Abstract
Aim:
To analyze the HDU requirement in an obstetric population in terms of utilization rate, indications for admission, interventions required and gestational outcome.
Setting and Design:
A retrospective observational study was carried out from May 2007 to May 2011 in the Dept. of Obstetrics and Gynecology and HDU of IPGME and R, Kolkata.
Materials and Methods:
Data related to obstetric history, pre-existing medical problems, indications for HDU admission, interventions required, length of stay and outcome were collected and results were analyzed.
Results:
Our obstetric HDU utilization rate was 11.2 per 1000 deliveries. Out of total 57 subjects 48 had no prior antenatal care. Majority (68.42%) admitted in HDU with only obstetric reasons, while 31.57% required HDU for pre-existing medical diseases. The major obstetric indications were septicemia (35.08%), PPH (29.08%) and hypertension was observed in 21.05% of women. Other less common causes included post surgical acute kidney injury, APH, chrioamnionitis and pyelonephritis. Half of the women with pre-existing medical disease had cardiovascular problems. Patients with medical diseases had more pre-term labor (10 vs 5; P ≤ 0.05), respiratory failure (9 vs 2; P ≤ 0.05), cardiac failure (7 vs 1; P ≤ 0.05), duration of stay more than 10 days (15 vs 6; P ≤ 0.05), fetal growth restriction (6vs 3; P ≤ 0.05) and prolonged recovery time. Maternal mortality was 12.28% and fetal mortality was 17.54%.
Conclusion:
Early screening of high risk mothers, vigilant antenatal care and proper maintenance of asepsis during delivery and postpartum period can reduce HDU utilization rate and can result in healthier outcome.
Keywords: High dependency unit, obstetric indication, pre-existing medical disease, pregnancy
INTRODUCTION
Though pregnancy and labor are considered a physiological process the potential for catastrophic complications is constant and may develop in a matter of minutes. There are approximately 118 life threatening events of ‘near miss mortality’ or ‘severe acute maternal morbidity’ (SAMM) for each maternal death.[1] Global prevalence of SAMM (defined as severe life threatening obstetric complication necessitating urgent medical intervention in order to prevent likely death of the mother) varies from 0.015 to 8.23%.[2] It is these ‘near misses’ or ‘SAMM’ which require High dependency unit (HDU) interference. The UK Department of Health defined HDU care as a level of care which lies in between a general ward and an intensive care unit (ICU).[3] It typically involves the patients with single organ failure and patients who are at a high risk of developing life threatening complications.
In Western India the incidence of mothers requiring intensive care unit is around 5.48 per 1000 deliveries.[4] In Eastern India we retrospectively analyzed the demographic parameters, reason for admission, course of the stay, prognostic factors and final outcome in HDU requiring cases. The aim was to review the obstetric admissions to our institutional HDU in terms of HDU utilisation rate, indications for admission, interventions needed and ultimate fetomaternaloutcome.
MATERIALS AND METHODS
This retrospective cohort study was conducted from May 2007 to May 2011 in the department of Obstetrics and Gynaecology, IPGME and R, Kolkata after ethical permission was granted from institutional ethical committee. This is one of the biggest tertiary care and referral institutes in Eastern India. A dedicated 14 bedded HDU complying with standard recommendation of size, equipment, medical and paramedical staffs is present. Of the total 5052 deliveries conducted over a period of four years, 354 were referred cases with obstetric complications. A total these obstetric patients 57 parturients required HDU during their course of treatment and were included in this study. These were essentially patients with single organ failure. The records of all of these (both antenatal and puerperal) were reviewed. Complications were either obstetric or medical. Obstetric morbidity was defined as morbidity originating from any cause related directly to pregnancy or its management during antepartum, intrapartum or postpartum period (up to 42 days after delivery). Medical morbidity was described as complications arising from any pre-existing medical conditions. Maternal demographic characteristics included age, past obstetric history and history of any underlying medical disorder. Complications of either gestational or medical origin were noted. Relevant data regarding obstetric events, indications for HDU transfer/admission, interventions required, length of stay, eventual outcomes were collected, reviewed, tabulated and analyzed. Antenatal mothers were monitored clinically along with cardio tocography, biophysical profile and Doppler study. All patients were individualized and managed with invasive or non-invasive measures as and when required. Discharged women were regularly reviewed up to six months. Obstetric events were defined by standards of Williams’s Obstetrics 22nd edition.[5] Maternal outcome was evaluated in terms of morbidity and mortality. Statistical data was analyzed by Graph Pad Prism version 4.03 (Graph Pad Software. in corporation, 2005). Fisher's exact test was employed to compare categorical variables between study and control subjects. This test was employed with Freeman-Halton extension when required. Continuous variables were compared between two groups by Student's unpaired t test. A P value < 0.05 was considered statistically significant.
