SUMMARY
Resection and simultaneous reconstruction with free flaps of wide tumours of the scalp and posterior neck region are difficult to perform through a single surgical approach. In such cases, the park-bench position – a lateral oblique position – could allow simultaneous resection and reconstruction of tumours of the scalp and occipital region without changing the patient's position. In the case described here, this position was used to treat microcystic adnexal carcinoma in a patient who presented with three scalp lesions and a lesion of the right scapular region. This arrangement allowed both resection and reconstruction with a microvascular flap without changing the patient's position, as a result of being able to find neck vessels suitable for microanastomosis. Reconstruction was carried out using a right latissimus dorsi myogenous and subcutaneous flap, and anastomoses were created between the thoracodorsal artery and vein, and the transverse cervical artery and vein. In this position, transverse cervical vessels are well placed, with good exposure, and are in an optimal location for use in microvascular surgery. At 8 months post-reconstruction, the patient was in good condition without local recurrence or distant metastases, and the flap showed a good lining and contour. In conclusion, the park-bench position facilitates surgical excision, flap harvesting and microsurgery in the same patient position.
KEY WORDS: Park-bench position, Maxillofacial, Free flap, Scalp reconstruction
RIASSUNTO
La simultanea demolizione e ricostruzione con lembi liberi di estesi tumori dello scalpo e della regione cervicale posteriore è difficile da eseguire mediante un singolo approccio chirurgico. In questi casi, la posizione park-bench – una posizione laterale obliqua – può permettere la simultanea demolizione e ricostruzione dello scalpo e della regione occipitale senza cambiare la posizione del paziente. Nel caso descritto, questa posizione è stata usata nel trattamento di un carcinoma microcistico annessiale, in un paziente che presentava tre lesioni del cuoio capelluto e una lesione della regione scapolare destra. Ciò ha permesso la demolizione e la ricostruzione con un lembo microvascolare senza variare la posizione del paziente, grazie alla possibilità di utilizzare i vasi del collo per le microanastomosi. La ricostruzione è stata effettuata mediante un lembo muscolare e sottocutaneo di latissimo del dorso, e le microanastomosi sono state effettuate tra l'arteria e la vena toracodorsale e l'arteria e la vena cervicale trasversa. Infatti, in questa disposizione, i vasi cervicali trasversi cadono bene, con una buona esposizione, diventando un'ottima collocazione per la chirurgia microvascolare. A 8 mesi dalla ricostruzione il paziente è in buona salute senza ripresa di malattia localmente e a distanza, il lembo presenta un buon "lining e contour". In conclusione, la posizione di park-bench permette la resezione chirurgica, il prelievo del lembo e la fase microchirurgica senza variare la posizione del paziente.
Introduction
Resection and simultaneous reconstruction with free flaps of wide tumours of the scalp and posterior neck region are difficult to perform through a single surgical approach 1. The sitting position was first proposed in neurosurgical practice by Albin and colleagues 2, and has several possible advantages including improved surgical exposure and anatomical orientation 3. Although the sitting position is ideal, most anaesthesiologists refuse the routine use of this position because of the risk of air embolism, which can be fatal 4, especially during bone surgery. Alternative approaches to the occipital and posterior neck region have been conventionally performed with the lateral and park-bench positions 4-6.
The park-bench position 7– a lateral oblique position – could allow simultaneous resection and reconstruction of tumours of the scalp and occipital region without changing the patient's position. This is useful when the surgeon is performing excision of a widely infiltrated tumour that needs wide margins and free flap reconstruction. In the case described here, the park-bench position was used to treat microcystic adnexal carcinoma (MAC), a rare eccrine gland tumour with low-grade malignancy and a low probability of metastasis. It has a tendency towards neurotropic spread and presents as multifocal with widely infiltrated margins. These characteristics make excisional surgery particularly challenging 8-10, and wide excision requires microsurgical reconstruction.
Clinical technique and technology
In May 2011, a 56-year-old man was seen for multiple skin lesions of the scalp and scapular region. The case history revealed previous surgical excision of a benign lesion of the scalp several years earlier (histopathological results not available), and, from July 2010, multiple interventions for excision of neoplasms of the scalp, which was confirmed histopathologically as MAC. The excision margins of both scalp and scapular lesions exhibited infiltration.
