Abstract
A poor nutritional state and a caloric deficit associate with increased morbidity and mortality, but a recent multicenter, randomized controlled trial found that early parenteral nutrition to supplement insufficient enteral nutrition increases morbidity in the intensive care unit, including prolonging the duration of renal replacement therapy, compared with withholding parenteral nutrition for 1 week. Whether early versus late parenteral nutrition impacts the incidence and recovery of AKI is unknown. Here, we report a prespecified analysis from this trial, the Early Parenteral Nutrition Completing Enteral Nutrition in Adult Critically Ill Patients (EPaNIC) study. The timing of parenteral nutrition did not affect the incidence of AKI, but early initiation seemed to slow renal recovery in patients with stage 2 AKI. Early parenteral nutrition did not affect the time course of creatinine and creatinine clearance but did increase plasma urea, urea/creatinine ratio, and nitrogen excretion beginning on the first day of amino acid infusion. In the group that received late parenteral nutrition, infusing amino acids after the first week also increased ureagenesis. During the first 2 weeks, ureagenesis resulted in net waste of 63% of the extra nitrogen intake from early parenteral nutrition. In conclusion, early parenteral nutrition does not seem to impact AKI incidence, although it may delay recovery in patients with stage 2 AKI. Substantial catabolism of the extra amino acids, which leads to higher levels of plasma urea, might explain the prolonged duration of renal replacement therapy observed with early parenteral nutrition.
The development of AKI is a frequent and devastating condition in patients admitted to the intensive care unit (ICU). Short-term mortality is high and increases with worsening AKI stages.1 In AKI survivors, renal recovery is often incomplete, progression to ESRD may be accelerated, and longer-term mortality rates are increased compared with non-AKI patients.2,3 Patient management consists of maximal prevention of additional renal damage by hemodynamic stabilization and prevention of (iatrogenic) nephrotoxicity. A curative strategy for established AKI is currently unavailable.4
Observational studies, finding associations between a poor nutritional state and increased morbidity and mortality of AKI patients5 and between accumulation of a caloric deficit and poor renal and survival outcome of ICU patients,6,7 have led to the hypothesis that feeding could ameliorate kidney injury and improve survival of ICU patients. However, nutrition, especially parenteral nutrition (PN), also has potential complications.8–11 Because of the lack of adequately designed studies, nutritional guidelines are largely based on expert opinion.12–14 These opinions invariably recommend the early initiation of enteral feeding but substantially differ in their recommendation on when to start supplemental PN.
The Early Parenteral Nutrition Completing Enteral Nutrition in Adult Critically Ill Patients (EPaNIC) study was the first large, multicenter, randomized controlled trial (RCT) addressing this important question. The study showed that early initiation of PN increased dependency on intensive care compared with withholding supplemental PN for 1 week (hereafter labeled early PN and late PN, respectively).15 Indeed, early PN prolonged the ICU and hospital length of stay (LOS), increased the incidence of new infections, and prolonged the need for mechanical ventilation. Renal harm was suggested by a clear prolongation of the duration of renal replacement therapy (RRT) in ICU and a trend for more AKI (defined as a doubling or more of ICU admission plasma creatinine). However, the number of patients requiring RRT was unaltered, and recovery to premorbid kidney function was not investigated.
It was preplanned to study the detailed impact of early versus late PN on the incidence and recovery of AKI and the time course of blood/urine markers of renal function during ICU stay.16 A priori, we hypothesized that early PN would attenuate kidney injury. However, the original study findings suggested that AKI incidence and renal recovery could be aggravated by increased macronutrient provision in the acute phase of critical illness.
Results
Baseline characteristics of the 4640 patients are shown in Table 1.
Table 1.
Baseline characteristics of the patients
| Parameter | Early PN (n=2312) | Late PN (n=2328) | P |
|---|---|---|---|
| Age (mean ± SD) | 64±14 | 64±15 | 0.54 |
| Men, n (%) | 1486 (64.3) | 1486 (63.8) | 0.75 |
| Body mass index categories, n (%) | 0.34 | ||
| <20 | 134 (5.8) | 141 (6.1) | |
| 20 to <25 | 854 (36.9) | 890 (38.2) | |
| 25 to <30 | 852 (36.9) | 864 (37.1) | |
| 30 to <40 | 430 (18.6) | 405 (17.4) | |
| ≥40 | 42 (1.8) | 28 (1.2) | |
| Nutritional risk score categories, n (%) | 0.72 | ||
| 3 | 1014 (43.9) | 1050 (45.1) | |
| 4 | 851 (36.8) | 862 (37.0) | |
| 5 | 231 (10.0) | 207 (8.9) | |
| 6 | 178 (7.7) | 171 (7.4) | |
| 7 | 38 (1.6) | 38 (1.6) | |
| Diabetes mellitus, n (%) | 391 (16.9) | 417 (17.9) | 0.37 |
| History of malignancy, n (%) | 437 (18.9) | 457 (19.6) | 0.53 |
| Acute Physiology and Chronic Health Evaluation II on ICU admission (mean ± SD) | 23±11 | 23±10 | 0.86 |
| Emergency admission, n (%) | 956 (41.4) | 970 (41.7) | 0.83 |
| Sepsis on ICU admission, n (%) | 510 (22.1) | 505 (21.7) | 0.76 |
| Reason for ICU admission, n (%) | >0.99 | ||
| Cardiac surgery | 1410 (61.0) | 1408 (60.5) | |
| Complicated abdominal or pelvic surgery | 170 (7.4) | 178 (7.6) | |
| Transplantation | 165 (7.1) | 163 (7.0) | |
| Trauma, burns, or reconstructive surgery | 99 (4.3) | 107 (4.6) | |
| Complicated pulmonary or esophageal surgery | 86 (3.7) | 83 (3.6) | |
| Respiratory disease | 72 (3.1) | 71 (3.1) | |
| Complicated vascular surgery | 65 (2.8) | 69 (3.0) | |
| Complicated neurosurgery | 61 (2.6) | 54 (2.3) | |
| Gastroenterologic or hepatic disease | 55 (2.4) | 61 (2.6) | |
| Hematologic or oncological disease | 18 (0.8) | 16 (0.7) | |
| Neurologic disease | 14 (0.6) | 15 (0.6) | |
| Cardiovascular disease | 8 (0.4) | 10 (0.4) | |
| Renal disease | 8 (0.4) | 10 (0.4) | |
| Neurologic presentation of medical disease | 10 (0.3) | 7 (0.3) | |
| Metabolic disorder | 2 (0.1) | 4 (0.2) | |
| Other | 69 (3.0) | 72 (3.1) | |
| Dialysis-dependent kidney failure before ICU admission, n (%) | 34 (1.5) | 35 (1.5) | 0.93 |
| Minimum baseline creatinine (mg/dl; median [interquartile range]) | 0.92 (0.78–1.08) | 0.93 (0.78–1.09) | 0.76 |
| Minimum baseline estimated from Modification of Diet in Renal Disease formula, n (%) | 506 (21.9) | 557 (23.9) | 0.10 |
| Randomization baseline creatinine (mg/dl; median [interquartile range]) | 0.97 (0.79–1.25) | 0.97 (0.79–1.26) | 0.40 |
Incidence of AKI and Renal Recovery
Assessed relative to the last plasma creatinine before randomization (randomization baseline) or the estimated premorbid creatinine level (minimum baseline), 843 (18.4%) or 1133 (24.8%) patients, respectively, developed AKI. The intervention affected neither the incidence of AKI stages 1–3 nor the time frame of AKI development (Table 2).
