SUMMARY
The diagnostic role of audio-impedancemetry in superior semicircular canal dehiscence (SSCD) disease is well known. In particular, since the first reports, the presence of evoked acoustic reflexes has represented a determining instrumental exhibit in differential diagnosis with other middle ear pathologies that are responsible for a mild-low frequencies air-bone gap (ABG). Even though high resolution computed tomography (HRCT) completed by parasagittal reformatted images still represents the diagnostic gold standard, several instrumental tests can support a suspect of labyrinthine capsule dehiscence when "suggestive" symptoms occur. Objective and subjective audiometry often represents the starting point of the diagnostic course aimed at investigating the cause responsible for the so-called "intra-labyrinthine conductive hearing loss".
The purpose of this study is to evaluate the role of tympanometry, in particular of the inter-aural asymmetry ratio in peak compliance as a function of different mild-low frequencies ABG on the affected side, in the diagnostic work-up in patients with unilateral SSCD. The working hypothesis is that an increase in admittance of the "inner-middle ear" conduction system due to a "third mobile window" could be detected by tympanometry. A retrospective review of the clinical records of 45 patients with unilateral dehiscence selected from a pool of 140 subjects diagnosed with SSCD at our institution from 2003 to 2011 was performed. Values of ABG amplitude on the dehiscent side and tympanometric measurements of both ears were collected for each patient in the study group (n = 45). An asymmetry between tympanometric peak compliance of the involved side and that of the contralateral side was investigated by calculating the inter-aural difference and the asymmetry ratio of compliance at the eardrum. A statistically significant correlation (p = 0.015 by Fisher's test) between an asymmetry ratio ≥ 14% in favour of the pathologic ear and an ABG > 20 dB nHL on the same side was found. When "evocative" symptoms of SSCD associated with important ABG occur, the inter-aural difference in tympanometric peak compliance at the eardrum in favour of the "suspected" side could suggest an intra-labyrinthine origin for the asymmetry. Tympanometry would thus prove to be a useful instrument in clinical-instrumental diagnosis of SSCD in detection of cases associated with alterations of inner ear impedance.
KEY WORDS: Superior semicircular canal dehiscence, Tympanometry, Inner ear impedance, Intra-labyrinthine conductive hearing loss
RIASSUNTO
Il ruolo diagnostico svolto dall'audio-impedenzometria nella patologia da deiscenza del canale semicircolare superiore (DCSS) è noto da tempo. In particolare la presenza di riflessi stapediali evocabili ha rappresentato fin dai primi studi un reperto strumentale determinante nella diagnosi differenziale con altre patologie dell'orecchio medio responsabili della presenza di un gap trasmissivo sui toni mediogravi. Nonostante lo studio TC ad alta risoluzione completo di ricostruzioni lungo i piani dei CSS rappresenti ancora il gold standard diagnostico, in presenza di sintomi "evocativi" numerosi sono gli esami strumentali in grado di avvalorare il sospetto di deiscenza della capsula labirintica. L'audiometria soggettiva ed oggettiva rappresenta spesso il punto di partenza dell'iter diagnostico mirato alla ricerca della causa responsabile del cosiddetto "deficit di conduzione intra-labirintico". L'obbiettivo di questo studio è valutare il ruolo della timpanometria, in particolare dell'asymmetry ratio inter-aurale tra i picchi di compliance in funzione dell'entità del deficit trasmissivo del lato patologico, nella diagnosi di DCSS monolaterale. L'ipotesi è che l'aumento di ammettenza del sistema di conduzione "orecchio medio-interno" determinato dalla presenza di una "terza finestra mobile" possa venire in tal modo oggettivato. Sono stati a tal proposito revisionati retrospettivamente i dati clinici di un sottocampione di 45 pazienti affetti da deiscenza monolaterale appartenente al gruppo di 140 soggetti cui è stata posta diagnosi di DCSS presso il nostro istituto dal 2003 al 2011. Per ogni paziente sono stati raccolti i valori di ampiezza di deficit trasmissivo del lato affetto ed i dati timpanometrici bilaterali. è stata ricercata un'asimmetria tra il picco di compliance del lato affetto e quello del lato sano calcolando la differenza di compliance inter-aurale e la asymmetry ratio, ottenendo una correlazione statisticamente significativa (p = 0,015 al test di Fisher) tra asymmetry ratio ≥ 14% a favore del lato patologico ed un gap trasmissivo > 20 dB nHL omolaterale. In presenza dunque di sintomi "evocativi" di DCSS e di un importante deficit trasmissivo, la differenza inter-aurale tra i picchi di compliance timpanometrici a favore del lato "sospetto" potrebbe pertanto far ipotizzare un'origine intra-labirintica di tale asimmetria. La timpanometria si dimostrerebbe quindi utile strumento nella diagnostica clinico-strumentale della patologia da deiscenza potendo individuare i casi associati ad alterazioni dell'impedenza dell'orecchio interno.
Introduction
Superior semicircular canal dehiscence (SSCD) syndrome is a recently described pathological condition caused by the absence of the bony roof of the anterior semicircular canal that results in abnormal exposure of the inner ear to the action of the surrounding structures 1. The lesion is responsible for the onset of substantial variance of both cochlear and vestibular symptoms including imbalance, sound and/or pressure induced vertigo, autophony and hyperacusis 1 2. The reason why some patients develop only vestibular or cochlear symptoms, while in others both patterns are clearly present, has not been clarified. Although clinical and instrumental findings expressing the vestibular features of the pathology, and in particular vertical/torsional nystagmus induced by sound and/or pressure stimuli, first allowed Minor et al. to characterize this clinical entity 1 2, the diagnostic role of audiometry and impedance audiometric testing in SSCD has been well established. Mainly, a mild-low frequency air-bone gap (ABG) associated with evoked acoustic reflexes has represented a determining instrumental sign in differential diagnosis with other middle ear pathologies since the first reports 2 3. In fact, it is well known that in some patients with SSCD this pathological third-window lesion becomes responsible for dissipation of acoustic energy at low frequencies through the vestibule, resulting in hearing loss by air conduction and improvement of cochlear sensitivity to bone-conducted sounds 4 5. A tendency to lateralize the Weber tuning fork test to the affected side, even positioning the instrument away from the head, has also been described as a distinctive feature of this condition in addition to values of bone conduction threshold < 0 dB nHL 1 2. Even though high resolution computed tomography (HRCT) completed by parasagittal reformatted images along the plane of the SSC definitely continues to represent the gold standard 6, several instrumental tests can support a diagnostic hypothesis of labyrinthine capsule dehiscence when "suggestive" symptoms occur. Among these, the study of vestibular evoked myogenic potentials (VEMPs) has assumed a crucial role 7 8, especially after the recent introduction of ocular VEMPs 9 10. Nonetheless, in daily clinical practice subjective and objective audiometry often represents the starting point of the diagnostic course aimed at investigating the cause responsible for the socalled "inner ear conductive hearing loss" 11 - 13.
