Abstract
Objective
The course of lung function in community members exposed to World Trade Center (WTC) dust and fumes remains undefined. We studied longitudinal spirometry among patients in the WTC Environmental Health Center (WTCEHC) treatment program.
Methods
Observational study of 946 WTCEHC patients with repeated spirometry measures analyzed on the population as a whole and stratified by smoking status, initial spirometry pattern and WTC-related exposure category.
Results
Improvement in forced expiratory volume (FVC; 54.4 ml/year; 95% CI: 45.0-63.8) and forced expiratory volume in one second (FEV1; 36.8 ml/year; 95% CI: 29.3-44.3) was noted for the population as a whole. Heavy smokers did not improve. Spirometry changes differed depending on initial spirometry pattern and exposure category.
Conclusions
These data demonstrate spirometry improvement in select populations suggesting reversibility in airway injury and reinforcing the importance of continued treatment.
Background
The destruction of the World Trade Center (WTC) towers on September 11, 2011 released massive amounts of dust, gas and fumes with potential environmental and occupational exposures for thousands of individuals, including community members who lived (Residents) and worked (Local workers) in the area, as well as for those involved in rescue, recovery (Rescue/recovery workers) and clean-up (Clean-up workers). These groups were potentially exposed via inhalation to the initial WTC dust clouds created as the buildings collapsed, resuspended dust from incompletely cleaned indoor and outdoor areas, fumes from fires that burned for four months, and exposure from prolonged clean-up activities. (1) Settled outdoor and indoor dust was composed of highly alkaline materials (pH 11) consisting of pulverized concrete, fiberglass, glass, plastics and other building materials and contained polycyclic aromatic hydrocarbons, volatile organic compounds, lead, dioxin, and furans.(2), (3)
Persistent WTC-related adverse medical and mental health effects have been well described in rescue and recovery workers as well as in community members.(4-8) These studies suggest that most exposed symptomatic individuals have asthma-like symptoms. Detailed evaluations have suggested that many have bronchial hyperresponsiveness (9), small airways disease (10, 11) and some have interstitial lung disease. (12, 13) Two longitudinal studies of spirometry in rescue and recovery workers showed loss of lung function. (14, 15) Community members who lived or worked in the vicinity of the WTC towers have symptoms that are similar to those of rescue and recovery workers, but their potential exposures and demographics may differ (8). Longitudinal studies have not been reported for community members with potential WTC exposure.
The Bellevue Hospital Center World Trade Center Environmental Health Center (WTCEHC) is a medical and mental health treatment program that focuses on community members including Residents, Local workers, and Clean-up workers.(8) Launched in 2005 through joint efforts of the local communities, organized labor, and the medical community, the program was initially funded by philanthropic organizations and subsequently by city and federal agencies. Evaluation and treatment guidelines were developed for common health complaints, which were predominantly upper and lower respiratory symptoms, and patients were treated for asthma-like symptoms unless further evaluation revealed a different diagnosis. We now report longitudinal analyses of repeated spirometry measurements in patients who enrolled in the WTCEHC and presented for repeated treatment or monitoring between 2005 and 2011. Our objectives are to characterize longitudinal changes in spirometry in the WTCEHC population as a whole and after stratification for smoking, baseline lung function pattern, and WTC-related exposure category to assist our understanding of disease evolution in patients enrolled in the WTC medical treatment program.
Methods
Subjects
Individuals were self-referred to the WTCEHC with medical and/or mental health symptoms related to September 11, 2001 exposures as previously described. (8) The Institutional Review Board of New York University School of Medicine approved the research database (NCT00404898). Only data from patients who provided informed consent were used for analysis.
Procedures
Clinic protocol
At enrollment, patients responded to a multi-dimensional interviewer-administered questionnaire that included characterizations of WTC-related exposures and potential exposure category as Residents, Local worker, and Clean-up workers or Rescue/recovery, respiratory symptoms and history of tobacco use. The WTCEHC treatment protocol included treatment of asthma-like symptoms based on guidelines for asthma management,(16) with patients evaluated with additional studies if findings were inconsistent with an asthma diagnosis.
Spirometry
All individuals were referred for screening spirometry at time of enrollment, and at repeat clinic visits for therapeutic evaluation, or at visits scheduled for routine monitoring. Spirometry was performed in accordance with American Thoracic Society/European Respiratory Society standards (17) on a Viasys Vmax spirometer (Yorba Linda, CA). Spirometry data were electronically downloaded along with an automated quality assurance code. All studies were performed in the Bellevue Hospital Center Pulmonary Function (PFT) Laboratory. Data for pre-bronchodilator forced vital capacity (FVC) and forced expiratory volume in one second (FEV1) are presented in liters (L) or as % of predicted (% FVC and % FEV1) derived from NHANES III.(18) Patients were categorized as having a spirometry pattern of Normal, Low FVC, Obstructed, or Low FVC/obstructed at enrollment using definition based on the lower limits of normal as previously described.(19, 20)
Definitions
Individuals were classified as having WTC dust cloud exposure if they reported being in the initial WTC dust cloud from the collapsing buildings. Patients were characterized as Resident, Local worker, Rescue/recovery worker, Clean-up worker, or Other, based on their initial questionnaire responses about residence and workplace.(8) Patients who reported > 5 pack-year history of tobacco use were defined as heavy smokers. Respiratory symptoms were defined by at least one symptom of wheezing, chest tightness, dyspnea, or nasal or sinus symptoms with onset after September 11, 2001 and occurring with a frequency ≥ 2 times per week in the month before enrollment in the WTCEHC. A patient's “last visit” was considered the visit closest to December 12, 2011 when the analysis was conducted.
