Abstract
During HIV/SIV infection, mucosal immune system dysfunction and systemic immune activation are associated with progression to AIDS, however it is unclear to what extent pre-existing gastrointestinal damage relates to disease progression after infection. Pigtail macaques (PTM) are an excellent model in which to assess mucosal dysfunction in relation to HIV/SIV pathogenesis, as the majority of these animals have high levels of gastrointestinal damage, immune activation, and microbial translocation prior to infection, and rapidly progress to AIDS upon SIV infection. Here we characterized the mucosal immune environment prior to and throughout SIV infection in 13 uninfected PTM and 9 SIV-infected PTM, of which 3 were slow progressors. This small subset of slow progressors had limited innate immune activation in mucosal tissues in the periphery, which was associated with a more intact colonic epithelial barrier. Furthermore, we found that pre-infection levels of microbial translocation, as measured by lipopolysaccharide binding protein (LBP), in PTM correlated with the rate of progression to AIDS. These data suggest that pre-existing levels of microbial translocation and gastrointestinal tract dysfunction may influence the rate of HIV disease progression.
Introduction
It has become increasingly clear that during human immunodeficiency virus (HIV) infection, progression to acquired immunodeficiency syndrome (AIDS) is intimately associated with dysfunction of gastrointestinal immunity (1, 2). Indeed, it has been well established that HIV infection in humans, and likewise pathogenic simian immunodeficiency virus (SIV) infection of non-human Asian primates, results in significant damage to the immunological and structural barrier of the gastrointestinal (GI) tract, beginning within days of infection (1–4). Dysfunction in the GI tract in pathogenic HIV/SIV infection includes massive depletion of CD4+ T-cells, damage to the epithelial barrier, and alteration in the cytokines produced by resident lymphocytes (1, 5–8). Further, the hampered barrier function in the GI tract results in deleterious effects such as translocation of luminal contents from the GI tract and consequent inflammation (2–4, 9–11). This presence of bacterial products (microbial translocation) in the periphery contributes to systemic immune activation, which is a cornerstone of progression to AIDS (9, 12–14). Though the importance of immune activation and dysfunction of the mucosal immune system in AIDS progression is appreciated, the mechanisms underpinning these dysfunctions are unclear.
SIV infection of pigtail macaques (Macaca nemestrina, PTM) is regarded as a model to evaluate how gastrointestinal damage and immunological alterations influence AIDS progression (15–18). PTM progress to AIDS rapidly and the immunologic and virologic aspects of SIV infection are becoming increasingly well-established (16–18). Gastrointestinal damage, which is associated with AIDS progression, tends to be increased in SIV-uninfected PTM compared to SIV-uninfected rhesus macaques (Macaca mulatta, RM) (15). Furthermore, during SIV infection, PTM have higher levels of T-cell turnover and activation in peripheral blood when compared to their RM counterparts (16), and are prone to thrombocytopenia (19). Hence, PTM are an excellent model to unravel mechanisms underlying the dysfunction of the mucosal immune system that contributes to AIDS progression.
Here, we extended upon previous research characterizing SIV infection in PTM (16) with the aim of understanding the influence of SIV infection on gastrointestinal immunity and SIV disease progression. We analyzed CD4+ T-cell loss, immune activation, microbial translocation and barrier function in GI tract tissues. Further, with the inadvertent opportunity to follow three slow progressors, we also aimed to define correlates of progression by comparing these factors in SIV-uninfected and SIV-infected slow progressor and progressor PTM. Given our small sample size of slow progressors, these comparisons may not necessarily be extrapolated to disease characterization in all models of slow progression, but may point to important indicators of progression for future research in larger studies.
Materials and Methods
Study animals and sample collection
Nine PTM were infected intravenously with 3,000 TCID50 of SIVmac239. PTM were monitored prior to SIV infection to progression to AIDS (6/9 animals; progressors; P) or scheduled euthanasia after lack of AIDS progression after >700 days (3/9 animals; slow progressors; SP). Thirteen SIV-uninfected animals were also analyzed for comparison (of note, in SIV- PTM the number of animals analyzed is variable depending on tissues collected). Upon necropsy, blood, axillary lymph nodes (ALN), mesenteric lymph nodes (MLN), jejunum, and colon were collected. Lymphocytes were isolated and cryopreserved from LNs and GI tract tissues as previously described (15). All animals were housed and cared for in accordance with the American Association for Accreditation of Laboratory Animal Care (AAALAC) standards in AAALAC-accredited facilities, and all animal procedures were performed according to protocols approved by the Institutional Animal Care and Use Committee of the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Viral loads
Viral RNA levels in plasma were determined by real-time reverse transcription-PCR (ABI Prism 7700 sequence detection system; Applied Biosystems, Carlsbad, CA, USA) using reverse-transcribed viral RNA in plasma samples from SIVmac239-inoculated PTM as previously described (20).
Immunohistochemistry and quantitative image analysis
Staining of tissue sections and quantitative image analysis were performed as previously described (15, 21). Epithelial barrier integrity in the colon was determined by immunochemistry (IHC) for the tight junction protein claudin-3 (rabbit polyclonal, Labvision, Fremont, CA, USA), and immune activation in the MLN, colon, jejunum, and ALN by IHC for the type I interferon responsive gene product, myxovirus protein A (MxA; mouse monoclonal, clone M143; from Drs Otto Haller and Georg Kochs, Department of Virology, University of Freiburg, Freiburg, Germany). High-power (x400) whole tissue scans were obtained using a ScanScope CS System (Aperio Technologies, Vista, CA, USA) and imported into Photoshop CS3 (Adobe Systems, Mountain View, California, USA). The percent area of tissue stained for MxA was determined in the entire MLN and the lamina propria of colon and jejunum as previously described (15) using Photoshop CS3 tools with FoveaPro plugins (Version 3.0; Reindeer Graphics, Asheville, NC, USA) and the ratio of damaged to intact colonic epithelium was measured using the Aperio pen tool to outline and calculate the length of colonic breaches (claudin-3 negative regions) divided by the length of intact colonic epithelium (claudin-3 positive regions).