The purpose of this study is to confirm the diagnostic value of the well established audiometric patterns of SSCD and detect additional "evocative" audio-impedancemetric patterns. In particular, this analysis was made to demonstrate SSCD-induced increased ear admittance (due to the "third-window mechanism") through tympanometric testing to determine whether the ear affected by SSCD showed a statistically significant higher amplitude in peak compliance compared to the controlateral ear under different conditions of ABG measurement.
Methods
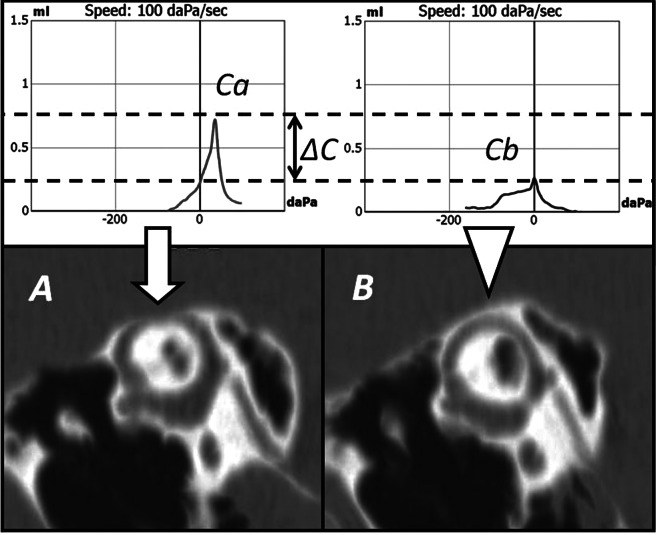
A retrospective review of the clinical records of 140 patients (70 males and 70 females, mean age = 53 years, range = 8-80 years) diagnosed with SSCD at the ENT Unit of our institution over a 9-year period (January 2003 - September 2011) was performed. Among these, 46 subjects (33%) presented with bilateral dehiscence. Diagnostic criteria were radiological evidence of bony dehiscence of the superior canal as well as at least one suggestive sign of SSCD on vestibular testing (sound and/or pressure-evoked eye movements or threshold lowering of VEMPs). All patients had underwent the same detailed audio-vestibular evaluation including full anamnesis, otoscopy, audio-impedancemetric testing, infrared video-oculoscopic examination, bi-mastoid vibration test, air-conducted cervical VEMPs (c-VEMPs) study with threshold analysis and temporal bone HRCT scans with multiplanar reconstructions on the plane aligning with vertical canals. Since the aim of this study is to identify through tympanometry SSCD-induced asymmetry in admittance between the ears of each subject enrolled in the analysis, cases affected by bilateral dehiscence (n = 46) were excluded from the investigation because of the considerable inter-individual variance in impedancemetric measurements emerging from literature 14 - 18. Attention was thus focused on the inter-aural gap in tympanometric peak compliance in unilateral cases. A sub-sample of 45 patients with unilateral SSCD (23 males and 22 females, mean age = 53 years, range age = 8-80 years, 20 right affected ears, 25 left affected ears) was included in this study, once those cases associated with external and/ or middle ear pathologies or with previous ear surgery (n = 49) because of their unsuitability for a tympanometric study were excluded. All patients had intact tympanic membranes at otoscopy. Pure-tone audiometry was examined using standard clinical procedures to obtain air conduction (125-8000 Hz) and bone conduction (250-4000 Hz) thresholds with masking if needed. For each affected ear, the mean mild-low frequency ABG was calculated by using the pure tone average (PTA) between gaps at 250 and 500 Hz. Impedancemetry was performed with the aid of an Amplaid 728 impedance meter, with patients in a sitting position. Standard tympanometry (using a 226 Hz probe tone) showed bilateral type-A peaked curves 16 in all 45 subjects, with peak compliance ranging within endomeatal pressure values of -100 and +100 daPa. For each patient, the mean value among 3 consequent tympanometric measurements performed within 30 min with the subject in the same position was collected and considered in the analysis. In all cases in which an ossicular discontinuity was suspected, tympanometry with 667 Hz-probe tone was performed to exclude this. For each subject belonging to this sub-sample, asymmetry between tympanometric peak compliance of the ear involved by dehiscence (Ca) and that of the contralateral ear (Cb) was investigated by calculating the inter-aural difference of compliance (ΔC) at the eardrum (Fig. 1), and the asymmetry ratio (ΔC%) expressing in percentage the ratio of ΔC to the sum of the 2 values of compliance as shown below:
Fig. 1.
The upper image shows tympanometric peak compliance measurements of the right dehiscent ear (Ca) and the left healthy ear (Cb) corresponding to impedancemetric data of the patient n. 25 from the study group. Two parallel dotted lines indicate the levels corresponding to the peak compliances of the two sides (0.73 ml for the right side and 0.27 ml for the left side). The distance between the two dotted lines indicates the inter-aural difference (ΔC) in tympanometric peak compliance (0.46 ml in this case). The lower images represent the HRCT reformatted scans aligning with the plane of the SSC (Pöschl plane) of the same patient. Fig. 1A represents the right affected superior canal (dehiscence indicated by the arrow). Fig. 1B represents the left superior canal (intact bony roof indicated by the arrowhead).