Patient selection
Patients were included for analysis if they had no respiratory symptom prior to September 11, 2001, had valid longitudinal spirometry defined as an acceptable baseline spirometry measurement, and had at least one valid repeated measurement. Patients with follow-up spirometry duration less than 90 days were excluded.
Statistical methods
Continuous variables were summarized using mean and standard deviation (SD) and compared across groups using the nonparametric Kruskal-Wallis test. Categorical variables were summarized by counts and proportions and compared using Chi-square test. (21) Crude estimates of within-individual annual change of spirometry measurements were calculated as the difference between the last and first spirometry measurements divided by the time duration. Initial analyses using these crude estimates as outcomes examined potential factors that might be associated with the temporal change in spirometry, so these could subsequently be used as stratification variable in longitudinal analysis. We considered the following variables: age at baseline, gender, race/ethnicity, income, body mass index (BMI), smoking status, dust cloud exposure, WTC-related exposure category and baseline spirometry patterns. A linear mixed-effects model was used to investigate longitudinal changes of lung function using all repeated spirometry measurements.(22, 23) Separate models were fit with FVC, % FVC, FEV1 and % FEV1 as dependent variables for the entire longitudinal population and subsequently for strata defined by smoking status, baseline spirometry pattern or WTC exposure category. In each model, a fixed linear effect of the follow-up time (defined as duration since joining the program) was estimated with adjustment for potential confounders. Random intercept and slope were assumed to explain within-subject correlation among repeated measurements and among-subject heterogeneity. We used the alpha level of 0.05 to declare significance for tests and analyses in the whole population, and alpha level of 0.01 in the stratified analyses to account for multiple testing issue. Statistical analyses were conducted using SAS (version 9.2).
Results
Baseline characteristics
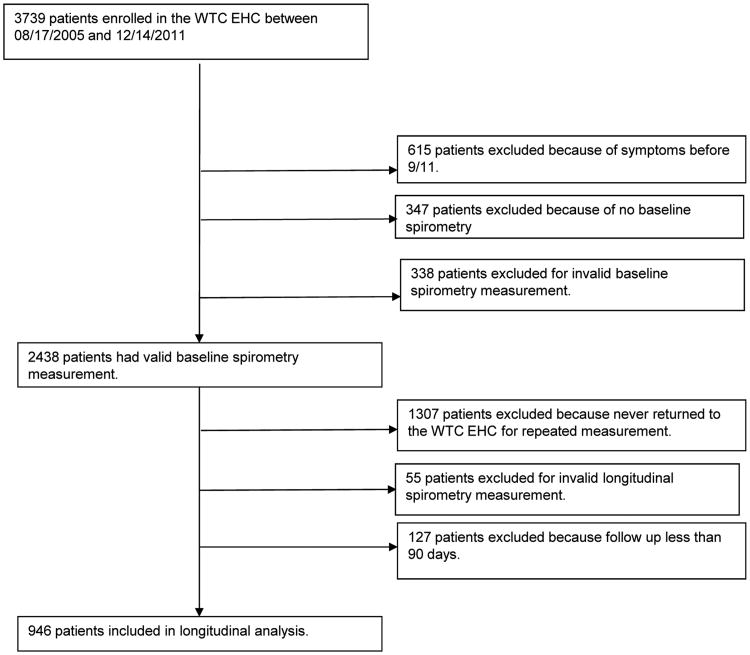
The final study population consisted of 946 subjects who enrolled in the WTCEHC between August 17, 2005 and December 14, 2011, had new onset and persistent respiratory symptoms, and fit criteria for longitudinal assessment (Figure 1). The population was diverse as can be seen by the characteristics of the study population (Table 1): 478 (50.5%) were female and 429 (52.5%) were Hispanic. Many, 445 (47.6%) reported being caught in the WTC dust cloud. The largest group with potential WTC exposure was the Local worker group (438; 46.3%). Heavy smokers comprised 21.1% of the group (196; 21.1%). Most (86.1%) had current respiratory symptoms.
Figure 1. Flow diagram of patient identification for longitudinal analysis.
Table 1.