Cellular staining and flow cytometry
Multicolor flow cytometric analysis was performed on thawed samples as previously described (15), using pre-determined optimal concentrations of antibodies that cross-react with PTM, which included: CD3 (clone SP34-2, BD Biosciences, San Jose, CA, USA), CD4 (OKT4, eBioscience, San Diego, CA, USA), CD8 (RPA-T8, eBioscience or 3B5, Invitrogen, Grand Island, NY, USA), CD14 (M5E2, Biolegend, San Diego, CA, USA or TüK4, Invitrogen), CD45 (MB46D6, Miltenyi, Cambridge, MA, USA), CD20 (2H7, eBioscience), CD27 (O323, eBioscience), CD38 (OKT10, NIH Nonhuman Primate Reagent Resource), CD28 (28.2, Beckman Coulter, Brea, CA, USA), CD95 (DX2, BD Biosciences), CD103 (B-Ly7, eBioscience), IL-17 (eBio64CAP17, eBioscience), IL-22 (IL22JOP, eBioscience), and Aqua Live/Dead dye (Invitrogen). Flow cytometric acquisition was performed on at least 100,000 cells on a BD LSRFortessa cytometer driven by the FACS DiVa software (version 6.0; BD Biosciences). Analysis of the acquired data was performed using FlowJo software (version 9.4.11; TreeStar, Ashland, OR, USA). We used a threshold of 200 collected events for all analysis of specific cell subsets.
Plasma LBP levels
Plasma LBP was quantified with a commercially available ELISA assay (Biometec, Greifswald, Germany) according to the manufacturer’s protocol. We ran samples in duplicate and subtracted the background.
Statistical analysis
We performed Mann-Whitney U test for all t-test P values and performed Bonferroni adjustment for multiple comparisons, horizontal bars in Fig.s reflect mean. Spearman rank calculation and linear regression were calculated for comparative correlations, performed using Prism software (Version 5.0; GraphPad, La Jolla, CA, USA).
Results
Slow progression in pigtail macaques
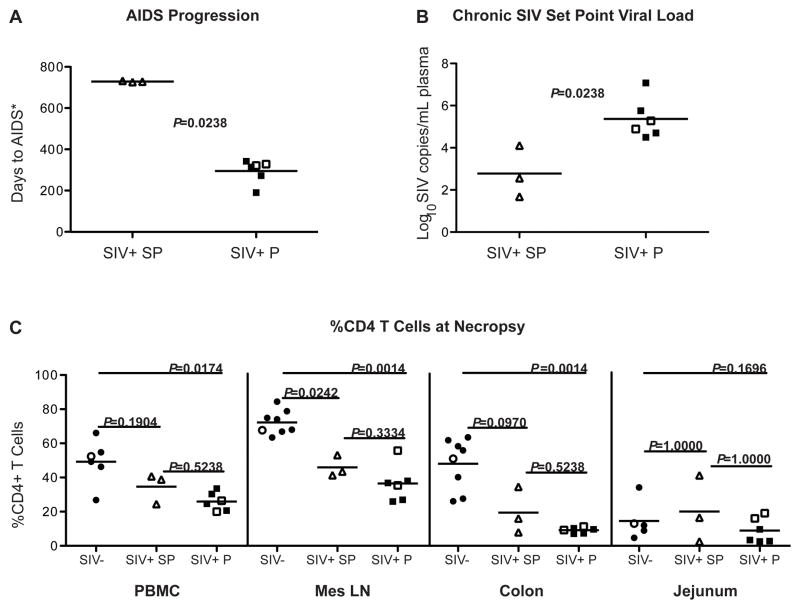
Gastrointestinal immune dysfunction is a key factor in driving immune activation and HIV/SIV disease pathogenesis (1, 3, 6). However, it is unclear to what extent mucosal determinants relate to the rate of progression to AIDS. Thus, in order to better understand the mucosal immunology of pathogenic SIV infection relative to the rate of AIDS progression, we studied mucosal tissues in a cohort of 9 SIVmac239-infected PTM with differential disease progression, in which SIV disease kinetics have been previously described in peripheral blood (16), and 13 uninfected PTM (15). Six of the 9 SIV-infected PTM rapidly progressed to AIDS while 3 maintained a slow progressor (SP) phenotype, evident by a lack of AIDS progression after >700 days post-inoculation, at which point the animals were euthanized (16). Of note, because these animals were scheduled for euthanasia and may have otherwise eventually progressed, we refer to them as slow progressors rather than long-term non-progressors. The 6 progressing animals (P) exhibited AIDS-defining illnesses at an average of 296 days post-infection, which was significantly more rapid than the 3 slow progressors, who were euthanized on days 727, 729, and 733 (P=0.02, Fig. 1A), a comparison which is likely understated, since the SPs had not yet progressed to AIDS at the time of necropsy. Of note, all 3 of the SP, along with 2 progressors and 2 SIV- PTM, possessed the potentially protective Mane-A1*084 allele. Consistent with this slow progressor phenotype, despite similar peak viremia between the groups, the SP were better able to suppress viremia during the chronic stage of SIV infection (Fig. 1B). The set point viral load during the chronic stage of SIV infection was, on average, 2.78 log10 SIV copies/mL plasma in slow progressors, significantly lower than that of the progressors who had an average of 5.54 log10 SIV copies/mL plasma (P=0.02; Fig. 1B).
Fig. 1. AIDS progression, viremia, and CD4+ lymphocyte populations in pigtail macaques during SIV infection.
(A) Progression to AIDS in SIV+ slow progressors (SP) and SIV+ progressors (P). Progression measured as days post infection until AIDS defining illness (*or scheduled euthanasia in SP). (B) Set point viral load measured during chronic infection (>200 days post infection). (C) The percentage of CD4+ T cells was measured by flow cytometry, gated on live, singlet, CD3+ T cells. Cells measured were from peripheral blood mononuclear cells (PBMC, left), mesenteric lymph nodes (MLN, left center), colon (right, center), and jejunum (right), obtained at necropsy. Horizontal lines represent mean and P-values were calculated using Mann-Whitney nonparametric U test. For multiple comparisons, P-value was adjusted with Bonferroni correction. SIV-uninfected, circles; SIV-uninfected Mane-A1*084+, open circles; SIV+ Mane-A1*084+ slow progressors, open triangles; SIV+ progressors, squares; SIV+ Mane-A1*084+ progressors, open squares.
HIV preferentially infects CD4+ T-cells, and a characteristic of disease progression is rapid loss of this crucial subset in mucosal tissues, followed by chronic depletion of CD4+ T-cells in peripheral tissues (7, 22–24). Thus, to assess whether differences in viral load were reflected in CD4+ T-cell maintenance we measured the percentage of lymphocyte populations in tissues from necropsy by flow cytometry.. In peripheral blood mononuclear cells (PBMC), slow progressors maintained a slightly higher percentage of CD4+ T-cells than progressors, though not significantly so (Fig. 1C left). However, when progressors were compared to SIV- PTM, there is, as expected, a significant decline of CD4+ T-cells in peripheral blood (Fig. 1C, P=0.02).
