Abstract
Background
Methicillin-resistant Staphylococcus aureus (MRSA) “colonization pressure” (CP) predicts infections in hospitals. We applied the CP concept to staphylococcal transmission within households. We tested the hypothesis that children with S aureus skin and soft tissue infection (SSTI) plus colonization (“cases”) with higher baseline household CP (HHCP) would be at greater risk for persistent colonization and recurrent SSTI during study period.
Methods
We collected baseline colonization swabs from 92 cases and 296 of their household contacts. Cases underwent decolonization. S aureus HHCP was calculated as the proportion of colonized household contacts at baseline (excluding cases). S aureus colonization and recurrent SSTI in cases were followed for 12 months.
Results
Overall, median S aureus HHCP was 60% (mean = 55%). For cases colonized with MRSA, median MRSA HHCP was 11% (mean 29%); methicillin-susceptible S aureus (MSSA)–colonized cases had a median MSSA HHCP of 50% (mean = 49%). Over 1 year, MRSA HHCP was an independent risk factor for persistent MRSA colonization in cases (each 10-unit increase in HHCP associated with an adjusted odds ratio of 1.25; 95% confidence interval, 1.06–1.47). HHCP was not associated with recurrent SSTI in cases.
Conclusions
MRSA HHCP is associated with persistent colonization in outpatients. Further studies are needed to determine the relationship between persistent colonization of household contacts, environmental contamination, and SSTI.
Keywords: Staphylococcus aureus, Methicillin-Resistant, Methicillin-Sensitive, Colonization Pressure, Skin Infections
Methicillin-resistant Staphylococcus aureus (MRSA) was once associated almost exclusively with healthcare-associated infections. However, new epidemic strains have emerged outside of the healthcare environment and are designated community-associated (CA) MRSA [1, 2]. These strains cause significant morbidity and mortality in immunocompetent children [3]. Community-associated MRSA has been associated with asymptomatic nasal colonization, superficial cutaneous abscesses, and invasive infections [3–7]. S aureus infections cluster in households [8–13]. Frequent skin-to-skin contact, sharing personal hygiene items, and contamination of household fomites may play an important role in the spread of S aureus [10, 14]. Thus, colonized household contacts of patients with MRSA infections may perpetuate transmission [8–13, 15].
Colonization pressure (CP) is a measure used in healthcare settings to determine the magnitude of the microorganism reservoir within a healthcare unit. It has been defined as the proportion of patients on a given unit colonized during a defined period. Colonization pressure is a predictive factor for nosocomial transmission of MRSA [16–18], vancomycin-resistant Enterococcus [19], and Clostridium difficile [20, 21]. One investigation demonstrated that MRSA nosocomial transmission was 7 times more likely when the preceding month's CP was above the median CP over the 2-year study period [16]. However, no previous studies have examined S aureus CP outside of healthcare facilities. It is unclear whether the magnitude of contemporary household S aureus colonization is related to persistent colonization or subsequent infections in patients or their household contacts. These transmission dynamics must be understood to develop evidence-based guidelines for screening and treating household contacts of patients with CA S aureus infections.
We recently conducted a 2-arm, individual vs household decolonization intervention study for pediatric patients with community-onset S aureus skin and soft tissue infection (SSTI) and colonization (ie, cases). Drawing on those cases randomized to the individual decolonization group, we aimed to measure the household CP (HHCP), defined as the proportion of household contacts colonized at study enrollment. We then evaluated the association between baseline HHCP and ongoing colonization in cases and subsequent incidence of SSTI in cases and their household contacts. Our hypothesis was that cases with a higher baseline HHCP would be at greater risk for persistent S aureus colonization and recurrent SSTI during the longitudinal study.
METHODS
Study Design and Participant Recruitment
This study was approved by the Washington University Institutional Review Board. Informed consent was obtained at study enrollment for cases and household contacts. Patients aged 6 months to 20 years with SSTI were screened from May 2008 to December 2009 from the Emergency Department and ambulatory wound center of St Louis Children's Hospital (SLCH) and from 9 community pediatric practices affiliated with a practice-based research network in metropolitan St Louis, MO [22]. Patients with traditional healthcare-associated S aureus risk factors (indwelling catheter or percutaneous medical device, post-operative wound infection, on dialysis, or residence in a long-term care facility) were excluded from screening. To detect colonization of cases, culture swabs (BBL Liquid Stuart; Becton Dickinson, Sparks, MD) were obtained at the time of screening from the anterior nares, axillae, and inguinal folds as described previously [22, 23]. To confirm the presence of an S aureus infection, wound culture results were obtained from the SLCH microbiology laboratory or the relevant provider's office. Patients both colonized and infected with S aureus (MRSA or methicillin-susceptible S aureus [MSSA]) were eligible for enrollment in a decolonization trial and were invited to return to SLCH for an enrollment visit. At the time of enrollment, the colonization status of household contacts was assessed by culturing their anterior nares, axillae, and inguinal folds as described previously [22]. A household contact was defined as a person who spent more than half of each week in the primary household of the case. We analyzed the cohort of cases randomized to the individual decolonization group.