Table 2.
Incidence of AKI
| AKI Stage | Early PN | Late PN | P |
|---|---|---|---|
| AKI (any) | |||
| Versus minimum baseline, n (%) | 568 (24.9) | 565 (24.6) | 0.82 |
| First-day AKI versus minimum baseline, median (IQR) | 1 (1–2) | 1 (1–2) | 0.74 |
| Versus randomization baseline, n (%) | 421 (18.5) | 422 (18.4) | 0.95 |
| First-day AKI versus randomization baseline, median (IQR) | 2 (1–3) | 2 (1–3) | 0.17 |
| AKI stage 1 | |||
| Versus minimum baseline, n (%) | 219 (9.6) | 197 (8.6) | 0.23 |
| First-day AKI versus minimum baseline, median (IQR) | 2 (1–3) | 1 (1–2) | 0.20 |
| Versus randomization baseline, n (%) | 142 (6.2) | 131 (5.7) | 0.46 |
| First-day AKI versus randomization baseline, median (IQR) | 2 (1–3) | 2 (1–4) | 0.58 |
| AKI stage 2 | |||
| Versus minimum baseline, n (%) | 99 (4.3) | 107 (4.7) | 0.60 |
| First-day AKI versus minimum baseline, median (IQR) | 1 (1–2) | 1 (1–2) | 0.30 |
| Versus randomization baseline, n (%) | 61 (2.7) | 73 (3.2) | 0.31 |
| First-day AKI versus randomization baseline, median (IQR) | 2 (1–4) | 2 (1–2) | 0.61 |
| AKI stage 3 | |||
| Versus minimum baseline, n (%) | 250 (11.0) | 261 (11.4) | 0.66 |
| First-day AKI versus minimum baseline, median (IQR) | 1 (1–2) | 1 (1–1) | 0.20 |
| Versus randomization baseline, n (%) | 218 (9.6) | 218 (9.5) | 0.94 |
| First-day AKI versus randomization baseline, median (IQR) | 2 (1–3) | 2 (1–3) | 0.23 |
The AKI stage represents the maximum AKI score during ICU stay. The first-day AKI corresponds to the first ICU day with AKI stage 1 or higher. IQR, interquartile range
In the total AKI population and stage 1 AKI, the in-ICU duration of AKI, ICU and hospital LOS, renal recovery at ICU and hospital discharge, and in-ICU, in-hospital, and 90-day mortality were unaffected by the intervention (Table 3 and Supplemental Table 1). In patients with stage 2 AKI, the in-ICU duration of AKI and the time to alive hospital discharge were significantly longer in the early PN group, but a similar number of patients were alive and AKI-free at hospital discharge. In patients with stage 3 AKI, ICU LOS was longer in the early PN group, without a difference in renal recovery parameters and mortality. In patients with new RRT (n=359, 7.7%), the number of patients who were deceased or still RRT-dependent at hospital discharge was unaffected (100 [54.9%] in the early versus 100 [56.5%] in the late PN group; P=0.77).
Table 3.
Recovery from AKI and outcome
| AKI Stage | Early PN | Late PN | P |
|---|---|---|---|
| AKI (any; n=1133) | |||
| AKI days in ICU in patients discharged alive from ICU, median (IQR; n=453 and 461 in early versus late PN) | 3 (1–10) | 4 (2–9) | 0.32 |
| ICU length of stay in patients discharged alive from ICU, median (IQR) | 10 (5–20) | 9 (4–19) | 0.09 |
| Discharged alive from hospital without AKI, n (%) | 317 (55.8) | 314 (55.6) | 0.94 |
| Hospital mortality, n (%) | 158 (27.8) | 153 (27.1) | 0.78 |
| AKI stage 1 (n=416) | |||
| AKI days in ICU in patients discharged alive from ICU, median (IQR; n=211 and 185 in early versus late PN) | 1 (1–2) | 2 (1–3) | 0.35 |
| ICU length of stay in patients discharged alive from ICU, median (IQR) | 6 (4–11) | 5 (3–10) | 0.07 |
| Discharged alive from hospital without AKI, n (%) | 168 (76.7) | 148 (75.1) | 0.71 |
| Hospital mortality, n (%) | 22 (10.0) | 30 (15.2) | 0.11 |
| AKI stage 2 (n=206) | |||
| AKI days in ICU in patients discharged alive from ICU, median (IQR; n=80 and 95 in early versus late PN) | 5 (3–9) | 4 (2–6) | 0.04 |
| ICU length of stay in patients discharged alive from ICU, median (IQR) | 10 (5–19) | 9 (4–17) | 0.41 |
| Discharged alive from hospital without AKI, n (%) | 63 (63.6) | 68 (63.6) | 0.99 |
| Hospital mortality, n (%) | 26 (26.3) | 18 (16.8) | 0.10 |
| AKI stage 3 (n=511) | |||
| AKI days in ICU in patients discharged alive from ICU, median (IQR; n=162 and 181 in early versus late PN) | 12 (7–21) | 11 (6–21) | 0.17 |
| ICU length of stay in patients discharged alive from ICU, median (IQR) | 18 (10–31) | 14 (7–27) | 0.04 |
| Discharged alive from hospital without AKI, n (%) | 86 (34.4) | 98 (37.5) | 0.46 |
| Hospital mortality, n (%) | 110 (44.0) | 105 (40.2) | 0.39 |
Recovery from AKI was assessed versus the minimum baseline. For every AKI stage, the presence of AKI at a particular time point was defined as meeting stage 1 or higher versus the minimum baseline. IQR, interquartile range.