According to the literature, differences of ΔC ≥ 0.22 ml and asymmetry ratios of ΔC% ≥ 14% have been assumed as to be sufficient to express a significant (pathologic) impedancemetric difference between the two ears. The subsample of 45 patients was then stratified for different values of ABG amplitude on the affected ear and correlations between ΔC and ΔC% in favour of the pathological side, and different ABG entities on the affected ear were finally investigated. To determine if correlations were statistically significant, a X 2 test (chi-square test, Fisher's test) was used to analyze the data. A 0.05 level of significance (p) was considered statistically significant.
Results
Of the 91 patients remaining after excluding from the initial pool those cases associated with positive histories for pathological middle and/or external ear-system processes and those with previous ear surgery (n = 49), 87% presented with at least one cochlear symptom in anamnesis (hyperacusis, hearing loss, tinnitus, autophony, aural fullness). Among these, 58 subjects complained of hearing loss on the pathological side. Analyzing the audiometric records of the ears affected by SSCD (n = 137, with 45 ears from 45 patients affected by unilateral dehiscence and 92 ears from 46 patients with bilateral SSCD), 13 (9%) were consistent with normal hearing function, 27 ears (20%) showed sensorineural hearing loss, while in 41 cases (30%) the type of hearing impairment was mixed and in 56 ears (41%) was conductive (14 cases presented with values of bone conduction threshold < 0 dB nHL). Despite the presence of a mild-low frequencies ABG in 71% of audiometric tests (n = 97), 80 cases showed normally evoked acoustic reflexes. Of the mean mild-low frequencies ABG for each ear in this group, 47 audiograms had an ABG < 15 dB nHL, 37 had an ABG ≥ 15 dB nHL and ≤ 30 dB nHL, and 13 had an ABG > 30 dB nHL. Gap values ranged from 7.5 dB to 55 dB nHL, with a mean value of 18.3 dB nHL, a median of 15 dB nHL and standard deviation (SD) of 12.2 dB nHL. Concerning the sub-sample of 45 patients affected by unilateral dehiscence, the hearing function of the pathological ear was normal in 2 cases (4%) and consistent with sensorineural hearing loss in 6 ears (13%), while mixed type hearing impairment was registered in 16 cases (36%) and conductive in 21 ears (47%), with 4 cases presenting with values of bone conduction threshold < 0 dB nHL. As for impedancemetry, ipsi- and contralateral acoustic reflexes were bilaterally present in 35 patients, bilaterally absent in 5 cases, absent only contralaterally to the lesion in 4 patients and absent only ipsilaterally to the lesion in 1 case. Tympanometric peak compliance ranged between 0.18 and 2.77 ml (mean = 0.82 ml, median = 0.75 ml, SD = 0.47 ml), with mean peak compliance on affected ears of 0.83 ml (median = 0.76 ml, SD = 0.45 ml) and mean peak compliance on non-involved ears of 0.81 ml (median = 0.75 ml, SD = 0.50 ml). For each patient in the study group, between ear-difference in tympanometric peak compliance was measured and expressed in terms of inter-aural difference (ΔC) and asymmetry ratio (ΔC%) of compliance as previously described. Measurements of ΔC ranged from 0 to 1.81 ml (mean = 0.28 ml, median = 0.17 ml, SD = 0.33 ml) and ΔC% values ranged between 0 and 82% (mean = 15.8%, median = 14%, SD = 14.3%) (Table I).
Table I.
Audio-impedancemetric data of the study group: SSCD side = side affected by superior semicircular canal dehiscence; ABG = mean air-bone gap between gap values at 250 and 500 Hz on the pathological ear; Ca = tympanometric peak compliance on the affected ear; SRa = stapedial reflexes on the affected side; Cb = tympanometric peak compliance on the healthy ear; SRb = stapedial reflexes on the healthy side; |ΔC| = absolute value of inter-aural difference between tympanometric peak compliances; |ΔC%| = absolute value of inter-aural asymmetry ratio between tympanometric peak compliances; M = male; F = female; R = right; L = left; P = present; A = absent.
| Patient | Age | Sex | SSCD side | ABG (dB) | Ca (ml) | SRa | Cb (ml) | SRb | |ΔC| (ml) | |ΔC%| (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 75 | F | R | 0 | 0.82 | P | 0.95 | P | 0.13 | 7 |
| 2 | 59 | M | L | 25 | 0.76 | P | 0.77 | P | 0.01 | 1 |
| 3 | 54 | F | L | 22.5 | 0.68 | P | 0.51 | P | 0.17 | 14 |
| 4 | 8 | F | L | 25 | 0.33 | P | 0.20 | P | 0.13 | 25 |
| 5 | 22 | F | R | 17.5 | 1.87 | P | 1.42 | P | 0.45 | 14 |
| 6 | 33 | M | R | 25 | 0.43 | P | 0.59 | P | 0.16 | 16 |
| 7 | 62 | M | L | 10 | 0.75 | P | 1.30 | A | 0.55 | 27 |
