Abstract
Importance
Despite the national goal to reduce catheter-associated urinary tract infection (CAUTI) by 25% by 2013, limited data exist describing prevention practices for CAUTI in US hospitals and none tie national practice use to CAUTI-specific standardized infection ratios (SIRs).
Objective
To identify practices currently used to prevent CAUTI and to compare use and SIRs for a national sample of US hospitals with hospitals in the state of Michigan, which launched a CAUTI prevention initiative in 2007 (“Keystone Bladder Bundle Initiative”).
Design and setting
In 2009, we surveyed infection preventionists at a sample of US hospitals and all Michigan hospitals. CAUTI rate differences between Michigan and non-Michigan hospitals were assessed using SIRs.
Participants
470 infection preventionists.
Main Outcome Measures
Reported regular use of CAUTI prevention practices and CAUTI specific SIRs.
Results
Michigan hospitals, compared with hospitals in the rest of the United States, more frequently participated in collaboratives to reduce healthcare-associated infection (94% vs. 67%, p < 0.001), and used bladder scanners (53% vs. 39%, p = 0.04), as well as catheter reminders or stop-orders and/or nurse-initiated discontinuation (44% vs. 23%, p < 0.001). More frequent use of preventive practices coincided with a 25% reduction in CAUTI rates in the state of Michigan, a significantly greater reduction than the 6% overall decrease observed in the rest of the United States.
Conclusions and Relevance
We observed more frequent use of key prevention practices and a lower rate of CAUTI in Michigan hospitals relative to non-Michigan hospitals. This may be related to Michigan’s significantly higher use of practices aimed at timely removal of urinary catheters, the key focus area of Michigan’s Keystone Bladder Bundle Initiative.
Background
Preventing healthcare-associated infection (HAI) has emerged as a key focal point for improving the safety of hospitalized patients.1–3 Indeed, as of 1 October 2008, the Centers for Medicare and Medicaid Services (CMS) decided to no longer reimburse hospitals for the additional costs of caring for patients who develop certain preventable infections during hospitalization.4–6 The first hospital-acquired condition chosen for non-payment was catheter-associated urinary tract infection (CAUTI),7 which is one of the most common HAIs in the United States8–10 The CMS chose CAUTI in part because it is considered “reasonably preventable.”7 A key premise underlying this CMS policy is that there are evidence-based practices and multimodal prevention strategies that hospitals can take to reduce their CAUTI rates.5
We have previously shown that in 2005 US hospitals did not have a dominant strategy for preventing CAUTI.11 Although more recent data indicate that the use of various practices to prevent three of the most common HAIs – central line-associated bloodstream infection, ventilator-associated pneumonia, and CAUTI – has increased between 2005 and 2009, none of the practices to prevent CAUTI were used by more than half of US, non-federal hospitals in 2009.12 A recent study by Conway and colleagues also revealed that adoption of policies to prevent CAUTI in intensive care units (ICUs) is lacking, with only 42% of ICUs reporting having written policies in place for at least 1 of 4 prevention practices: use of portable bladder ultrasound scanners, condom catheters for men, urinary catheter reminders or stop-orders, or nurse-initiated urinary catheter discontinuation.13
Prior to implementation of the CMS no-payment policy, there was only one statewide initiative focused on urinary catheters and CAUTI prevention. In 2007, modeled after a successful multimodal intervention to prevent central line-associated bloodstream infection,14 the Michigan Health & Hospital Association’s Keystone Center launched a statewide initiative known as the “Keystone Bladder Bundle Initiative” to reduce CAUTI.15 This initiative consisted of the following key practices to reduce CAUTI: urinary catheter reminders or removal prompts and nurse-initiated urinary catheter discontinuation protocols; alternatives to indwelling urinary catheterization; portable bladder ultrasound monitoring; and insertion care and maintenance. Although urinary catheter use seemed to decrease by approximately 30% among Michigan hospitals participating in this initiative,16 the specific types of CAUTI prevention practices used, and whether there was a difference in practice use between Michigan and non-Michigan hospitals have not been assessed. Whether CAUTI rates were affected by this initiative is also unknown. Our objective was to use this natural experiment to examine these issues and thereby inform national stakeholders and policymakers in their ongoing efforts to reduce CAUTI.
