Abstract
Purpura fulminans is a rare syndrome of intravascular thrombosis and hemorrhagic infarction of the skin, which is an unusual cutaneous manifestation of disseminated intravascular coagulation. It often occurs in small children and babies due to infection and/or sepsis, rarely in adults in clinic. We report the first case of deadly purpura fulminans following thermal injury in a 64-year-old Chinese woman. The purpura developed sharply and aggravated multiple organ dysfunction. The patient died of purpura fulminans, disseminated intravascular coagulation, and multiple organ dysfunction syndrome.
1. Introduction
Purpura fulminans (PF) is a life-threatening hemorrhagic condition characterized by acute onset hypotension, fever, cutaneous hemorrhage, and necrosis [1]. It is often caused by the infection of Staphylococcus aureus, hemolytic streptococcus and meningococcus [2], and can be classified into three distinct categories: inherited or acquired abnormalities of protein C or other coagulation systems, acute infectious PF, and idiopathic PF [3]. PF often occurs in small children and babies due to infection and/or sepsis, rarely in adults following thermal injury. In this report, we describe a case of PF following alcohol flame thermal injury.
2. Case Presentation
A 64-year-old Chinese woman was admitted to our department with an 18-day history of alcohol flame burn and a 12-hour painful erythema on the right buttocks. Physical examination showed a low-grade fever (37.8°C), burn wounds (2% TBSA) on the left inner thigh covered by traditional Chinese medicine (Figure 1(a)), and petechial rash on the right buttocks (Figure 1(b)). Past medical history and family history were unremarkable. Laboratory findings include haemoglobin anomaly (95 g/L), leukocytosis (15.38 × 109/L), thrombocytopenia (90 × 109/L), and prolonged APTT (69.5 s). Tests of kidney and liver function and abdominal ultrasound showed no abnormality of note.
Figure 1.
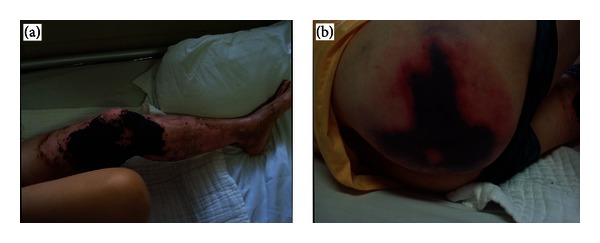
Photograph of the patient when admitted to the department. (a) Alcohol flame burn covered by traditional Chinese medicine. (b) Painful erythema on the right buttocks.
The purpura developed sharply and occurred on the lower extremities in the next morning. Laboratory tests showed decreased platelet (21 × 109/L), haemoglobin (57 g/L), fibrinogen (0.82 g/L, normal more than 1.8 g/L) and factor VIII activity (29.1%, normal 70%–150%), increased leukocytosis (18.09 × 109/L), D-dimer (30018 ng/mL, normal less than 392 ng/mL), and APTT (67.8 s). Thrombophilia screens displayed low antithrombin III activity (57.1%, normal 75%–125%) but normal protein C and S concentrations. There were no abnormalities in prothrombin time, thrombin time, C3, C4, anticardiolipin, antinuclear, and IgG or IgA antibody levels.
The patient was diagnosed with PF and received antibiotics (imipenem, cilastatin sodium, and ticarcillin), fluid resuscitation, and component blood transfusion (fresh frozen plasma and blood platelets) but complicated by new emergence and enlargement of rash, which gradually enlarged into an irregular pattern of full-thickness skin and soft-tissue loss (Figures 2(a)–2(d)). She received bilateral lower extremities escharotomy but developed acute renal failure with anuria 24 h later. Test of kidney and liver function revealed increased creatinine (201 umol/L), glutamic-pyruvic transaminase (391.8 IU/L), and glutamic oxaloacetic transaminase (939.8 IU/L). The blood routine test revealed decreased platelet (11 × 109/L), haemoglobin (40 g/L), and red blood cell (1.34 × 1012/L).
Figure 2.

Photograph of the sharply developed purpura. Purpuric rash in the (a) left arm, (b) left lower limbs, (c) buttocks and (d) left ear.
The patient received methylprednisolone treatment, but it did not work. The purpuric rash covered approximately 70% TBSA in the next afternoon, and the platelet count was 9 × 109/L, haemoglobin was 31 g/L, and leukocytosis was 27.28 × 109/L. Test of kidney and liver function revealed increased creatinine (308 umol/L), glutamic-pyruvic transaminase (1354 IU/L), and glutamic-oxalacetic transaminase (4009 IU/L). Myocardial enzyme levels, including creatine kinase and lactic dehydrogenase, were increased notably. The bacterial cultivation indicated Staphylococcus epidermidis and Enterobacter cloacae in burn wound but not in blood, which were sensitive to multiple antibiotics including imipenem, cilastatin sodium, and ticarcillin. Consequently, the patient died on the sixth day after admission of purpura fulminans, disseminated intravascular coagulation, and multiple organ dysfunction syndrome.