| 8 | 55 | F | L | 52.5 | 0.35 | P | 0.29 | P | 0.06 | 9 |
| 9 | 53 | F | R | 7.5 | 0.58 | P | 0.56 | P | 0.02 | 2 |
| 10 | 63 | M | L | 55 | 1.12 | A | 0.85 | A | 0.27 | 14 |
| 11 | 54 | M | L | 22.5 | 0.56 | P | 0.95 | P | 0.39 | 26 |
| 12 | 58 | F | R | 12.5 | 0.84 | P | 0.64 | P | 0.20 | 14 |
| 13 | 68 | F | L | 7.5 | 1.98 | P | 2.35 | P | 0.37 | 9 |
| 14 | 35 | F | R | 0 | 0.62 | P | 0.74 | P | 0.12 | 9 |
| 15 | 65 | F | R | 17.5 | 0.25 | A | 0.26 | A | 0.01 | 2 |
| 16 | 36 | M | L | 0 | 0.97 | P | 1.22 | P | 0.25 | 11 |
| 17 | 57 | F | R | 12.5 | 0.21 | A | 0.27 | A | 0.06 | 13 |
| 18 | 71 | M | L | 27.5 | 0.55 | P | 0.63 | P | 0.08 | 7 |
| 19 | 37 | M | L | 10 | 0.70 | P | 1.17 | P | 0.47 | 25 |
| 20 | 40 | M | R | 17.5 | 1.01 | P | 1.29 | P | 0.28 | 12 |
| 21 | 37 | M | L | 2.5 | 0.89 | P | 0.58 | P | 0.31 | 21 |
| 22 | 78 | F | L | 35 | 0.79 | P | 0.43 | P | 0.36 | 30 |
| 23 | 18 | F | L | 15 | 1.14 | A | 0.71 | P | 0.43 | 23 |
| 24 | 45 | M | R | 10 | 0.59 | P | 0.75 | P | 0.16 | 12 |
| 25 | 68 | F | R | 22.5 | 0.73 | A | 0.27 | A | 0.46 | 46 |
| 26 | 47 | F | L | 10 | 1.06 | P | 0.79 | P | 0.27 | 15 |
| 27 | 52 | M | R | 15 | 0.85 | P | 0.97 | P | 0.12 | 7 |
| 28 | 41 | F | R | 5 | 1.10 | P | 0.83 | P | 0.27 | 14 |
| 29 | 19 | M | R | 12.5 | 1.01 | P | 0.75 | P | 0.26 | 15 |
| 30 | 67 | M | L | 7.5 | 1.65 | P | 2.77 | P | 1.12 | 25 |
| 31 | 72 | M | L | 20 | 1.04 | P | 1.11 | P | 0.07 | 3 |
| 32 | 50 | M | L | 0 | 0.73 | P | 0.91 | P | 0.18 | 11 |
| 33 | 58 | M | L | 25 | 2.01 | A | 0.20 | A | 1.81 | 82 |
| 34 | 67 | F | R | 17.5 | 0.77 | P | 1.40 | P | 0.63 | 29 |
| 35 | 68 | F | R | 7.5 | 0.18 | P | 0.25 | A | 0.07 | 16 |
| 36 | 37 | M | L | 5 | 0.90 | P | 0.92 | P | 0.02 | 1 |
| 37 | 74 | M | L | 15 | 0.60 | P | 0.75 | P | 0.15 | 11 |
| 38 | 54 | M | L | 12.5 | 0.99 | P | 0.95 | P | 0.04 | 2 |
| 39 | 65 | M | R | 22.5 | 1.82 | P | 0.87 | P | 0.95 | 35 |
| 40 | 70 | F | R | 35 | 0.60 | P | 0.45 | A | 0.15 | 14 |
| 41 | 62 | M | R | 10 | 0.30 | P | 0.46 | P | 0.16 | 21 |
| 42 | 48 | F | L | 0 | 0.70 | P | 0.70 | P | 0.00 | 0 |
| 43 | 61 | M | L | 7.5 | 0.42 | P | 0.42 | P | 0.00 | 0 |
| 44 | 47 | F | L | 12.5 | 0.83 | P | 0.76 | P | 0.07 | 4 |
| 45 | 80 | F | R | 7.5 | 0.49 | P | 0.67 | A | 0.18 | 16 |
Considering 0.22 ml and 14% as the minimal cut-off value expressing a significant (pathologic) ΔC and ΔC% respectively, the relationship of inter-aural asymmetry of tympanometric peak compliance with different amplitudes of mean mild-low frequencies ABG on the affected ear was investigated. This was done to analyze the inter-aural spread of compliance in those patients in which the thirdwindow mechanism should result in a higher dissipation of acoustic energy (as shown by the pseudo-conductive hearing loss in audiometric testing).
Once the study group was stratified in function of the ABG on the affected side, no statistically significant correlation between ears with ABG ≤ 20 dB nHL and subjects with relevant inter-aural ΔC (p = 0.467) (Table II) and ΔC% (p = 0.166) (Table III) in favour of the dehiscent side was obtained. Considering patients with ABG > 20 dB nHL on the affected side, a weak correlation with pathologic ΔC (p = 0.156) (Table IV) and a statistically significant correlation with pathologic ΔC% (p = 0.015) (Table V) in favour of the pathological side was obtained.
Table II.
Correlation between ears with ABG ≤ 20 dB nHL on the affected side and subjects with inter-aural difference between tympanometric peak compliances (ΔC) ≥ 0.22 ml in favour of the pathological side, with the corresponding P value.
| ΔC (ml) | ||||
|---|---|---|---|---|
| ABG (dB nHL) | < 0.22 | ≥ 0.22 | ||
| > 20 | 13 | 5 | 18 | |
| ≤ 20 | 21 | 6 | 27 | |
| 34 | 11 | 45 | ||
p = 0.467
Table III.
Correlation between ears with ABG ≤ 20 dB nHL on the affected side and subjects with inter-aural asymmetry ratio between tympanometric peak compliances (ΔC%) ≥ 14% in favour of the pathological side, with the corresponding P value.
| ΔC% (%) | ||||
|---|---|---|---|---|
| ABG (dB nHL) | < 14 | ≥ 14 | ||
| > 20 | 10 | 8 | 18 | |
| ≤ 20 | 20 | 7 | 27 | |
| 30 | 15 | 45 | ||
p = 0.166
Table IV.
Correlations between ears with ABG > 20 dB nHL on the affected side and subjects with inter-aural difference between tympanometric peak compliances (ΔC) ≥ 0.22 ml in favour of the pathological side, with the corresponding P value.
| ΔC (ml) | ||||
|---|---|---|---|---|
| ABG (dB nHL) | < 0.22 | ≥ 0.22 | ||
| ≤ 20 | 26 | 6 | 32 | |
| > 20 | 8 | 5 | 13 | |
| 34 | 11 | 45 | ||
p = 0.156
Table V.