Because depletion of CD4+ T-cells is most prevalent in the GI tract (7, 23), we quantified the CD4+ T-cell populations in mucosal sites including mesenteric lymph nodes (MLN), colon, and jejunum, to represent mucosal secondary lymphoid tissues, large intestine, and small intestine, respectively. In the MLN, slow progressors had an average of 45.97% CD4+ T-cells while progressors had an average of 36.47% (P=0.33; Fig. 1C left center). Similar to PBMCs, when compared to uninfected PTM, the loss of CD4+ T-cells in the MLN was more pronounced in progressors than SP (P<0.01 and P=0.02, respectively). Furthermore, the loss of CD4+ T-cells in the colon was more pronounced in progressors than SP (P<0.01 versus P=0.10; Fig. 1C right center) when compared to uninfected PTM. However, in the jejunum, low pre-SIV levels of CD4+ T-cells persisted after SIV infection, with only a slight indication of CD4+ T-cell decline in progressors versus SIV- PTM (P=0.17; Fig. 1C right). This depletion of CD4+ T-cells from the GI tract and limited peripheral CD4+ T-cell loss of slow progressors is consistent with models of nonprogressive SIV infection of natural hosts, which also have moderate depletion of mucosal CD4+ T-cells, but do not progress to AIDS (25–27).
Recent data has shown that specific mucosal CD4+ T-cell subsets that produce IL-17 and IL-22, cytokines associated with mucosal immune homeostasis, are lost during pathogenic SIV infection of rhesus macaques (6, 28–30). Similarly, in our cohort of SIV-infected PTM here, we found significant loss of IL-17 and IL-22 producing CD4+ T-cells in mucosal tissues (P<0.01; Suppl. Fig. 1B–C). Furthermore, loss of essential homeostatic lymphocytes in mucosal tissues during SIV infection has been associated with loss of CD103+ dendritic cells (DCs), which are crucial for directing homeostatic T-cell responses, including Th17 (6, 31). Indeed, these CD103+ DCs are also significantly lost in SIV-infected progressor PTM (P<0.01, Suppl. Fig. 1D), which may underlie loss of IL-17 and IL-22 producing CD4+ T-cells.
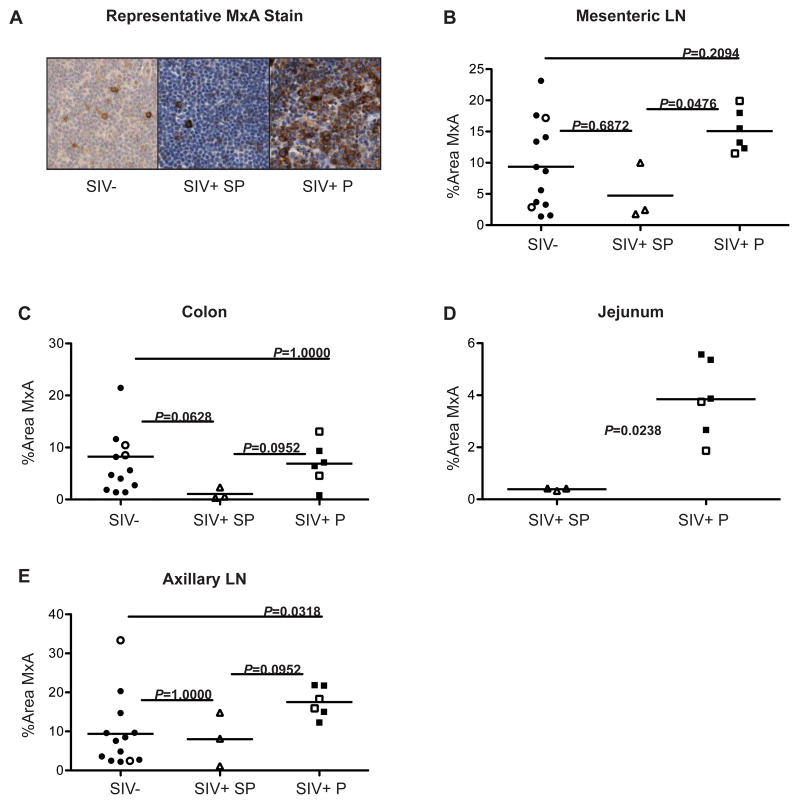
Immune activation is decreased in PTM slow progressors
Given that systemic immune activation is a principal predictor of CD4+ T-cell loss and AIDS progression (12–14), we next characterized immune activation in mucosal and systemic tissues from PTM. It has been previously established that PTM exhibit higher levels of immune activation in the absence of SIV infection compared to rhesus macaques, and that after SIV infection, PTM have high levels of T-cell turnover and activation in peripheral blood (16). We quantified immune activation in tissue sections stained by IHC with a monoclonal antibody against MxA, a protein produced in response to type-1 interferon (indicating local immune activation) (32) (Fig. 2A). Comparing MxA expression in the SIV-negative, SP, and progressor PTM revealed that slow progressors exhibited markedly less immune activation than progressors in all 3 of the GI tract sites we evaluated (Fig. 2B–D). In the MLN, SP had an average of 4.74% of the tissue occupied by MxA as compared to progressors, who had an average of 15.08% of the tissue occupied by MxA (P= 0.05; Fig. 2B). However, the SP had similar levels of activation compared to uninfected PTM, who had an average of 9.36% MxA (P=0.69; Fig. 2B) in the MLN. In the lamina propria of the colon, SP demonstrated noticeably less activation than both progressors (average of 6.89% MxA; P= 0.10) or uninfected PTM (average of 8.23% MxA; P=0.06) with SP having only an average of 1.07% MxA (Fig. 2C). However, perhaps surprisingly, the amount of activation in the colon was comparable between progressors and uninfected animals (P=1.00). Furthermore, in the lamina propria of the jejunum, SP showed significantly less immune activation compared to progressors, with SP having an average of 0.39% of the lamina propria occupied by MxA compared to 3.85% MxA in progressors (P=0.02; Fig. 2D) (uninfected PTM data not available). These data are consistent with previous studies demonstrating high levels of underlying mucosal damage and immune activation in the GI tract of uninfected PTM (15), but indicate that slow progressors may have additional mechanisms to dampen immune activation in the GI tract, independent of SIV infection.
Fig. 2. Immune activation in the GI tract and periphery is reduced in slow progressors.