Clinically, the patient presented with three scalp lesions (two as scars from previous interventions (6 and 3 cm, respectively), one in the cranial portion (Fig. 1), and a lesion of the right scapular region (a linear scar from previous intervention, measuring 5.5 cm); each lesion presented as a hard rubbery neoplasm involving the deep planes.
Fig. 1.
The patient presented with three scalp lesions (two in scars from previous interventions (6 and 3 cm, respectively), one in the cranial portion, and a lesion of the right scapular region (a linear scar from a previous intervention, measuring 5.5 cm); each lesion presented as a hard rubbery neoplasm involving the deep planes.
Contrast computed tomography of the head and neck revealed the three lesions of the scalp and the scapular lesion infiltrating the deep planes, without cranial bone invasion. According to the reduced glucidic metabolism of the eccrine component of the adnexal tumours, positron emission tomography (PET) did not show any area of high glucidic metabolism.
To achieve both resection and reconstruction in a single surgical session, the patient was placed in the lateral decubitus position (park-bench position) (Fig. 2), and the upper half of the body was tilted upward by 30°, after orotracheal intubation with an 8.0 mm internal diameter endotracheal tube. The patient's head was rotated face down by 30°, the vertex tilted down by 15-30° and the chin was flexed down by 15° so that the nuchal muscles were extended adequately. The left shoulder and arm were positioned outside the operating table, and the arm was supported by a sling. The right arm was positioned on a stack of blankets and taped to the table. An axillary roll was positioned just caudal to the left axilla. A pillow was positioned between the legs, which were flexed. A Mayfield headrest was applied (Fig. 2). This arrangement allowed both resection and reconstruction with local or microvascular flaps without changing the patient's position, so that the neck vessels are suitable for microanastomosis. MAC has a tendency towards local infiltration and neurotropic spread; therefore, surgery included wide resection margins of the parieto-occipito-temporal scalp (deep margin including the pericranium) and skin of the posterior neck (Fig. 3), and excision and radicalization of the scapular lesion.
Fig. 2.
The park-bench position is a variation of the lateral position. In this position, the dependent shoulder and arm are positioned outside the operating table and the arm is supported by a sling.
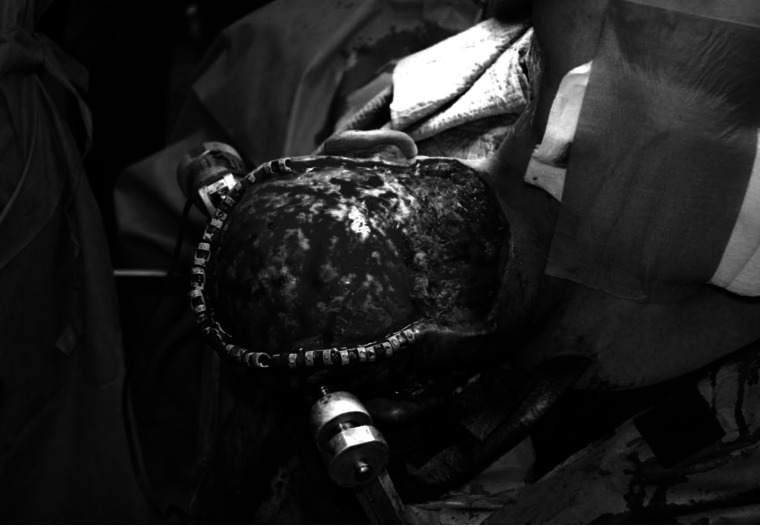
Fig. 3.
MAC has a tendency to local infiltration and neurotropic spread; therefore, surgery requires wide resection margins of the parieto-occipitotemporal scalp (deep margin including the pericranium) and skin of the posterior neck.
A cervical lymph node biopsy at V level in the right neck was performed. Intraoperative frozen section analysis of the circumferential resection margins, deep pericranium margin and neck V level lymph nodes was performed.