Methods
Study Design and Data Collection
We conducted a survey to compare the use of specific infection prevention practices by US hospitals. In March 2009, we mailed surveys to infection preventionists at a national random sample of hospitals in the United States. The study sample had been originally derived for a similar survey study conducted in 2005.11,17,18 Specifically, we identified all non-federal, general medical and surgical hospitals with an intensive care unit (ICU) and at least 50 hospital beds using the 2005 American Hospital Association (AHA) Database™ (fiscal year 2003 data). We then stratified hospitals into 2 bed size groups (50–250 beds and ≥ 251 beds), and selected a random sample of 300 hospitals from each group. The 2009 survey was sent to the same hospitals sampled in 2005 with a few exceptions due to closure or merger between the longitudinal survey time points. In addition, we included all hospitals in the state of Michigan. Updated information about hospital bed size was obtained from the 2007 AHA Database and because the original sample had only included hospitals with more than 50 beds, to ensure greater comparability between Michigan and non-Michigan hospitals, we excluded Michigan hospitals with bed size less than 50.
Study Measures
The survey instrument, which has been previously described,11, 17, 18 included questions about the following: facility characteristics, the infection control program, infection preventionists, and frequency of use for hospital practices related to prevention and monitoring of CAUTI and other device-associated infections. Responses about the frequency of use of practices to prevent CAUTI were assigned values between 1 (never) and 5 (always). We defined responses of 4 (almost always) or 5 (always) as regular use of the respective prevention practice. All prevention practices examined were dichotomized into binary dependent variables, with regular use (as defined earlier) coded as 1 and 0 otherwise. The “Michigan” variable was modeled as a dichotomous variable with Michigan hospitals coded as 1 and serves as an independent proxy variable for the Keystone Bladder Bundle Initiative,15 which was implemented in 52% of all acute care hospitals in Michigan. The safety culture score was defined as the average of responses regarding agreement to two statements about safety (“Leadership is driving us to be a safety-centered institution” and “I would feel safe being treated here as a patient”). Each of these survey items were scored from 1 (“Strongly Agree”) to 5 (“Strongly Disagree”) and prior to averaging the responses we reverse-scored them, so a higher score indicated greater safety-centeredness.
Because we were interested in investigating the associations between process and outcome measures, we partnered with the Centers for Disease Control and Prevention and the Michigan Department of Community Health to derive 2010 standardized infection ratio (SIR) estimates for CAUTI that were aggregated to the state-level. SIR is calculated by dividing the total number of observed infection events for a given population by an expected number of infection events for that population. SIR is similar in concept to standardized mortality ratios, indirectly standardizing expected values using rates from a standard population, and is a practical risk-adjustment statistic for comparing HAI rates.19, 20 For estimating the 2010 CAUTI SIR, the 2009 National Healthcare Safety Network (NHSN) CAUTI rates were used as the standard. Through our partnerships with Centers for Disease Control and Prevention and the Michigan Department of Community Health, we received data that compared the aggregate SIR specific to Michigan hospitals to the aggregate SIR for non-Michigan hospitals. The identities of all hospitals used to derive SIR estimates were kept confidential from our study team.
Statistical Analysis
We used χ2 estimates from 2-sample tests of equality of proportions to determine statistical significance between the reported regular use of infection prevention practices and hospital characteristics in Michigan vs. non-Michigan hospitals in 2009. We used logistic regression to examine multivariable associations between hospital characteristics and the use of the various infection prevention practices. To compare reductions in CAUTI rates in Michigan versus those in the rest of the United States, we compared SIRs that were specific to Michigan to those that were estimated for all other states and examined the respective SIR 95% confidence intervals to assess the degree of overlap and statistical difference. Reported P-values are two-tailed; all analyses were conducted using Stata version 11.0 (Stata Corp LP).
