SUMMARY
Schwannomas are benign, encapsulated, slow-growing and usually solitary tumours originating from Schwann cells of the peripheral nerve sheath. Approximately 25-40% of cases are seen in the head and neck region, of which 1% in the oral cavity. We report a rare case of lingual schwannoma in a young woman who was treated with complete transoral excision, and also review the literature of the past two decades, analyzing epidemiological and clinical data of the 35 cases reported. Lingual schwannomas generally present as a painless lump with an average size of 2 cm in the fourth decade of life and with no gender predilection. Complete transoral excision can be considered standard treatment for these tumours, with no recurrences documented in the literature.
KEY WORDS: Oral schwannoma, Head and neck schwannoma, Oral tumour
RIASSUNTO
Gli schwannomi sono tumori benigni solitari, incapsulati e a lenta crescita che originano dalle cellule di Schwann presenti nella guaina dei nervi periferici. Circa il 25-40% dei casi sono osservati nella regione testa-collo, di cui l'1% nella cavità orale. Gli schwannomi linguali si presentano generalmente nella quarta decade di vita, senza predilezione di genere, come nodulo solitario e indolore con dimensione media di circa 2 cm. Il trattamento d'elezione riportato in letteratura è l'asportazione chirurgica, infatti, l'escissione transorale di questo tipo di lesione è radicale e non si documentano casi di recidiva locale. Presentiamo un caso raro di schwannoma linguale in una giovane donna trattata chirurgicamente con completa asportazione trans-orale della lesione e revisione completa della letteratura degli ultimi 20 anni che riporta un totale di 35 casi.
Introduction
Schwannoma or neurilemmoma is a rare, benign neurogenic neoplasm composed of Schwann cells (nerve sheath). It is usually slow growing, solitary, well demarcated and encapsulated 1 2. Approximately 25-40% of all cases involve the head and neck, of which 1% are located in the oral cavity 3. They originate more frequently from sensory nerves and can affect all cranial nerves, except the olfactory and optic, which are extensions of white matter from the brain 5. In the tongue, the distinction between hypoglossal, glossopharyngeal or lingual nerve origin is difficult, given their proximity. These tumours usually appear between the second and fourth decade of life, with no predilection for gender or race 5. The size and locations of lesions determine the presence and intensity of symptoms. The goal of treatment is complete excision, which results in low rates of recurrence 6. Here, we present an unusual case of lingual schwannoma and review the English language literature.
A search of the terms "lingual schwannoma", "tongue schwannoma", lingual neurilemmoma" and "tongue neurilemmoma" was performed using PubMed. Only literature in English and published from 1990 to 2010 was included. Cases without complete information and cases of localization on the palate, buccal mucosa or vestibule were excluded.
Data on gender, age, size, location, clinical presentation, type of treatment and follow-up were extracted from the original reports (Table I).
Table I.
Demographics and treatment characteristics of 36 cases with lingual schwannoma reported in the literature.
| Sex | Age (years) |
Size (cm) |
Site | Presentation | Surgical approach | Follow-up (months) |
|
|---|---|---|---|---|---|---|---|