Reconstruction was carried out using a right latissimus dorsi myogenous and subcutaneous flap (Fig. 4). The muscular and subcutaneous component was adequately shaped to fill the scalp defect, and the vascular pedicle (thoracodorsal vessels) was isolated. The flap was grafted in the defect area, and anastomoses were created between the thoracodorsal artery and vein, and the transverse cervical artery and vein (Fig. 5). Usually, the park-bench position makes exposure difficult of the most-used vessels for microvascular anastomoses (such as facial artery and vein) during head and neck reconstructive surgery. However, in this position, transverse cervical vessels are well placed, with good exposure, and are in an optimal location for use in microvascular surgery (Fig. 5). A full-thickness skin graft was harvested from the anteromedial thigh, and was fashioned to cover the latissimus dorsi flap in the defect area and the scapular residual defect.
Fig. 4.
In the present case, the park-bench position allowed both resection and defect reconstruction in a single surgical approach, without changing the patient's position.
Fig. 5.

In the park-bench position, transverse cervical vessels are well placed, with good exposure, and are in an optimal location for use in microvascular surgery. Anastomoses were created between the thoracodorsal artery and vein, and the transverse cervical artery and vein.
During postoperative recovery, focal skin necrosis occurred at the donor site. This complication was treated by surgical revision and two full-thickness skin grafts harvested from the contralateral anteromedial thigh; during the following days, the patient underwent 20 sessions of hyperbaric oxygen therapy, and healed uneventfully.
Histopathological examination of the scalp sample showed epithelial proliferation that progressively involved microcysts, strands and cords as the tumour invaded the deeper tissues from the skin surface, MAC-wide and multifocal invasion of the dermohypodermal layer, with micronests and solid cords consisting of mildly atypical monomorphous cuboid cells embedded in an abundant desmoplastic stroma, with perineural invasion, was observed. In addition, the right scapular sample reported focal hypodermal invasion of MAC. In both cases, surgical margins were clear of cancer cells.
Metastasis was found in the occipital lymph node, without extracapsular spread; UICC TNM staging of the tumour was T3N1M0, stage III.
Eight weeks postoperatively, radiotherapy was administered. In particular, brachytherapy focused on the posterior scalp, occipital region and bilateral neck. A total dose of 54 Gy in 27 fractions (2 Gy/fraction) was administered. At 8 months post-reconstruction, the patient was in good health without local recurrence or distant metastases. In particular, the flap showed a good lining and contours, but had a colour mismatch (Fig. 6).
Fig. 6.
Postoperative view (8-month follow-up).
The park-bench position allows surgical excision, flap harvesting and microsurgery in the same patient position.
Discussion
In wide resection of the scalp, occipital region and posterior aspect of the neck, the park-bench position allows both surgical excision and defect reconstruction in a single approach. Essential advantages are decreased operating time without complications of other surgical positions 11.
Indeed, the use of the sitting or upright position for patients undergoing posterior neck and occipital surgery facilitates surgical access, but presents unique physiological challenges for the anaesthesiologist with the potential for serious complications 2, especially in bone surgery. These complications include haemodynamic instability, venous air embolism (VAE) with the possibility of paradoxical air embolism, pneumocephalus, quadriplegia and compressive peripheral neuropathy 12. Alternative positions for surgical access to the occipital and nuchal region include the prone and lateral positions 13. The prone position provides good exposure of the dorsal surface of the body, and allows access to the posterior head, neck and spinal column 14.
However, in the present case, the prone position did not allow contemporary reconstruction of the scalp defect, since in raising the latissimus dorsi flap, we had to move the patient to a lateral position.
An inferior scapular flap could be an alternative reconstructive solution, but in the presented case a homolateral subcutaneous scapular lesion was present. Moreover, the latissimus dorsi muscle has long been the flap of choice for reconstruction of extensive scalp defects. Its many attributes make it well suited for the role; i.e. a flat muscle with a large surface area, constant pedicle of good length and calibre and negligible donor site morbidity. Although initially bulky and unsightly, the eventual aesthetics of a latissimus dorsi free flap following muscle atrophy and skin graft maturation are very acceptable 15.