Enrollment and Follow-up
At enrollment, cases were provided with a hygiene curriculum and instructed to apply 2% mupirocin ointment to the anterior nares twice daily and perform daily body washes with 4% chlorhexidine solution, each for 5 days. A standardized questionnaire was administered to collect demographic information about each household. Characteristics of cases, including past medical history, hygiene routines, school or daycare attendance, healthcare contact, and other risk factors, were recorded.
Cases were followed longitudinally with follow-up visits at SLCH 1, 3, 6, and 12 months after enrollment. Colonization status of cases was assessed with nasal, axillary, and inguinal swabs at each visit. A survey was administered to ascertain incident SSTI in cases and household contacts; participants were asked to report the occurrence of skin abscess, boil, cellulitis, impetigo, or spider bite.
Colonization Pressure Calculation
Calculations were performed to determine the proportion of household contacts colonized at baseline with MRSA, MSSA, or overall S aureus (ie, CP) as follows:
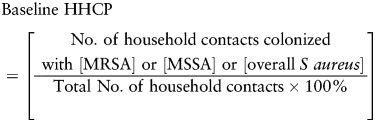 |
Cases were excluded from the CP calculation because they were presumably affected by the decolonization intervention. Household contacts not providing swabs were also excluded. Median baseline household CP is reported.
Statistical Analysis
Potential household risk factors for higher baseline HHCP were assessed using Mann-Whitney U tests. We then evaluated whether cases with persistent colonization or cases and household contacts with a recurrent infection during follow-up had a higher baseline HHCP than those without persistent colonization or SSTI at each follow-up time point separately, also using Mann-Whitney U tests.
To examine the association between baseline HHCP and likelihood of MRSA and MSSA colonization and SSTI during the entire follow-up period, we performed a separate analysis including other postulated risk factors, using all data from the follow-up period (1, 3, 6, and 12 months). We performed mixed-effects logistic regression models using the SAS procedure PROC GLIMMIX to model the repeated measures. Logit was used as the link function to estimate odds ratios (ORs) and 95% confidence intervals (CIs). A random intercept was included for subject, because observations over time were nested within subjects. Each risk factor was first examined separately in bivariate analysis. Then multivariable models were run including factors that are either known or widely hypothesized to be associated with colonization or recurrent infection: baseline MRSA HHCP and MSSA HHCP (our primary risk factors of interest); case's age (per 1 year increase), race, gender, and insurance status; case and household contact SSTI in the past year; sharing a bath, bath towel, or bed with a household contact; household crowding (defined as >2 people per bedroom); having a healthcare worker in home; colonization with MRSA or MSSA at prior time points; taking antibiotics or having recurrent SSTI during each follow-up interval (for models predicting MRSA and MSSA colonization); and time (per 1 month increase) [6, 7, 10, 17, 24, 25]. For all analyses, a P < .05 was considered significant. Statistical analyses were performed with SPSS 18.0 for Windows (IBM SPSS, Chicago, IL) and SAS version 9.2 for Windows (SAS Institute, Inc, Cary, NC).
RESULTS
Baseline Patient Characteristics and Colonization Pressure
We evaluated 92 cases and 296 (91%) of their 325 household contacts. The mean age (±SD) of the cases was 6.3 (±5.7) years. The mean number of people in each household, including the case, was 4.5 (range, 2–12) (Table 1).
Table 1.
Patient and Household Characteristics
| Characteristic | Cases N = 92 (%) |
|---|---|
| Age, years, mean ± SD | 6.3 ± 5.7 |
| Race | |
| White and other | 36 (39) |
| African American | 56 (61) |
| Gender | |
| Male | 55 (60) |
| Female | 37 (40) |
| Number of persons in household, mean (range) | 4.5 (2–12) |
| Household crowdinga | 15 (16) |
| Case SSTI in last year | 41 (45) |
| Household contact SSTI in last year | 67 (22) |
Abbreviations: SD, standard deviation; SSTI, skin or soft tissue infection.
aDefined as >2 people per bedroom.
Of 92 cases, 50 (54%) were colonized at baseline with MRSA only, 34 (37%) with MSSA only, and 8 (9%) with both MRSA and MSSA at different body sites. MRSA was isolated from 68 (74%) SSTI cultures, and MSSA was isolated from 24 (26%) SSTI cultures. One hundred sixty-nine (57%) household contacts were colonized with S aureus: 50 (17%) with MRSA only, 113 (38%) with MSSA only, and 6 (2%) with both MRSA and MSSA.