Baseline characteristics of the WTC EHC longitudinal population (N=946) as whole and stratified by baseline spirometry pattern.
| Variable a | Longitudinal population N=946 | Normal N=642 | Low FVC N=193 | Obstructed N=75 | Low FVC/obstructed N=36 | p-value b |
|---|---|---|---|---|---|---|
| Age | 0.16 | |||||
| Mean(SD) | 50.2(11.1) | 50.0(11.4) | 50.5(10.2) | 49.6(10.8) | 53.5(11.3) | |
| Gender N(%) | 0.08 | |||||
| Female | 478(50.5) | 340 (53.0) | 93 (48.2) | 32(42.7) | 13(36.1) | |
| Male | 468(49.5) | 302 (47.0) | 100(51.8) | 43(57.3) | 23(63.9) | |
| Race/Ethnicity N(%) | <.0001 | |||||
| Hispanic | 429 (52.5) | 304(47.4) | 88(45.6) | 28(37.3) | 9(25.0) | |
| White | 257 (27.2) | 173(27.0) | 41(21.2) | 25(33.3) | 18(50.0) | |
| Black | 163(17.2) | 118(18.4) | 26(13.5) | 15(20.0) | 4(11.1) | |
| Asian | 68(7.2) | 32(5.0) | 28(14.5) | 5(6.7) | 3(8.3) | |
| Other | 29(3.1) | 15(2.3) | 10(5.2) | 2(2.7) | 2(5.6) | |
| Income/year | 0.05 | |||||
| ≤15K | 434(46.8) | 284(45.0) | 104(55.3) | 33 (45.2) | 13 (37.1) | |
| 15K-30K | 155(16.7) | 108(17.1) | 31(16.5) | 13 (17.8) | 3(8.6) | |
| >30K | 338(36.5) | 239(37.9) | 53(28.2) | 27(37.0) | 19(54.3) | |
| BMI N(%) | 0.0023 | |||||
| Normal | 249(26.3) | 164(25.6) | 47(24.4) | 33(44.0) | 5(13.9) | |
| Over weight | 353(37.3) | 248(38.6) | 63(32.6) | 25(33.3) | 17(47.2) | |
| Obesity | 344(36.4) | 230(35.8) | 83(43.0) | 17(22.7) | 14(38.9) | |
| Tobacco N(%) | 0.0016 | |||||
| ≤5pack-year | 733(78.9) | 512(81.1) | 151(79.5) | 46(63.0) | 24(68.6) | |
| >pack-year | 196(21.1) | 119(18.9) | 39(20.5) | 27(37.0) | 11(31.4) | |
| Caught in WTC dust cloud N(%) | 0.93 | |||||
| No | 489(52.4) | 330(52.1) | 104(54.2) | 37(50.0) | 18(51.4) | |
| Yes | 445(47.6) | 303(47.9) | 88(45.8) | 37(50.0) | 17(48.6) | |
| WTC exposure category N(%) | 0.014 | |||||
| Local worker | 438(46.3) | 294(45.8) | 94(48.7) | 30(40.0) | 20(55.6) | |
| Clean up worker | 247(26.1) | 185(28.8) | 45(23.3) | 12(16.0) | 5(13.9) | |
| Resident | 172(18.2) | 108(16.8) | 39(20.2) | 20(26.7) | 5(13.9) | |
| Rescue/recovery | 67(7.1) | 42(6.5) | 13(6.7) | 8(10.7) | 4(11.1) | |
| Other | 22(2.3) | 13(2.0) | 2(1.0) | 5(6.7) | 2(5.6) | |
| Respiratory symptoms | 0.21 | |||||
| No | 130(13.9) | 94(14.8) | 28(14.7) | 6(8.2) | 2(5.7) | |
| Yes | 802(86.1) | 540(85.2) | 162(85.3) | 67(91.8) | 33(94.3) |
Data were missing on “Caught in WTC dust cloud” for 12 subjects, “Income” for 19 subjects, “Tobacco” for 17 subjects, and “Lower respiratory symptom” for 14 subjects.
P-value were from Chi-square or ANOVA tests comparing baseline characteristic across spirometry pattern subgroups of the longitudinal population.
When classified by baseline spirometry pattern (Table 1), the most common abnormal pattern was Low FVC, a finding similar to that previously published.(8, 15, 19, 24) Distributions of Race/ethnicity, BMI, and tobacco differed among spirometry patterns. WTC dust cloud exposure was not associated with baseline spirometry pattern, whereas the distribution of WTC exposure categories differed among spirometry patterns (p = 0.014) with the Low FVC/Obstructed group having the highest proportion of Local workers.
Longitudinal analysis
The average number of repeated observations was 3 (range 2-10). The average duration of follow-up was 2.43 years (SD = 1.37 years) and the longest was 5.94 years. Initial analyses, based on crude estimates of individual annual change (Appendix Table 1), indicated that smoking status, spirometry pattern and WTC-related exposure category might be associated with the temporal change of FVC, % FVC, FEV1, and % FEV1, but not WTC dust cloud exposure or the presence of respiratory symptoms. Therefore, we conducted longitudinal analyses in the population as whole and then stratified by smoking status, spirometry pattern and WTC-related exposure category.