In long-stay patients (ICU stay≥7 days), independent from randomization, AKI incidence and renal recovery at hospital discharge were comparable in different strata of cumulative caloric intake until day 7. In patients with stage 2 AKI, cumulative caloric intake until day 7 correlated with the number of in-ICU AKI days (ρ=0.273, P=0.006; ρ=0.211, P=0.03 for total caloric intake and parenteral caloric intake, respectively).
Time Course of Renal Function Parameters during ICU Stay
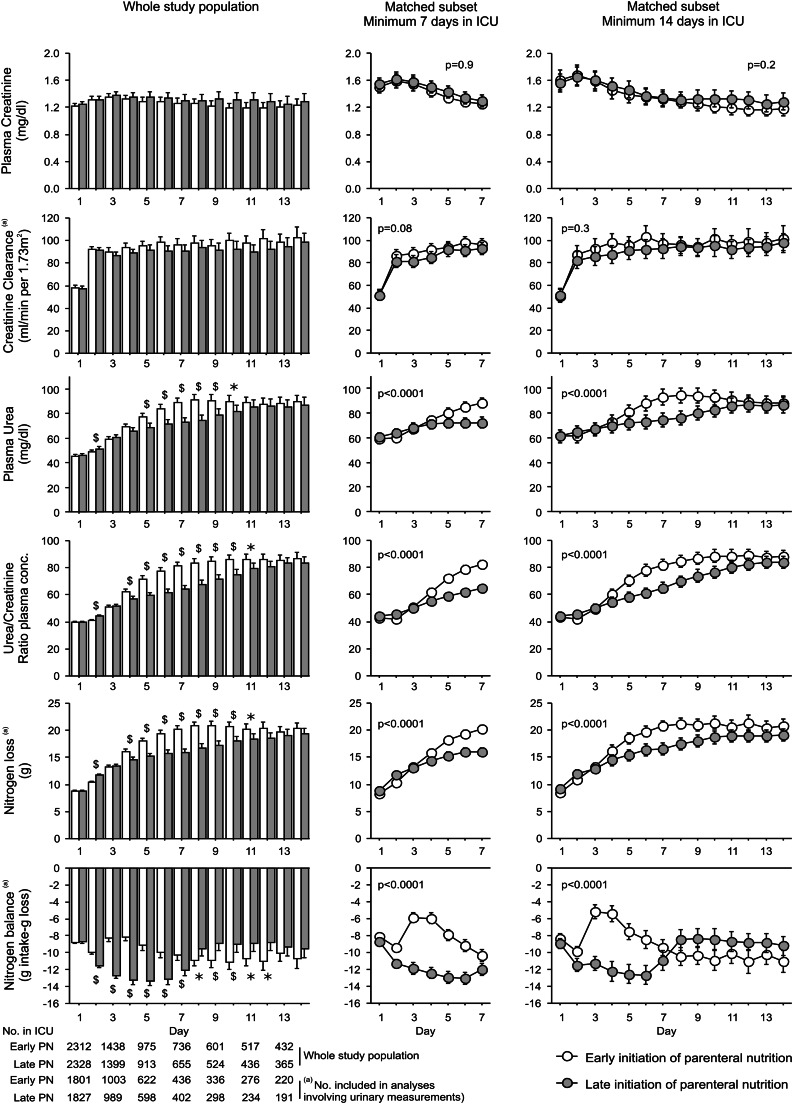
The time course of the plasma creatinine levels and creatinine clearances from day 1 to 14 was not different between randomization groups (Figure 1). Plasma levels of urea, a marker of renal (dys)function but also of protein catabolism, increased over time in both groups. At day 2, plasma urea was slightly higher in the late than the early PN group. In contrast, from day 5 to 10, plasma urea was significantly higher with early PN. To differentiate between AKI-induced increases in plasma urea and changes related to ureagenesis from amino acid breakdown,17 we calculated the daily plasma urea/creatinine ratio. This ratio was slightly higher in the late PN group at day 2 but substantially increased in the early PN group from day 4 on, and it was higher than in the late PN group from day 4 to 11. In both groups, nitrogen loss increased with time in ICU. At day 2, the loss was slightly higher with late PN. From day 4 to 11, nitrogen loss was significantly higher with early PN. The calculated nitrogen balance was somewhat less negative with early PN from day 2 to 7, whereas from day 8 to 12, the calculated nitrogen balance was less negative with late PN. To estimate the percentage of extra administered nitrogen by early PN that was net broken down to urea, we compared the extra nitrogen loss with the supplementary nitrogen intake over a defined time period (Table 4). After 1 week, ∼30% of the extra administered nitrogen by early PN was net broken down to urea. At day 14, 63% of the extra nitrogen intake was net wasted in ureagenesis. All these analyses were confirmed in propensity score-matched subsets of long-stay patients.
Figure 1.
Time profile of renal function and markers of catabolism. Left panel indicates the daily plasma creatinine, creatinine clearance, plasma urea, plasma urea/creatinine ratio, nitrogen loss, and nitrogen balance from day 1 to 14 for the whole study population, respectively (n=4640; n=3628 included in analyses involving urinary measurements). Bar graphs represent means and 95% confidence intervals. P values lower than 0.01 are shown. *0.001≤P<0.01 and $P<0.001 between randomization groups. Center and right panels represent the same parameters from day 1 to 7 and day 14, respectively, for a propensity score-matched subset of patients with a minimum ICU stay of 7 and 14 days, respectively (n=1308 [7 days], n=690 [14 days]; n=760 [7 days], n=328 [14 days] included in analyses involving urinary measurements) (Supplemental Material). Line charts show means and 95% confidence intervals. The P value corresponding to repeated-measures ANOVA is shown.
Table 4.