The median baseline overall S aureus HHCP was 60% (mean = 55%); MRSA median HHCP was 0% (mean = 20%), and MSSA median HHCP was 33% (mean = 36%). Median MRSA HHCP was 11% (mean = 29%) in households in which the case was colonized with MRSA at baseline, and 0% (mean = 5%) in households where the case was colonized with only MSSA at baseline. Median MSSA HHCP was 50% (mean = 49%) in households in which the case was colonized with MSSA at baseline, and 0% (mean = 24%) in households where the case was colonized with only MRSA at baseline.
Cases with household contacts who experienced an SSTI in the past year had a higher baseline S aureus HHCP than cases without that history (67% vs 50%, P = .04). No other risk factors were found to predict overall S aureus HHCP (Table 2). When the analysis was stratified by MRSA and MSSA, none of the studied risk factors were found to be associated with HHCP (data not shown).
Table 2.
Risk Factors for Baseline Staphylococcus aureus Household Colonization Pressurea
| Risk Factor | Baseline S aureus HHCP, Median % (IQR) |
P | |
|---|---|---|---|
| Participants With Risk Factor | Participants Without Risk Factor | ||
| African American raceb | 65 (33–100) | 50 (0–75) | .16 |
| Medicaid or no insuranceb | 67 (31–100) | 42 (0–75) | .09 |
| Household crowdingc | 50 (22–100) | 60 (25–100) | .72 |
| Household contact SSTI last year | 67 (33–100) | 50 (0–75) | .04 |
| Case SSTI last yearb | 50 (24–88) | 67 (21–100) | .41 |
| Prison worker in household | 33 (33–67) | 60 (22–100) | .55 |
| Hospital worker in household | 50 (26–75) | 65 (21–100) | .65 |
| Dog or cat in household | 50 (27–75) | 67 (19–100) | .24 |
| Case shares bedb | 55 (21–100) | 67 (25–100) | .76 |
| Case shares bathb | 64 (0–100) | 60 (31–76) | .90 |
| Case shares bath towelb | 67 (33–100) | 50 (0–75) | .08 |
| Alcohol based sanitizer use in household | 60 (21–88) | 67 (28–100) | .40 |
| Case bathes dailyb | 67 (33–100) | 50 (0–100) | .21 |
| Case washes linens weeklyb | 67 (29–100) | 50 (0–100) | .58 |
Abbreviations: HHCP, household colonization pressure; IQR, interquartile range; SSTI, skin and soft tissue infection.
aMann-Whitney U test was used to analyze differences in median between groups.
bVariables measured for the case only–not necessarily representative of all household contacts.
cDefined as >2 people per bedroom.
Baseline Colonization Pressure and Follow-up Colonization MRSA Colonization
Of the 78 cases available for sampling at the 1-month follow-up visit, 22 (28%) were colonized with MRSA and 15 of 72 (21%), 10 of 71 (14%), and 11 of 68 (16%) were colonized with MRSA at the 3-month, 6-month, and 12-month follow-up visits, respectively. Cases colonized with MRSA at 1, 3, 6, and 12 months, or any follow-up visit, had a higher baseline MRSA HHCP than those who were not colonized with MRSA at longitudinal samplings (Table 3). In bivariate mixed-effects logistic regression models for the repeated measures (including all follow-up time points), risk factors for MRSA colonization during follow-up were higher baseline MRSA HHCP (each 10-unit increase associated with an OR of 1.53; 95% CI, 1.25–1.88; P < .001), colonization with MRSA at the previous time point (OR = 6.98; 95% CI, 3.14–15.50; P < .001), sharing a bath with a household contact (OR = 4.65; 95% CI, 1.10–19.62; P = .036), and taking antibiotics during a follow-up interval (OR = 3.21; 95% CI, 1.39–7.40; P = .006). Higher baseline MSSA HHCP (10-unit increase OR of .72; 95% CI, .58–.89; P = .003) and increasing age (increase of 1 year associated with an OR of 0.85; 95% CI, .76–.96; P = .008) were inversely related to MRSA colonization during follow-up. Colonization with MSSA at a previous time point (OR = .35; 95% CI, .12–1.00; P = .050) and time since study enrollment (each 1-month increase associated with an OR of .91; 95% CI, .82–1.00; P = .050) trended with an inverse association.
Table 3.