| Karaca et al., 2010 7 | F | 13 | 2.0 | Oral tongue | Dysphagia | Transoral | 12 |
| Gupta et al., 2009 8 | F | 18 | 1.0 | Oral tongue | Lump | Transoral | |
| Cohen et al., 2009 6 | F | 19 | 1.8 | Oral tongue | Lump | Transoral | |
| M | 77 | 0.7 | Oral tongue | Lump | Transoral | ||
| Pereira et al., 2009 9 | M | 12 | 1.5 | Oral tongue | Lump | Transoral | 12 |
| Ferreti Bonan et al., 2008 10 | F | 46 | Oral tongue | Lump | Transoral | 12 | |
| Sawhney et al., 2008 5 | F | 37 | 4.6 | Tongue base | Dysphagia/snoring | Submandibular | |
| Batra et al., 2007 11 | M | 30 | 3.0 | Tongue base | Abscess | Transoral | 9 |
| M | 33 | 3.0 | Tongue base | Dysphonia | Transoral | 6 | |
| Enoz et al., 2006 3 | M | 7 | 2.5 | Oral tongue | Lump | Transoral | 60 |
| Ballesteros et al., 2007 12 | F | 31 | 2.0 | Tongue base | Local pain | CO2 - transoral | |
| Patnayak et al., 2007 13 | F | 45 | 2.0 | Oral tongue | Lump | transoral | |
| Mehzrad et al., 2006 14 | M | 49 | 2.2 | Tongue base | Local pain | CO2 - transoral | 3 |
| Hsu et al., 2006 15 | F | 39 | 1.0 | Oral tongue | Lump | Transoral | 137 |
| F | 39 | 4.0 | Tongue base | Dysphagia | Transhyoid | 23 | |
| M | 9 | 1.2 | Oral tongue | Lump | Transoral | 56 | |
| F | 32 | 1.8 | Tongue base | Lump | Transoral | 63 | |
| M | 25 | 0.9 | Oral tongue | Lump | Transoral | 28 | |
| F | 15 | 1.2 | Oral tongue | Lump | Transoral | 136 | |
| M | 38 | 3.0 | Oral tongue | Lump | Transoral | 135 | |
| F | 12 | 1.6 | Oral tongue | Lump | Transoral | 13 | |
| M | 45 | 0.5 | Oral tongue | Lump | Transoral | 203 | |
| M | 20 | 5.0 | Tongue base | Bleeding | Transoral | 3 | |
| Ying et al., 2006 4 | F | 26 | 4.0 | Tongue base | Dysphagia/otalgia | Transoral | |
| Vafiadis et al., 2005 16 | M | 18 | 3.1 | Oral tongue | Lump | Transoral | 36 |
| Hwang et al., 2005 17 | M | 23 | 2.8 | Oral tongue | Lump | Transoral | 6 |
| Nakasato et al., 2005 18 | F | 9 | 2.0 | Tongue base | Lump | Transoral | 17 |
| Cinar et al., 2004 19 | M | 7 | 1.0 | Oral tongue | Lump | Transoral | |
| Bassichis et al., 2004 20 | M | 9 | 2.3 | Tongue base | Snore | Transoral | 60 |
| Mevio et al., 2002 21 | F | 35 | 5.0 | Oral tongue | Lump | Transoral | |
| Pfeifle et al., 2001 22 | F | 30 | 0.3 | Oral tongue | Lump | Transoral | |
| M | 18 | 2.0 | Oral tongue | Lump | Transoral | ||
| de Bree et al., 2000 23 | F | 24 | Tongue base | Lump | Submandibular | ||
| Lopez et al., 1993 24 | M | 33 | 1.2 | Oral tongue | Lump | Transoral | |
| M | 24 | 0.6 | Oral tongue | Lump | Transoral |
Case report
A 26-year-old woman was referred to our department to investigate a lingual nodule found by MRI (Fig. 1) during investigation of chronic cervical pain. The patient reported paresthesias in the left half of the tongue lasting two years, which was related to a dental extraction. The patient was a non-smoker and had no significant personal or familial medical history.
Fig. 1.
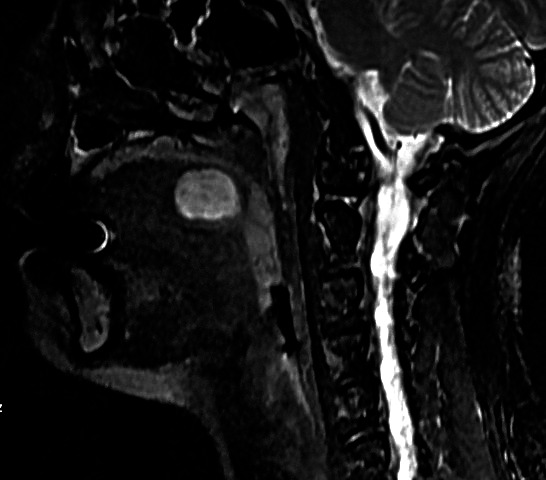
Parasagital T2-weighted MRI showing a well-delimited nodule with a heterogeneous high signal.
Clinical examination revealed a nodule 2.5 cm in size, elastic, tender, smooth, at left side of midline, in the transition between the oral tongue and base of the tongue, covered by normal mucosa (Fig. 2). Cervical lymph nodes were not identified. The remaining physical examination was unremarkable. After discussing options with the patient, we proposed transoral excision.