Nitrogen intake and loss over time
| Population | Median Nitrogen Intake (g) | Median Nitrogen Loss (g) | Nitrogen Difference in Early and Late PN Net Wasted (%) | ||||
|---|---|---|---|---|---|---|---|
| Early PN | Late PN | Difference | Early PN | Late PN | Difference | ||
| Whole study population, with dialyzed patients and patients with insufficient urine data excluded (n=3628) | |||||||
| Day 3 | 1.5 | 0.0 | 1.5 | 12.2 | 12.2 | 0.0 | 0 |
| Day 4 | 9.3 | 0.0 | 9.3 | 15.0 | 13.4 | 1.6 | 17.0 |
| Day 5 | 9.8 | 0.0 | 9.8 | 16.8 | 14.1 | 2.6 | 26.6 |
| Day 6 | 10.4 | 0.0 | 10.4 | 18.5 | 14.2 | 4.3 | 41.0 |
| Day 7 | 10.7 | 1.6 | 9.1 | 18.9 | 14.7 | 4.2 | 45.9 |
| Cumulative days 1–7 | 50.8 | 8.0 | 42.8 | 100.1 | 89.3 | 10.8 | 25.2 |
| Cumulative days 3–7 | 49.9 | 7.4 | 42.5 | 82.5 | 69.9 | 12.6 | 29.6 |
| Cumulative days 1–14 | 122.3 | 85.3 | 37.0 | 243.9 | 220.5 | 23.5 | 63.4 |
| Propensity score-matched subset minimum 7 days in ICU (n=760) | |||||||
| Cumulative days 1–7 | 50.8 | 8.2 | 42.6 | 100.0 | 90.3 | 9.7 | 22.8 |
| Cumulative days 3–7 | 50.3 | 7.6 | 42.7 | 82.5 | 70.1 | 12.4 | 29.1 |
| Cumulative days 1–14 | 121.7 | 84.8 | 36.9 | 243.9 | 221.8 | 22.1 | 60.1 |
| Propensity score-matched subset minimum 14 days in ICU (n=328) | |||||||
| Cumulative days 1–7 | 54.1 | 11.5 | 42.7 | 105.5 | 93.6 | 11.9 | 27.9 |
| Cumulative days 3–7 | 53.3 | 11.2 | 42.1 | 86.2 | 71.1 | 15.1 | 35.8 |
| Cumulative days 1–14 | 127.1 | 85.4 | 41.7 | 246.4 | 220.0 | 26.3 | 63.2 |
Determinants of Duration of RRT in ICU
The original study, showing a 3-day longer RRT duration with early PN, together with the currently observed absence of large differences in AKI incidence and ultimate renal recovery, led us to investigate which factors determined the RRT duration in ICU in relation to early or late PN. At the first day of RRT, plasma creatinine was comparable in both groups, but urinary output and plasma urea were higher in the early than the late PN group (Table 5). At the last RRT day, urinary output, plasma creatinine, and urea were comparable for both randomization groups. When the numbers of in-ICU RRT days with oliguria (urinary output<7.2 ml/kg ideal body weight), elevated plasma creatinine (more than two times the upper limit of normal), and elevated plasma urea (more than two times the upper limit of normal) were jointly entered into multiple regression analysis, with RRT duration in ICU as a dependent variable, only oliguria and hyperuremia days were maintained in the model (Table 6). When the number of ICU days with oliguria, elevated creatinine, and hyperuremia were entered in the model, all three variables were statistically maintained.
Table 5.
Urinary output, plasma creatinine, and plasma urea on the first and last days of new RRT in the ICU (n=359)
| Parameter | Early PN | Late PN | P |
|---|---|---|---|
| First day of RRT in ICU | |||
| Urinary output (ml/d) | 326 (120–700) | 250 (100–631) | 0.03 |
| Plasma creatinine (mg/dl) | 2.77 (1.93–3.71) | 2.80 (1.86–3.83) | 0.71 |
| Plasma urea (mg/dl) | 120 (82–162) | 98 (67–141) | 0.007 |
| Last day of RRT in ICU | |||
| Urinary output (ml/d) | 300 (40–1100) | 480 (50–1200) | 0.19 |
| Plasma creatinine (mg/dl) | 1.63 (0.91–2.71) | 1.91 (1.17–2.79) | 0.08 |
| Plasma urea (mg/dl) | 85 (53–133) | 87 (57–120) | 0.81 |
Data express median (interquartile range).
Table 6.
Multiple linear regression evaluating the independent variables associated with duration of new RRT in the ICU (n=359)
| Independent Variable | β-Coefficienta (95% Confidence Interval) | Standardized-βb | P |
|---|---|---|---|
| Model 1: independent variables evaluated during period on RRT in ICU | |||
| Number of days with urinary output<7.2 ml/kg ideal body weight | 0.474 (0.437–0.511) | 0.697 | <0.001 |
| Number of days with creatinine more than two times the upper limit of normal | 0.024 (−0.029 to 0.077) | 0.032 | 0.37 |
| Number of days with urea more than two times the upper limit of normal | 0.218 (0.168–0.268) | 0.307 | <0.001 |
| Model 2: independent variables evaluated during total ICU stay | |||
| Number of days with urinary output<7.2 ml/kg ideal body weight | 0.543 (0.497–0.588) | 0.722 | <0.001 |
| Number of days with creatinine more than two times the upper limit of normal | 0.080 (0.017–0.143) | 0.095 | 0.01 |
| Number of days with urea more than two times the upper limit of normal | 0.131 (0.079–0.183) | 0.183 | <0.001 |
Regression coefficient.
Standardized regression coefficient.
Discussion
Early full nutritional support of ICU patients has been recommended by European guidelines, which were mainly based on observational studies describing associations between a caloric deficit and adverse outcome.5–7,12 In this preplanned subanalysis of a large, multicenter RCT on the impact of early versus late initiation of PN in critically ill patients, the incidence of AKI stages 1–3 was unaffected by the intervention. Likewise, renal recovery and survival at hospital discharge were similar in both groups. In patients who developed stage 2 AKI, however, renal recovery was slightly prolonged by early PN. Daily measurements of creatinine and creatinine clearance in ICU in the entire study population revealed similar time courses for both groups, which were confirmed after propensity-score matching of long-stay patients. Contrasting with the minimal impact on renal recovery, ureagenesis and nitrogen loss, assessed over the first 2 weeks in ICU, were significantly increased by early PN. Indeed, after a small relative increase at day 2 by late PN, ureagenesis and nitrogen loss increased substantially by early PN. In the second week in ICU, when supplemental PN was also administered in the late PN group, markers of amino acid catabolism increased also in this group. Over the first 2 weeks, two thirds of the extra administered nitrogen through early PN was net wasted in ureagenesis. The higher plasma urea levels may have contributed to the longer RRT duration with early PN.
In the original study report, the incidence of AKI, defined as a minimum doubling of the ICU admission creatinine, was not significantly affected, although a trend was present for more AKI with early PN.15 In the current study, a more sensitive definition of AKI was used, which confirmed the absence of an effect on AKI incidence. Likewise, in the total study population as well as matched subsets of long-stay patients, there was no difference in the time course of creatinine or creatinine clearance.