RESULTS
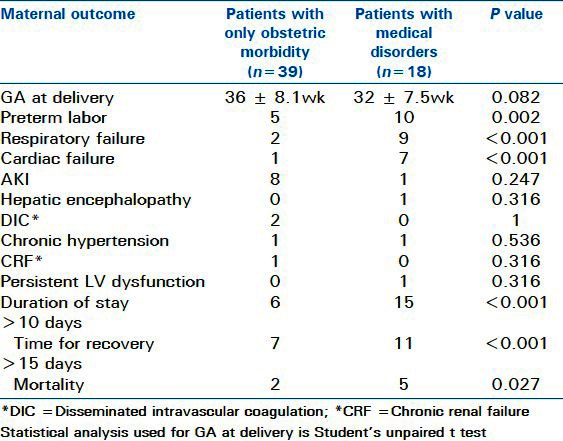
Demography of our study population revealed [Table 1] mean age of patients with only obstetric morbidity and cases with prior medical disease at 24.6 ± 4.23 and 24.9 ± 4.33 years respectively. Gestational age at delivery ranged between 8 and 40 weeks. Thirty one primipara (54.38%) and 26 multipara (45.61%) were observed to have required HDU admission. Mode of delivery was either vaginal or abdominal as per obstetric indication and a majority (73%) had delivered at home. Forty eight mothers (84.21%) received no prior antenatal care. On examination anemia was present in all patients [Table 2] with haemoglobin level ranging between 6 to 9 gm/dl. Hypotension, tachycardia and fever were observed in 29 (50.87%), 56 (98.29%) and 22 (38.59%) women respectively. Hypertension was present in 12 women with blood pressure ranged between 140/90 and 200/ 120mmhg. Other disease specific features were splenomegaly, gum bleeding and icterus. Interventions [Table 3] required during HDU stay were inotropes (14), antibiotics (57), mechanical ventilation (11) and central venous monitoring (23). Nine out of 10 patients with acute kidney injury (AKI) required hemodialysis while the tenth patient improved spontaneously on third day of delivery with antibiotics, inotropes and blood transfusion. Indications for HDU utilization as described in Table 4 showed that thirty nine (68.12%) women presented with various obstetric complications like; septicemia (20/57 = 35.08%), hypertension in 12 cases (21.05%) which included pre-eclampsia (7), eclampsia (3) and two women with HELLP (Hemolysis, elevated liver enzymes and low platelet count), postpartum hemorrhage (PPH) (17/57 = 29.82%), antepartum hemorrhage including one placenta previa and one abruption placenta case (2/57 = 3.5%), post surgical AKI (10/57 = 17.54%), uterine perforation during abortion (2/57 = 3.5%), uterine rupture due to placenta percetra (1/57 = 1.57%) and one ruptured ectopic pregnancy. Sepsis was mainly peureperal, postoperative, following criminal abortion or due to pyelonephritis, chrioamnionitis and following acute blood loss. One of these patients with