Baseline Household Colonization Pressure by Colonization Status of Cases at Follow-upa
| Follow-up Visit | Baseline MRSA HHCP, Median % (IQR) |
P | Baseline MSSA HHCP, Median % (IQR) |
P | ||
|---|---|---|---|---|---|---|
| Colonized With MRSA at Follow-up | Not Colonized With MRSA at Follow-up | Colonized With MSSA at Follow-up | Not Colonized With MSSA at Follow-up | |||
| Ever Colonizedb | 42 (0–62) | 0 (0–0) | <.001 | 50 (0–67) | 0 (0–46) | .01 |
| 1 Month | 50 (23–69) | 0 (0–0) | <.001 | 50 (0–67) | 25 (0–50) | .16 |
| 3 Months | 25 (0–50) | 0 (0–25) | .01 | 50 (19–67) | 25 (0–50) | .04 |
| 6 Months | 42 (0–81) | 0 (0–31) | .01 | 45 (0–100) | 25 (0–50) | .11 |
| 12 Months | 50 (0–60) | 0 (0–25) | .01 | 50 (0–75) | 25 (0–50) | .03 |
Abbreviations: HHCP, household colonization pressure; IQR, interquartile range; MRSA, methicillin-resistant. Staphylococcus aureus; MSSA, methicillin-sensitive S aureus.
aMann-Whitney U test was used to analyze differences in mean between groups.
bColonized at any of the follow-up visits.
In the multivariable model (Table 4), higher baseline MRSA HHCP (each 10-unit increase associated with an adjusted OR [aOR] of 1.25; 95% CI, 1.06–1.47; P = .007) was an independent risk factor for case MRSA colonization during follow-up. Colonization with MRSA at the previous time point trended towards significance (aOR = 2.72; 95% CI, .85–8.77; P = .093). Higher baseline MSSA HHCP (10-unit increase aOR of .82; 95% CI, .70–.97; P = .020) was inversely related to MRSA colonization during follow-up.
Table 4.
Multivariable Analysis of Risk Factors for Staphylococcus aureus Colonization and SSTI Over 12 Months
| Risk Factor | MRSA Colonizationa aOR (95% CI) | MSSA Colonizationb aOR (95% CI) | SSTIc aOR (95% CI) |
|---|---|---|---|
| Baseline MRSA HHCP (10 unit increase) | 1.25 (1.06–1.47) | 1.04 (.90–1.20) | .92 (.82–1.04) |
| Baseline MSSA HHCP (10 unit increase) | .82 (.70–.97) | 1.09 (.98–1.21) | 1.05 (.96–1.16) |
| Case age (1 year increase) | .93 (.83–1.04) | 1.04 (.97–1.12) | .93 (.86–.997) |
| African American race | .75 (.22–2.53) | 2.36 (1.01–5.53) | 1.31 (.59–2.92) |
| Male | 1.12 (.40–3.12) | 1.16 (.58–2.33) | .75 (.37–1.55) |
| Medicaid or no insurance | 1.57 (.48–5.14) | 1.04 (.45–2.41) | .66 (.29–1.49) |
| Case SSTI past year | 1.63 (.59–4.55) | .97 (.45–2.10) | 2.40 (1.17–4.90) |
| HH contact SSTI past year | 1.20 (.46–3.11) | .88 (.43–1.78) | 1.35 (.68–2.69) |
| Sharing bath with HH contact | 1.17 (.40–3.44) | .65 (.26–1.64) | 2.15 (.97–4.78) |
| Sharing bath towel with HH contact | .91 (.31–2.70) | .51 (.21–1.22) | .84 (.39–1.77) |
| Sharing bed with HH contact | .74 (.22–2.48) | 1.23 (.49–3.10) | .83 (.34–1.99) |
| Household crowdingd | 1.31 (.45–3.86) | 2.35 (.97–5.73) | 1.44 (.65–3.21) |
| Healthcare worker in home | 1.36 (.43–4.32) | .65 (.27–1.57) | 1.17 (.52–2.63) |
| Colonization with MRSA at prior time point | 2.72 (.85–8.77) | .58 (.23–1.46) | 2.54 (1.17–5.51) |
| Colonization with MSSA at prior time point | .70 (.24–2.02) | 4.51 (1.92–1.55) | 1.83 (.90–3.73) |
| Taking antibiotics during follow-up interval | 1.46 (.60–3.55) | 1.23 (.59–2.58) | NA |
| Having recurrent SSTI at current time point | 1.75 (.74–4.15) | 1.23 (.58–2.62) | NA |
| SSTI at prior time point | NA | NA | .67 (.34–1.34) |
| Time (1 month increase) | .96 (.86–1.08) | 1.02 (.94–1.11) | 1.05 (.97–1.14) |
Bold numbers represent statistically significant values. Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; HH, household; HHCP, household colonization pressure; MRSA, methicillin-resistant S aureus; MSSA, methicillin-sensitive S aureus; NA, not applicable; SSTI, skin and soft tissue infection.
aMRSA model: N = 73 patients, 261 observations.
bMSSA model: N = 73 patients, 261 observations.
cSSTI model: N = 75 patients, 264 observations.
dDefined as >2 people per bedroom.