The original analysis of the EPaNIC trial also suggested that early PN might hamper renal recovery. Indeed, despite an equal number of patients requiring RRT, the RRT duration in ICU was prolonged by early PN.15 The current more sophisticated analysis of renal recovery confirmed a comparable incidence of stage 3 AKI in both groups (the category in which newly dialyzed patients are staged), but refuted a major impact on renal recovery in these patients. In the current analysis, renal recovery was defined as being alive and free from AKI, which implies being free from RRT and a return of plasma creatinine to non-AKI levels. The RRT duration in ICU may give information on partial renal recovery. Also, RRT duration could have been influenced by nonrenal factors. In this regard, the elevated urea levels evoked by early PN, likely explained by net degradation of the extra administered amino acids, may have contributed. Indeed, it was striking to observe that the number of days with elevated urea levels was a significant, independent determinant of the RRT duration when corrected for the number of days with creatinine elevations and oliguria. In addition, both urinary output and plasma urea were higher in the early PN group at the time of RRT initiation. The higher urinary output suggests that RRT may have been initiated earlier because of the higher urea levels. In addition, given the relative hyperuremia by early PN over the first 2 weeks, the similar uremia at the last RRT day could suggest that urea elevations may have driven the prolonged duration of RRT.
The current results are in line with other recent RCTs that did not observe a benefit of altering caloric/protein intake on renal outcome, although only rough markers of kidney dysfunction were studied18–20; also, the relatively smaller trials may lack statistical power.19,20 The EDEN trial, a large, multicenter study in patients with acute lung injury, found no benefit of a trophic versus full enteral nutrition regimen.18 Regarding the kidney, both randomization groups had similar rates of renal failure-free days through day 28 (creatinine<2 mg/dl). Arabi et al.19 investigated the impact of hypocaloric versus full feeding in ICU. The primary end points of 28- and 180-day mortality, and also the need for RRT, were unaffected by randomization. The TICACOS trial was a pilot study on indirect calorimetry-guided feeding versus fixed-formula feeding of ICU patients. With higher calorie and protein intake in the indirect calorimetry group, this study also did not find a difference in a combined renal end point (creatinine>1.2 mg/dl or need for RRT).20
Protein catabolism and muscle wasting commonly occur in ICU patients and are associated with prolonged ventilator times and hampered recovery.21,22 Nutritional strategies seem a rational choice for counteracting catabolism and ensuing negative nitrogen balances.23 However, it is unclear whether and to what extent catabolism can be reversed or even converted into anabolism by artificial feeding.24–26 The results of this study are remarkable. At day 2, nitrogen loss was slightly lower in early versus late PN, probably reflecting less catabolism of endogenous proteins. However, of the extra nitrogen administered by early PN, 30% was net wasted within the first week. From day 3 to 7, the net wasted nitrogen fraction progressively increased. This finding may suggest saturation of nitrogen uptake by early PN. The difference between the two feeding strategies was even larger when the difference in cumulative nitrogen intake and loss was evaluated over 14 days. At day 14, about two thirds of the supplementary nitrogen was net wasted. This result may confirm saturation, as mentioned above, and suggests a progressive failing to retain nitrogen when early PN was given. Hence, these results may oppose part of the critique on the EPaNIC trial that not enough proteins/amino acids would have been administered in the early PN group.27 Because the capacity to build in nitrogen was easily saturated and seemed already substantially exceeded with the administered amount of amino acids, it seems unlikely that a higher amount would have led to more anabolism. The limited ability to retain the extra nitrogen over a longer time period may also explain why the functional status at hospital discharge was not affected by the feeding regimen, as previously reported.15 The data also suggest that the risks of (early) PN are predominant over the potential benefits, with infectious complications,8,10,11 hyperglycemia9 (although carefully avoided in this study), and liver dysfunction28 as a consequence.
A number of mechanisms potentially drive the critically ill body to profound catabolism.29–31 Additional research is required to understand why catabolism is so nonresponsive to feeding in the critically ill. Another point to consider is the physiologic rationale for this highly resistant catabolism. Although catabolism undoubtedly comes at a price and ultimately leads to devastating consequences, recent evidence suggests that (short-term) catabolism, invoked by the natural response to illness (anorexia), may, to a certain extent, be adaptive and beneficial, possibly in part by more efficient autophagy, a major cellular repair pathway.32–34
Some limitations of the present work need to be addressed. First, the minimum baseline creatinine had to be imputed for 1063 patients. However, imputation rate was equal in both groups, and findings were similar against the randomization baseline. Second, there were no creatinine clearance data available beyond ICU discharge. Third, the urea/creatinine ratio is only a rough marker of protein catabolism and can also rise with prerenal azotemia.17 However, the other catabolic markers (nitrogen excretion/balance) changed in the same direction. Fourth, patients requiring RRT needed to be excluded from the analyses involving urinary markers, including calculation of nitrogen loss. Fifth, for multiple regression, independent variables are assumed to be unrelated, which is not the case. We, therefore, do not exclude a role of plasma creatinine in determining the need for RRT. However, the aim of the analysis was to assess which factors are most strongly associated with RRT duration to assess which factors would guide the clinician most to initiate, continue, or stop RRT. In addition, the variance-inflating factor was less than or equal to two for all variables (data not shown), which excludes problematic multicollinearity. Therefore, we consider multiple regression analysis to be valid in this case. Although in theory, other nonrenal factors may have accounted for the difference in RRT duration, the volume and acid–base status, the daily potassium and phosphorus levels, and the incidence of hypercalcemia were similar in both groups (Supplemental Figure 1), which makes involvement of these factors less likely. Finally, not all determinants of the nitrogen balance could be taken into account. Nitrogen intake by blood (products) and albumin could not be calculated, and nonurinary and nonurea losses were estimated on commonly used estimations.35,36 The distribution volume of urea, roughly equal to the body water content, was probably underestimated in patients with a positive fluid balance.37 However, the mentioned inaccuracies were assumed to be equally distributed, and our conclusions were only based on between-group differences. The estimated net wasted nitrogen fraction could not differentiate between breakdown of infused or endogenous amino acids. Finally, nutritional practices not only differ in the timing of PN but also, because the lack of substantial evidence, in the nutrient content, which may, to some extent, limit the extrapolation of the current findings.
In conclusion, early PN had no impact on the AKI incidence or the time course of renal function parameters. In patients with established AKI, there was no major impact on renal recovery, although early PN may have delayed recovery in patients with stage 2 AKI. The extra amino acid supply by early PN seemed inefficient to reverse the negative nitrogen balance, not because of insufficient amino acid delivery, but rather because of insufficient incorporation with, instead, increased degradation into urea. The substantial catabolism of the extra amino acids, leading to pronounced urea generation, may have prolonged the RRT duration observed with early PN.