Annual change of FVC, % FVC, FEV1, and % FEV1 estimated via linear mixed-effects models adjusted for appropriate variables, as shown in Table 2, revealed significant improvement in spirometry parameters in the overall sample: with a 54.4 ml/year improvement in FVC (95% CI: 45-63.8) and a 36.8 ml/year in FEV1 (95% CI: 29.3-44.3). These changes translated into a 1.37 %/year (95% CI: 1.11-1.64) improvement in % FVC and a 1.12 %/year (95% CI: 0.85-1.38) improvement in % FEV1. Temporal trends in lung function differed between heavy-smokers and non- or light- smokers (Table 2), with the non- or light- smoker group showing significant (p<0.0001) improvement in all spirometry parameters, whereas no improvement was observed among heavy smokers.
Table 2.
Estimates of the linear annual change of FEV1 and FVC (ml/year) and FEV1% and FVC% (percent/year) from the linear mixed-effects model for the total longitudinal population1, each lung pattern subgroup1, and each smoking category2.
| FVC | FVC% | FEV1 | FEV1% | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. | Estimate a | 95% CI | Estimate a | 95% CI | Estimate a | 95% CI | Estimate a | 95% CI | |
| Total population1 | 946 | 54.4*** | (45.0,63.8) | 1.37*** | (1.11,1.64) | 36.8*** | (29.3,44.3) | 1.12*** | (0.85,1.38) |
| Smoking status2 | |||||||||
| Light/none | 733 | 60.2*** | (50.3,70.2) | 1.49*** | (1.21,1.78) | 41.9*** | (33.7,50.2) | 1.25*** | (0.96,1.54) |
| Heavy | 196 | 25.6 | (-1.1,52.3) | 0.81 | (0.14,1.49) | 13.1 | (-4.7,30.9) | 0.47 | (-0.17,1.11) |
| Spirometry pattern3 | |||||||||
| Normal | 642 | 47.3*** | (36.5,58.2) | 1.16*** | (0.85,1.47) | 29.2*** | (20.7,37.7) | 0.82*** | (0.50,1.14) |
| Low FVC | 193 | 72.8*** | (52.9,92.6) | 2.02*** | (1.50,2.54) | 37.8*** | (22.9,52.8) | 1.31*** | (0.81,1.82) |
| Obstructed | 75 | 17.9 | (-26.5,62.4) | 0.14 | (-1.18,1.45) | 50.2* | (14.2,84.2) | 1.45 | (0.21,2.69) |
| Low FVC/Obstructed | 36 | 122.4* | (45.0,199.8) | 3.93*** | (2.18,5.68) | 153.1*** | (82.0,224.3) | 5.13*** | (2.98,7.28) |
| Exposure category4 | |||||||||
| Local worker | 438 | 28** | (13.0,43.0) | 0.91*** | (0.51,1.32) | 24.6*** | (12.3,36.8) | 0.81** | (0.39, 1.23) |
| Resident | 172 | 59.5*** | (31.3,87.7) | 1.71*** | (0.84,2.57) | 44.5*** | (25.4,63.5) | 1.57** | (0.76,2.38) |
| Rescue/recovery | 67 | 122.8*** | (86.1,159.6) | 3.01*** | (2.22,3.81) | 80.4*** | (52.3,108.5) | 2.47*** | (1.68,3.26) |
| Clean-up worker | 247 | 61.3*** | (46.3,76.3) | 1.42*** | (1.02,1.82) | 36.3*** | (24.2,48.4) | 0.95 | (0.53,1.37) |
Linear mixed effects model with a linear term of time was adjusted for baseline age, BMI, gender, race/ethnicity, income, dust-cloud exposure, WTC exposure category, smoking status, and baseline spirometry pattern.
Linear mixed effects model with a linear term of time within each smoking group was adjusted for baseline age, BMI, gender, race/ethnicity, income, dust-cloud exposure, WTC exposure category, and baseline spirometry pattern.
Linear mixed effects model with a linear term of time within each spirometry pattern group was adjusted for baseline age, BMI, gender, race/ethnicity, income, dust-cloud exposure, WTC exposure category, and smoking status.
Linear mixed effects model with a linear term of time within each exposure category was adjusted for baseline age, BMI, gender, race/ethnicity, income, dust-cloud exposure, smoking status, and baseline spirometry pattern.
: P-value<0.01;
: P-value<0.001;
: P-value<0.0001
Longitudinal analysis and spirometry pattern
Changes in longitudinal spirometry differed between each spirometry pattern group (Table 2). The Normal group demonstrated improvement in both FVC and FEV1: FVC (47.3; 95% CI: 36.5-58.2), % FVC (1.16; 95% CI: 0.85-1.47), FEV1 (29.2; 95% CI: 20.7-37.7) and % FEV1 (0.82; 95% CI: 0.5-1.14). In the groups with abnormal spirometry, the Low FVC group and the Low FVC/Obstructed group demonstrated significant increases in all spirometry parameters. In contrast, the Obstructed group only showed a significant increase in FEV1 (50.2; 95% CI: 14.2-84.2). The Low FVC/Obstructed group had the greatest improvement for both FVC and FEV1.