MSSA Colonization. Of the 78 cases available for sampling at the 1-month follow-up visit, 22 (28%) were colonized with MSSA and 19 of 72 (26%), 23 of 71 (32%), and 20 of 68 (29%) were colonized with MSSA at the 3-month, 6-month, and 12-month follow-up visits, respectively. Cases colonized with MSSA at 3 and 12 months, or any follow-up visit, had a higher baseline MSSA HHCP than those who were not colonized with MSSA at longitudinal samplings (Table 3). In bivariate mixed-effects logistic regression models for the repeated measures (including all follow-up time points), risk factors for MSSA colonization during follow-up were higher baseline MSSA HHCP (10-unit increase OR of 1.22; 95% CI, 1.06–1.40; P = .005), colonization with MSSA at the previous time point (OR = 5.63; 95% CI, 2.67–11.85; P < .001), increasing age (increase of 1 year OR of 1.09; 95% CI, 1.01–1.18; P = .037), and African American race (OR = 2.99; 95% CI, 1.09–8.14; P = .033). Patients with Medicaid or no insurance trended to be colonized with MSSA during follow-up (OR = 2.67; 95% CI, .93–7.77; P = .068). Sharing a bath with a household contact (OR = .28; 95% CI, .09–.85; P = .025) was inversely related with MSSA colonization during follow-up, and colonization with MRSA at a previous time point trended with a negative association (OR = .43; 95% CI, .19–1.01; P = .053).
In the multivariable model (Table 4), African American race (vs whites/other races) (aOR = 2.36; 95% CI, 1.01–5.53; P = .047) and being colonized with MSSA at the previous time point (aOR = 4.51; 95% CI, 1.92–10.55; P < .001) were independent risk factors for case MSSA colonization during follow-up. Crowding in the household trended towards significance (aOR = 2.35; 95% CI, 0.97–5.73; P = .060).
Baseline Colonization Pressure and Incident SSTI in Cases and Their HH Contacts during Follow-up
At the 1-month follow-up visit, recurrent SSTI was reported by 21 of 81 (26%) cases. Assessing recurrence of SSTI cumulatively, 36 of 76 (47%) cases reported SSTI over 3 months, 46 of 76 (61%) cases reported SSTI over 6 months, and 56 of 78 (72%) cases reported SSTI over 12 months. Cases experiencing SSTI over the 1-month, 3-month, 6-month, and 12-month follow-up intervals did not have a higher baseline S aureus HHCP than those not experiencing SSTI (Table 5). In sub-analyses, baseline MRSA and MSSA HHCP were not associated with recurrent SSTI (data not shown).
Table 5.
Baseline Household Colonization Pressure “R by Incidence of SSTI in Cases and Household Contacts Over Follow-up Intervalsa
| Follow-up Interval | Baseline Staphylococcus aureus HHCP, Median % (IQR) |
P | Baseline S aureus HHCP, Median % (IQR) |
P | ||
|---|---|---|---|---|---|---|
| Case With SSTI | Case Without SSTI | Household Contact With SSTI | Household Contact Without SSTI | |||
| 0–1 Month | 50 (0–100) | 67 (33–100) | .35 | 67 (50–100) | 64 (29–75) | .21 |
| 0–3 Months | 57 (0–100) | 50 (33–75) | .92 | 67 (50–100) | 60 (29–75) | .16 |
| 0–6 Months | 50 (8–100) | 60 (25–75) | .82 | 60 (33–100) | 64 (33–75) | .33 |
| 0–12 Months | 50 (0–100) | 60 (50–69) | .93 | 67 (50–100) | 50 (29–73) | .02 |
Abbreviations: HHCP, household colonization pressure; IQR, interquartile range; SSTI, skin and soft tissue infection.
aMann-Whitney U test was used to analyze difference in means between groups.
Assessing incidence of SSTI in household contacts cumulatively, 20 of 281 (7%) contacts reported SSTI over 1 month, 28 of 271 (10%) contacts reported SSTI over 3 months, 40 of 254 (16%) contacts reported SSTI over 6 months, and 36 of 226 (16%) contacts reported SSTI over 12 months. Household contacts experiencing SSTI over the 12-month follow-up study period had a higher baseline S aureus HHCP than those not experiencing SSTI (P = .02) (Table 5).