Fig. 2.

Gross examination of the excised tumour showing a 2.5 × 2.0 cm capsulated, smooth and tender nodule.
The procedure and postoperative period were uneventful, with good functional results. The patient received a liquid diet and was discharged on the first postoperative day. Histopathological examination of the surgical specimen revealed a schwannoma, mainly composed of a Antoni A pattern with Verocay bodies (Fig. 3). Immunohistochemistry showed positive staining for S-100 protein, confirming the diagnosis of schwannoma. (Fig. 4).
Fig. 3.
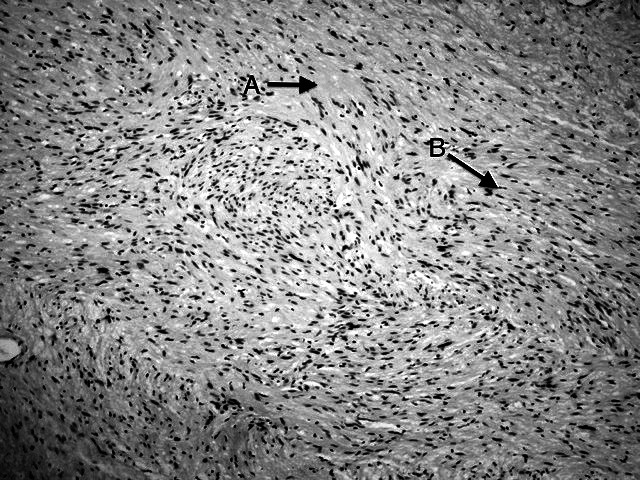
Verocay bodies (A) between palisading nuclei (B) of an Antoni A area.
Fig. 4.
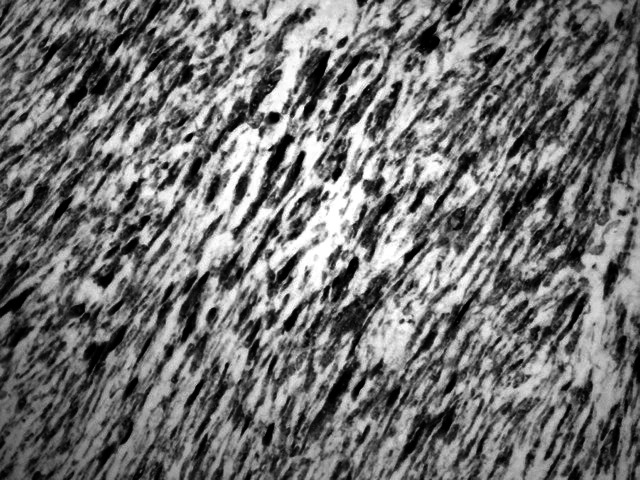
Immunohistochemistry showing positive staining for S-100 protein.
Discussion
We identified 35 reported cases of lingual schwannoma through a search in PubMed. Including the case reported here, 36 patients with a diagnosis of lingual schwannoma have been reported (Table I). The mean age at diagnosis was 27 years. The age groups most affected were the 2nd, 3rd and 4th decades of life (22.2, 19.4 and 30.5% respectively). There was no predisposition for gender (18 men and 18 women). Two-thirds (24 cases) of tumours arose in the oral tongue with the remaining one-third affecting the tongue base. Lingual nodule without associated symptoms was the clinical presentation in 26 cases. Sore throat was the first symptom in two cases and dysphagia in 4 cases, 2 of which were associated with otalgia and sleep apnoea. Bleeding, local infection, dysphonia and sleep apnoea were the initial presentation in one patient each. All tumours that showed symptoms were located at the base of the tongue, where only three patients (25%) were asymptomatic. Of the tumours located in the oral tongue, only one was associated with symptoms (dysphagia) (2.7%). The mean size of tumours was 2 cm (1.7 cm when located in the oral tongue and 2.8 cm at the base of the tongue). Standard treatment was transoral excision, performed in 86% of 36 cases. However, for tumours located at the base of the tongue, in 2 cases CO2 laser was used, and in three other cases, the approach was transcervical (two submandibular and one transhyoid). All tumours in the oral tongue were treated with simple transoral excision. All cases had histopathologically- confirmed diagnosis as schwannoma. Only 14% of cases had no immunohistochemistry with the protein S-100 for diagnostic confirmation. There were no reports of recurrence.