Results
The overall survey response rate was 71%. The survey was sent to 131 Michigan hospitals and 79% responded. Of the 566 non-Michigan hospitals that were sent the survey, 69% responded. Of the 103 Michigan hospitals that responded, 25 had hospital bed size less than 50 and were removed from our analyses. Our final analytic study sample included 78 Michigan hospitals, 64% of which reported participating in the Keystone Bladder Bundle Initiative, and 392 non-Michigan hospitals. Almost all Michigan hospitals were participating in a collaborative effort to prevent HAI, and the overall percentage of collaborative participants in Michigan was greater than in non-Michigan hospitals (94% vs. 67%, p < 0.001). Table 1 compares Michigan and non-Michigan hospitals across a number of characteristics. Several statistically significant differences were noted. Michigan hospitals were more likely to routinely monitor duration and/or discontinuation of urinary catheters (60% vs. 39%, p < 0.001), while non-Michigan hospitals were more likely to have an established system to monitor urinary tract infection rates (59% vs. 79%, p < 0.001).
Table 1.
Characteristics of Responding Hospitals -Michigan Vs. Non-Michigan
| Characteristic | Michigan hospitals (n =78) | Non-Michigan hospitals (n = 392) | P-value |
|---|---|---|---|
| Hospital bed size >=250 | 33% | 45% | 0.07 |
| Has hospitalists | 68% | 77% | 0.11 |
| Lead infection preventionist certified in infection control | 54% | 64% | 0.14 |
| Has system in place to monitor urinary catheter placement | 59% | 57% | 0.83 |
| Routinely monitors duration and/or discontinuation of urinary catheters | 60% | 39% | <0.001 |
| Has an established surveillance system for monitoring urinary tract infection rates | 59% | 79% | <0.001 |
| Regular use of alcohol-based hand rub for general infection prevention* | 90% | 95% | 0.17 |
| Leadership driving for a safety-centered institution*a | 82% | 77% | 0.38 |
| Would feel safe being treated at their respective institution*a | 72% | 77% | 0.40 |
| Strong to very strong perceived importance of urinary tract infection prevention* | 63% | 58% | 0.52 |
| Moderate to large increase in importance of urinary tract infection prevention as a result of the CMS rule change* | 64% | 65% | 1.00 |
As reported by each institution’s lead infection preventionist.
Survey questions were on a 5-point scale ranging from strongly disagree to strongly agree. “Agree” (4) and “Strongly agree” (5) responses are reflected in the table percentages.
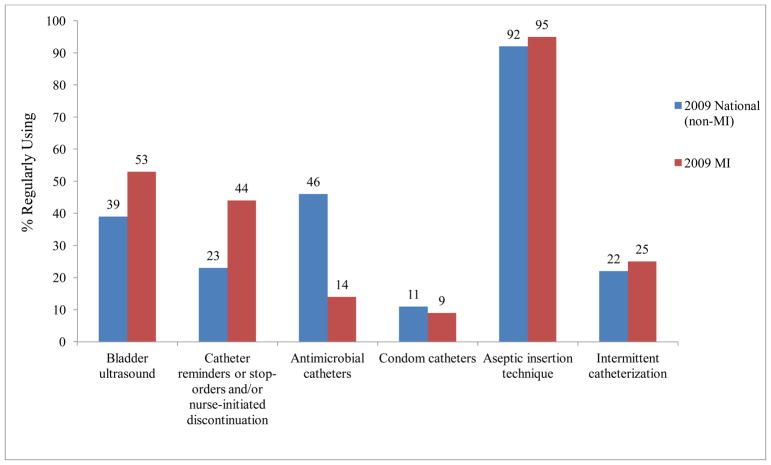
Figure 1 shows the distribution of the CAUTI prevention practices in Michigan and non-Michigan hospitals. Michigan hospitals were more likely than non-Michigan hospitals to use portable bladder scanners (53% vs. 39%, p = 0.04) as well as catheter reminders or stop-orders and/or nurse-initiated discontinuation (44% vs. 23%, p < 0.001); conversely, non-Michigan hospitals were more likely to use antimicrobial urinary catheters (14% vs. 46%, p < 0.001).
