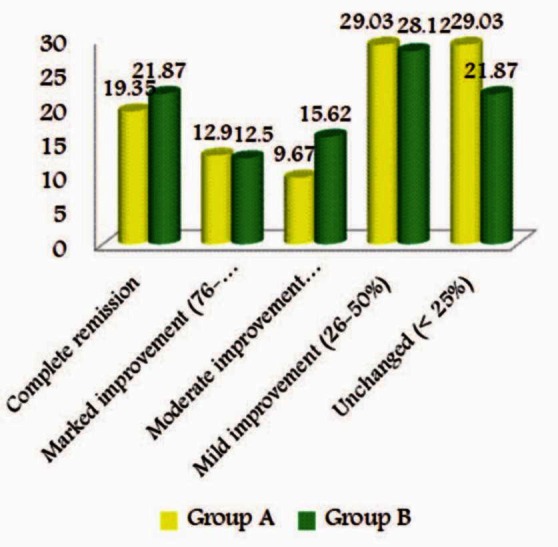
Overall effect of therapy
Discussion
The etiological factors classified under various headings such as chromosomal anomalies (Bijadosha) have been postulated to be one of the principal genetic factors in male infertility. These disorders occur due to the vitiation of the Bijabhaga of parents, which is responsible for the formation of Bija in the fetus.[17] Several somatic chromosomal abnormalities are associated with male infertility. A specific defect in the male sex (Y) chromosome can cause the common form of male infertility, that is, oligozoospermia.[18] Certain genetic disorders that cause oligozoospermia are Klinefelter's Syndrome, Kallmann's syndrome, Reifenstein's Sydrome, Testicular Malposition (Cryptorchidism), and so on.
Dietetic factors are described as Shukravaha Srotodushtikara Nidanas, particularly Anasana (Fasting),[19] Alpa-Pramitaasana (Inadequate diet),[20] and Visamaasana (Irregular diet),[21] which can impede the agni and may produce Shukradushti, which ultimately leads to impaired fertility. Deprived sustenance may alter the metabolism, which may result in dhatu kshaya. Shukra is the essence of all the former dhatus. Thus, any disturbances in the digestive process may lead to defective formation of Shukra, that is, Majjakshaya leads to Alpa Shukra.[22] Very low caloric or protein deficiency causes hypogonadism and decreases the function of the Leydig cell and further leads to infertility.[23] Kshara (Alkali), lavana (Salt), and Amla (Sour)[24] may cover the drugs of chemicals/pesticides described in modern medicine. The factors can be listed as Khavaigunyakara for Shukravaha srotas.
Viharaja Nidanas like excessive coitus (Ati maithuna), untimely coitus (Akala maithuna), coitus in other than vagina (Ayouvana maithuna), abstinence, intercourse with unaroused partner, coitus in old age (Jaraya Gamana), excessive exercise (Ati Vyayama), excessive exposure to heat (Ati-Ushna sevana),[25] and suppression of ejaculation (Shukravega Nigrahaha) are said to be responsible for the Shukravaha sroto dushti, which leads to Kshina Shukra.
The psychological causative factors are Chinta (worry), Bhaya (fear),[20] Krodha (anger), Shoka (depression), and so on, and unhealthy sexual/coital practices. Iatrogenic causative factors include improper Kshara (Alkali),[26] Agni (cauterization), and Sastra Karma (surgical procedures), anti-psychotic drugs such as[27] Cyproterone, Ketoconazole, and the like, disease-Induced factors include — diseases such as Hemorrhoids, Varicocele and so on, and other factors like smoking[28] and caffeine are also known causative factors of oligozoospermia.