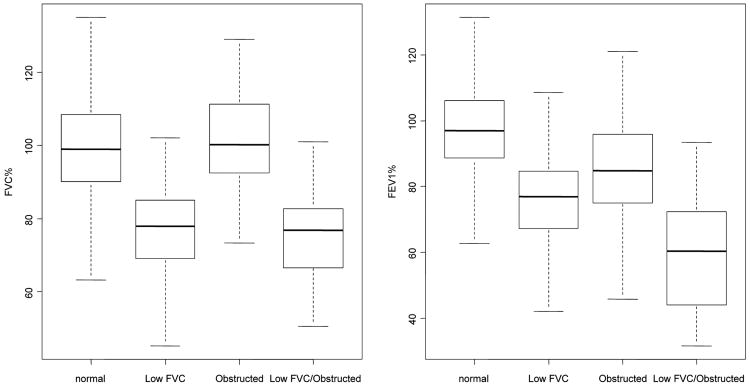
We further examined spirometry measurements as predicted values at the participants' last visit to the WTCEHC stratified by initial spirometry patterns (Figure 2). At their last visit, the Low FVC group and the Low FVC/Obstructed group continued to have abnormal spirometry with median values of % FVC and % FEV1 less than 80%. The Obstructed group had lower FEV1 measurements compared to the Normal group at the last visit.
Figure 2. Boxplots of spirometry parameters at last-visit for each lung function subgroup1.
1Outlier data points more than 1.5 times the interquartile range from the box are not shown.
Longitudinal spirometry and WTC exposure category
When stratified by WTC-related exposure category (Table 2), longitudinal analysis indicated statistically significant improvement in all lung function parameters among Local worker, Resident, Rescue/recovery and Clean-up workers, with the exception of % FEV1 among the Clean-up group (p ≥ 0.01). The Rescue/recovery group demonstrated the greatest annual improvement in all lung function parameters, whereas the Local worker group showed the least improvement.
Discussion
We report longitudinal assessment of spirometry parameters in a group of community members with potential for WTC dust exposures. Our analyses of a group of patients with heterogeneous exposures to environmental contaminants related to the September 11 disaster showed statistically significant temporal improvements in lung function in the group as a whole, with the degree of improvement varying by the pattern of spirometry at enrollment, the category of WTC-related exposure, and smoking status.
We demonstrated overall improvement in spirometry parameters during an average 2.4-year follow-up period in this community cohort enrolled in a treatment program about four years after the WTC disaster on September 11, 2001. These data are in contrast to longitudinal analyses of lung function in those involved in rescue and recovery.(15), 19 In firefighters, an initial loss of lung function was detected within the first year after exposure with subsequent decline in lung function approximating the expected age related change.(14) Analysis of an additional rescue and recovery population also demonstrated a reduction of lung function over time although analysis was limited by lack of antecedent data.(15) Our baseline observational period started four years after the event, and unlike data in firefighters, we did not have lung function data prior to or within the immediate years after exposure. The increase in spirometry measurements is also in contrast to the anticipated loss of 31 ml/year in FEV1 that has been reported in longitudinal studies of non-smokers with asthma and the loss in lung function in patients with COPD.(25, 26)(27) The improvement in lung function in the WTCEHC population suggests the presence of a reversible component of lung injury in the population despite the delayed time of entry into the treatment program.
We demonstrated heterogeneity in response over time among the spirometry patterns. The distribution of the four spirometry patterns in our population was consistent with other populations (19) and with the spectrum of diseases that have been described for WTC exposed individuals, which include reactive airways dysfunction, irritant-induced asthma, sarcoidosis and other interstitial lung diseases.(4, 6, 12, 28, 29) The variability in improvement among the four spirometry patterns suggests different mechanisms for the development of each pattern. A Normal spirometry pattern can be seen in patients without any underlying lung disease, but is also consistent with asthma or airway hyper-responsiveness. Alternatively, exposed patients with the normal pattern may have distal airway disease that is not reflected by spirometry.(30, 31) Indeed, the improvement in FVC in this population, and the absence of decline in FEV1, suggested the presence of reversible airway closure even in this group with a Normal spirometry pattern. Although most patients with WTC exposures and lower respiratory symptoms have been suggested to have asthma, an Obstructed pattern is uncommon in this as well as other reported WTC exposed cohorts. (19)The Obstructed group improved both FVC and FEV1 parameters, consistent with airway disease. The Low FVC pattern has been described as the predominant spirometry abnormality in WTC-exposed populations.(19) A reduced FVC can be consistent with sub-maximal effort, parenchymal disease, obesity, or alternatively can be associated with patchy peripheral air trapping.(20) Patients with the Low FVC pattern predominantly improved FVC over time, consistent with a component of reversible airflow obstruction. Patients with the combined Low FVC/Obstructed pattern had the most abnormal lung function at baseline yet the greatest improvement in spirometry. However, lung function in this group, as well as in the Low FVC group failed to return to the normal range. These findings suggest that all groups had some potential for reversibility of injury, however, the components that improved differed, reinforcing differences in type or location of injury or response to treatment.