Correlations between ears with ABG > 20 dB nHL on the affected side and subjects with inter-aural asymmetry ratio between tympanometric peak compliances (ΔC%) ≥ 14% in favour of the pathological side, with the corresponding P value.
| ΔC% (%) | ||||
|---|---|---|---|---|
| ABG (dB nHL) | < 14 | ≥ 14 | ||
| ≤ 20 | 25 | 7 | 32 | |
| > 20 | 5 | 8 | 13 | |
| 30 | 15 | 45 | ||
p = 0.015
Discussion
The existence of the so-called "third windows" was originally proposed by Ranke et al., referring to physiologic secondary fluid pathways between the inner ear and surrounding structures, beyond oval and round windows, being functionally ineffective when the two principal windows are open but coming into play when closed 19. This concept was resumed in experimental studies 20 and then in clinical experience to justify a consistent number of pathological cases with an otherwise unexplained conductive hearing loss 12 21. Similarly, the occurrence of an additional pathological fenestration between the inner ear and the cranial cavity has been hypothesized to be responsible for the onset of those peculiar symptoms and signs, including conductive hearing loss, which led Minor et al. to define SSCD Syndrome 1 - 3. Wide and exhaustive insight into the pathophysiologic basis of the mechanism at the origin of this clinical entity, especially concerning audiometric patterns, has been provided by the group of Merchant and Rosowsky 4 5 22. As clinicians have become familiar with this pathology, the different diagnostic and therapeutic aspects of SSCD have also been gradually pointed out, including instrumental findings that are useful in differential diagnosis with other otologic disorders. Nowadays, a wide series of clues and specific functional tests are available for advancing a diagnostic hypothesis of SSCD before resorting to radiologic confirmation. Over the last 10 years, when conductive hearing loss occurs in audiometric testing, even with poor vestibular symptomatology, clinicians have learned to use intact acoustic reflexes 2 3 and/or preserved air-conducted VEMPs responses (or with threshold lower than normal) 8 as useful tools to recognize a dehiscence pathology from other middle ear affections such as otosclerosis. If available, o-VEMPs 9, laser Doppler vibrometry of the umbo 4 and otoacoustic emissions testing 5 can also assist in diagnosis, sparing the patient unnecessary exploratory tympanotomies or unsuccessful stapedoplasties. To date, little attention has been given to tympanometric study in the diagnostic course of SSCD, and in particular there is a lack of knowledge about maximum compliance values and inter-aural asymmetries between peak compliances at the eardrum in previous case studies. Tympanometry has been classically used to provide diagnostic information on middle ear disorders 16 - 18 23 24. Nevertheless, experimental data supports the theory that mechanical functions in the inner ear can affect compliance measurements at the tympanic membrane. Metz firstly investigated the effects of increased labyrinthine fluid pressure on sound transmission in fresh cadaver temporal bones, yielding measurable impedance changes 14. Macrae and Bulteau found comparable data measuring firstly decreased and then enhanced compliance values by filling a cadaver vestibule with silastic and then draining the cochlear fluid, respectively 25. Other authors have then confirmed that impedancemetry and tympanic membrane displacements are clinically suitable indirect techniques which can detect changes in intra-labyrinthine pressure in humans 26 - 29. In 1973, Macrae observed an increasing in the input acoustic impedance of the cochlea in 4 subjects with acoustic neuroma, hypothesizing that those findings could be due to the indirect effect of the tumour on osmotic pressure of cochlear fluids 30. The first clinical evidences of primitive inner ear pathologies influencing measurements of impedance at the eardrum date to 1975 when Hall and Hughes 31, and contemporaneously Lloyd 32, studied the inter-aural stato-acoustic difference in patients with Ménière's disease. In particular, the former authors studied subjects with fullness due to unilateral Ménière's disease, observing reduced values of ipsilesional peak compliance in almost 90% of cases 31 33. Even though disproven by another study 34, these findings permitted the authors to confirm the pathophysiologic hypothesis of increased mechanical pressure in the intra-labyrinthine fluids as the basis of Ménière's disease, resulting in a stiffer system and in measurable reduced tympanometric values 33. Further studies have used impedance audiometry to detect changes in the stiffness of the middle-inner ear conduction system in patients with idiopathic or drug-induced endolymphatic hydrops 35 36. Similarly, by comparing the between-ear difference of maximum compliance at the eardrum, Goode found decreased conductance values on the involved side using a 660 Hz probe-tone tympanometer in 6 patients in which unilateral idiopathic perilymphatic hypertension was suspected 37.
Standard and multifrequency tympanometry has also been used to assess the inner ear mechanical effect on impedance in another pathological "third window" condition of the labyrinth: large vestibular aqueduct syndrome (LVAS). In particular, decreased stato-acoustic compliances were found in those patients with fluctuating hearing loss indicating increased inner ear pressure, while low resonance frequency values were found in patients with stable hearing function probably reflecting an increase in endolymphatic volume and reduced inner ear impedance due to the LVA acting as a "third window" 38 39. The only experimental study assessing SSCD-induced changes in impedance has been conducted on chinchillas with a surgically performed canal fenestration 22. Even if a statistically
significant increase in input admittance magnitude was seen, the authors did not use tympanometry to diagnose SSCD because of the small amplitude of impedancemetric changes induced by the dehiscence, and thus the likelihood for them to fall within normal ranges of values, being therefore not possible comparisons with normal ears 22. In regard to this latter difficulty, several aspects must be clarified to overcome these limits. Indeed, under physiological conditions, though it is reasonable to assume that the mobility of the tympano-ossicular system depends mainly on tympanic membrane status 40, there are several inter-individual variables that play a role in static impedance measurements, maintaining stable the probe-tone frequency. Irrespective of the variance due to age and sex of patients, being questionable the evidence whether it might be statistically significant 16 18 41 - 44, further anatomical variables such as external acoustic canal volume 41 45, size and state of the air in the middle ear and mastoid spaces, mobility of the ossicular chain 16 23 and finally input impedance to the cochlear fluids 20 24 can all influence impedance measurements at the tympanic membrane. Due to these factors, the amplitude of normality ranges of compliance and the degree of overlap between measurements of healthy and pathological ears are so considerable that any attempt to compare tympanometric data among subjects would be inappropriate. Nevertheless, since both external and middle ear structures within any individual would be expected to be highly similar due to general body symmetry, as demonstrated by Feldman's findings 15, the range of data should decrease when examining the behaviour of the tympano-ossicular system in the same subject 15 40 41 43 46. Moller firstly noted in 6 healthy individuals that the inter-aural differences in static admittance were smaller than the inter-subject range 47. Consistent with this line of reasoning, there are additional clinical findings in which no significant difference in impedancemetric measurements within the same normal subject was seen, making it a potentially feasible data to detect unilateral pathologies 40 43 44 47 48. In particular, according to de Jonge and Valente, 80% of healthy subjects develop differences in static acoustic values (ΔC) that do not exceed 0.22 ml 48. Another retrospective clinical review found a mean inter-aural difference of 0.14 ml, with 90% of the population within the values of 0.34 ml, but with significant dispersion as a function of age 44.