attempted criminal abortion at 24 weeks of gestation had sigmoid colon injury, for which colostomy was initially carried out and then dead baby delivered vaginally. Post surgical AKI patients included 7 women with history of LSCS and 3 cases that required hysterectomy for PPH. Eighteen (31.57%) obstetric patients with medical disorders required HDU [Table 5]. The disorders included (PPCM) peripartum cardiomyopathy (4), systemic lupus erythematus (2), grade IV MS with twins(1), infective endocarditis with dengue (1), atrial tachycardia (1), idiopathic DCM (1), chronic demylinatingpolyneuro radiculopathy (CIDP) (1), acute pancreatitis (1), Takayasu arteritis (1), deep vein thrombosis (DVT) with pregnancy (1), thalassemia intermedia (1), hepatitis E (2) and one of the each patient with non specificaortoarteritis and acute gall bladder syndrome. Table 6 compared the patients with only obstetric complications with those having pre-existing medical disorders. Obstetric group (Group A) had mean gestational age of 35.8 ± 6 weeks at delivery where as patients with medical disorders (Group B) had 32.5 ± 9 weeks. Morbid sequelae like respiratory failure, cardiac failure, prolonged hospital stay and prolonged time for recovery were observed more with Group B. Five maternal deaths (8.77%) occurred in the group with medical disorders (Group B) compared to two (3.5%) in Group-A. Causes of maternal mortality in obstetric group were cardiac failure in eclampsia and post hemorrhage sepsis leading to multi-organ failure and DIC (disseminated intravascular coagulation). In Group-B mortality occurred in a patient with acute pancreatitis, one SLE case with grade IV nephropathy, one patient with PPCM who presented postpartum with ejection fraction (EF) at 23%, one patient with hepatitis E who developed hepatic encephalopathy and one patient with DVT succumbed after pulmonary embolism.
Table 1.
Demography particulars of the study population
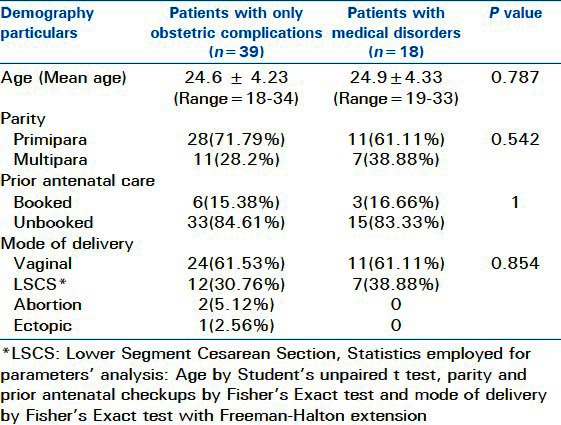
Table 2.
Clinical profile at admission in HDU
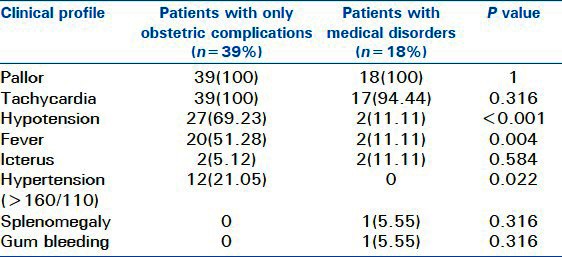
Table 3.
Investigations and interventions required in HDU
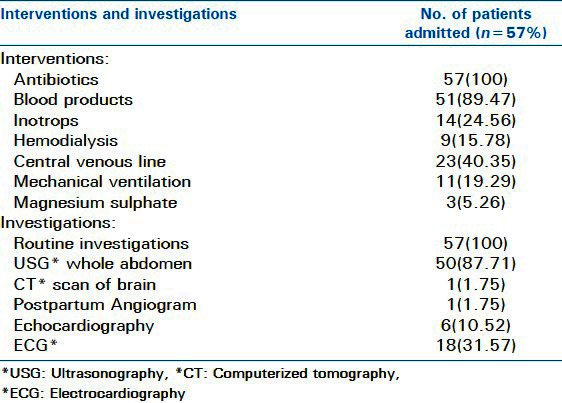
Table 4.