In the present case, excision of the neoplasm required wide tissue resection due to the wide resection margins necessary for the histopathological features of the MAC. MAC has a tendency to neurotropic spread and presents with widely infiltrated margins, and repairing the resulting defect poses a considerable reconstructive challenge 10.
In conclusion, the park-bench position facilitates exposure of suitable neck vessels, especially the transverse cervical artery and vein. Indeed, in cases where free tissue transfer is needed, placing patients in this position enables successful resection, and is an optimal choice for microvascular anastomosis.
References
- 1.Fujitsu K, Kitsuta Y, Takemoto Y, et al. Combined pre- and retrosigmoid approach for petroclival meningiomas with the aid of a rotatable head frame: peri-auricular threequarter twist-rotation approach: technical note. Skull Base. 2004;14:209–215. doi: 10.1055/s-2004-860952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albin MS, Babinski M, Maroon JC, et al. Anaesthetic management of posterior fossa surgery in the sitting position. Acta Anaesth Scand. 1976;20:117–128. doi: 10.1111/j.1399-6576.1976.tb05018.x. [DOI] [PubMed] [Google Scholar]
- 3.Black S, Ockert DB, Oliver WC, Jr, et al. Outcome following posterior fossa craniectomy in patients in the sitting or horizontal positions. Anesthesiology. 1988;69:49–56. doi: 10.1097/00000542-198807000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Sekhar LN, Tzortzidis F, Bucur SD. Patient positioning for cranial microsurgery. In: Sekhar LN, Oliveira E, editors. Cranial microsurgery. New York: Thieme; 1999. pp. 12–18. [Google Scholar]
- 5.Heros RC. Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg. 1986;64:559–562. doi: 10.3171/jns.1986.64.4.0559. [DOI] [PubMed] [Google Scholar]
- 6.Samii M, Cheatham M, Becker DP. Atlas of cranial base surgery. Philadelphia: W.B. Saunders Company; 1995. pp. 54–57. [Google Scholar]
- 7.Maniglia AJ, Fenstermaker RA, Ratcheson RA. Preservation of hearing in the surgical removal of cerebellopontine angle tumors. Otolaryngol Clin North Am. 1989;22:211–232. [PubMed] [Google Scholar]
- 8.Friedman PM, Friedman RH, Jiang SB, et al. Microcystic adnexal carcinoma: collaborative series review and update. J Am Acad Dermatol. 1999;41:225–231. doi: 10.1016/s0190-9622(99)70053-8. [DOI] [PubMed] [Google Scholar]
- 9.Goldstein DJ, Barr RJ, Santa Cruz DJ. Microcystic adnexal carcinoma: a distinct clinicopathologic entity. Cancer. 1982;50:566–572. doi: 10.1002/1097-0142(19820801)50:3<566::aid-cncr2820500330>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 10.Beltramini GA, Baj A, Moneghini L, et al. Microcystic adnexal carcinoma of the centrofacial region: a case report. Acta Otorhinolaryngol Ital. 2010;30:213–213. [PMC free article] [PubMed] [Google Scholar]
- 11.Porter JM, Pidgeon C, Cunningham AJ. The sitting position in neurosurgery: a critical appraisal. Br J Anaesth. 1999;82:117–128. doi: 10.1093/bja/82.1.117. [DOI] [PubMed] [Google Scholar]
- 12.Standefer M, Bay JW, Trusso R. The sitting position in neurosurgery: a retrospective analysis of 488 cases. Neurosurgery. 1984;14:649–658. doi: 10.1227/00006123-198406000-00001. [DOI] [PubMed] [Google Scholar]
- 13.St-Arnaud D, Paquin MJ. Safe positioning for neurosurgical patients. AORN J. 2008;87:1156–1168. doi: 10.1016/j.aorn.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 14.O'Connell P. Positioning impact on the surgical patient. Nurs Clin North Am. 2006;41:173–192. doi: 10.1016/j.cnur.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 15.Ch'ng S, Clark JR. The scapular angle adds versatility to the latissimus dorsi free flap in complicated scalp reconstruction. J Plast Reconstr Aesthet Surg. 2011;64:e248–e249. doi: 10.1016/j.bjps.2011.03.032. [DOI] [PubMed] [Google Scholar]