Ear asymmetry would thus seem to be more precisely quantified in terms of the ratio of compliance between the less stiff ear and the stiffer ear (Ca/Cb). According to the literature, normal values of between-ear ratio of compliance should range within 4/3 (= 1.33) 41 and 3/2 (= 1.5) 44 46, narrowing the 2/1 score (= 2) firstly proposed by Jerger 16. In the current study, we considered a minimal inter-aural difference (ΔC) of 0.22 ml and a minimal asymmetry ratio (ΔC%) of 14% (approximately equivalent to a ratio (Ca/ Cb) of 1.33 as demonstrated by the following equations) as sufficient to express a non-physiologic asymmetry of peak compliance, aiming to find SSCD-induced increased admittance measurements.
This correlation was determined once patients were stratified as a function of ΔC ≥ 0.22 ml and ΔC% ≥ 14% in favour of the pathological side, and then divided into two groups according to different amplitudes of mean mildlow frequencies ABG on the affected ear (≤ 20 dB nHL and > 20 dB nHL), in order to assess the role of impedancemetric differences as a function of hearing level. While between-ear differences of peak compliance (ΔC) do not seem to support any statistically significant outcome, the results provided evidence that patients with an ABG > 20 dB nHL on the dehiscent side tend to develop relevant asymmetry ratios (ΔC% ≥ 14%) in favour of the same side. In other words, acoustic compliance seems to be higher in those ears in which the considerable amplitude of conductive hearing loss would address clinicians to hypothesize a stiffening factor in the entire system, such as otosclerosis. Since the pathological asymmetry ratio in impedancemetric values points towards that ear as the most compliant, the otherwise unexplained mildlow frequencies ABG will unequivocally result from the improvement of the cochlear sensitivity to bone conduction and the acoustic energy dissipation through the dehiscence acting as a "third mobile window". Thus, even tympanometric asymmetry itself is likely to result from the same SSCD-induced increased compliance to the inner ear that is tested through the air-conducted VEMPs study. Definitive proof that the enhanced compliance measurements in these patients are the result of the dehiscence at the bony capsule of the vestibule will require ipsilesional lowering in tympanometric peak compliance after surgical canal repair, similar to postoperative closure of the ABG 3 49 and normalization of VEMPs amplitudes and thresholds 50 reported in literature.
Interpreting ear differences in this fashion enhances the power of stato-acoustic compliance as a diagnostic tool in evaluating unilateral inner ear pathologies, when combined with an audiometric test. We therefore recommend inclusion of acoustic impedance assessment and estimation of inter-aural asymmetry ratio in tympanometric peak compliance as a part of the diagnostic work-up before middle ear exploration in patients with a functionally and anatomically normal middle ear and unilateral unexplained conductive hearing loss. In particular, the importance of detecting bone-conduction threshold in pure tone audiometry should be stressed, in order to reveal an otherwise missed conductive or pseudo-conductive hearing loss. In the presence of an ABG, if acoustic reflexes and air-conducted c-VEMPs are preserved, then the patient must undergo HRCT scans of the temporal bones to assess the integrity of labyrinthine bony structures. Similarly, even the presence of an higher than normal asymmetry ratio in tympanometric peak compliance in favour of the "suspected" ear, when occurring a wide ABG amplitude on that side, should remind the clinician and orient diagnosis towards an inner ear pathology. Moreover, of the various instrumental tests described in the literature as useful diagnostic tools for SSCD, tympanometric testing is perhaps the most widely available and also relatively simple to perform. The only limit in the application of the test, although non-invasive, well tolerated, cheap and easily repeatable, is the necessity that the external/middle ear and ossicular chain are not involved in any pathology, other than the unilaterality of the inner ear lesion.
Conclusions
This report describes a new sign of unilateral dehiscence of the superior semicircular canal and evaluates its usefulness in diagnostic course: namely, pathological asymmetry in tympanometric peak compliance in favour of the involved ear in the presence of an important mild-low frequencies conductive hearing loss on the same side. This clinical finding gives a clue to intra-labyrinthine disease when middle ear status appears normal by otoscopy as well as the reminder of the impedancemetric battery. To date, this is the only clinical study reporting that tympanometric measurements are a useful tool in the diagnostic work-up of superior canal dehiscence syndrome. Therefore, when "evocative" symptoms of SSCD associated with an important ABG occur, inter-aural difference of tympanometric peak compliance at the eardrum in favour of the "suspected" side could suggest an intra-labyrinthine origin for this asymmetry. Tympanometry would thus prove to be a useful instrument in clinical-instrumental diagnosis of dehiscence pathology since it can detect, as well as cervical VEMPs (with threshold analysis), those cases associated with alterations of inner ear impedance. Nonetheless, it is still unknown why conductive hearing loss is present only in a subset of patients affected by SSCD, as long as the vestibular myogenic potentials threshold is lowered not in all subjects with clear radiological evidence of dehiscence at the SSC. Similarly, in this report, the explanation why not all patients from the study group presenting with considerable ABG develop pathological asymmetry in stato-acoustic measurements in favour of the involved side remains unclear. It is possible that, in addition to subclinical alterations in middle ear structures and state, it must be hypothesized that other intra-labyrinthine variables, such as the patency of the superior canal rather than natural plugging of dehiscence by middle fossa structures, can influence the impedance in the inner ear, resulting in different clinical and instrumental expression of the syndrome. A larger number of patients would provide more insight in this regard, which will be the subject of a future study, by comparing clinical and instrumental findings with different anatomo-morphological data. Another forthcoming objective will be to compare the results of the present study with the values of c-VEMPs thresholds in unilateral SSCD-patients, in order to determine if there is concordance between tympanometric and electrophysiological findings, as both instrumental tests are suitable for detecting inner ear admittance.