The pathogenesis of Kshina Shukra is not mentioned in the classics, but it is stated that the vitiation of Vata and Pitta Dosha, is responsible for the manifestation of Shukrakshaya.[29] Mithyahara Vihara Sevana leads to Agnimandya as well as Amotpatti, hence, laeding to an improper formation of Ahara Rasa; which further leads to Rasa Kshaya due to the fault of Jatharagni, resulting in the depletion of the successive Dhatus and ending in Shukrakshaya. It has been said that the etiological factor affecting the Dhatus may also disturb the Doshas. This may also happen vice-versa. The Nidanas lead to Doshadushti, Khavaigunya, Dushya-daurbalya, and Dhatvagnimandya. This may happen simultaneously or gradually. In this case of Kshina shukra, the provocation of Vata and Pitta damages the Shukradhatu also, causing Shukradhatu Daurbalya and Shukravaha Srotodushti.
Acharya Sushruta has indicated that Lakshanas of Shukrakshaya should be considered as that of Kshina Shukra.[7] It must also be noted that Dalhana has described Kshina Shukra as Swa-Maanat Alpibhuta Shukra, which means the Shukra is of sub-normal parameters and this may be in terms of Dravyataha (by substance), Gunataha (by property), or Karmataha (by action). Hence, it is clear that many other symptoms of Shukrakshaya or Kshina Shukra may not be available in the patients, due to the selective Kshaya of sperm count. Hence, it is clear that except for a decrease in sperm count; the symptoms of Kshina Shukra may not be well-appreciated in patients. The sperms are nowhere related to the sexual and physical parameters.
Nidana Parivarjana (cessation of causative factors)[30] and Panchakarma[31] are recommended for treating the malady Kshina Shukra, before administrating the Vajikarana therapy. The main line of treatment in Kshina Shukra has been suggested to be ‘Kshine Shukrakari Kriya,’[32] and Upachaya[33] is the primary line of treatment. It can also be managed by a line of treatment advocated for Shukravaha Srotodushti and Dushtashukra Rogas. Doshapratyanika Chikitsa can be adopted, that is, Vataja and Pittaja Shukradushti for the better management of Kshina Shukra. The drugs that have Madhura Rasa (Sweet), Snigdha, Guru Guna (unctuous and heavy quality), Jivana (promotes quality of life), and Brimhana (nourishing property) are highly recommended for the management of Kshina Shukra.
Opening of the blinding
The Blinding Committee of the Department, in the presence of Scholar and guide, opened the sealed cover containing the information on blinding after the statistical analysis of the collected data was completed. On unmasking it, it was found that Group A consisted of Placebo granules and Group B had Gokshura Granules.
Probable mode of action of Gokshura granules
Gokshura has Madhura rasa (sweet), Guru and Snigdha guna (unctuous and heavy quality), Sheeta Virya (Cold in Potency), Vrishya (Aphrodisiac), Rasayana (Rejuvinator), Brimhana (Nourishing therapy), and Vatapittahara properties.[34] Vatapittahara Karma does the Samprapti Vightatana in the Kshina Shukra, as it is a Vata- and Pitta-predominant disease. However, Madhura Rasa, Snigdha, and Guru Guna increase the Shukra Dhatu qualitatively and quantitatively. Gokshura is known for its utility in Mutravaha Srotas,[9] by correction of the Apana Vata, it exerts action on the Shukra also, along the lines similar to how Shukra Visarga is goverened by Apana Vata.
