Abstract
Unity in Diversity was a randomized controlled trial of a culturally tailored HIV prevention intervention for African American men who have sex with men (AA MSM). The intervention condition was six group-based sessions and one individual session. The control condition was a single-session HIV prevention review. Participants were aged 18 years or older, identified as African American/black race, reported having at least two sex partners in the prior 90 days (at least one of whom must be a male partner), unprotected anal sex with male partner in the prior 90 days and willing to test for HIV. Retention exceeded 95% at 3 month follow-up. Results of multivariate logistic regression analysis adjusting for baseline risk, HIV status and health insurance indicate intervention efficacy in decreasing the number of male sex partners and marginal effects on condom use with male partners and HIV negative/unknown partners. Specifically, intervention condition was associated with increased odds of zero male sex partners (AOR=3.03, 95%CI=1.26–7.28), condom use with male partners (AOR=2.64, 95%CI=0.95–7.36) and HIV negative/unknown status partners (AOR=3.19, 95%CI=0.98–10.38) at follow-up. These results contribute to the limited number of culturally appropriate models of HIV prevention intervention that are urgently needed for African American men who have sex with men to address their persistently high rates of HIV.
Introduction
According to both waves of the National HIV Behavioral Surveillance of men who have sex with men (MSM), racial disparities in HIV prevalence and incidence persist. African American men who have sex with men (AA MSM) experience 2.5 to 4 times the rate of HIV compared to white MSM (Celentano et al., 2005; German et al., 2011; Harawa et al., 2004; Koblin et al., 2000; Voelker, 2008). Research has identified high levels of stigmatization and reluctance to identify as gay or bi-sexual, as well as varying patterns of heterosexual activity and HIV risk disclosure to female partners among AA MSM (Catania et al., 2001; Centers for Disease Control and Prevention, 2003; Jimenez, 2003; Peterson, Bakeman, Blackshear Jr., & Stokes, 2003). A number of studies suggest that diversity within the AA MSM population warrants tailored intervention approaches (Brooks, Rotheram-Borus, Bing, Ayala, & Henry, 2003; Mays, Cochran, & Zamudio, 2004).
Although there has been an increase in effort to develop and test rigorous behavioral interventions tailored to AA MSM the literature on such interventions remains sparse (Johnson et al., 2008; Peterson & Jones, 2009). Three interventions that address cultural issues such as homophobia, racism and norms of masculinity have shown promising results in decreasing HIV risk. The Many Men Many Voices (3MV) was tested with a sample of HIV negative or unknown status men (Wilton et al., 2009). The Bruthas intervention was designed to address the sexual risk behaviors of AA men who have sex with men and women (Operario, Smith, Arnold, & Kegeles, 2010) and D-Up was an adaptation of the popular opinion leader model (Jones et al., 2008).
A social network approach to HIV prevention capitalizes on naturally occurring social influence processes and network structures to promote and maintain behavior change. Few studies have examined the social networks of AA MSM, yet considerations of the network as a source of social norms, support and information is critical ( Carpiano, Kelly, Easterbrook & Parsons, 2011; Williams, Wyatt, Resell, Peterson, & Asuan-O’Brien, 2004). Building from our prior successful social-network oriented HIV prevention interventions (Davey-Rothwell, Tobin, Yang, Sun, & Latkin, 2011; Tobin, Kuramoto, Davey-Rothwell, & Latkin, 2011) we developed the Unity iN Diversity intervention for AA MSM that sought to 1) teach information and skills about HIV risk, 2) establish pro-social norms about HIV testing and condom use, 3) increase proper and consistent condom use 4) improve communication skills for negotiating HIV risk reduction with partners and 5) encourage diffusion of information and skills to individuals’ social network members, The purpose of this study was to evaluate the efficacy of Unity iN Diversity (UND) on participant sexual risk and self-efficacy in communicating about HIV testing and condoms. This study was approved by the Centers for Disease Control and Prevention and Johns Hopkins University Institutional Review Board.