References
- 1.Minor LB, Solomon D, Zinreich JS, et al. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol Head Neck Surg. 1998;124:249–258. doi: 10.1001/archotol.124.3.249. [DOI] [PubMed] [Google Scholar]
- 2.Minor LB. Superior canal dehiscence syndrome. Am J Otol. 2000;21:9–19. [PubMed] [Google Scholar]
- 3.Minor LB, Carey JP, Cremer P, et al. Dehiscence of bone overlying the superior canal as a cause of apparent conductive hearing loss. Otol Neurotol. 2003;24:270–278. doi: 10.1097/00129492-200303000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Rosowski JJ, Songer JE, Nakajima HH, et al. Clinical, experimental and theoretical investigations of the effect of superior semicircular canal dehiscence on hearing mechanisms. Otol Neurotol. 2004;25:323–332. doi: 10.1097/00129492-200405000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Merchant SN, Rosowski JJ. Conductive hearing loss caused by third-window lesions of the inner ear. Otol Neurotol. 2008;29:282–289. doi: 10.1097/mao.0b013e318161ab24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belden CJ, Weg N, Minor LB, et al. CT evaluation of bone dehiscence of the superior semicircular canal as a cause of sound- and/or pressure-induced vertigo. Radiology. 2003;226:337–343. doi: 10.1148/radiol.2262010897. [DOI] [PubMed] [Google Scholar]
- 7.Colebatch JG, Halmagyi GM, Skuse NF. Myogenic potentials generated by a click-evoked vestibulocollic reflex. J Neurol Neurosurg Psychiatry. 1994;57:190–197. doi: 10.1136/jnnp.57.2.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brantberg K, Bergenius J, Tribukait A. Vestibular-evoked myogenic potentials in patients with dehiscence of the superior semicircular canal. Acta Otolaryngol. 1999;119:633–640. doi: 10.1080/00016489950180559. [DOI] [PubMed] [Google Scholar]
- 9.Rosengren SM, Aw ST, Halmagyi GM, et al. Ocular vestibular evoked myogenic potentials in superior canal dehiscence. J Neurol Neurosurg Psychiatry. 2008;79:559–568. doi: 10.1136/jnnp.2007.126730. [DOI] [PubMed] [Google Scholar]
- 10.Manzari L, Burgess AM, Curthoys IS. Effect of bone-conducted vibration of the midline forehead (Fz) in unilateral vestibular loss (uVL). Evidence for a new indicator of unilateral otolithic function. Acta Otorhinolaryngol Ital. 2010;30:175–181. [PMC free article] [PubMed] [Google Scholar]
- 11.Glorig A, Davis H. Age, noise and hearing loss. Ann Otol Rhinol Laryngol. 1961;70:556–571. doi: 10.1177/000348946107000219. [DOI] [PubMed] [Google Scholar]
- 12.House JW, Sheehy JL, Antunez JC. Stapedectomy in children. Laryngoscope. 1980;90:1804–1809. doi: 10.1288/00005537-198011000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Bance M. When is a conductive hearing loss not a conductive hearing loss? Causes of a mismatch in air-bone threshold measurements or a "pseudoconductive" hearing loss. J Otolaryngol. 2004;33:135–138. doi: 10.2310/7070.2004.00135. [DOI] [PubMed] [Google Scholar]
- 14.Metz O. The acoustic impedance measured on normal and pathological ears. Acta Otolaryngol. 1946;(Suppl.):63–63. [Google Scholar]
- 15.Feldman AS. Acoustic impedance studies of the normal ear. J Speech Hear Res. 1967;10:165–176. doi: 10.1044/jshr.1002.165. [DOI] [PubMed] [Google Scholar]
- 16.Jerger J. Clinical experience with impedance audiometry. Arch Otolaryngol. 1970;92:311–324. doi: 10.1001/archotol.1970.04310040005002. [DOI] [PubMed] [Google Scholar]
- 17.Klockhoff I. Clinical use of ear impedance measurements. J Laryngol Otol. 1971;85:243–254. doi: 10.1017/s0022215100073382. [DOI] [PubMed] [Google Scholar]
- 18.Jerger J, Jerger S, Mauldin L. Studies in impedance audiometry i. normal and sensorineural ears. Arch Otolaryngol. 1972;96:513–523. doi: 10.1001/archotol.1972.00770090791004. [DOI] [PubMed] [Google Scholar]
- 19.Ranke OF, Keidel WD, Weschke H. Hearing with closure of the oval window. Z Laryng Rhinol Otol. 1952;31:467–475. [PubMed] [Google Scholar]
- 20.Tonndorf J, Tabor JR. Closure of the cochlear windows: its effect upon air- and bone-conduction. Ann Otol Rhinol Laryngol. 1962;71:5–29. doi: 10.1177/000348946207100101. [DOI] [PubMed] [Google Scholar]
- 21.Bess FH, Miller GW, Glasscock ME, et al. Unexplained conductive hearing loss. South Med J. 1980;73:335–338. doi: 10.1097/00007611-198003000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Songer JE, Rosowski JJ. The effect of superior-canal opening on middle-ear input admittance and air-conducted stapes velocity in chinchilla. J Acoust Soc Am. 2006;120:258–269. doi: 10.1121/1.2204356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jerger J, Anthony L, Jerger S, et al. Studies in impedance audiometry III. Middle ear disorders. Arch Otolaryngol. 1974;99:165–171. doi: 10.1001/archotol.1974.00780030173003. [DOI] [PubMed] [Google Scholar]
- 24.Zwislocki J. Analysis of the middle-ear function. Part I: input impedance. Acoust Soc Am. 1962;34:1514–1523. [Google Scholar]