The amount of immune activation in necropsy tissues was measured by immunohistochemistry staining for MxA, an interferon-responsive protein. (A) Representative MxA stain (brown) in lymph node samples from SIV− (left), SIV+ slow progressors (center), and SIV+ progressors (right). The percent area of tissue quantified as positively stained for MxA in (B) mesenteric lymph node, (C) colon, (D) jejunum, and (E) axillary lymph node. Horizontal lines represent mean and P-values were calculated using Mann-Whitney nonparametric U test. For multiple comparisons, P-value was adjusted with Bonferroni correction. SIV-uninfected, circles; SIV-uninfected Mane-A1*084+, open circles; SIV+ Mane-A1*084+ slow progressors, open triangles; SIV+ progressors, squares; SIV+ Mane-A1*084+ progressors, open squares.
Though slow progressors were able to limit activation locally in the GI tract we also sought to investigate immune activation in peripheral lymphoid tissue. Of interest, while adaptive immune cell activation in T and B cells tended to be increased in progressors compared to SPs, it was not significantly different as measured by Ki67, CD38 and HLA-DR in CD4+ T-cells (Suppl. Fig. 2 A–B) and CD8+ T-cells (Suppl. Fig. 2 C–D), as well as CD27 and Ki67 in B-cells (Suppl. Fig. 3), though this could be due to the limited numbers of animals. However, we hypothesized that innate immune activation may be increased and thus, we quantified levels of MxA in the axillary lymph node (ALN) at necropsy (Fig. 2E). Of interest, slow progressors, with an average of 8.03% MxA in the ALN, had levels of peripheral immune activation comparable to that of uninfected PTM who had an average 9.39% MxA (P=1.00; Fig. 2E). Activation in the ALNs of progressors, on the other hand, was markedly higher, with an average 17.52% MxA, when compared to uninfected PTM (P=0.03), and slightly higher than SP (P=0.10). Thus, a key feature of progressive SIV infection in PTM is robust immune activation in systemic lymphoid sites.
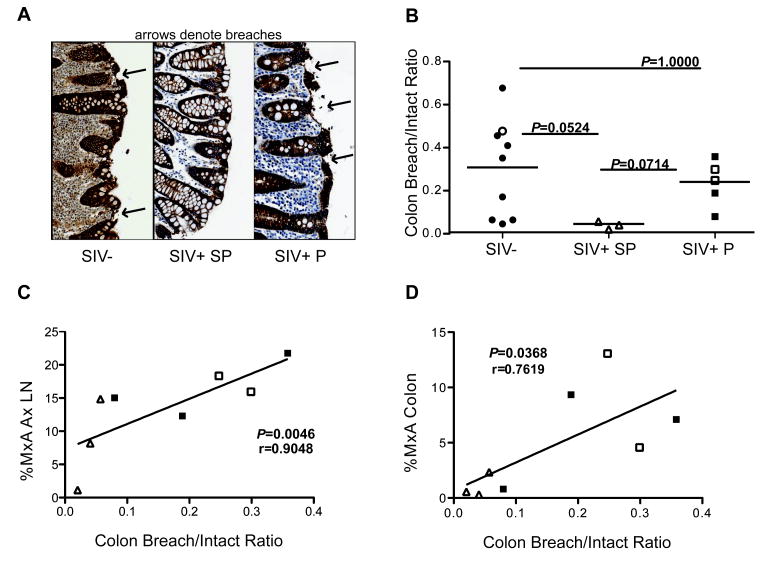
Systemic immune activation is associated with damage to the colon barrier
Pathogenic HIV/SIV infections are strongly associated with immune dysfunction and destruction of the GI epithelial barrier (1–4, 9). Thus, we quantified the continuity of the colonic barrier by IHC using antibodies against claudin-3, a tight junction protein, and quantified the ratio of the length of breached epithelium (not stained for claudin) to intact epithelium (stained for claudin) (Fig. 3A). Of interest, we found the underlying level of breaches in uninfected PTM was comparable to that of SIV+ progressors (P=1.00), while the level of breaches in slow progressors was lower than both uninfected (P=0.05) and SIV+ progressors (P=0.07). These data suggest that slow progressors may have pre-existing factors that protect their tight epithelial barrier from the damage that is typically characteristic of the GI tract of PTM as well as in pathogenic HIV/SIV infections. When we compared the GI epithelial damage to immune function, we found a strong correlation between the barrier integrity of the colon and the level of peripheral immune activation in infected PTM (P<0.01, Spearman r=0.90; Fig. 3C). Furthermore, we found the correlation between barrier integrity and activation was also significant locally in the colon (P=0.04, Spearman r=0.76; Fig. 3D). There was also a trend towards an association between barrier integrity and MLN activation (P=0.11, data not shown). These data suggest a relationship between colonic barrier integrity and local and systemic activation.
Fig. 3. Peripheral activation is related to colon epithelial damage, which is reduced in slow progressors.
The breach/intact ratio in colonic necropsy tissues was measured by immunohistochemical staining for claudin-3, a tight junction protein. Breached epithelium (not stained for claudin) was quantified in relation to intact epithelium (stained for claudin). (A) Representative claudin stain with arrows indicating epithelial breaches. (B) Comparison of colon breach/intact ratio in PTM. (C) The breach/intact ratio significantly correlates with the amount of immune activation, measured by MxA, in the axillary lymph node. (D) The breach/intact ratio significantly correlates with the amount of immune activation in the colon. Correlation determined by Spearman’s rank correlation. Line represents linear regression. Horizontal lines represent mean and P-values were calculated using Mann-Whitney nonparametric U test. For multiple comparisons, P-value was adjusted with Bonferroni correction. SIV-uninfected, circles; SIV+ Mane-A1*084+ slow progressors, open triangles; SIV+ progressors, squares; SIV+ Mane-A1*084+ progressors, open squares.