3. Discussion
PF is a lethal haemorrhagic condition usually associated with infection and/or sepsis. It occurs mainly in babies and small children, and the mortality rate in the acute phase ranges between 18% and 40% [4]. It is most commonly associated with Neisseria meningitidis sepsis, and proteins C and S and antithrombin III are always involved in the coagulopathy pathogenesis [5, 6]. DIC is believed to be the major pathophysiological mechanism [7]. The abnormal APTT, platelet count, and fibrinogen point towards ongoing coagulopathy as negative prognostic markers.
The mainstays of primary management are to remove the underlying cause of clotting abnormalities and with supportive treatment. Protein C supplementation could decrease mortality and morbidity [8], but the safety and efficacy of heparin therapy has not been confirmed [9]. The attention is turned to skin loss management after acute phase, including debridement and grafting, such as escharotomies, fasciotomies, or major amputations. Early escharotomy is recommended in case of amputation [10]. In this case, the PF started by the time that the burn injury approximately healed, and the Staphylococcus epidermidis and Enterobacter cloacae, which were the pathogens of PF, were detected on the wound but not in the blood. Although we used the sensitive antibiotics the first time, the remarkably impressive coagulopathy was ultimately uncontrollable. We suspected that there appears to be a preference for heparin application in cases of ongoing coagulopathy, especially in adults in which the possibility of hereditary proteins S and C deficiency is little.
Consent
Written informed consent was obtained from the next of kin of the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Conflict of Interests
The authors declare that they have no conflict of interests. The authors warrant that none of the authors has any financial interest with the information presented Authors' contribution. All authors have made substantial contributions to all of the following: (1) the conception and design of the study and acquisition, analysis, and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted. The paper, including related data, figures, and tables, has not been previously published, and the paper is not under consideration elsewhere.
Acknowledgment
The authors thank the patient's family for providing permission to publish her information.
References
- 1.Edlich RF, Cross CL, Dahlstrom JJ, Long WB. Modern concepts of the diagnosis and treatment of purpura fulminans. Journal of Environmental Pathology, Toxicology and Oncology. 2008;27(3):191–196. doi: 10.1615/jenvironpatholtoxicoloncol.v27.i3.30. [DOI] [PubMed] [Google Scholar]
- 2.Özdemir H, Kendirli T, Çiftçi E, İnce E. Purpura fulminans in a child due to Neisseria meningitidis. Infection. 2012;40(6):717–718. doi: 10.1007/s15010-012-0286-x. [DOI] [PubMed] [Google Scholar]
- 3.Bhardwaj N, Aggarwal S, Sharma A, Sharma V. Photoclinic: Streptococcal purpura fulminans. Archives of Iranian Medicine. 2012;15(2):115–116. [PubMed] [Google Scholar]
- 4.Chasan PE, Hansbrough JF, Cooper ML. Management of cutaneous manifestations of extensive purpura fulminans in a burn unit. Journal of Burn Care and Rehabilitation. 1992;13(4):410–413. doi: 10.1097/00004630-199207000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Aroor S, Varma C, Mundkur SC. Purpura fulminans in a child: a case report. Journal of Clinical and Diagnostic Research. 2012;6(10):1812–1813. doi: 10.7860/JCDR/2012/4339.2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tassin M, Llarena P, Laffaye F, Kaltenbach G. Protein C deficiency in patient with sepsis-associated disseminated intravascular coagulation and deep vein thrombosis. Archivos Argentinos de Pediatría. 2013;111(1):e28–e30. doi: 10.5546/aap.2013.e28. [DOI] [PubMed] [Google Scholar]
- 7.Grzelakowski P, Ługowski T, Kurzyna M, et al. Acute intermediate-risk pulmonary embolism with right-sided free-floating intracardiac thrombus, systemic inflammatory reaction syndrome, multiple organ dysfunction syndrome, disseminated intravascular coagulation and acute ischaemia of a limb. Kardiologia Polska. 2010;68(10):1140–1144. [PubMed] [Google Scholar]
- 8.Veldman A, Fischer D, Wong FY, et al. Human protein C concentrate in the treatment of purpura fulminans: a retrospective analysis of safety and outcome in 94 pediatric patients. Critical Care. 2010;14(4, article R156) doi: 10.1186/cc9226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith OP, White B, Vaughan D, et al. Use of protein-C concentrate, heparin, and haemodiafiltration in meningococcus-induced purpura fulminans. Lancet. 1997;350(9091):1590–1593. doi: 10.1016/s0140-6736(97)06356-3. [DOI] [PubMed] [Google Scholar]
- 10.Kondaa S, Zell D, Milikowski C, Alonso-Llamazares J. Purpura fulminans associated with streptococcus pneumoniae septicemia in an asplenic pediatric patient. Actas Dermo-Sifiliográficas. 2012 doi: 10.1016/j.adengl.2012.05.027. [DOI] [PubMed] [Google Scholar]