Figure 1.
Cauti Prevention Practices -Michigan Vs. Non-Michigan
Table 2 summarizes the results of multivariable logistic regression analyses assessing the association between our independent variables of interest and the use of CAUTI preventive practices. The odds of regularly using bladder ultrasound scanners, as well as urinary catheter reminders or stop-orders and/or nurse-initiated discontinuation, were 2-fold greater in hospitals located in Michigan (p = 0.01 and p = 0.007, respectively). Having systems in place to routinely monitor urinary catheter placement (p = 0.02), and urinary catheter duration and/or discontinuation (p < 0.001), as well as the perception that urinary tract infection prevention is an important institutional goal (p = 0.04), were also all associated with approximately 2- to 3-fold increases in the odds of regularly using urinary catheter reminders or stop-orders and/or nurse-initiated discontinuation. Conversely, the odds of regularly using antimicrobial urinary catheters were significantly higher among non-Michigan hospitals (p < 0.001).
Table 2.
Odds Ratios for Regular Use* of Cauti Prevention Practices
| Portable bladder ultrasound scanner | Urinary catheter reminders or stop-orders and/or nurse-initiated discontinuation | Antimicrobial urinary catheters | Condom catheters in men | Aseptic insertion technique | Intermittent catheterization | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Michigan | 2.02 | 1.18–3.43 | 2.19 | 1.24–3.86 | 0.18 | 0.09–0.36 | 1.10 | 0.45–2.66 | 1.93 | 0.56–6.60 | 1.32 | 0.71–2.45 |
| Has hospitalists | 1.55 | 0.96–2.50 | 0.93 | 0.54 – 1.59 | 1.21 | 0.75–1.96 | 1.13 | 0.51–2.51 | 1.20 | 0.47–3.06 | 1.67 | 0.94–2.99 |
| IP certified in infection control | 1.29 | 0.84–1.98 | 1.08 | 0.65 – 1.79 | 1.14 | 0.74–1.75 | 1.58 | 0.75–3.30 | 1.42 | 0.63–3.20 | 0.97 | 0.59–1.60 |
| Strong support from leadership for infection control | 0.91 | 0.55–1.50 | 1.09 | 0.59 – 2.03 | 0.99 | 0.59–1.65 | 0.73 | 0.33–1.64 | 0.71 | 0.28–1.83 | 1.04 | 0.57–1.89 |
| Monitoring urinary catheter placement | 1.24 | 0.80–1.93 | 1.98 | 1.14 – 3.44 | 0.85 | 0.55–1.33 | 1.44 | 0.71–2.95 | 1.60 | 0.70–3.70 | 2.09 | 1.22–3.57 |
| Monitoring urinary catheter duration | 0.80 | 0.51–1.25 | 3.13 | 1.88 – 5.22 | 1.42 | 0.91–2.21 | 0.81 | 0.40–1.63 | 1.57 | 0.62–4.00 | 0.86 | 0.51–1.44 |
| Safety culture score** | 1.06 | 0.76–1.48 | 1.29 | 0.86 – 1.95 | 1.19 | 0.85–1.68 | 0.88 | 0.51–1.54 | 2.00 | 1.06–3.78 | 0.92 | 0.62–1.35 |
| Effect of CMS rule change | 1.25 | 0.80–1.95 | 1.14 | 0.68 – 1.94 | 1.19 | 0.77–1.86 | 1.98 | 0.89–4.38 | 0.58 | 0.25–1.37 | 0.92 | 0.55–1.54 |
| Importance of UTI prevention | 0.80 | 0.51–1.28 | 1.82 | 1.04 – 3.18 | 1.09 | 0.69–1.74 | 1.32 | 0.62–2.80 | 2.00 | 0.83–4.81 | 0.96 | 0.56–1.64 |
| Alcohol based hand rub | 1.46 | 0.64–3.37 | 0.87 | 0.31 – 2.42 | 1.49 | 0.61–3.67 | 1.07 | 0.29–3.96 | 4.39 | 1.52–12.68 | 4.59 | 1.04–20.21 |
| ≥ 250 beds | 0.76 | 0.50 – 1.17 | 0.70 | 0.42 – 1.16 | 1.22 | 0.80–1.87 | 1.91 | 0.97–3.77 | 0.71 | 0.30–1.69 | 0.92 | 0.56–1.51 |
Regular use was defined as receiving a rating of 4 or 5 on a on a scale from 1–5 (with 1 being never and 5 being always) indicating the practice is used always or almost always.