Tribulus terrestris contains three groups of active phytochemicals. They are Dioscin, protodioscin, and diosgenin. Protodioscin is a potent natural precursor of the testosterone enhancer.[35] It also increases the production of Testosterone in another natural way. Tribulus leads to the production of the luteinizing hormone (LH). When the LH levels are increased, the natural production of testosterone also increases. LH is a hormone that also deals with sex drive. LH has been used to increase fertility and helps to relieve impotence.[35]
Probable mode of action of placebo
In present study barley powder was selected as the Placebo. The knowledge imparted regarding sexuality and fertility may be the reason behind the action of placebo, as psychological counseling has profound benefits on Shukra. The placebo effects presumably have different mediators depending on the specific learned association and whether it is referring to acquisition of the association or the placebo response. The central nervous system (CNS) is the primary location and mediator of the physiological basis of the placebo effect, through its role in learning and memory and its outputs on the sensory, motor, and autonomic pathways, as well as the immune and endocrine systems. People have individual traits that predispose them to be more or less responsive to certain stimuli; the interaction between the learned associations of the clinical situation and the person's particular biology produces a response. The response could be a basic physiological process, such as the modulation of sensory processing, release of neurotransmitters, or alterations in the hypothalamic–pituitary–adrenal axis or immune system activity. The placebo response could also be a slightly more complex physiological process, including change in mood, change in motivation/effort, or cognitive set-shifting.[36] Jon-Kar Zubieta published findings that the nucleus accumbens is central to the machinery of the placebo effect. His group has confirmed that specific neural circuits and neurotransmitter systems respond to the expectation of benefit during placebo administration, and that these expectations induce measurable physiological changes.[37]
Koshtha Shuddhi with Eranda Taila was carried out prior to administration of the granules. The Vatanulomana exerted by Eranda Taila corrects the gastrointestinal functioning by its properties of Deepana (Appetizer) and Pachana (Carminative).[38] Eranda Taila is widely prescribed as a Vatahara. Koshtha Shodhana increases the digestion and absorption of food and nutrients. Better bioavailability of food causes better nutrition to the Dhatus. Vatanulomana, especially correction of Apana Vata has its own benefits in Kshina Shukra. These are the possible mechanisms behind the placebo effect in the present study.
Conclusion
After detailed discussion on observations made and results achieved, this present study shows significant remission in the signs and symptoms of Kshina Shukra, vis-à-vis oligozoospermia, corroborated with definite improvement in the total sperm count. In toto, from this study it can be concluded that the Alternate Hypothesis of this study is accepted, that is, Gokshura is effective in the management of Kshina Shukra, with lifestyle modification. Gokshura Granules have shown superior results in the management of Kshina Shukra, as compared to placebo granules.
References
- 1.Inhorn MC. Global infertility and the globalization of new reproductive technologies: Lllustrations from Egypt. Soc Sci Med. 2003;56:1837–51. doi: 10.1016/s0277-9536(02)00208-3. [DOI] [PubMed] [Google Scholar]
- 2.Mehta RH, Makwana S, Ranga GM, Srinivasan RJ, Virk SS. Prevalence of Oligozoospermia and azoospermia in male partners of infertile couples from different parts of India. Asian J Androl. 2006;8:89–93. doi: 10.1111/j.1745-7262.2006.00050.x. [DOI] [PubMed] [Google Scholar]
- 3.Meletis CD, Barker J. Natural ways to enhance male fertility. Alternative and Complementary Therapies. 2004;10:22–7. [Google Scholar]
- 4.Norris S. PRB-00-32E. Ottawa: Parliamentary Information and Research Service, Library of Parliament; 2001. [Accessed on 2011 October 30]. Reproductive infertility: Prevalence, causes, trends and treatments. Available from http://www.parl.gc.ca/Content/LOP/researchpublications/prb0035-e.pdf . [Google Scholar]
- 5.Sharlip ID, Jarow JP, Belker AM, Lipshultz LI, Sigman M, Thomas AJ, et al. Best practice policies for male infertility. Fertil Steril. 2002;77:873–82. doi: 10.1016/s0015-0282(02)03105-9. [DOI] [PubMed] [Google Scholar]
- 6.Baghel MS. Researches in Ayurveda. In: Jain GK, editor. 2nd ed. Jamnagar: Mridu Ayurveda Publication and Sales; 2005. [Google Scholar]
- 7.Sushruta, Sushruta Samhita, Vaidya Jadavji Trikamji Acharya., editors. Sharira Sthana, Shukrashonita Shuddhisharira, 2/4. 9th ed. Varanasi: Chaukhamba Orientalia; 2007. p. 344. [Google Scholar]
- 8.World Health Organization. 4th ed. Vol. 10. Cambridge, United Kingdom: Cambridge University Press; 1999. WHO Laboratory Manual for the Examination of Human Semen and Sperm Cervical Mucus Interaction; p. 128. [Google Scholar]
- 9.Sharma PC, Yelne MB, Dennis TJ. Vol. 3. New Delhi: Central Council For Research In Aurveda and Siddha; 2002. Data base on medicinal plants used in Ayurveda; p. 229. [Google Scholar]
- 10.Pandya K, Solanki B, Maniar K, Gurav N, Bhatt S. Natural herbal supplements- A study on their nutritional value and their phytochemical constituents. International Journal of Pharmaceutical Sciences and Research. 2011;2:1480–94. [Google Scholar]
- 11.Anonymus. A monograph of identity, safety and clinical usage. Mumbai: CHEMEXCIL; 1992. Selected medicinal plants of India. A monograph Published by scientists at Bhavan's Swami Prakashananda Ayurvedic Research Centre; p. 325. [Google Scholar]
- 12.Bhavamishra, Bhavaprakash Nighantu. In: Reprint. Dr. Chunekar K.C, Dr. Pandey G.S, editors. Varanasi: Chaukambha Sanskrit Sansthan; 2004. p. 292. [Google Scholar]
- 13.Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332. for the CONSORT Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.2011. Jul 20, Available from: http://www.ctri.nic.in .