Concise Methods
Study Design
The EPaNIC study was a prospective, multicenter RCT of 4640 adult ICU patients. The study followed the Declaration of Helsinki. Written informed consent was obtained from the patient or legal guardian. The detailed protocol has been described previously and was approved by the institutional review boards of the respective centers.15 The study design is summarized in Supplemental Material. In brief, patients were randomly assigned to early or late PN. In both groups, when the patient was unable to eat, enteral nutrition was started on the day after ICU admission and increased two times daily when tolerated. When enteral nutrition was insufficient to cover the calculated caloric requirement, supplemental PN was initiated at day 3 in the early PN group. In the late PN group, supplemental PN was only initiated when patients were still in ICU at day 8.
For the current analysis, the staging of AKI was based on the existing guidelines.38–40 AKI stages 1 and 2 were defined as 1.5- and 2-fold rises, respectively, from baseline in plasma creatinine. AKI stage 3 was scored when at least one of the three following criteria was met: minimum threefold rise in plasma creatinine; need for RRT in patients without preexisting RRT need; plasma creatinine≥4 mg/dl with a minimum rise from baseline of 0.5 mg/dl. Because hourly urine output was not recorded, urinary criteria for AKI were omitted. The criterion of any 0.3-mg/dl rise in plasma creatinine over a 48-hour reference period was omitted because of technical limitations.
The impact of the intervention on the incidence of AKI was assessed using two types of baseline creatinine: the plasma creatinine immediately before randomization (randomization baseline) and the estimated premorbid baseline value (minimum baseline). To assess the impact on recovery from AKI, the minimum baseline was used (more information on the rationale is in Supplemental Material). Patients with preadmission RRT were excluded (n=69). For the randomization baseline, the latest measurement of plasma creatinine before ICU admission was retrieved. For emergency admissions, a maximum time frame of 24 hours was allowed between the latest known creatinine and the moment of ICU admission. For elective admissions, the time window was extended to a maximum of 3 months. Creatinine measurements were retrieved from the hospital databases, and in case of no available measurements within that time frame, they were also manually retrieved by searching the documents from referring hospitals/physicians. When no preadmission creatinine measurement was available, the first ICU measurement was used as randomization baseline (n=307). For the minimum baseline, the lowest plasma creatinine in 3 months before ICU admission (elective admission) or the lowest plasma creatinine from 3 months to 1 week before ICU admission (emergency admission) was used. In case of missing values (n=1063), a baseline creatinine was calculated from the Modification of Diet in Renal Disease formula using an estimated GFR of 75 ml/min per 1.73 m2.38 This minimum baseline creatinine is a better estimate of the premorbid kidney function than the randomization baseline. To study the rate of AKI development over time, we compared, in the whole AKI population and per AKI stage, the first day when the patient met the AKI criteria (stage 1 or higher) between both randomization groups.
We assessed the impact of the two nutritional strategies on recovery from AKI and outcome by comparing the following outcome measures: number of days that patients, who were ultimately discharged alive from ICU, fulfilled the AKI criteria in ICU (stage 1 AKI or higher); ICU LOS in these patients; time to alive discharge from ICU and hospital; proportion of patients with an ICU LOS exceeding 7 or 14 days; proportion of patients who were free from AKI (stage 1 or higher) at ICU discharge; proportion of patients discharged alive and AKI-free from hospital; and ICU, hospital, and 90-day mortality. For renal recovery at hospital discharge, we retrieved the last in-hospital plasma creatinine from the hospital databases, and for patients who received RRT, we studied through the medical records and nephrology databases whether patients were still RRT-dependent at that time. In patients with new need for RRT in ICU, we compared the number of patients that were deceased or still RRT-dependent at hospital discharge.
To further analyze a potential impact of nutrition on AKI, we compared, in long-stay patients (ICU stay≥7 days) and independent from randomization, the incidence of the different AKI stages (against minimum and randomization baseline) and the degree of renal recovery at hospital discharge (being alive and AKI-free at hospital discharge) between three strata of cumulative caloric intake until day 7 (achieved cumulative intake between 0th and 30th percentile, between 30th and 70th percentile, or between 70th and 100th percentile). In addition, we calculated, for all AKI subgroups, Spearman correlation coefficient between the cumulative caloric intake until day 7 (enteral/parenteral and parenteral alone in ICU-surviving patients with ICU stay≥7 days) and the number of in-ICU AKI days.
For all patients, we compared the time course of plasma creatinine, creatinine clearance, plasma urea, plasma urea/creatinine ratio, estimated nitrogen loss, and nitrogen balance from day 1 to 14 in ICU in the two randomization arms (calculations of creatinine clearance, nitrogen loss, and balance are in Supplemental Material). Data from patients who were discharged before day 14 were censored at the time of ICU discharge. Missing data for a single day were intrapolated. Patients requiring RRT and patients with missing urine measurements at >2 consecutive days were excluded from analyses involving urinary markers. Because only ICU measurements were included in the database and ICU stay was significantly prolonged by early PN, uncorrected analyses were prone to selection bias. Therefore, we repeated these analyses in a propensity score-matched subset of long-stay patients with a minimum ICU stay of 7 or 14 days (Supplemental Material).
To assess whether kidney function markers were comparable at the time of initiation and discontinuation of new RRT in both groups, we compared the urinary output, plasma creatinine, and plasma urea at the first and last day of RRT in ICU in these patients. To assess the relative contribution of urinary output, plasma creatinine, and plasma urea levels in the clinician’s decision on the timing of RRT in ICU in patients with new RRT, we used multiple regression analysis (Statistical Analyses).
Statistical Analyses
Continuous data were compared using the unpaired t test, median test, and Mann–Whitney U test as appropriate. Proportions were assessed with the chi-squared test. Multiple linear regression analysis was performed using the least-squares method after square root transformation of all variables. The following independent variables were entered into the model for duration of RRT in ICU as dependent variable: the number of days with urinary output <7.2 ml/kg ideal body weight, number of days with plasma creatinine more than two times the upper limit of normal (1.9 mg/dl), and the number of days with plasma urea more than two times the upper limit of normal (100 mg/dl).41 The urea and creatinine cutoffs are well above the 75th percentile of the nondialyzed population at any ICU day. The choice of the oliguria cutoff was based on results from a multicenter survey, in which a urinary output of approximately 7.2 ml/kg per day (<0.3 ml/kg per hour for 24 hours) revealed the best predictive power for successful discontinuation of RRT.41 We performed this analysis for the RRT period in ICU (model 1) and the entire ICU stay (model 2), the latter to exclude potential bias by studying the independent variables only in the period on RRT.