The safety culture score was defined as the average of responses regarding agreement to two statements about safety: “Leadership is driving us to be a safety-centered institution” and “I would feel safe being treated here as a patient”. Each OR adjusted for all other variables listed in characteristic column of table.
Abbreviations: CAUTI = catheter-associated urinary tract infection; IP= infection preventionist; OR = Odds Ratio; CI = Confidence Interval; CMS = Centers for Medicare and Medicaid Services; UTI = urinary tract infection
Table 3 lists the differences in 2010 CAUTI rates between Michigan and non-Michigan hospitals that reported to NHSN. CAUTI rate data is derived from all wards and ICUs (neonatal ICUs excluded) from the NHSN reporting facilities. The 2010 estimate for the national CAUTI specific SIR with Michigan hospitals excluded was 0.94 (95% CI: 0.92, 0.96), whereas the SIR estimate specific to Michigan was 0.75 (95% CI: 0.63, 0.87). These estimates suggest that CAUTI rates in Michigan hospitals decreased by approximately 25% from 2009 to 2010, while CAUTI rates in hospitals in the rest of the United States (aggregated) decreased by approximately 6% during the same period. Of the 24 Michigan hospitals that reported to NHSN and contributed to the SIR estimate specific to Michigan, 58% were participating in the Keystone Bladder Bundle Initiative (estimate provided by the CDC).
Table 3.
2010 National Healthcare Safety Network Standardized Infection Ratios for Cauti–Michigan Vs. Non-MichiganA
| Number of Infections | |||||
|---|---|---|---|---|---|
| Location | Number of Facilities | Observed | Expected* | SIR | 95% CI |
| National | 1062 | 9,845 | 10,456 | 0.94 | 0.92 – 0.96 |
| Michigan | 24 | 150 | 201 | 0.75 | 0.63 – 0.87 |
Data obtained through cooperation with the Centers for Disease Control and Prevention, National Healthcare Safety Network (NHSN) and the Michigan Department of Community Health. Data presented are derived from facilities reporting to NHSN during 2010 and include data from all ICUs and wards; excludes NICUs.
Expected values are based on indirect standardization to 2009 NHSN catheter-associated urinary tract infection rates.
Abbreviations: CAUTI–catheter-associated urinary tract infection; SIR: standardized infection ratio = Observed/Expected; CI=confidence interval.