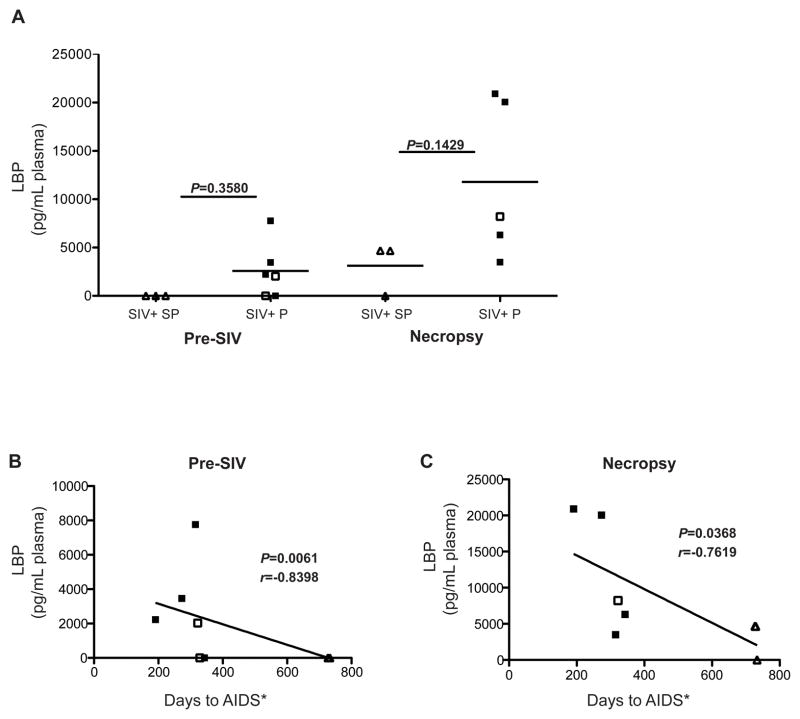
Microbial translocation predicts AIDS progression
Intestinal damage in SIV infection has been shown to result in microbial translocation, a cause of systemic immune activation (3, 9, 15). Given that we observed greater intestinal damage as well as local and peripheral immune activation in progressors, we sought to determine whether a potential relationship existed between microbial translocation and progression to AIDS. In order to measure microbial translocation, we quantified the concentration of lipopolysaccharide-binding protein (LBP) throughout infection in the plasma of PTM by ELISA. LBP is produced in response to bacterial lipopolysaccharide (LPS) and thus indicates presence of microbial products in the bloodstream (33), and LBP may be the most reliable measurement of systemic microbial translocation in plasma of non-human primates (34). Prior to SIV infection, the PTM that went on to become progressors tended to have higher levels of plasma LBP (Fig. 4A). Furthermore, at necropsy, while all animals had increases in LBP, the PTM with AIDS had slightly higher levels of LBP compared to the slow progressors (P=0.14, Fig. 4A). Importantly, levels of LBP prior to SIV infection significantly correlated with the rate to AIDS progression after SIV infection (P<0.01, Spearman r=−0.84; Fig. 4B). Thus, pre-existing levels of microbial translocation may dictate the rate of disease progression once infected. Furthermore, we also found a significant correlation between microbial translocation as measured by LBP at necropsy and progression to AIDS (P=0.04, Spearman r=−0.76; Fig. 4C). Notably, this relationship was statistically stronger than the relationships we observed between time to AIDS progression and typical disease indicators, such as set-point viral load and absolute CD4+ T cell count at necropsy (Suppl. Fig. 4A–B). Furthermore, it presented a more extreme disparity than the comparison of CD4 count at necropsy between groups, as LTNP had only slightly higher absolute CD4 counts than progressors, and the relationship was not statistically significant (P=0.26, Suppl. Fig. 4C). Though our findings are limited to a small subset of PTM, our data indicate that plasma LBP might serve as a potential identifier of susceptibility to AIDS progression both prior to and during SIV infection. Furthermore, our data support the role of microbial translocation in predicting AIDS progression.
Fig. 4. Microbial translocation pre-infection and at necropsy correlate with AIDS progression.
Lipopolysaccharide-binding protein (LBP) was measured in plasma as a marker of microbial translocation. (A) The concentration of LBP in plasma prior to infection (left) and at necropsy (right). The plasma LBP concentration (B) pre-SIV infection, and (C) at necropsy, negatively correlates with days until AIDS progression (*or scheduled necropsy in SP). Correlation determined by Spearman’s rank correlation. Line represents linear regression. Horizontal lines represent mean and P-values were calculated using Mann-Whitney nonparametric U test. SIV+ Mane-A1*084+ slow progressors, open triangles; SIV+ progressors, squares; SIV+ Mane-A1*084+ progressors, open squares.
Discussion
In order to better understand how mucosal immune dysfunction relates to disease progression after HIV/SIV infection we studied immune activation, GI barrier function, mucosal immunity, and microbial translocation in uninfected PTM, SIV-infected PTM who progressed to AIDS, and SIV-infected slow progressor PTM. We found that despite moderate depletion of CD4+ T-cells in slow progressors, these animals had dampened innate immune activation compared to either uninfected PTM or progressors, as measured by the interferon-responsive gene MxA. Furthermore, we found that this decreased innate immune activation was associated with a more intact tight epithelial barrier of the colon compared to progressors, who had significantly more damage to the GI tract. Finally, we found a correlation between microbial translocation pre-infection and at necropsy with the time to AIDS progression. These data suggest the importance of limitation of peripheral immune activation, maintenance of mucosal homeostatic immune subsets, and suppression of microbial translocation in limiting, and possibly predicting, progression to AIDS.
The decreased innate immune activation observed in all tissues in the slow progressors is of interest considering the incomplete understanding of cause versus effect in HIV-infected slow progressors and long-term non-progressors (LTNP). While it is intuitive to suggest that lower virus replication results in decreased immune activation and disease progression in slow progressors, here the finding that SP had lower immune activation than uninfected animals suggests that dampened immune activation pre-infection may play a role in the lack of AIDS progression, and potentially could be itself why viremia is lower in slow progressors. Indeed, HIV preferentially infects activated CD4+ T-cells (35), thus pre-existing lower levels of immune activation may limit the pool of targets for HIV infection, and thus decrease viremia in SP. This is also consistent with the moderate CD4+ T-cell depletion we observed in mucosal tissues in SP, which also occurs in natural host non-progressive SIV infection (25, 26, 36), without inducing local activation or microbial translocation. Slow progressors also had decreased damage to the tight epithelial barrier in the colon compared to progressors and uninfected PTM, further supporting that pre-infection mucosal factors may, in part, underlie lack of progression, and that these observations are not the result of decreased virus alone.
The role of the somewhat protective ManeA1*084 allele here is unclear. While all of the slow progressors possessed this allele, several SIV− and SIV+ progressors were also ManeA1*084+, with no protective effects. Thus, the importance of this allele in slow progression, and whether ManeA1*084 plays a role in mucosal immunity, needs to be further investigated. Furthermore, another caveat of these data is the comparison of healthy animals to those progressed to AIDS, with opportunistic infections and poor health. While comparing animals that have progressed to AIDS to uninfected animals or to slow progressors has the potential to confound the conclusions, the clear trend for increased GI dysfunction, even prior to SIV infection, indicates that the results are not compromised by the presence of opportunistic infections.