To correct for multiple comparisons of the between-group changes in plasma/urinary markers of the whole-study population over consecutive days, P values<0.01 were considered significant. Otherwise, P values<0.05 were considered statistically significant. Analyses were performed using Statview 5.0.1 and JMP 10.0 software (SAS Institute, Cary, NC).
Disclosures
The authors declare to have no financial conflict of interest to disclose. Baxter Healthcare provided an unrestricted research grant that covered less than one third of the costs of the original EPaNIC study. The company was not involved in the design of the study; the collection, analysis, or interpretation of the data; the preparation of the manuscript; or the decision to submit the manuscript for publication.
Acknowledgments
We thank Sylvia Van Hulle, Sandra Hendrickx, Albert Herelixka, Tine Vanhullebusch, and Katrien Reyniers for data entry and the clinical staff, nurses, and fellows for patient care and compliance with the study protocol.
J.G. and M.P.C. received a Fellowship from the Research Foundation-Flanders (FWO). G.H. received a Clinical Research Fund postdoctoral fellowship (KOF) granted by the University Hospitals Leuven. G.V.d.B., through the University of Leuven, receives structural research financing through the Methusalem program funded by the Flemish Government. This work was supported by University of Leuven Research Fund GOA-2007/14 (to G.V.d.B.). The University of Leuven received an unconditional and nonrestrictive research grant for the EPaNIC trial from Baxter Healthcare.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2012070732/-/DCSupplemental.
References
- 1.Bagshaw SM, George C, Bellomo R, ANZICS Database Management Committe : A comparison of the RIFLE and AKIN criteria for acute kidney injury in critically ill patients. Nephrol Dial Transplant 23: 1569–1574, 2008 [DOI] [PubMed] [Google Scholar]
- 2.Amdur RL, Chawla LS, Amodeo S, Kimmel PL, Palant CE: Outcomes following diagnosis of acute renal failure in U.S. veterans: Focus on acute tubular necrosis. Kidney Int 76: 1089–1097, 2009 [DOI] [PubMed] [Google Scholar]
- 3.Coca SG, Yusuf B, Shlipak MG, Garg AX, Parikh CR: Long-term risk of mortality and other adverse outcomes after acute kidney injury: A systematic review and meta-analysis. Am J Kidney Dis 53: 961–973, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murugan R, Kellum JA: Acute kidney injury: What’s the prognosis? Nat Rev Nephrol 7: 209–217, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fiaccadori E, Lombardi M, Leonardi S, Rotelli CF, Tortorella G, Borghetti A: Prevalence and clinical outcome associated with preexisting malnutrition in acute renal failure: A prospective cohort study. J Am Soc Nephrol 10: 581–593, 1999 [DOI] [PubMed] [Google Scholar]
- 6.Dvir D, Cohen J, Singer P: Computerized energy balance and complications in critically ill patients: An observational study. Clin Nutr 25: 37–44, 2006 [DOI] [PubMed] [Google Scholar]
- 7.Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, Heyland DK: The relationship between nutritional intake and clinical outcomes in critically ill patients: Results of an international multicenter observational study. Intensive Care Med 35: 1728–1737, 2009 [DOI] [PubMed] [Google Scholar]
- 8.Braunschweig CL, Levy P, Sheean PM, Wang X: Enteral compared with parenteral nutrition: A meta-analysis. Am J Clin Nutr 74: 534–542, 2001 [DOI] [PubMed] [Google Scholar]
- 9.Gramlich L, Kichian K, Pinilla J, Rodych NJ, Dhaliwal R, Heyland DK: Does enteral nutrition compared to parenteral nutrition result in better outcomes in critically ill adult patients? A systematic review of the literature. Nutrition 20: 843–848, 2004 [DOI] [PubMed] [Google Scholar]
- 10.Peter JV, Moran JL, Phillips-Hughes J: A metaanalysis of treatment outcomes of early enteral versus early parenteral nutrition in hospitalized patients. Crit Care Med 33: 213–220, discussion 260–261, 2005 [DOI] [PubMed] [Google Scholar]
- 11.Simpson F, Doig GS: Parenteral vs. enteral nutrition in the critically ill patient: A meta-analysis of trials using the intention to treat principle. Intensive Care Med 31: 12–23, 2005 [DOI] [PubMed] [Google Scholar]
- 12.Singer P, Berger MM, Van den Berghe G, Biolo G, Calder P, Forbes A, Griffiths R, Kreyman G, Leverve X, Pichard C, ESPEN : ESPEN Guidelines on Parenteral Nutrition: Intensive care. Clin Nutr 28: 387–400, 2009 [DOI] [PubMed] [Google Scholar]
- 13.Heyland DK, Dhaliwal R, Drover JW, Gramlich L, Dodek P, Canadian Critical Care Clinical Practice Guidelines Committee : Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. JPEN J Parenter Enteral Nutr 27: 355–373, 2003 [DOI] [PubMed] [Google Scholar]
- 14.Martindale RG, McClave SA, Vanek VW, McCarthy M, Roberts P, Taylor B, Ochoa JB, Napolitano L, Cresci G, American College of Critical Care Medicine. A.S.P.E.N. Board of Directors : Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition: Executive Summary. Crit Care Med 37: 1757–1761, 2009 [DOI] [PubMed] [Google Scholar]
- 15.Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, Van Cromphaut S, Ingels C, Meersseman P, Muller J, Vlasselaers D, Debaveye Y, Desmet L, Dubois J, Van Assche A, Vanderheyden S, Wilmer A, Van den Berghe G: Early versus late parenteral nutrition in critically ill adults. N Engl J Med 365: 506–517, 2011 [DOI] [PubMed] [Google Scholar]
- 16.Casaer MP, Hermans G, Wilmer A, Van den Berghe G: Impact of early parenteral nutrition completing enteral nutrition in adult critically ill patients (EPaNIC trial): A study protocol and statistical analysis plan for a randomized controlled trial. Trials 12: 21, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van den Berghe G, Wouters P, Weekers F, Mohan S, Baxter RC, Veldhuis JD, Bowers CY, Bouillon R: Reactivation of pituitary hormone release and metabolic improvement by infusion of growth hormone-releasing peptide and thyrotropin-releasing hormone in patients with protracted critical illness. J Clin Endocrinol Metab 84: 1311–1323, 1999 [DOI] [PubMed] [Google Scholar]