Risk Factors for SSTI in Cases at Follow-up
In bivariate mixed-effects logistic regression models, sharing a bath with a household contact (OR = 2.41; 95% CI, 1.34–4.33; P = .003) and having an SSTI in the past year (OR = 2.05; 95% CI, 1.14–3.69; P = .018) were risk factors for recurrent SSTI during follow-up. Length of time (in months) from study enrollment trended to be associated with recurrent SSTI (OR = 1.06; 95% CI, .99–1.13; P = .079; longer time associated with increased risk). Increasing age (increase of 1 year OR of .91; 95% CI, .86–.96; P < .001) was inversely related to recurrent SSTI during follow-up.
In the multivariable model (Table 4), having an SSTI in the past year (aOR = 2.40; 95% CI, 1.17–4.90; P = .017) and colonization with MRSA at the previous time point (aOR = 2.54; 95% CI, 1.17–5.51; P = .019) were independent risk factors for recurrent SSTI during follow-up. Sharing a bath with a household contact (aOR = 2.15; 95% CI, .97–4.78; P = .060) and colonization with MSSA at the previous time point (aOR = 1.83; 95% CI, .90–3.73; P = .096) trended towards significance. Older age (increase of 1 year aOR of .93; 95% CI, .86–.997; P = .043) was inversely related to recurrent SSTI during follow-up.
DISCUSSION
We describe a novel application of S aureus CP that may be useful in the community setting. Our data demonstrate that high MRSA HHCP is associated with persistent MRSA colonization in pediatric cases. It is interesting to note that we did not find a relationship between baseline S aureus HHCP and subsequent SSTI in cases.
There are currently no clear recommendations for screening household contacts of cases with recurrent CA S aureus SSTI. Recent recommendations by the Infectious Diseases Society of America state that in households where interpersonal transmission is suspected, decolonization strategies may be considered [26]. Families with high MRSA HHCP (and thus at increased risk for ongoing MRSA colonization) might be the optimal target for intervention. To determine the HHCP, household contacts of cases could be cultured. Implementing a household decolonization regimen in households with high HHCP may prevent ongoing colonization and possibly future SSTI. Previously described risk factors for MRSA colonization, such as African American race, low socioeconomic status, and hospitalization or surgery in the past year [6], cannot be altered; however, MRSA HHCP could be manipulated by an intervention such as household level decolonization.
With few exceptions, prior studies of S aureus CP have been performed in the hospital setting. The importance of CP in MRSA nosocomial transmission was demonstrated by Merrer et al [17] in France. They demonstrated that the relative risk for MRSA acquisition increased as weekly CP increased; weekly CP was the only significant and independent risk factor for MRSA nosocomial transmission. A multicenter cohort study performed by Bloemendaal et al [18] looked at the acquisition and cross-transmission of S aureus in intensive care units (ICUs). Cross-transmission accounted for 40% of all S aureus acquisitions in the ICUs studied. This group demonstrated that pre-acquisition CP, defined as the mean percentage of patients in a unit colonized with S aureus during the 3 days preceding the new acquisition, significantly correlated with a higher rate of MRSA and MSSA acquisition. Our study tested this concept in the community setting and likewise found that baseline colonization of household contacts was associated with longitudinal colonization of cases, possibly due to reacquisition.
S aureus transmission dynamics in the outpatient setting have similarities with nosocomial transmission dynamics, but there are significant differences. In the hospital setting, contact with individuals other than healthcare staff is limited. Thus, efforts such as nurse or patient cohorting, contact precautions, and enhancement of environmental cleaning have been successful in decreasing S aureus transmission [16]. Although these prevention measures are effective at interrupting transmission between patients in the hospital, they may not be applicable after patients are discharged. In the community setting, people in households share personal items with each other and interact with people outside of the household. It is clear that CA S aureus is a disease of households, characterized by recurrences of SSTI in cases and their household contacts [8, 10, 12, 27]; due to the lack of understanding of the household transmission dynamics of S aureus, efforts to control transmission in the community have been challenging.
As shown in a prior study by our group, children colonized with CA MRSA are at higher risk for subsequent SSTI [10]. In this study, we found a relationship between S aureus HHCP and a history of SSTI in household contacts in the year prior to study enrollment. On the basis of these findings, it was surprising that no relationship was demonstrated between baseline S aureus HHCP and recurrent SSTI in cases. This may be because all cases performed decolonization measures, because this was a subcohort from an intervention study. Decolonizing cases may have masked our ability to find a relationship between HHCP and recurrent infection. There could also be other unmeasured influences on infection development. The routes by which disease-causing MRSA is acquired need to be more thoroughly examined. As previously posited by Miller and Diep [14], the reservoir of MRSA might not be endogenous colonization exclusively; environmental sources might influence CA MRSA transmission. Acquisition could also come from sources external to the household. If these other routes play an important role in the transmission of S aureus in the community setting, we might expect SSTI to occur even in households with low HHCP.