Observed obstetrical indications for admission in HDU
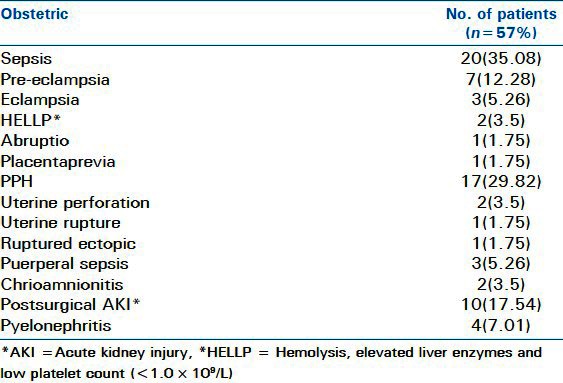
Table 5.
Observed medical indications for admission in HDU
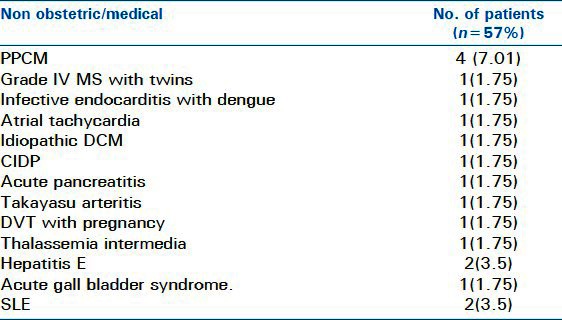
Table 6.
Comparison of obstetric and non obstetric group in terms of maternal outcome
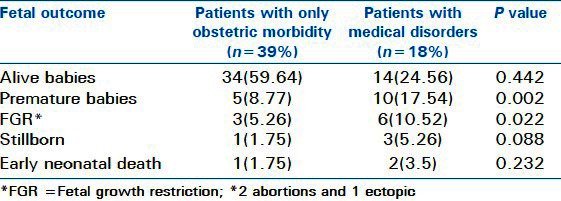
Fifty seven pregnancies resulted in 48 live births [Table 7]. Birth weight of the live babies ranged between 1,232 and 3,525 gms. Prenatal mortality included four stillborn babies and three early neonatal deaths. The two criminal abortions were at 6 and 24 weeks of gestation. One patient with eclampsia delivered still born at 32 weeks. In non obstetric group fetal demise was observed in SLE, PPCM, severe MS with twin pregnancy and the case with acute pancreatitis.
Table 7.
Comparison of obstetric and non obstetric group in terms of fetal outcome
DISCUSSION
During the 4 year study period 5052 mothers delivered and 57 patients required HDU admission. Thus obstetric admission in HDU was 11.2 per 1000 deliveries. This data from Eastern India differed from that of Western India, where incidence of ICU utilization by obstetric patients was 5.4 per 1000 deliveries, during 5 years.[4] The incidence varies widely among developed nations also:1.3 in 10 years in Hong Kong,[6] 2.4 over two years in Netherlands,[7] 10.2 in 4 years in Dublin (Ireland)[8] and 26.7 in 23 years in UK.[9] Unfortunately, data regarding HDU requirement for obstetric causes from other developing nations is lacking. It is interesting to note that despite gross socio – economic differences HDU/ICU utilization rate here, was almost comparable to some of the developed countries like Ireland and UK. Limited accessibility and inadequate availability of HDU, ICU services and higher mortality prior receiving medical attention may help explain this contradiction. We feel that this above incidence of HDU utilization reveals just the tip of the iceberg.