Because of their rarity 24, schwannomas are not generally part of the differential diagnosis of oral cavity lesions. Although the tongue is one of the most common tumour locations in the mouth, only 36 cases of lingual schwannoma have been reported in the English literature in the last 20 years (Table I).
Lingual schwannoma can affect all age groups, being most commonly found between 10 and 40 years of age, without gender predisposition. In this site, they usually appear as slow-growing, progressive nodules, showing with symptoms that, when present, vary according to their size and location. In the tongue, two-thirds of cases involve the oral portion, and about one-third involve the base. The most common clinical presentation is a painless submucosal nodule with an average size of 2 cm. However, when in the base of the tongue, these tumours cause symptoms such as sore throat, dysphagia, sleep apnoea, dysphonia, bleeding, infection and pain in about 75% of cases.
The risk of malignant transformation of head and neck schwannoma varies from 8 to 10%3, and one case occurring in the tongue has been reported 25. The best imaging technique, especially in this location, is MRI, which should reveal a well-defined nodule with homogeneous hyperintense signal on T2-weighted and isointense to muscle on T1-weighted images 3. It is histopathologically characterized by a mixture of two patterns of tissue growth, namely type A and B Antoni. The first is densely composed of elongated schwann cells forming palisades. Type B has a myxoid, looser and disorganized arrangement. Between these cellular arrangements, there are Verocay bodies, which are acellular eosinophilic areas 4. Variations in this composition have no known clinical significance 5. The immunohistochemical markers S-100 and Leu 7, used in most cases, confirm the schwann-cell origin of these tumours and confirm diagnosis 15.
Standard treatment is complete surgical excision, and a transoral approach is the most widely used. However, for schwannomas located at the base of the tongue, cervical access (transhyoid or submandibular) or use of CO2 laser are feasible options. When complete excision is performed, recurrence has not been reported.
References
- 1.Waal I, Snow GB. Benign Tumors and Tumor-Like Lesions. In: Cummings CW, Frederickson JM, Harker LA, et al., editors. Head and Neck Surgery. St Louis: Mosby; 1998. pp. 1407–1417. [Google Scholar]
- 2.Neville BW, Damm DD, Allen C. Soft-Tissue Tumors. In: Neville BW, Damm DD, White DH, editors. Color Atlas of Clinical Oral Patrhology. Hamilton: BC Decker; 2003. pp. 275–312. [Google Scholar]
- 3.Enoz M, Suoglu Y, Ilhan R. Lingual schwannoma. J Cancer Res Ther. 2006;2:76–78. doi: 10.4103/0973-1482.25856. [DOI] [PubMed] [Google Scholar]
- 4.Ying YL, Zimmer LA, Myers EN. Base of tongue schwannoma: a case report. Laryngoscope. 2006;116:1284–1287. doi: 10.1097/01.mlg.0000224358.55022.8a. [DOI] [PubMed] [Google Scholar]
- 5.Sawhney R, Carron MA, Mathog RH. Tongue base schwannoma: report, review, and unique surgical approach. Am J Otolaryngol. 2008;29:119–122. doi: 10.1016/j.amjoto.2006.08.003. r. [DOI] [PubMed] [Google Scholar]
- 6.Cohen M, Wang MB. Schwannoma of the tongue: two case reports and review of the literature. Eur Arch Otorhinolaryngol. 2009;266:1823–1829. doi: 10.1007/s00405-008-0907-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karaca CT, Habesoglu TE, Naiboglu B, et al. Schwannoma of the tongue in a child. Am J Otolaryngol. 2010;31:46–48. doi: 10.1016/j.amjoto.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Gupta P, Garg A, Dhingra KK, et al. Schwannoma tongue: a rare entity. ANZ J Surg. 2009;79:93–94. doi: 10.1111/j.1445-2197.2008.04818.x. [DOI] [PubMed] [Google Scholar]