- 15.Costa P, Arnould B, Cour F, Boyer P, Marrel A, Jaudinot EO, et al. Quality of Sexual Life Questionnaire (QVS): A reliable, sensitive and reproducible instrument to assess quality of life in subjects with erectile dysfunction. [Last accessed on 2010 Feb 1];Int J Impot Res. 2003 15:173–84. doi: 10.1038/sj.ijir.3900995. 2003 Available from: http://www.nature.com/ijir . [DOI] [PubMed] [Google Scholar]
- 16.Mahajan BK. Biostatistics for medical students and research workers. 6th ed. New Delhi: J P Brothers medical publishers limited; 2006. Methods; pp. 168–85. [Google Scholar]
- 17.Agnivesha . In: Charaka, Dridhabala, Charaka Samhita. 5th ed. Yadavji Trikamji Acharya., editor. Varanasi: Chaukhamba Surbharati Prakashan; 2001. p. 303. Sharira Sthana, Atulyagotriyam, 2/18. [Google Scholar]
- 18.Poongothai J, Gopenath TS, Manonayaki S. Genetics of human male infertility. Singapore Med J. 2009;50:336–47. [PubMed] [Google Scholar]
- 19.Agnivesha . In: Charaka, Dridhabala, Charaka Samhita. 5th ed. Yadavji Trikamji Acharya., editor. Varanasi: Chaukhamba Surbharati Prakashan; 2001. p. 397. Chikitsa Sthana, Vijikaran Adhyaya, Puman Jatabaladikam- Vijikaran Padam, 2/4/43. [Google Scholar]
- 20.Agnivesha . In: Charaka, Dridhabala, Charaka Samhita. 5th ed. Yadavji Trikamji Acharya., editor. Varanasi: Chaukhamba Surbharati Prakashan; 2001. p. 103. Sutra Sthana, Kiyant Shirsiyam Adhyaya, 17/76. [Google Scholar]
- 21.Agnivesha . In: Charaka, Dridhabala, Charaka Samhita. 5th ed. Yadavji Trikamji Acharya., editor. Varanasi: Chaukhamba Surbharati Prakashan; 2001. p. 641. Chikitsa Sthana, Yoni Yvapat Chikitsadhyaya, 30/164-167. [Google Scholar]
- 22.Sushruta, Sushruta Samhita, Vaidya Jadavji Trikamji Acharya., editors. 9th ed. Varanasi: Chaukamba Orientalia; 2007. p. 69. Sutra Sthana, Doshadhatumalakshayavriddhi Vijnyaniya, 15/9. [Google Scholar]
- 23.Smith SR, Chhetri MK, Johanson J, Radfar N, Migeon CJ. The pituitarygonadal axis in men with protein-calorie malnutrition. J Clin Endocrinol Metab. 1975;41:60–9. doi: 10.1210/jcem-41-1-60. [DOI] [PubMed] [Google Scholar]
- 24.Agnivesha . In: Charaka, Dridhabala, Charaka Samhita. 5th ed. Yadavji Trikamji Acharya., editor. Varanasi: Chaukhamba Surbharati Prakashan; 2001. p. 143. Sutra Sthana, Aatrya Bhadrakapiya Adhyaya, 26/43-44. [Google Scholar]
- 25.Agnivesha . In: Charaka, Dridhabala, Charaka Samhita. 5th ed. Yadavji Trikamji Acharya., editor. Varanasi: Chaukhamba Surbharati Prakashan; 2001. p. 640. Chikitsa Sthana, Yoniyvapat Chikitsadhyaya, 30/135-138. [Google Scholar]