The indications leading to HDU admission were analyzed among the obstetric patients with only pregnancy induced complications. Sepsis accounted for the majority (35.08%) of admissions, followed by PPH (29.82%) and severe hypertensive disorders (BP³160/100MMHG)of pregnancy (21.05%). Common causes of sepsis were massive obstetric hemorrhage, chorioamnionitis, UTI, puerperal infections and sequelae of operative interventions including criminal abortions. The common offending pathogens were Escherichia coli, Klebsiella, Staphylococcus aureus, Pseudomonas aeruginosa, bacteroids and anaerobes. The underlying factors responsible for sepsis were unsupervised home delivery in unhygienic environment, failure to administer necessary antibiotics, rising trend of operative intervention and increased incidence of PPH occurring in the background of maternal malnutrition and anemia. It has been postulated that anemia predisposes to susceptibility to sepsis.[10] Of the whole study population forty eight (84.21%) cases were unbooked and referred with unsupervised no previous history of antenatal care. On analyzing the association of sepsis with surgical procedures, we observed that almost 21.05% (12/57) of cases developed sepsis after various operative procedures (two criminal abortions, seven LSCS and three hysterectomies indicated for PPH).
In other studies the important obstetric causes for HDU admission revolve around PPH and hypertensive disorders.[4,6–9] Sepsis ranked least in all the above series. Although in our study more commonly sepsis was associated patients requiring HDU for obstetric reasons only, while Hongkong study observed sepsis mostly among non obstetric cases.[6] In this study PPH and hypertensive disorders were the next two common causes. In rural India majority of the deliveries are conducted at home or at health centre's with inadequate infrastructure. Naturally unsupervised deliveries, dogmatic traditional approaches during birth, failure to use of uterotonics and underlying anemia continue to make PPH responsible for almost 28% of maternal mortality in India. It has been observed that anemia and poor nutrition contribute to the risk of hemodynamic compromise arising from blood loss during delivery and this increases the maternal morbidity. Regarding hypertensive patients requiring HDU care, the probable reasons appeared to be lack of timely diagnosis and inappropriate management coupled with ignorance of life threatening complications like HELLP and eclampsia.
Among non obstetric complications we observed various medical disorders necessitating HDU admission. Majority were patients with cardiac disease PPCM (4), grade IV MS with twins (1), infective endocarditis with dengue (1), atrial tachycardia (1) and idiopathic DCM (1). Similar observations were echoed in certain Western studies.[6,7,9] Again HDU admission was either emergency or anticipatory. Anticipatory admissions included a patient with atrial tachycardia requiring emergency LSCS and another with CIDP. Keeping in mind the imminent risk of respiratory failure in CIDP she was kept admitted in HDU and later delivered by LSCS at 35 weeks due to progressive fetal growth restriction (FGR) (baby weight 2.1kg). The patient with atrial tachycardia had a heart rate of 150-170/min in her last trimester, which remained refractory to treatment and ultimately subsided after delivering the baby. Emergency admissions included life threatening obstetrical complications along with medical disorders like SLE, MS with twins, Non specificaortoarteritis and hypertensive retinopathy with superimposed pre eclampsia etc. Immediate maternal disease related morbidities were significantly increased in the obstetric cases with prior medical disease, these included cardiac failure, respiratory failure, and prolonged hospital stay and increased recovery time. Majority of women from this group also delivered prior to term. In subsequent follow-up patients were found to have developed CRF (1), chronic hypertension (2) and persistent left ventricular dysfunction (1). In the present series patients with medical disorders had more mortality in comparison to obstetric group (5/18 vs. 2/39; P ≤ 0.05). Fetal outcome was also worse in the non obstetric category with more incidence of premature babies, FGR, still birth and early neonatal death. Maternal mortality was 12.28% and fetal mortality was 17.54% (stillborn-4, early neonatal death-3, abortions-2, ectopic-1). The other Indian study from Western India reported fetal and maternal mortality of 52% and 21.6% respectively.[4] In contrast in developed countries maternal mortality of HDU admissions was nil while prenatal mortality was 1.05% to 8%.[6,8] One salient point noted was that unbooked patients and those referred from remote rural areas had worse prognosis. In this study maternal mortality and or transfer to ICCU (Intensive Coronary Care Unit)/ITU (Intensive Therapeutic Unit) were taken as worst outcome end points. The main reasons were poor nutrition coupled with unsupervised births, illegal abortions, absence of modern diagnostic/therapeutic amenities, anesthetic hazards and finally delay in referral and necessary intervention. Karnad et al. also attributed high maternal age, absence of prenatal care, transfer to ICU> 24 hours after onset of acute problem and severity of illness at the time of admission as assessed by APACHE II score to be the factors responsible for maternal mortality.[4] We failed to find any significant relation between maternal mortality or morbidity with age, parity and gestational age.