- 9.Pereira LJ, Pereira PP, dos Santos Jde P, et al. Lingual schwannoma involving the posterior lateral border of the tongue in a young individual: case report. J Clin Pediatr Dent. 2008;33:59–62. doi: 10.17796/jcpd.33.1.h131208u28306576. [DOI] [PubMed] [Google Scholar]
- 10.Ferreti Bonan PR, Martelli H, Jr, Nogueira Dos Santos LA, et al. Multinodular neurilemmoma of the tongue: a case report with differential immunohistochemical profile. Minerva Stomatol. 2008;57:71–75. [PubMed] [Google Scholar]
- 11.Batra K, Rai AK, Chaudhary N, et al. Two cases of neurilemmoma of the tongue. Ear Nose Throat J. 2007;86:679–681. [PubMed] [Google Scholar]
- 12.Ballesteros F, Vilaseca I, Blanch JL, et al. Base of tongue neurilemmoma: excision by transoral laser microsurgery. Acta Otolaryngol. 2007;127:1005–1007. doi: 10.1080/00016480601110261. [DOI] [PubMed] [Google Scholar]
- 13.Patnayak R, Anuradha SV, Uppin SM, et al. Schwannoma of tongue - a case report and short review of literature. Acta Oncol. 2007;2007:265–266. doi: 10.1080/02841860600897959. S. [DOI] [PubMed] [Google Scholar]
- 14.Mehrzad H, Persaud R, Papadimitriou N, et al. Schwannoma of tongue base treated with transoral carbon dioxide laser. Lasers Med Sci. 2006;21:235–237. doi: 10.1007/s10103-006-0402-1. [DOI] [PubMed] [Google Scholar]
- 15.Hsu YC, Hwang CF, Hsu RF, et al. Schwannoma (neurilemmoma) of the tongue. Acta Otolaryngol. 2006;126:861–865. doi: 10.1080/00016480500527219. [DOI] [PubMed] [Google Scholar]
- 16.Vafiadis M, Fiska A, Panopoulou M, et al. A clinical case report of a Schwannoma of the tipo f the tongue. B-ENT. 2005;1:201–204. [PubMed] [Google Scholar]
- 17.Hwang K, Kim SG, Ahn SI, et al. Neurilemmoma of the tongue. J Craniofac Surg. 2005;16:859–861. doi: 10.1097/01.scs.0000164333.81428.f3. [DOI] [PubMed] [Google Scholar]
- 18.Nakasato T, Kamada Y, Ehara S, et al. Multilobular neurilemmoma of the tongue in a child. AJNR Am J Neuroradiol. 2005;26:421–423. [PMC free article] [PubMed] [Google Scholar]
- 19.Cinar F, Cinar S, Harman G. Schwannoma of the tip of the tongue in a child. Plast Reconstr Surg. 2004;114:1657–1658. [PubMed] [Google Scholar]
- 20.Bassichis BA, McClay JE, et al. Pedunculated neurilemmoma of the tongue base. Otolaryngol Head Neck Surg. 2004;130:639–641. doi: 10.1016/j.otohns.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 21.Mevio E, Gorini E, Lenzi A, et al. Schwannoma of the tongue: one case report. Rev Laryngol Otol Rhinol (Bord) 2002;123:259–261. [PubMed] [Google Scholar]
- 22.Pfeifle R, Baur DA, Paulino A, et al. Schwannoma of the tongue: report of 2 cases. J Oral Maxillofac Surg. 2001;59:802–804. doi: 10.1053/joms.2001.24298. [DOI] [PubMed] [Google Scholar]
- 23.Bree R, Westerveld GJ, Smeele LE. Submandibular approach for excision of a large schwannoma in the base of the tongue. Eur Arch Otorhinolaryngol. 2000;257:283–286. doi: 10.1007/s004050050241. [DOI] [PubMed] [Google Scholar]
- 24.López JI, Ballestin C. Intraoral schwannoma. A clinicopathologic and immunohistochemical study of nine cases. Arch Anat Cytol Pathol. 1993;41:18–23. [PubMed] [Google Scholar]
- 25.Piatelli A, Angelone A, Pizzicannella G, et al. Malignant schwannoma of the tongue. Report of a case and review of the literature. Acta Stomatol Belg. 1984;81:213–225. [PubMed] [Google Scholar]