Methods
Study population and recruitment
Recruitment occurred from August 2007 through August 2008 at several different venues including bars, clubs, cafes, restaurants and college campuses. We also utilized print advertisements in city and University-based newspapers and acquired referrals from agencies that provide services to AA MSM. We conducted internet-based recruitment using web-sites that catered to AA MSM (e.g., Gay Black Chat and Adam4Adam).
Screening procedures
Potential participants were screened using a two-step process involving a telephone-based survey followed by an in-person screening visit. The in-person screening entailed a screening survey that was administered using audio computer-assisted self-interview (ACASI) technology (Ghanem, Hutton, Zenilman, Zimba, & Erbelding, 2005; Macalino, Celentano, Latkin, Strathdee, & Vlahov, 2002). The enrollment criteria were being aged 18 years old or older, identifying as African American or black race/ethnicity, having at least two sex partners in the prior 90 days (at least one of whom must be a male partner), having unprotected anal sex with a male partner in the prior 90 days and being willing to take an HIV test. All participants, regardless of eligibility, received $20 for completing the in-person screening visit.
Baseline data collection procedures
Participants provided written informed consent and completed a survey which assessed demographics, sexual risk, and drug use risk behavior using ACASI. A social network inventory survey was administered by a trained research assistant which collected information about the participant’s support network (those who provide emotional, material or health-related support) and drug or sex network. At the end of the baseline visit, participants who self-reported negative or unknown status were tested for HIV antibodies using Oraquick specimen collection testing kits and were provided with HIV pre- and post-test counseling. Preliminary positive results were confirmed using Western blot assays of a serum specimen collected by a trained phlebotomist. Participants who reported sero-positive status were asked to provide documentation such as CD4 or viral load test results or HIV medication. Those who could not provide documentation were tested with the Oraquick kits to confirm their HIV status. Participants received $40 for the baseline.
Randomization
After approximately 12 participants completed the baseline visit, a randomization session was scheduled. At this session, participants names were entered into a computerized program by the Data Manager which assigned individuals to a condition using a two-block design. The first session of the intervention condition and the only session of the control condition were conducted immediately after randomization. The two groups met in separate rooms in the research clinic. The two condition sessions ended at different times to minimize contamination between the conditions.
Intervention development activities and theoretical background
An Intervention Advisory Board (IAB), comprised of advocates and professionals who served the AA MSM community, as well as lay community members, was convened for the purpose of obtaining input for tailoring the intervention. IAB members were recruited using fliers and word-of-mouth referral and met bimonthly to review and discuss proposed activities for the intervention. To underscore that this intervention was designed to be inclusive of all AA MSM regardless of their sexual identities, HIV serostatus or age, the IAB suggested the project name: Unity in Diversity (UND). With the goal of developing an intervention that was flexible, the IAB recommended a framework that allowed AA MSM to focus on important dimensions of their lives.
The intervention consisted of six group sessions which were organized into a rubric of: Taking Care of Self, Relationships, and Community and was informed by a number of behavior change theories (Table 1). Drawing from the Information-Motivation-Behavior Model (Fisher, Fisher, Amico, & Harman, 2006) activities such as viewing videos and group problem-solving discussions sought to increase knowledge about HIV risk and testing and increase motivation to engage in preventive behaviors including HIV testing and asking partners about their HIV status. To capitalize on social influence processes (e.g. Social Network Theory (Latkin, Sherman, & Knowlton, 2003), the intervention was delivered in small group-based sessions which enabled participants to learn from their peers experiences and to establish and promote social norms about condom use and testing. Role-play activities were included so that participants could practice and role-model communication skills. Sessions included numerous opportunities to practice skills to increase condom use self-efficacy (e.g. Social Cognitive Theory; Bandura, 1986) such as an activity where the participants wore alcohol-vision goggles to simulate the challenges to proper condom use while under the influence of drugs and/or alcohol. An individual session was conducted by a facilitator in a private setting and allowed participants to address risk and increase motivation to engage in prevention behaviors. The intervention was standardized and manualized and was delivered by two AA male co-facilitators. Sessions were held twice a week typically in the afternoon (1–3pm) at the research clinic. Randomization resulted in thirteen intervention condition groups with a mean of 6 participants with a range of 4–8 participants. In each session, participants were given an assignment to have a conversation with someone in their social network about the topics discussed in the group session. The purpose of the homework assignment was to provide additional opportunities to practice the skills from the intervention and increase self-efficacy, as well as to share information and skills with others. Participants received $25 for each session that they attended.