The WTCEHC includes individuals with a variety of potential exposures to the WTC dust and fumes and we grouped patients according to their potential for exposure. Longitudinal changes in lung function differed in these WTC exposure categories, with the Local workers demonstrating the least improvement. The Local worker category included people who worked either within the WTC towers or worked in surrounding buildings, many of whom evacuated on September 11, 2001 and returned to work in the surrounding buildings one week later. This category also had the highest likelihood of dust cloud exposure. We did not see a relationship with dust cloud exposure and temporal longitudinal changes in lung function in the cohort as a whole, however, the possibility remains that this intense exposure combined with subsequent exposures influenced disease pattern and longitudinal change in a specific category. Further detailed characterization of the specific exposure within each of these categories is warranted to improve our understanding of a dose-response relationship. Moreover, the data suggest that close observation of the Local worker group is warranted.
The use of tobacco had an important influence in our findings. In contrast to the group as a whole, we did not detect temporal improvement in lung function among heavy smokers. The finding of a lack of improvement among heavy smokers may be particularly important as the information can be used in counseling WTC-affected patients regarding the importance of smoking cessation.
The longitudinal analyses were modeled with a linear time trend for changes in spirometry over time and showed improvement in lung function over the observation period. However, it would be unreasonable to expect that this improvement would be sustained over prolonged periods of time and we expect the positive changes to be counterbalanced by normal age-related decline in spirometry measurements. Our current data were too sparse at the longer time points for a definitive long-term analysis of this issue. Exploratory analysis using an alternate model with quadratic time trend (data not shown) suggested an initial improvement in lung function followed by a subsequent decline. Future studies with a longer follow-up period will fully characterize the long-term changes in lung function in this population.
There are several potential limitations to this study. Although patients were treated in a standardized manner and were provided medications free of charge, we do not have data to assess medication adherence and thus cannot directly attribute changes in lung function to treatment. Nevertheless, the improvements in FVC and FEV1 suggest the potential for reversibility of airway injury. The possibility exists that the initial spirometry measurements were suboptimal and improved over time with patient experience. However, we used stringent criteria for inclusion of spirometry values making this explanation unlikely. Previous investigators have demonstrated that the reduced FVC pattern is associated with weight gain;(15) however, our patients with a reduced FVC improved despite the absence of significant changes in weight over time (data not shown). Our data are collected in the practical setting of a treatment program with patient's follow-up visits being clinically indicated or after a routine monitoring visit, and only 39% of symptomatic patients with valid baseline spirometry measurement had follow-up visits raising the possibility of bias in our results. We acknowledge that the findings might differ for a general population but these findings appear to have important implications for WTC treatment programs.
In summary, we have observed an improvement in lung function among community members of the WTCEHC during their initial years of enrollment. The improvement in lung function suggests reversible injury amenable to treatment. The different initial lung function patterns and their varied responses over time reinforce the heterogeneity of potential lung injury. The effect of tobacco use on lung function reinforces that WTCEHC patients should be urged to avoid other potential sources of lung injury and in particular to stop all exposures to tobacco. Although subjects with abnormal lung function improved, predicted spirometry measurements did not return to normal values and differences were noted between exposure categories. The residual abnormalities reinforce the need for treatment and continued monitoring for populations affected by this environmental disaster and suggest the importance of clinical interventions for other environmental disasters.
Acknowledgments
We would like to thank Terry Miles for his continued support and advice. We would like to thank Ruchel Ramos and Edith Davis for all their help in administering the program. We would like to thank the members of the WTC Community Advisory Committee for their invaluable advice and efforts on behalf of the program.
Funding: American Red Cross Liberty Disaster Relief Fund, City of New York, CDC-NIOSH 1E11OH009630, CDC NIOSH Contracts 200-2011-39391, 200-2011-39397, NIEHS Center Grant ES00260, CDC BAA-200-2011-39413, NIH NIEH T32 ES07267
Appendix Table 1.