- 18.Rice TW, Wheeler AP, Thompson BT, Steingrub J, Hite RD, Moss M, Morris A, Dong N, Rock P, National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network : Initial trophic vs full enteral feeding in patients with acute lung injury: The EDEN randomized trial. JAMA 307: 795–803, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arabi YM, Tamim HM, Dhar GS, Al-Dawood A, Al-Sultan M, Sakkijha MH, Kahoul SH, Brits R: Permissive underfeeding and intensive insulin therapy in critically ill patients: A randomized controlled trial. Am J Clin Nutr 93: 569–577, 2011 [DOI] [PubMed] [Google Scholar]
- 20.Singer P, Anbar R, Cohen J, Shapiro H, Shalita-Chesner M, Lev S, Grozovski E, Theilla M, Frishman S, Madar Z: The tight calorie control study (TICACOS): A prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med 37: 601–609, 2011 [DOI] [PubMed] [Google Scholar]
- 21.De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Durand-Zaleski I, Boussarsar M, Cerf C, Renaud E, Mesrati F, Carlet J, Raphaël JC, Outin H, Bastuji-Garin S, Groupe de Réflexion et d’Etude des Neuromyopathies en Réanimation : Paresis acquired in the intensive care unit: A prospective multicenter study. JAMA 288: 2859–2867, 2002 [DOI] [PubMed] [Google Scholar]
- 22.De Jonghe B, Bastuji-Garin S, Durand MC, Malissin I, Rodrigues P, Cerf C, Outin H, Sharshar T, Groupe de Réflexion et d’Etude des Neuromyopathies en Réanimation : Respiratory weakness is associated with limb weakness and delayed weaning in critical illness. Crit Care Med 35: 2007–2015, 2007 [DOI] [PubMed] [Google Scholar]
- 23.Debaveye Y, Van den Berghe G: Risks and benefits of nutritional support during critical illness. Annu Rev Nutr 26: 513–538, 2006 [DOI] [PubMed] [Google Scholar]
- 24.Streat SJ, Beddoe AH, Hill GL: Aggressive nutritional support does not prevent protein loss despite fat gain in septic intensive care patients. J Trauma 27: 262–266, 1987 [DOI] [PubMed] [Google Scholar]
- 25.Frankenfield DC, Smith JS, Cooney RN: Accelerated nitrogen loss after traumatic injury is not attenuated by achievement of energy balance. JPEN J Parenter Enteral Nutr 21: 324–329, 1997 [DOI] [PubMed] [Google Scholar]
- 26.Ishibashi N, Plank LD, Sando K, Hill GL: Optimal protein requirements during the first 2 weeks after the onset of critical illness. Crit Care Med 26: 1529–1535, 1998 [DOI] [PubMed] [Google Scholar]
- 27.Wischmeyer P: Parenteral nutrition and calorie delivery in the ICU: Controversy, clarity, or call to action? Curr Opin Crit Care 18: 164–173, 2012 [DOI] [PubMed] [Google Scholar]
- 28.Grau T, Bonet A, Rubio M, Mateo D, Farré M, Acosta JA, Blesa A, Montejo JC, de Lorenzo AG, Mesejo A, Working Group on Nutrition and Metabolism of the Spanish Society of Critical Care : Liver dysfunction associated with artificial nutrition in critically ill patients. Crit Care 11: R10, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vanhorebeek I, Van den Berghe G: Hormonal and metabolic strategies to attenuate catabolism in critically ill patients. Curr Opin Pharmacol 4: 621–628, 2004 [DOI] [PubMed] [Google Scholar]
- 30.Mitch WE, Goldberg AL: Mechanisms of muscle wasting. The role of the ubiquitin-proteasome pathway. N Engl J Med 335: 1897–1905, 1996 [DOI] [PubMed] [Google Scholar]
- 31.Derde S, Vanhorebeek I, Ververs EJ, Vanhees I, Darras VM, Van Herck E, Larsson L, Van den Berghe G: Increasing intravenous glucose load in the presence of normoglycemia: Effect on outcome and metabolism in critically ill rabbits. Crit Care Med 38: 602–611, 2010 [DOI] [PubMed] [Google Scholar]
- 32.Vanhorebeek I, Gunst J, Derde S, Derese I, Boussemaere M, Güiza F, Martinet W, Timmermans JP, D’Hoore A, Wouters PJ, Van den Berghe G: Insufficient activation of autophagy allows cellular damage to accumulate in critically ill patients. J Clin Endocrinol Metab 96: E633–E645, 2011 [DOI] [PubMed] [Google Scholar]
- 33.Derde S, Vanhorebeek I, Güiza F, Derese I, Gunst J, Fahrenkrog B, Martinet W, Vervenne H, Ververs EJ, Larsson L, Van den Berghe G: Early parenteral nutrition evokes a phenotype of autophagy deficiency in liver and skeletal muscle of critically ill rabbits. Endocrinology 153: 2267–2276, 2012 [DOI] [PubMed] [Google Scholar]
- 34.Gunst J, Derese I, Aertgeerts A, Ververs EJ, Wauters A, Van den Berghe G, Vanhorebeek I: Insufficient autophagy contributes to mitochondrial dysfunction, organ failure, and adverse outcome in an animal model of critical illness. Crit Care Med 41: 177–189, 2013 [DOI] [PubMed] [Google Scholar]
- 35.Voerman BJ, Strack van Schijndel RJ, Groeneveld AB, de Boer H, Nauta JP, Thijs LG: Effects of human growth hormone in critically ill nonseptic patients: Results from a prospective, randomized, placebo-controlled trial. Crit Care Med 23: 665–673, 1995 [DOI] [PubMed] [Google Scholar]
- 36.Hsu CW, Sun SF, Lin SL, Huang HH, Wong KF: Moderate glucose control results in less negative nitrogen balances in medical intensive care unit patients: A randomized, controlled study. Crit Care 16: R56, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Himmelfarb J, Evanson J, Hakim RM, Freedman S, Shyr Y, Ikizler TA: Urea volume of distribution exceeds total body water in patients with acute renal failure. Kidney Int 61: 317–323, 2002 [DOI] [PubMed] [Google Scholar]
- 38.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup : Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8: R204–R212, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A, Acute Kidney Injury Network : Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care 11: R31, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kidney Disease: Improving Global Outcome (KDIGO) Acute Kidney Injury Working Group : KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2: 1–138, 2012 [Google Scholar]
- 41.Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Straaten HO, Ronco C, Kellum JA: Discontinuation of continuous renal replacement therapy: A post hoc analysis of a prospective multicenter observational study. Crit Care Med 37: 2576–2582, 2009 [DOI] [PubMed] [Google Scholar]