- 25.Macrae JH, Bulteau VG. Cochlear effects in tympanometry. J Aud Res. 1976;16:102–113. [Google Scholar]
- 26.Klockhoff I, Anggård G, Anggård L. Recording of craniolabyrinthine pressure transmission in man by acoustic impedance method. Acta Otolaryngol. 1966;61:361–370. [PubMed] [Google Scholar]
- 27.Magnano M, Albera R, Lerda W, et al. Evaluation of the cochlear aqueduct patency comparison of two non-invasive techniques. Acta Otorhinolaryngol Ital. 1997;17:403–408. [PubMed] [Google Scholar]
- 28.Macrae JH. Effects of body position on the auditory system. J Speech Hear Res. 1972;15:330–339. doi: 10.1044/jshr.1502.330. [DOI] [PubMed] [Google Scholar]
- 29.Casselbrant M. Indirect determination of variations in the inner ear pressure in man. An experimental study. Acta Otolaryngol Suppl. 1979;362:3–57. [PubMed] [Google Scholar]
- 30.Macrae JH. Acoustic neuromas and the acoustic impedance of the ear. J Speech Hear Disord. 1973;38:345–353. doi: 10.1044/jshd.3803.345. [DOI] [PubMed] [Google Scholar]
- 31.Hall M, Hughes R. Maximum compliance and the symptom of fullness in Meniere Disease. Arch Otolaryngol. 1975;101:227–231. doi: 10.1001/archotol.1975.00780330023005. [DOI] [PubMed] [Google Scholar]
- 32.Lloyd L. Impedance measurements in the diagnosis of Meniere's disease. J S Afr Speech Hear Assoc. 1975;1975:49–62. [PubMed] [Google Scholar]
- 33.Hall M. Maximum compliance and Ménière's disease. Laryngoscope. 1978;88:1512–1517. doi: 10.1002/lary.1978.88.9.1512. [DOI] [PubMed] [Google Scholar]
- 34.Herman LE, Carver WF, Arenberg IK. Static compliance of the eardrum in Meniere Disease. Arch Otolaryngol. 1977;103:84–86. doi: 10.1001/archotol.1977.00780190064005. [DOI] [PubMed] [Google Scholar]
- 35.Bianchedi M, Croce A, Neri G, et al. Multifrequency tympanometry in Meniere's disease: preliminary results. Acta Otorhinolaryngol Ital. 1996;16:1–5. [PubMed] [Google Scholar]
- 36.Abramo A, Benfari G, Marullo T. Positional impedance tests with acetazolamide: a clinical test for evaluating endolymphatic hydrops. Acta Otorhinolaryngol Ital. 1996;16:401–406. [PubMed] [Google Scholar]
- 37.Goode RL. Perilymph hypertension and the indirect measurement of cochlear pressure. Laryngoscope. 1981;91:1706–1713. doi: 10.1288/00005537-198110000-00017. [DOI] [PubMed] [Google Scholar]
- 38.Bilgen C, Kirkim G, Kirazli T. Middle ear impedance measurements in large vestibular aqueduct syndrome. Auris Nasus Larynx. 2009;36:263–268. doi: 10.1016/j.anl.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 39.Sato E, Nakashima T, Lilly DJ, et al. Tympanometric findings in patients with enlarged vestibular aqueducts. Laryngoscope. 2002;112:1642–1646. doi: 10.1097/00005537-200209000-00021. [DOI] [PubMed] [Google Scholar]
- 40.Feldman AS. Eardrum abnormality and the measurement of middle ear function. Arch Otolaryngol. 1974;99:211–217. doi: 10.1001/archotol.1974.00780030219013. [DOI] [PubMed] [Google Scholar]
- 41.Brooks DN. Tympanometry: between ear symmetry and normative values. J Am Aud Soc. 1979;5:112–117. [PubMed] [Google Scholar]
- 42.Hall JW, Weaver T. Impedance audiometry in a young population. The effect of age, sex, and tympanogram abnormalities. J Otolaryngol. 1979;8:210–222. [PubMed] [Google Scholar]
- 43.Osterhammel D, Osterhammel P. Age and sex variations for the normal stapedial reflex thresholds and tympanometric compliance values. Scand Audiol. 1979;8:153–158. doi: 10.3109/01050397909076316. [DOI] [PubMed] [Google Scholar]
- 44.Mallardi V, D'Auria E, Frogheri G. Static compliance of the normal ear: study of the interaural differences and ratios. Acta Otorhinolaryngol Ital. 1985;5(Suppl. 5):3–21. 9. [PubMed] [Google Scholar]
- 45.Shanks JE, Lilly DJ. An evaluation of tympanometric estimates of ear canal volume. J Speech Hear Res. 1981;24:557–566. doi: 10.1044/jshr.2404.557. [DOI] [PubMed] [Google Scholar]
- 46.Wilson RH, Shanks JE, Velde TM. Aural acoustic-immittance measurements: inter-aural differences. J Speech Hear Disord. 1981;46:413–421. doi: 10.1044/jshd.4604.413. [DOI] [PubMed] [Google Scholar]
- 47.Moller A. Improved technique for detailed measurements of the middle ear impedance. J Acoust Soc Am. 1960;32:250–257. [Google Scholar]
- 48.Jonge RR, Valente M. Interpreting ear differences in static compliance measurements. J Speech Hear Disord. 1979;44:209–213. doi: 10.1044/jshd.4402.209. [DOI] [PubMed] [Google Scholar]
- 49.Limb CJ, Carey JP, Srireddy S, et al. Auditory function in patients with surgically treated superior semicircular canal dehiscence. Otol Neurotol. 2006;27:969–980. doi: 10.1097/01.mao.0000235376.70492.8e. [DOI] [PubMed] [Google Scholar]
- 50.Brantberg K, Bergenius J, Mendel L, et al. Symptoms, findings and treatment in patients with dehiscence of the superior semicircular canal. Acta Otolaryngol. 2001;121:68–75. doi: 10.1080/000164801300006308. [DOI] [PubMed] [Google Scholar]