Discussion
Several important findings emerged from our national study. First, many hospitals in the United States do not have established systems to routinely monitor the placement nor the duration of urinary catheters in their hospitalized patients, despite the strong link between urinary catheters and subsequent infection. Second, certain practices are being used by a higher percentage of Michigan hospitals compared with those outside Michigan. However, with the exception of aseptic technique for urinary catheter insertion – which was almost universally reported as being used regularly – most infection control practices to prevent CAUTI are used infrequently in US hospitals. Third, despite relatively infrequent use of CAUTI prevention practices overall, we observed significantly lower CAUTI rates among Michigan hospitals compared to non-Michigan hospitals in 2010. A plausible explanation for more frequent use of certain prevention practices within Michigan hospitals is that many hospitals in Michigan participated in the Keystone Bladder Bundle Initiative, a statewide collaborative effort implemented in 2007 to reduce CAUTI by primarily focusing on reducing urinary catheter use.15 The results of our multivariable analyses suggest that participation in the Keystone Bladder Bundle Initiative may have contributed to the increased odds of regular use of portable bladder ultrasound scanners, as well as urinary catheter reminders or stop-orders and/or nurse-initiated catheter discontinuation. Furthermore, the decreased odds of antimicrobial urinary catheter use in Michigan hospitals is consistent with the fact that these particular devices were not included in the recommended bundle of prevention practices that was disseminated through the Keystone Bladder Bundle Initiative.
We have recently reported increases in several CAUTI prevention practices in non-federal and Veterans Affairs hospitals between 2005 and 2009, including a 9% to 20% increase in the use of urinary catheter reminders or stop-orders in non-federal hospitals.12 However, it is notable that the regular use of this particular prevention practice seems much higher among Michigan hospitals. Urinary catheter reminders or stop-orders are straightforward interventions to reduce the use of unnecessary urinary catheters and therefore may reduce the number of CAUTIs. A recent meta-analysis found the use of catheter reminder or stop-order systems led to a 37% reduction in the mean duration of catheterization and a 52% reduction in CAUTI rates.21 Early catheter removal would also help reduce the non-infectious complications of indwelling urinary catheter use such as discomfort and immobility.22
Our study results strengthen other research investigating the effect of the Keystone Bladder Bundle Initiative on reducing urinary catheter prevalence and appropriate indications for catheter use. This research demonstrated that from baseline to the end of year 2 following the intervention, urinary catheter use decreased from 18.1% to 13.8% and the proportion of catheterized patients with appropriate indications increased from 44.3% to 57.6%.16 The current study extends these previous findings by further elucidating how hospitals were able to achieve these results and by highlighting the potential effect on CAUTI rates.
Our study has several limitations. First, since the response rate was less than 100%, our results have some susceptibility to non-response bias. If non-responding hospitals were systematically different from responding hospitals, generalizing results to all US hospitals may be impossible. Second, we relied on self-reported data from the lead infection preventionist at each hospital to determine how frequently the various prevention practices were used. Although an individual respondent may have overstated or understated how frequently the various practices were used, we have no reason to believe this would be a systematic issue. Third, we did not have access to (and thus could not adjust for) patient-level or hospital case-mix data, and our regression estimates could be biased due to unmeasured confounding. Fourth, we were unable to directly explore relationships between the use of the various infection prevention practices and CAUTI outcomes in the specific hospitals surveyed, because most of the participant hospitals were unable to provide CAUTI rate data. Furthermore, we could not directly link the greater CAUTI SIR reduction within Michigan to our findings suggesting greater adoption of certain CAUTI prevention practices in Michigan hospitals. Only slightly more than half of the hospitals in Michigan that reported CAUTI rate data to the NHSN (which was subsequently used to derive the Michigan-specific SIR estimates) were participating in the Keystone Bladder Bundle Initiative. Still, the magnitude of the improvement in CAUTI rates coupled with the overlapping recent success of reducing urinary catheter use within Michigan following the implementation of this statewide initiative16 suggests that adopting and complying with evidenced-based infection prevention practices may help reduce CAUTI. Other structural and safety culture factors apart from elements promoted in the Keystone Bladder Bundle Initiative, however, may also explain the lower CAUTI rates observed in Michigan hospitals. For instance, participation in other general collaborative efforts to reduce HAI may have spill-over effects that independently impact CAUTI rates. Because causal interpretations of our results require strong assumptions, great care should be taken with any generalization or extrapolation.