Effects on average annual lung function change of FEV1 and FVC (ml/year) and FEV1% and FVC% (percent/year) in total longitudinal population1.
| FVC a | FVC% a | FEV1a | FEV1% a | |||||
|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI b | Estimate | 95% CI b | Estimate | 95% CI b | Estimate | 95% CI b | |
| Dust cloud | ||||||||
| Yes | 7 | (-14.3,28.4) | 0.06 | (-0.54, 0.66) | 7.4 | (-9.5,24.3) | 0.32 | (-0.30,0.95) |
| No | Ref | Ref | Ref | Ref | ||||
| Tobacco | ||||||||
| Heavy | -49.4*** | (-74.8, -24.0) | -1.13** | (-1.85, -0.41) | -25.2* | (-45.3,-5.1) | -0.97* | (-1.72, -0.23) |
| Light/none | Ref | Ref | Ref | Ref | ||||
| Spirometry pattern | ||||||||
| Normal | Ref | Ref | Ref | Ref | ||||
| Low FVC | 42.2** | (16.7, 67.7) | 0.85* | (0.13, 1.58) | 22.6* | (2.1,43.0) | 0.81* | (0.53,1.56) |
| Obstructed | -15.8 | (-52.9, 21.3) | -0.55 | (-1.59, 0.49) | 13 | (-17.0, 42.9) | 0.32 | (-0.79,1.43) |
| Obstructed and low FVC | 80.1** | (25.2,135.0) | 2.55** | (1.04,4.07) | 87.2** | (42.1,132.4) | 3.31*** | (1.68,4.94) |
| Exposure category | ||||||||
| Local workers | Ref | Ref | Ref | Ref | ||||
| Clean-up workers | 35.2* | (4.5, 65.9) | 0.45 | (-0.42,1.31) | 31.7* | (7.4,56.0) | 0.65 | (-0.26,1.55) |
| Resident | 45.8* | (16.6,75.0) | 0.81 | (-0.01,1.63) | 21.6 | (-1.6, 44.8) | 0.6 | (-0.27,1.46) |
| Rescue/recovery | 22.5** | (38.1,126,2) | 2.62*** | (1.44,3.80) | 43.4* | (8.7,78.1) | 1.07 | (-0.17,2.31) |
| other | -11.7 | (-79.8,56.5) | -0.71 | (-2.53, 1.10) | 13.2 | (-42.3,68.6) | -0.22 | (-2.19,1.74) |
| Respiratory symptoms | ||||||||
| No | 27.1 | (-1.9,56.1) | 0.71 | (-0.11, 1.53) | 8.5 | (-14.5, 31.4) | 0.39 | (-0.46, 1.25) |
| Yes | Ref | Ref | Ref | Ref | ||||
All results were from linear regression models adjusted with age, gender, race, BMI, income, and lower respiratory symptom.
After removing outliers, regression models were fit with 820, 841, 828, and 825 subjects for FEV1, FEV1%, FVC, and FVC% respectively.
: P-value<0.05;
: P-value<0.005;
: P-value<0.0005
Footnotes
The authors have no potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lioy PJ, Georgopoulos P. The anatomy of the exposures that occurred around the World Trade Center site: 9/11 and beyond. Ann N Y Acad Sci. 2006;1076:54–79. doi: 10.1196/annals.1371.002. [DOI] [PubMed] [Google Scholar]
- 2.Lioy PJ, Weisel CP, Millette JR, et al. Characterization of the dust/smoke aerosol that settled east of the World Trade Center (WTC) in lower Manhattan after the collapse of the WTC 11 September 2001. Environ Health Perspect. 2002;110:703–714. doi: 10.1289/ehp.02110703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yiin LM, Millette JR, Vette A, et al. Comparisons of the dust/smoke particulate that settled inside the surrounding buildings and outside on the streets of southern New York City after the collapse of the World Trade Center, September 11, 2001. J Air Waste Manag Assoc. 2004;54:515–528. doi: 10.1080/10473289.2004.10470935. [DOI] [PubMed] [Google Scholar]
- 4.Prezant DJ, Weiden M, Banauch GI, et al. Cough and bronchial responsiveness in firefighters at the World Trade Center site. N Engl J Med. 2002;347:806–815. doi: 10.1056/NEJMoa021300. [DOI] [PubMed] [Google Scholar]
- 5.Prezant DJ, Levin S, Kelly KJ, Aldrich TK. Upper and lower respiratory diseases after occupational and environmental disasters. Mt Sinai J Med. 2008;75:89–100. doi: 10.1002/msj.20028. [DOI] [PubMed] [Google Scholar]
- 6.Reibman J, Lin S, Hwang SA, et al. The World Trade Center residents' respiratory health study: new-onset respiratory symptoms and pulmonary function. Environ Health Perspect. 2005;113:406–411. doi: 10.1289/ehp.7375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin S, Reibman J, Bowers JA, et al. Upper respiratory symptoms and other health effects among residents living near the World Trade Center site after September 11, 2001. Am J Epidemiol. 2005;162:499–507. doi: 10.1093/aje/kwi233. [DOI] [PubMed] [Google Scholar]
- 8.Reibman J, Liu M, Cheng Q, et al. Characteristics of a residential and working community with diverse exposure to World Trade Center dust, gas, and fumes. J Occup Environ Med. 2009;51:534–541. doi: 10.1097/JOM.0b013e3181a0365b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banauch GI, Alleyne D, Sanchez R, et al. Persistent hyperreactivity and reactive airway dysfunction in firefighters at the World Trade Center. Am J Respir Crit Care Med. 2003;168:54–62. doi: 10.1164/rccm.200211-1329OC. [DOI] [PubMed] [Google Scholar]