- 26.Agnivesha . In: Charaka, Dridhabala, Charaka Samhita. 5th ed. Yadavji Trikamji Acharya., editor. Varanasi: Chaukhamba Surbharati Prakashan; 2001. p. 503. Chikitsa Sthana, Arsha Chikitsa, 14/34. [Google Scholar]
- 27.Blair J, Simpson G. Effects of Antipsychotic drugs on reproductive functions. Dis Nerv Syst. 1966;27:645–7. [PubMed] [Google Scholar]
- 28.Banerjee A, Pakrashi A, Chatterjee S, Ghosh S, Dutta SK. Semen characteristics of tobacco users in India. Arch Androl. 1993;30:35–40. doi: 10.3109/01485019308988366. [DOI] [PubMed] [Google Scholar]
- 29.Sushruta, Sushruta Samhita, Vaidya Jadavji Trikamji Acharya., editors. 9th ed. Varanasi: Chaukamba Orientalia; 2007. p. 74. Sutra Sthana, Doshadhatumalakshayavriddhi Vijnyaniya,15/9. [Google Scholar]
- 30.Sushruta, Sushruta Samhita, Vaidya Jadavji Trikamji Acharya., editors. 9th ed. Varanasi: Chaukamba Orientalia; 2007. p. 597. Uttara Tantra, Aupadravikam Adhyaya, 1/25. [Google Scholar]
- 31.Agnivesha, editor; Yadavji Trikamji Acharya., editor. Charaka, Dridhabala, Charaka Samhita. 5th ed. Varanasi: Chaukhamba Surbharati Prakashan; 2001. p. 640. Chikitsa Sthana, Yoniyvapat Chikitsadhyaya, 30/126-127. [Google Scholar]
- 32.Vagbhata, Ashtanaga Hridaya, Dr. Anna Moreshwar Kunte., editors. Varanasi: Chaukambha Surabharati prakashana; 2002. p. 365. Sharira Sthana, Garbhavakranti Adhyaya, 1/14. [Google Scholar]
- 33.Sushruta, Sushruta Samhita, Vaidya Jadavji Trikamji Acharya., editors. 9th ed. Varanasi: Chaukamba Orientalia; 2007. pp. 2–3. Sutra Sthana, Vedotpatti Adhyaya, 1/7. [Google Scholar]
- 34.Anonymus. Part-I, Vol I. New Delhi: Ministry of Health And Family Welfare, Department of AYUSH, Government of India; The Ayurvedic Pharmacopoeia of India; p. 40. [Google Scholar]
- 35.Gauthaman K, Adaikan PG, Prasad RN. Aphrodisiac properties of Tribulus Terrestris extract (Protodioscin) in normal and castrated rats. Life Sci. 2002;71:1385–96. doi: 10.1016/s0024-3205(02)01858-1. [DOI] [PubMed] [Google Scholar]
- 36.Oken BS. Placebo effects: Clinical aspects and neurobiology. Brain. 2008;131:2812–23. doi: 10.1093/brain/awn116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brain region central to placebo effect identified. [Last accessed on Nov 01, 2011]. Available from: http://www.eurekalert.org/pub_releases/2007-07/cp-brc071607.php .
- 38.Bhavamishra, Bhavaprakash Nighantu. In: Reprint. Dr. Chunekar K.C, Dr. Pandey G.S, editors. Varanasi: Chaukambha Sanskrit Sansthan; 2004. p. 781. [Google Scholar]