Limitations notwithstanding, we provide an estimate of the practices US hospitals are using to prevent CAUTI. We also identified several hospital characteristics associated with the use of various CAUTI prevention practices, and how these practices differed between Michigan and non-Michigan hospitals. Furthermore, we found that recent reductions in CAUTI rates among Michigan hospitals were greater than hospitals in the rest of the United States combined, and are on target with the US Department of Health and Human Services goal of reducing CAUTI by 25% by 2013.23 We observed more frequent use of key preventive practices in Michigan hospitals relative to non-Michigan hospitals, particularly practices that were recommended in the Keystone Bladder Bundle Initiative. Thus, participating in collaborative efforts to reduce CAUTI may positively influence the adoption of infection prevention measures, which may subsequently reduce both urinary catheter use and CAUTI rates.
Acknowledgments
Funding/Support: This project was supported by the Blue Cross Blue Shield of Michigan Foundation (to Dr. Saint) and the National Institute of Nursing Research (5 R01 NR010700) (to Drs. Saint and Krein).
We thank Carolyn Gould, MD, MSCR, Scott Fridkin, MD, Jason Snow, PhD, and Paul Malpiedi, MPH of the Centers for Disease Control and Prevention, and Jennie Finks, DVM, MVPH of the Michigan Department of Community Health for their assistance in estimating and providing the standardized infection ratio data reported on in this article.
Footnotes
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Potential Conflicts of Interest: Dr. Saint has received numerous honoraria and speaking fees from academic medical centers, hospitals, group-purchasing organizations (e.g., VHA, Premier), specialty societies, state-based hospital associations and non-profit foundations (e.g., Michigan Health and Hospital Association, Institute for Healthcare Improvement) for lectures about CAUTI and implementation science. Mr. Watson is employed by the Michigan Health and Hospital Association. No other potential conflict of interest is noted.
References
- 1.Burke JP. Patient safety: infection control - a problem for patient safety. N Engl J Med. 2003;348:651–6. doi: 10.1056/NEJMhpr020557. [DOI] [PubMed] [Google Scholar]
- 2.Gerberding JL. Hospital-onset infections: a patient safety issue. Ann Int Med. 2002;137:665–70. doi: 10.7326/0003-4819-137-8-200210150-00011. [DOI] [PubMed] [Google Scholar]
- 3.Saint S, Howell JD, Krein SL. Implementation science: how to jump-start infection prevention. Infect Control Hosp Epidemiol. 2010;31(Suppl 1):S14–7. doi: 10.1086/655991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pronovost PJ, Goeschel CA, Wachter RM. The wisdom and justice of not paying for “preventable complications. JAMA. 2008;299:2197–9. doi: 10.1001/jama.299.18.2197. [DOI] [PubMed] [Google Scholar]
- 5.Saint S, Meddings JA, Calfee DP, Kowalski CP, Krein SL. Catheter-associated urinary tract infection and the Medicare rules changes. Ann Int Med. 2009;150:877–85. doi: 10.7326/0003-4819-150-12-200906160-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wald HL, Kramer AM. Nonpayment for harms resulting from medical care: catheter-associated urinary tract infections. JAMA. 2007;298:2782–4. doi: 10.1001/jama.298.23.2782. [DOI] [PubMed] [Google Scholar]
- 7.Medicare program; changes to the hospital inpatient prospective payment systems and fiscal year 2008 rates. Fed Regist. 2007;72:47129–8175. [PubMed] [Google Scholar]
- 8.Haley RW, Culver DH, White JW, Morgan WM, Emori TG. The nationwide nosocomial infection rate. A new need for vital statistics. Am J Epidemiol. 1985;121:159–67. doi: 10.1093/oxfordjournals.aje.a113988. [DOI] [PubMed] [Google Scholar]