- 10.Oppenheimer BW, Goldring RM, Herberg ME, et al. Distal airway function in symptomatic subjects with normal spirometry following World Trade Center dust exposure. Chest. 2007;132:1275–1282. doi: 10.1378/chest.07-0913. [DOI] [PubMed] [Google Scholar]
- 11.Friedman SM, Maslow CB, Reibman J, et al. Case-control study of lung function in World Trade Center Health Registry area residents and workers. Am J Respir Crit Care Med. 2011;184:582–589. doi: 10.1164/rccm.201011-1909OC. [DOI] [PubMed] [Google Scholar]
- 12.Izbicki G, Chavko R, Banauch GI, et al. World Trade Center "sarcoid-like" granulomatous pulmonary disease in New York City Fire Department rescue workers. Chest. 2007;131:1414–1423. doi: 10.1378/chest.06-2114. [DOI] [PubMed] [Google Scholar]
- 13.Caplan-Shaw CE, Yee H, Rogers L, et al. Lung Pathologic Findings in a Local Residential and Working Community Exposed to World Trade Center Dust, Gas, and Fumes. J Occup Environ Med. 2011 doi: 10.1097/JOM.0b013e31822fff60. [DOI] [PubMed] [Google Scholar]
- 14.Aldrich TK, Gustave J, Hall CB, et al. Lung function in rescue workers at the World Trade Center after 7 years. N Engl J Med. 2010;362:1263–1272. doi: 10.1056/NEJMoa0910087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Skloot GS, Schechter CB, Herbert R, et al. Longitudinal assessment of spirometry in the World Trade Center medical monitoring program. Chest. 2009;135:492–498. doi: 10.1378/chest.08-1391. [DOI] [PubMed] [Google Scholar]
- 16.EPRIII: Guidelines for the Diagnosis and Management of Asthma. U.S. Department of Health and Human Services, National Institutes of Health; 2007. [Google Scholar]
- 17.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 18.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–187. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 19.Herbert R, Moline J, Skloot G, et al. The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect. 2006;114:1853–1858. doi: 10.1289/ehp.9592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 21.Agresti a. Categorical Data Analysis. New York: Wiley-Interscience; 2002. [Google Scholar]
- 22.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 23.Sherrill DL, Lebowitz MD, Halonen M, Barbee RA, Burrows B. Longitudinal evaluation of the association between pulmonary function and total serum IgE. Am J Respir Crit Care Med. 1995;152:98–102. doi: 10.1164/ajrccm.152.1.7599870. [DOI] [PubMed] [Google Scholar]
- 24.Banauch GI, Dhala A, Prezant DJ. Pulmonary disease in rescue workers at the World Trade Center site. Curr Opin Pulm Med. 2005;11:160–168. doi: 10.1097/01.mcp.0000151716.96241.0a. [DOI] [PubMed] [Google Scholar]
- 25.Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15-year follow-up study of ventilatory function in adults with asthma. N Engl J Med. 1998;339:1194–1200. doi: 10.1056/NEJM199810223391703. [DOI] [PubMed] [Google Scholar]
- 26.Vestbo J, Edwards LD, Scanlon PD, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med. 2011;365:1184–1192. doi: 10.1056/NEJMoa1105482. [DOI] [PubMed] [Google Scholar]
- 27.Drummond MB, Hansel NN, Connett JE, Scanlon PD, Tashkin DP, Wise RA. Spirometric predictors of lung function decline and mortality in early chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185:1301–1306. doi: 10.1164/rccm.201202-0223OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crowley LE, Herbert R, Moline JM, et al. “Sarcoid like” granulomatous pulmonary disease in World Trade Center disaster responders. Am J Ind Med. 2011;54:175–184. doi: 10.1002/ajim.20924. [DOI] [PubMed] [Google Scholar]
- 29.Wu M, Gordon RE, Herbert R, et al. Case report: Lung disease in World Trade Center responders exposed to dust and smoke: carbon nanotubes found in the lungs of World Trade Center patients and dust samples. Environ Health Perspect. 2010;118:499–504. doi: 10.1289/ehp.0901159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mead J. The lung's “quiet zone”. N Engl J Med. 1970;282:1318–1319. doi: 10.1056/NEJM197006042822311. [DOI] [PubMed] [Google Scholar]
- 31.Contoli M, Bousquet J, Fabbri LM, et al. The small airways and distal lung compartment in asthma and COPD: a time for reappraisal. Allergy. 2010;65:141–151. doi: 10.1111/j.1398-9995.2009.02242.x. [DOI] [PubMed] [Google Scholar]