Interestingly, uninfected and progressively infected animals demonstrated similarly high amounts of immune activation in the GI tract; however, elevated innate immune activation in the axillary LN was only observed in progressively infected animals. Systemic immune activation in HIV/SIV infections is multifaceted, though it has been demonstrated that one factor which contributes to systemic activation is microbial translocation (9, 15). Indeed, our finding that damage to the colonic epithelium in infected animals closely correlated with the amount of both local and peripheral innate immune activation suggests that local damage to the GI tract can result in systemic microbial translocation in the context of SIV infection. Furthermore, this indicates that damage to the GI tract and local microbial translocation in the lamina propria may be the first break down of this chain of events, and that dysfunctional gastrointestinal immunity after infection results in reduced microbial immune responses and microbial clearance, leading to systemic microbial translocation and immune activation during SIV infection.
Our finding that levels of microbial translocation at death correlated with AIDS progression supports the role of microbial translocation in contributing to disease progression and mortality in HIV infection (37). However, we extend on this premise with our evidence showing a direct relationship between pre-infection levels of microbial translocation and AIDS progression. Indeed, it has been demonstrated that PTM have greater levels of microbial translocation in the absence of SIV infection and that they progress faster than models such as RM who have less inherent microbial translocation (15). This direct association may point to an important role for monitoring plasma bacterial products and/or serum proteins expressed in response to microbial products (i.e. LBP) in uninfected animals to ascertain the susceptibility and rate to disease progression in SIV infection. Given our small sample size, future studies are warranted to assess the strength of pre-infection microbial translocation as a predictor of AIDS progression in larger cohorts. Indeed, ascertaining pre-existing levels of microbial products in non-human primate studies may be an ideal and informative opportunity in vaccination and pre-exposure prophylaxis experiments to further determine the role of pre-existing GI damage and disease progression in addition to its potential role in acquisition given that microbial translocation increases T-cell activation at mucosal sites.
Here, we have characterized SIV infection in mucosal tissues of PTM and have found that GI tract immune subsets may have a role in limiting microbial translocation and systemic activation, and that pre-infection microbial translocation is associated with disease progression upon SIV infection. The observations in this study point to key factors to be explored in the mucosal immunology of SIV infection. Importantly, our study highlights the benefit of using PTM to elucidate key factors in progression, as we have seen here that factors causing pathology in uninfected PTM, such as local immune activation and damage to the barrier of the colon, are not sufficient in and of themselves to cause the levels of systemic activation observed in SIV-infected PTM. Rather, the underlying innate immune activation and GI damage may be potentiated by mucosal immune dysfunction caused by infection, which predicts progression. Indeed, the pre-existing GI immune activation may make PTM a better model for mucosal immunology studies in the context of heightened immune activation and/or GI enteropathies that exist in areas with high prevalence of HIV such as sub-Saharan Africa (38, 39). Understanding how SIV infected slow progressor PTM prevent systemic immune activation may allow for better treatment regimens, especially considering that in HIV-infected, HAART treated individuals, morbidity and mortality is associated with systemic immune activation and microbial translocation (37, 40–42). Furthermore, these data point to the GI tract as an essential target for therapies, such as probiotics, aimed to support GI tract physiology and suppress microbial translocation.
Supplementary Material
Acknowledgments
We would like to acknowledge Heather Cronise, JoAnne Swerczek, Richard Herbert, and all the veterinary staff at the NIH animal center. We would like to thank Dr. Vanessa Hirsch for assistance in diagnosing AIDS pathologies. We would like to thank the Cleveland Immunopathogenesis Consortium (BBC/CLIC) for advice and helpful discussions. We would like to thank NIH Nonhuman Primate Reagent Resource at Beth Israel Deaconess Medical Center for providing non-commercially available cross-reactive antibodies. We would like to acknowledge the Pathology/Histotechnology Laboratory (PHL) for histology support located at the Frederick National Laboratory for Cancer Research, Frederick, MD, USA. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
This project has been funded in part with federal funds from the National Cancer Institute, National Institutes of Health, under Contract No. HHSN261200800001E.
References
- 1.Brenchley JM, Douek DC. HIV infection and the gastrointestinal immune system. Mucosal Immunol. 2008;1:23–30. doi: 10.1038/mi.2007.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lackner AA, Mohan M, Veazey RS. The gastrointestinal tract and AIDS pathogenesis. Gastroenterology. 2009;136:1965–1978. doi: 10.1053/j.gastro.2008.12.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Estes JD, Harris LD, Klatt NR, Tabb B, Pittaluga S, Paiardini M, Barclay GR, Smedley J, Pung R, Oliveira KM, Hirsch VM, Silvestri G, Douek DC, Miller CJ, Haase AT, Lifson J, Brenchley JM. Damaged Intestinal Epithelial Integrity Linked to Microbial Translocation in Pathogenic Simian Immunodeficiency Virus Infections. PLoS Pathog. 2010;6:e1001052. doi: 10.1371/journal.ppat.1001052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nazli A, Chan O, Dobson-Belaire WN, Ouellet M, Tremblay MJ, Gray-Owen SD, Arsenault AL, Kaushic C. Exposure to HIV-1 Directly Impairs Mucosal Epithelial Barrier Integrity Allowing Microbial Translocation. PLoS Pathog. 2010;6:e1000852. doi: 10.1371/journal.ppat.1000852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mattapallil JJ, Douek DC, Hill B, Nishimura Y, Martin M, Roederer M. Massive infection and loss of memory CD4+ T cells in multiple tissues during acute SIV infection. Nature. 2005;434:1093–1097. doi: 10.1038/nature03501. [DOI] [PubMed] [Google Scholar]