Table 1.
Intervention Overview: Content, theoretical components and sample activities
| Session | Objectives | Theoretical Components | Sample Activities |
|---|---|---|---|
| 1: Introduction | To introduce program goals and to increase awareness about HIV and MSM stereotypes and to increase motivation to ask partners their HIV status. | IMB | Group discussion about stereotypes and assumptions about HIV status. |
| 2: Taking Care of Self | To review HIV and STI knowledge. To emphasize importance of knowing HIV status and increase motivation and self-efficacy for HIV testing. |
IMB, SCT | HIV/STI knowledge game; Know your HIV status video. |
| 3: Taking Care of Self | To review condom use skills and increase efficacy for condom use. To discuss personal responsibility to use condoms and asking partner status. |
IMB, SCT | Condom skills practice; Personal Responsibility video. |
| 4: Taking Care of Relationships | To review effective communication skills with social networks. To practice skills when talking to partners about testing and disclosure of status. |
IMB, SCT, SNT | Communications role play and group problem solving; Protecting your partner video. |
| 5: Taking Care of Community | To discuss mentoring social network members and decreasing HIV and MSM-related stigma | SNT | Group discussion about mentoring; group problem-solving scenarios about dealing with stigma. |
| 6: Individual session | To conduct a personal risk assessment. To set goals for risk reduction. |
IMB, SCT, social identity | Risk assessment and goal setting worksheets. |
| 7: Graduation and sustainability of skills | To discuss managing risk behavior relapse prevention strategies. To remind participants about 3 month follow-up visit. |
IMB, SCT, SNT | Group discussion about risk behavior relapse triggers and prevention strategies. |
All sessions were audio-recorded and monitored for quality assurance. Sessions were randomly selected and reviewed by a trained research assistant for fidelity to content and procedures (0=inadequate; 1=adequate). Fidelity to the curriculum was high (over 90% of sessions rated as adequate).
Control condition
The control condition consisted of one, small-group based HIV prevention and care session (typically 10–15 minutes) delivered by a single facilitator who reviewed the different health resources available to AA MSM in the city. This session was conducted in the same clinic as the intervention condition. Participants received $25 for this session.
Three-month follow-up procedures
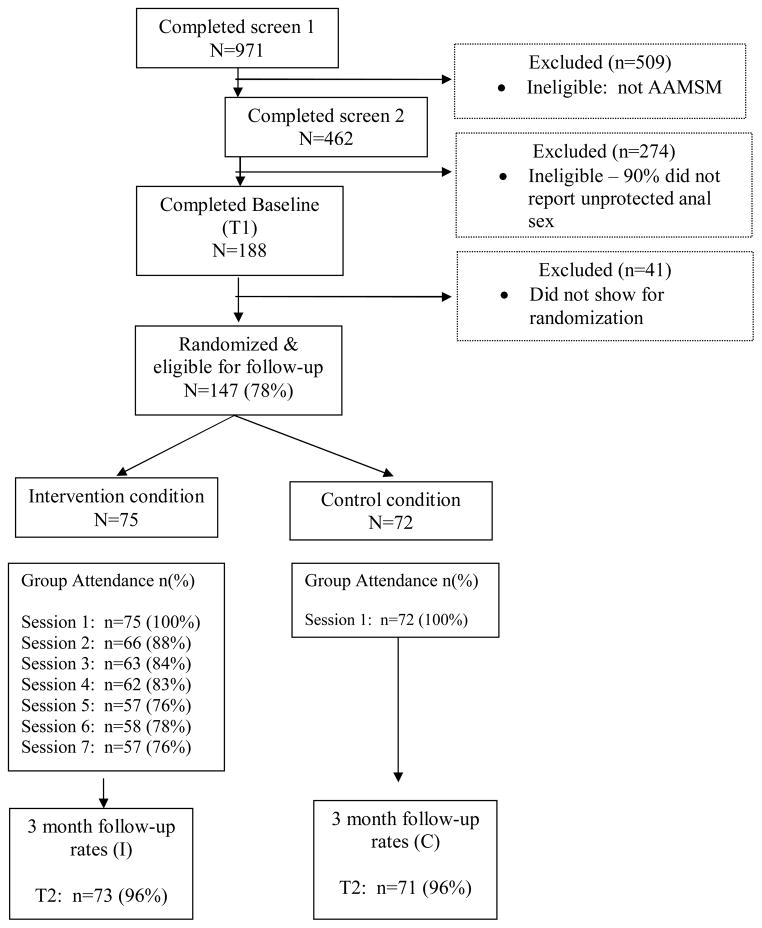
The follow-up assessments were conducted with participants from both conditions three months after the baseline interview. Procedures included using ACASI to complete the behavioral risk assessment and interviewer administered survey of the HIV communications measures and social network survey. Participants received $45 for the follow-up visit. Research assistants were blinded to the condition of the participant. Retention of randomized participants for both conditions exceeded 95% (see Figure 1).