This study is limited in that the colonization status of household contacts was ascertained at only one time (baseline). Therefore, we were unable to determine the natural history of household contacts' S aureus colonization and thus the evolution of CP over the 12-month follow-up period. However, we did achieve a high rate of participation from household contacts, with 90% of these individuals providing colonization swabs at enrollment. Persistent colonization may be influenced by exposure to contaminated fomites, external environments, or other unmeasured confounders. Lastly, although strain typing was not performed, the conclusions of this study are applicable to clinicians treating patients with recurrent SSTI who do not routinely have molecular typing available to guide their treatment practices.
This is the first study to evaluate the effect of S aureus CP in the household setting. This could be a useful tool to predict future MRSA colonization and possibly to identify those families at higher risk of MRSA transmission in order to inform targeted eradication interventions. This study opens many avenues for future research. A validation study directing decolonization measures towards families whose MRSA HHCP is higher than a designated level (such as 20%, the mean in this study) could be performed to determine the potential impact on colonization and SSTI outcomes by targeting these “high-risk” households. The CP concept might also be useful in other outpatient settings, such as schools or daycare centers. Further studies using molecular typing to dissect the relative contributions of endogenous and exogenous sources for S aureus acquisition will also improve our understanding of S aureus transmission dynamics.
Acknowledgments
We thank Drs David Hunstad and Carey-Ann Burnham for thoughtful review of this manuscript. We also thank Emma Epplin and Genevieve Hayek for assistance with patient recruitment.
Disclaimer. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of the National Center for Research Resources or the National Institutes of Health.
Financial support. This work was supported by the Infectious Diseases Society of America/National Foundation for Infectious Diseases Pfizer Fellowship in Clinical Disease; the National Center for Research Resources at the National Institutes of Health (grant numbers UL1-RR024992, KL2RR024994, K23AI091690); the Children's Discovery Institute of Washington University and St Louis Children's Hospital; and the Washington University Department of Pediatrics.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Okuma K, Iwakawa K, Turnidge JD, et al. Dissemination of new methicillin-resistant Staphylococcus aureus clones in the community. J Clin Microbiol. 2002;40:4289–94. doi: 10.1128/JCM.40.11.4289-4294.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daum RS. Community-acquired methicillin-resistant Staphylococcus aureus infections. Pediatr Infect Dis J. 1998;17:745–6. doi: 10.1097/00006454-199808000-00015. [DOI] [PubMed] [Google Scholar]
- 3.From the Centers for Disease Control and Prevention. Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus–Minnesota and North Dakota, 1997–1999. JAMA. 1999;282:1123–5. [PubMed] [Google Scholar]
- 4.Gonzalez BE, Martinez-Aguilar G, Hulten KG, et al. Severe Staphylococcal sepsis in adolescents in the era of community-acquired methicillin-resistant Staphylococcus aureus. Pediatrics. 2005;115:642–8. doi: 10.1542/peds.2004-2300. [DOI] [PubMed] [Google Scholar]
- 5.Martinez-Aguilar G, Avalos-Mishaan A, Hulten K, et al. Community-acquired, methicillin-resistant and methicillin-susceptible Staphylococcus aureus musculoskeletal infections in children. Pediatr Infect Dis J. 2004;23:701–6. doi: 10.1097/01.inf.0000133044.79130.2a. [DOI] [PubMed] [Google Scholar]
- 6.Fritz SA, Garbutt J, Elward A, et al. Prevalence of and risk factors for community-acquired methicillin-resistant and methicillin-sensitive Staphylococcus aureus colonization in children seen in a practice-based research network. Pediatrics. 2008;121:1090–8. doi: 10.1542/peds.2007-2104. [DOI] [PubMed] [Google Scholar]
- 7.Daum RS, Clinical practice. Skin and soft-tissue infections caused by methicillin-resistant Staphylococcus aureus. N Engl J Med. 2007;357:380–90. doi: 10.1056/NEJMcp070747. [DOI] [PubMed] [Google Scholar]
- 8.Johansson PJ, Gustafsson EB, Ringberg H. High prevalence of MRSA in household contacts. Scand J Infect Dis. 2007;39:764–8. doi: 10.1080/00365540701302501. [DOI] [PubMed] [Google Scholar]