- 6.Klatt NR, Estes JD, Sun X, Ortiz AM, Barber JS, Harris LD, Cervasi B, Yokomizo LK, Pan L, Vinton CL, Tabb B, Canary LA, Dang Q, Hirsch VM, Alter G, Belkaid Y, Lifson JD, Silvestri G, Milner JD, Paiardini M, Haddad EK, Brenchley JM. Loss of mucosal CD103+ DCs and IL-17+ and IL-22+ lymphocytes is associated with mucosal damage in SIV infection. Mucosal Immunol. 2012 doi: 10.1038/mi.2012.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Veazey RS, DeMaria M, Chalifoux LV, Shvetz DE, Pauley DR, Knight HL, Rosenzweig M, Johnson RP, Desrosiers RC, Lackner AA. Gastrointestinal Tract as a Major Site of CD4+ T Cell Depletion and Viral Replication in SIV Infection. Science. 1998;280:427–431. doi: 10.1126/science.280.5362.427. [DOI] [PubMed] [Google Scholar]
- 8.Mohan M, Kaushal D, Aye PP, Alvarez X, Veazey RS, Lackner AA. Focused examination of the intestinal lamina propria yields greater molecular insight into mechanisms underlying SIV induced immune dysfunction. PLoS One. 2012;7:e34561. doi: 10.1371/journal.pone.0034561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S, Kazzaz Z, Bornstein E, Lambotte O, Altmann D, Blazar BR, Rodriguez B, Teixeira-Johnson L, Landay A, Martin JN, Hecht FM, Picker LJ, Lederman MM, Deeks SG, Douek DC. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006;12:1365–1371. doi: 10.1038/nm1511. [DOI] [PubMed] [Google Scholar]
- 10.Pandrea I, Cornell E, Wilson C, Ribeiro RM, Ma D, Kristoff J, Xu C, Haret-Richter GS, Trichel A, Apetrei C, Landay A, Tracy R. Coagulation biomarkers predict disease progression in SIV-infected nonhuman primates. Blood. 2012 doi: 10.1182/blood-2012-03-414706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brenchley JM, Price DA, Douek DC. HIV disease: fallout from a mucosal catastrophe? Nat Immunol. 2006;7:235–239. doi: 10.1038/ni1316. [DOI] [PubMed] [Google Scholar]
- 12.Giorgi JV, Hultin LE, McKeating JA, Johnson TD, Owens B, Jacobson LP, Shih R, Lewis J, Wiley DJ, Phair JP, Wolinsky SM, Detels R. Shorter survival in advanced human immunodeficiency virus type 1 infection is more closely associated with T lymphocyte activation than with plasma virus burden or virus chemokine coreceptor usage. J Infect Dis. 1999;179:859–870. doi: 10.1086/314660. [DOI] [PubMed] [Google Scholar]
- 13.Sousa AE, Carneiro J, Meier-Schellersheim M, Grossman Z, Victorino RM. CD4 T cell depletion is linked directly to immune activation in the pathogenesis of HIV-1 and HIV-2 but only indirectly to the viral load. J Immunol. 2002;169:3400–3406. doi: 10.4049/jimmunol.169.6.3400. [DOI] [PubMed] [Google Scholar]
- 14.Hunt PW, Brenchley J, Sinclair E, McCune JM, Roland M, Page-Shafer K, Hsue P, Emu B, Krone M, Lampiris H, Douek D, Martin JN, Deeks SG. Relationship between T cell activation and CD4+ T cell count in HIV-seropositive individuals with undetectable plasma HIV RNA levels in the absence of therapy. J Infect Dis. 2008;197:126–133. doi: 10.1086/524143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klatt NR, Harris LD, Vinton CL, Sung H, Briant JA, Tabb B, Morcock D, McGinty JW, Lifson JD, Lafont BA, Martin MA, Levine AD, Estes JD, Brenchley JM. Compromised gastrointestinal integrity in pigtail macaques is associated with increased microbial translocation, immune activation, and IL-17 production in the absence of SIV infection. Mucosal Immunol. 2010;3:387–398. doi: 10.1038/mi.2010.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klatt NR, Canary LA, Vanderford TH, Vinton CL, Engram JC, Dunham RM, Cronise HE, Swerczek JM, Lafont BA, Picker LJ, Silvestri G, Brenchley JM. Dynamics of simian immunodeficiency virus SIVmac239 infection in pigtail macaques. J Virol. 2011;86:1203–1213. doi: 10.1128/JVI.06033-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Batten CJ, De Rose R, Wilson KM, Agy MB, Chea S, Stratov I, Montefiori DC, Kent SJ. Comparative evaluation of simian, simian-human, and human immunodeficiency virus infections in the pigtail macaque (Macaca nemestrina) model. AIDS Res Hum Retroviruses. 2006;22:580–588. doi: 10.1089/aid.2006.22.580. [DOI] [PubMed] [Google Scholar]
- 18.Mason RD, Rose RD, Seddiki N, Kelleher AD, Kent SJ. Low pre-infection levels and loss of central memory CD4+ T cells may predict rapid progression in SIV-infected pigtail macaques. Virology. 2008;381:11–15. doi: 10.1016/j.virol.2008.08.042. [DOI] [PubMed] [Google Scholar]
- 19.Alcantara S, Reece J, Amarasena T, Rose RD, Manitta J, Amin J, Kent SJ. Thrombocytopenia is strongly associated with simian AIDS in pigtail macaques. J Acquir Immune Defic Syndr. 2009;51:374–379. doi: 10.1097/QAI.0b013e3181a9cbcf. [DOI] [PubMed] [Google Scholar]
- 20.Kubo M, Nishimura Y, Shingai M, Lee W, Brenchley J, Lafont B, Buckler-White A, Igarashi T, Martin MA. Initiation of antiretroviral therapy 48 hours after infection with simian immunodeficiency virus potently suppresses acute-phase viremia and blocks the massive loss of memory CD4+ T cells but fails to prevent disease. J Virol. 2009;83:7099–7108. doi: 10.1128/JVI.02522-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Estes JD, Gordon SN, Zeng M, Chahroudi AM, Dunham RM, Staprans SI, Reilly CS, Silvestri G, Haase AT. Early resolution of acute immune activation and induction of PD-1 in SIV-infected sooty mangabeys distinguishes nonpathogenic from pathogenic infection in rhesus macaques. J Immunol. 2008;180:6798–6807. doi: 10.4049/jimmunol.180.10.6798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Douek DC, Picker LJ, Koup RA. T cell dynamics in HIV-1 infection. Annu Rev Immunol. 2003;21:265–304. doi: 10.1146/annurev.immunol.21.120601.141053. [DOI] [PubMed] [Google Scholar]