- 9.Haley RW, Hooton TM, Culver DH, Stanley RC, Emori TG, Hardison CD, et al. Nosocomial infections in U.S. hospitals, 1975–1976: estimated frequency by selected characteristics of patients. Am J Med. 1981;70:947–59. doi: 10.1016/0002-9343(81)90561-1. [DOI] [PubMed] [Google Scholar]
- 10.Klevens RM, Edwards JR, Andrus ML, Peterson KD, Dudeck MA, Horan TC. Dialysis Surveillance Report: National Healthcare Safety Network (NHSN)-data summary for 2006. Semin Dial. 2008;21:24–8. doi: 10.1111/j.1525-139X.2007.00379.x. [DOI] [PubMed] [Google Scholar]
- 11.Saint S, Kowalski CP, Kaufman SR, Hofer TP, Kauffman CA, Olmsted RN, et al. Preventing hospital-acquired urinary tract infection in the United States: a national study. Clin Infect Dis. 2008;46:243–50. doi: 10.1086/524662. [DOI] [PubMed] [Google Scholar]
- 12.Krein SL, Kowalski CP, Hofer TP, Saint S. Preventing hospital-acquired infections: A national survey of practices reported by U.S. hospitals in 2005 and 2009. J Gen Intern Med. 2012;27(7):773–79. doi: 10.1007/s11606-011-1935-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conway LJ, Pogorzelska M, Larson E, Stone PW. Adoption of policies to prevent catheter-associated urinary tract infections in United States intensive care units. Am J Infect Control. 2012 doi: 10.1016/j.ajic.2011.09.020. [In Press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU [see comment] N Engl J Med. 2006;355:2725–32. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- 15.Saint S, Olmsted RN, Fakih MG, Kowalski CP, Watson SR, Sales AE, et al. Translating health care-associated urinary tract infection prevention research into practice via the bladder bundle. Jt Comm J Qual Patient Saf. 2009;35:449–55. doi: 10.1016/s1553-7250(09)35062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fakih MG, Watson SR, Greene MT, Kennedy EH, Olmsted RN, Krein SL, et al. Reducing inappropriate urinary catheter use: a statewide effort. Arch Intern Med. 2012;172:255–60. doi: 10.1001/archinternmed.2011.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krein SL, Hofer TP, Kowalski CP, Olmsted RN, Kauffman CA, Forman JH, et al. Use of central venous catheter-related bloodstream infection prevention practices by US hospitals. Mayo Clin Proc. 2007;82:672–8. doi: 10.4065/82.6.672. [DOI] [PubMed] [Google Scholar]
- 18.Krein SL, Kowalski CP, Damschroder L, Forman J, Kaufman SR, Saint S. Preventing ventilator-associated pneumonia in the United States: a multicenter mixed-methods study. Infect Control Hosp Epidemiol. 2008;29:933–40. doi: 10.1086/591455. [DOI] [PubMed] [Google Scholar]
- 19.Gustafson TL. Three uses of the standardized infection ratio (SIR) in infection control. Infect Control Hosp Epidemiol. 2006;27:427–30. doi: 10.1086/503019. [DOI] [PubMed] [Google Scholar]
- 20.National Center for Emerging and Zoonotic Infectious Diseases. [May 2, 2012];National HAI standardized infection ratio (SIR) report. 2010 Jan-Dec; Accessed at http://www.cdc.gov/hai/pdfs/SIR/national-SIR-Report_03_29_2012.pdf on.
- 21.Meddings J, Rogers MAM, Macy M, Saint S. Systematic review and meta-analysis: reminder systems to reduce catheter-associated urinary tract infections and urinary catheter use in hospitalized patients. Clin Infect Dis. 2010;51:550–60. doi: 10.1086/655133. [DOI] [PubMed] [Google Scholar]
- 22.Saint S, Lipsky BA, Goold SD. Indwelling urinary catheters: a one-point restraint? Ann Int Med. 2002;137:125–7. doi: 10.7326/0003-4819-137-2-200207160-00012. [DOI] [PubMed] [Google Scholar]
- 23.U.S. Department of Health and Human Services. [28 February 2012];HHS Action Plan to Prevent Healthcare-Associated Infections. 2009 Accessed at http://www.hhs.gov/ash/initiatives/hai/nationaltargets#cauti on.