Sepsis was the major indication for HDU admission followed by PPH and hypertension. Fetomaternal mortality was related to hypertensive and medical disorders during pregnancy. Comparatively favorable outcome was noted in patients with obstetric complications. Improved treatment strategies for obstetric hemorrhage and sepsis along with timely management of critically ill patients in the high-dependency unit may help decrease maternal mortality and morbidity as a high-dependency care unit fulfils the needs of at least half of the obstetric population who require higher acuity care and simultaneously save considerable expenditure. Emphasis on early detection of maternal problems and prompt referral to tertiary centers could minimize the prevalence of multiple organ failure and mortality in these women. Our findings highlight the need for establishing a high dependency unit in all such centre's in order to avoid unnecessary admission to the intensive care unit and to ensure proper management. Again, since puerperal morbidity has now become a focal parameter for quality of maternal care, a continued psychosocial follow-up of these patients should ideally be implemented to ensure better quality of life. This review is a reminder that constant vigilance, judicious judgment along with provision of adequate resources are still the major stepping stones on the road to maternal safety.
Footnotes
Source of Support: No support from outside
Conflict of Interest: No.
REFERENCES
- 1.Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: Case control study. BMJ. 2001;322:1089–93. doi: 10.1136/bmj.322.7294.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Say L, Pattison RC, Giilmezoglu AM. WHO systematic review of maternal morbidity and mortality: The prevalence of severe acute maternal morbidity (near miss) Reprod Health. 2004;1:3. doi: 10.1186/1742-4755-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guidelines on admission to and discharge from Intensive care and High Dependency units. London: DOH; 1996. Department of Health/NHS Executive. [Google Scholar]
- 4.Karnad DR, Lapsia V, Krishnan A, Salvi VS. Prognostic factors in obstetric patients admitted to an Indian intensive care unit. Crit Care Med. 2004;32:1294–9. doi: 10.1097/01.ccm.0000128549.72276.00. [DOI] [PubMed] [Google Scholar]
- 5.Cunningham FG, Lenovo KJ, Bloom SL, Hauth JC, Gilstrap L, Wenstorm KD, editors. 22nd ed. New York: McGraw Hill Companies; 2005. Williams obstetrics. [Google Scholar]
- 6.Leung NY, Lau AC, Chan KK, Yan WW. Clinical characteristics and outcomes of obstetric patients admitted to Intensive care unit: A 10 –year retrospective review. Hong Kong Med J. 2010;16:18–25. [PubMed] [Google Scholar]
- 7.Zwart JJ, Dupis JR, Ory F, Roosmalen J. Obstetric intensive care unit admission: A 2 year national wide population –based cohort study. Intensive Care Med. 2010;36:256–63. doi: 10.1007/s00134-009-1707-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryan M, Hamilton V, Bowen M, Mckenna P. The role of high dependency unit in a regional obstetric hospital. Anesthesia. 2000;55:1155–8. doi: 10.1046/j.1365-2044.2000.01627.x. [DOI] [PubMed] [Google Scholar]
- 9.Saravankumar K, Davies L, Lewis M, Cooper GM. High dependency care in obstetric setting in the UK. Anaesthesia. 2008;63:1081–6. doi: 10.1111/j.1365-2044.2008.05581.x. [DOI] [PubMed] [Google Scholar]
- 10.Santo LD, Romano G, Conte AD, Simone V de, Grimaldi F, Cotrufo M, et al. Pre-operative anemia in patients undergoing coronary artery bypass grafting predicts acute kidney injury. J ThoracCardiovascSurg. 2009;138:965–70. doi: 10.1016/j.jtcvs.2009.05.013. [DOI] [PubMed] [Google Scholar]