- 23.Brenchley JM, Schacker TW, Ruff LE, Price DA, Taylor JH, Beilman GJ, Nguyen PL, Khoruts A, Larson M, Haase AT, Douek DC. CD4+ T Cell Depletion during all Stages of HIV Disease Occurs Predominantly in the Gastrointestinal Tract. J Exp Med. 2004;200:749–759. doi: 10.1084/jem.20040874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenberg ZF, Fauci AS. The immunopathogenesis of HIV infection. Adv Immunol. 1989;47:377–431. doi: 10.1016/s0065-2776(08)60665-3. [DOI] [PubMed] [Google Scholar]
- 25.Gordon SN, Klatt NR, Bosinger SE, Brenchley JM, Milush JM, Engram JC, Dunham RM, Paiardini M, Klucking S, Danesh A, Strobert EA, Apetrei C, Pandrea IV, Kelvin D, Douek DC, Staprans SI, Sodora DL, Silvestri G. Severe depletion of mucosal CD4+ T cells in AIDS-free simian immunodeficiency virus-infected sooty mangabeys. J Immunol. 2007;179:3026–3034. doi: 10.4049/jimmunol.179.5.3026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pandrea IV, Gautam R, Ribeiro RM, Brenchley JM, Butler IF, Pattison M, Rasmussen T, Marx PA, Silvestri G, Lackner AA, Perelson AS, Douek DC, Veazey RS, Apetrei C. Acute Loss of Intestinal CD4+ T Cells Is Not Predictive of Simian Immunodeficiency Virus Virulence. J Immunol. 2007;179:3035–3046. doi: 10.4049/jimmunol.179.5.3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pandrea I, Sodora DL, Silvestri G, Apetrei C. Into the wild: simian immunodeficiency virus (SIV) infection in natural hosts. Trends Immunol. 2008;29:419– 428. doi: 10.1016/j.it.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Klatt NR, Brenchley JM. Th17 cell dynamics in HIV infection. Curr Opin HIV AIDS. 2010;5:135–140. doi: 10.1097/COH.0b013e3283364846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu H, Wang X, Liu DX, Moroney-Rasmussen T, Lackner AA, Veazey RS. IL-17-producing innate lymphoid cells are restricted to mucosal tissues and are depleted in SIV-infected macaques. Mucosal Immunol. 2012 doi: 10.1038/mi.2012.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reeves RK, Rajakumar PA, Evans TI, Connole M, Gillis J, Wong FE, Kuzmichev YV, Carville A, Johnson RP. Gut inflammation and indoleamine deoxygenase inhibit IL-17 production and promote cytotoxic potential in NKp44+ mucosal NK cells during SIV infection. Blood. 2011 doi: 10.1182/blood-2011-04-347260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jaensson-Gyllenback E, Kotarsky K, Zapata F, Persson EK, Gundersen TE, Blomhoff R, Agace WW. Bile retinoids imprint intestinal CD103+ dendritic cells with the ability to generate gut-tropic T cells. Mucosal Immunol. 2010 doi: 10.1038/mi.2010.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ronni T, Sareneva T, Pirhonen J, Julkunen I. Activation of IFN-alpha, IFN-gamma, MxA, and IFN regulatory factor 1 genes in influenza A virus-infected human peripheral blood mononuclear cells. J Immunol. 1995;154:2764–2774. [PubMed] [Google Scholar]
- 33.Lichtfuss GF, Hoy J, Rajasuriar R, Kramski M, Crowe SM, Lewin SR. Biomarkers of immune dysfunction following combination antiretroviral therapy for HIV infection. Biomark Med. 2011;5:171–186. doi: 10.2217/bmm.11.15. [DOI] [PubMed] [Google Scholar]
- 34.Leinert C, Stahl-Hennig C, Ecker A, Schneider T, Fuchs D, Sauermann U, Sopper S. Microbial translocation in simian immunodeficiency virus (SIV)-infected rhesus monkeys (Macaca mulatta) J Med Primatol. 2010;39:243–251. doi: 10.1111/j.1600-0684.2010.00429.x. [DOI] [PubMed] [Google Scholar]
- 35.Douek DC, Brenchley JM, Betts MR, Ambrozak DR, Hill BJ, Okamoto Y, Casazza JP, Kuruppu J, Kunstman K, Wolinsky S, Grossman Z, Dybul M, Oxenius A, Price DA, Connors M, Koup RA. HIV preferentially infects HIV-specific CD4+ T cells. Nature. 2002;417:95–98. doi: 10.1038/417095a. [DOI] [PubMed] [Google Scholar]
- 36.Paiardini M, Pandrea I, Apetrei C, Silvestri G. Lessons Learned from the Natural Hosts of HIV-Related Viruses. Annual Review of Medicine. 2009;60:485–495. doi: 10.1146/annurev.med.60.041807.123753. [DOI] [PubMed] [Google Scholar]
- 37.Sandler NG, Wand H, Roque A, Law M, Nason MC, Nixon DE, Pedersen C, Ruxrungtham K, Lewin SR, Emery S, Neaton JD, Brenchley JM, Deeks SG, Sereti I, Douek DC. Plasma levels of soluble CD14 independently predict mortality in HIV infection. J Infect Dis. 2011;203:780–790. doi: 10.1093/infdis/jiq118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rizzardini G, Trabattoni D, Saresella M, Piconi S, Lukwiya M, Declich S, Fabiani M, Ferrante P, Clerici M. Immune activation in HIV-infected African individuals. Italian-Ugandan AIDS cooperation program. AIDS. 1998;12:2387–2396. doi: 10.1097/00002030-199818000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Clerici M, Butto S, Lukwiya M, Saresella M, Declich S, Trabattoni D, Pastori C, Piconi S, Fracasso C, Fabiani M, Ferrante P, Rizzardini G, Lopalco L. Immune activation in africa is environmentally-driven and is associated with upregulation of CCR5. Italian-Ugandan AIDS Project. AIDS. 2000;14:2083–2092. doi: 10.1097/00002030-200009290-00003. [DOI] [PubMed] [Google Scholar]
- 40.Kuller LH, Tracy R, Belloso W, De Wit S, Drummond F, Lane HC, Ledergerber B, Lundgren J, Neuhaus J, Nixon D, Paton NI, Neaton JD. Inflammatory and coagulation biomarkers and mortality in patients with HIV infection. PLoS Med. 2008;5:e203. doi: 10.1371/journal.pmed.0050203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rodger AJ, Fox Z, Lundgren JD, Kuller LH, Boesecke C, Gey D, Skoutelis A, Goetz MB, Phillips AN. Activation and coagulation biomarkers are independent predictors of the development of opportunistic disease in patients with HIV infection. J Infect Dis. 2009;200:973–983. doi: 10.1086/605447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jiang W, Lederman MM, Hunt P, Sieg SF, Haley K, Rodriguez B, Landay A, Martin J, Sinclair E, Asher AI, Deeks SG, Douek DC, Brenchley JM. Plasma levels of bacterial DNA correlate with immune activation and the magnitude of immune restoration in persons with antiretroviral-Treated HIV infection. J Infect Dis. 2009;199:1177–1185. doi: 10.1086/597476. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.