- 9.Jones TF, Creech CB, Erwin P, et al. Family outbreaks of invasive community-associated methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis. 2006;42:e76–8. doi: 10.1086/503265. [DOI] [PubMed] [Google Scholar]
- 10.Fritz SA, Epplin EK, Garbutt J, Storch GA. Skin infection in children colonized with community-associated methicillin-resistant Staphylococcus aureus. J Infect. 2009;59:394–401. doi: 10.1016/j.jinf.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dietrich DW, Auld DB, Mermel LA. Community-acquired methicillin-resistant Staphylococcus aureus in southern New England children. Pediatrics. 2004;113:e347–52. doi: 10.1542/peds.113.4.e347. [DOI] [PubMed] [Google Scholar]
- 12.Huijsdens XW, van Santen-Verheuvel MG, Spalburg E, et al. Multiple cases of familial transmission of community-acquired methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2006;44:2994–6. doi: 10.1128/JCM.00846-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Osterlund A, Kahlmeter G, Bieber L, et al. Intrafamilial spread of highly virulent Staphylococcus aureus strains carrying the gene for Panton-Valentine leukocidin. Scand J Infect Dis. 2002;34:763–4. doi: 10.1080/00365540260348554. [DOI] [PubMed] [Google Scholar]
- 14.Miller LG, Diep BA. Colonization, fomites, and virulence: rethinking the pathogenesis of community-associated methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis. 2008;46:752–60. doi: 10.1086/526773. [DOI] [PubMed] [Google Scholar]
- 15.Lautenbach E, Tolomeo P, Nachamkin I, et al. The impact of household transmission on duration of outpatient colonization with methicillin-resistant Staphylococcus aureus. Epidemiol Infect. 2010;138:683–5. doi: 10.1017/S0950268810000099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams VR, Callery S, Vearncombe M, Simor AE. The role of colonization pressure in nosocomial transmission of methicillin-resistant Staphylococcus aureus. Am J Infect Control. 2009;37:106–10. doi: 10.1016/j.ajic.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Merrer J, Santoli F, Appere de Vecchi C, et al. “Colonization pressure” and risk of acquisition of methicillin-resistant Staphylococcus aureus in a medical intensive care unit. Infect Control Hosp Epidemiol. 2000;21:718–23. doi: 10.1086/501721. [DOI] [PubMed] [Google Scholar]
- 18.Bloemendaal AL, Fluit AC, Jansen WM, et al. Acquisition and cross-transmission of Staphylococcus aureus in European intensive care units. Infect Control Hosp Epidemiol. 2009;30:117–24. doi: 10.1086/593126. [DOI] [PubMed] [Google Scholar]
- 19.Bonten MJ, Slaughter S, Ambergen AW, The role of, et al. “colonization pressure” in the spread of vancomycin-resistant enterococci: an important infection control variable. Arch Intern Med. 1998;158:1127–32. doi: 10.1001/archinte.158.10.1127. [DOI] [PubMed] [Google Scholar]
- 20.Dubberke ER, Reske KA, Olsen MA, et al. Evaluation of Clostridium difficile-associated disease pressure as a risk factor for C. difficile-associated disease. Arch Intern Med. 2007;167:1092–7. doi: 10.1001/archinte.167.10.1092. [DOI] [PubMed] [Google Scholar]
- 21.Lawrence SJ, Puzniak LA, Shadel BN, et al. Clostridium difficile in the intensive care unit: epidemiology, costs, and colonization pressure. Infect Control Hosp Epidemiol. 2007;28:123–30. doi: 10.1086/511793. [DOI] [PubMed] [Google Scholar]
- 22.Fritz SA, Hogan PG, Hayek G, et al. Household versus individual approaches to eradication of community-associated Staphylococcus aureus in children: a randomized trial. Clin Infect Dis. 2012;54:743–51. doi: 10.1093/cid/cir919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clinical and Laboratory Standards Institute. Wayne, PA: Clinical and Laboratory Standards Institute; 2012. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Second Informational Supplement. [Google Scholar]
- 24.Creech CB, Kernodle DS, Alsentzer A, et al. Increasing rates of nasal carriage of methicillin-resistant Staphylococcus aureus in healthy children. Pediatr Infect Dis J. 2005;24:617–21. doi: 10.1097/01.inf.0000168746.62226.a4. [DOI] [PubMed] [Google Scholar]
- 25.Kaplan SL. Community-acquired methicillin-resistant Staphylococcus aureus infections in children. Semin Pediatr Infect Dis. 2006;17:113–9. doi: 10.1053/j.spid.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52:e18–55. doi: 10.1093/cid/ciq146. [DOI] [PubMed] [Google Scholar]
- 27.Ellis MW, Hospenthal DR, Dooley DP, et al. Natural history of community-acquired methicillin-resistant Staphylococcus aureus colonization and infection in soldiers. Clin Infect Dis. 2004;39:971–9. doi: 10.1086/423965. [DOI] [PubMed] [Google Scholar]