Figure 1.
Participant flow Unity in Diversity, Baltimore Maryland
Measures
Sex risk outcomes
All sex risk outcomes data were collected using ACASI.
Number of partners
Participants reported their total number of sex partners in the past three months and indicated partner gender. Results were not normally distributed. Therefore, categorical variables were constructed as having “no partner,” “one partner only,” or “two or more partners.”
Condom Use
Participants were asked about condom use with each sex partner. A dichotomous variable was created based on the proportion of condom use during receptive or insertive anal sex during the past 3 months with any partners indicated as 100% condom use versus less. Separate variables were constructed for condom use with male partners and by partner’s HIV status.
Sex while drunk or high
For the three most recent sex partners, participants were asked if they were using drugs or alcohol the last time they had sex with these partners. Participants were considered as having sex under drug or alcohol influence if they responded affirmatively with any of the three most recent sex partners.
Communication Outcomes
Participants were asked to indicate their confidence in having conversations with their sex partners about HIV risk. Using a three-point Likert scale, participants were asked if they agreed, disagreed or neither agreed nor disagreed with the statement “I have a difficult time talking to my partner about using condoms.” Additionally, they were asked “how sure are you that you can have a conversation about using condoms with your sex partner?”; “how sure are you that you can have a conversation about getting tested for HIV together,” and “how sure are you that you can ask a new partner to use a condom before you have sex for the first time?” The last question was asked using the three-point Likert scale of very sure, neither sure nor unsure, not sure. A dichotomous variable was created based on the distribution of responses (1=Very Sure; 0=somewhat-not sure). These questions were added to the survey after enrollment began, therefore only 108 cases were collected.
Covariates
Socio-demographic characteristics measured included self-reported age, highest educational grade completed, current health insurance status, and homelessness in the prior 90 days. Participants were asked about incarceration in their lifetime and the prior 90 days. Participants indicated their current employment status as working full or part time, not working, or on disability. To assess sexual identity, participants were asked “do you consider yourself to be heterosexual or straight, bisexual, queer, homosexual or gay, not sure/questioning, or other?” A variable for HIV serostatus was created based on the results of the Oraquick testing or documentation of seropositive status. HIV seropositive status was a measure of self-reported and validated HIV-positive status or Western blot confirmed Oraquick-positive results. Participants reported substance use in the prior 90 days by type of drug and by route of administration.
Statistical Analysis
Chi-square tests for categorical and t-tests for continuous variables were used to compare baseline demographics of Index participants. Fisher’s exact test was used in lieu of chi-square tests when variables had sparse cells (less than five participants in a category). Multinomial regressions were used to examine the association between the intervention status and number of sex partners at follow-up; logistic regressions were conducted to examine the association between intervention status and dichotomized outcomes of sexual risk behavior and sex under the influence at follow-up. For condom use with HIV-positive partners and HIV-negative/unknown partners, these analyses were only conducted among those with HIV-positive partners and HIV-negative/unknown partners at baseline, respectively. Each model further adjusted for respective outcome at baseline to account for potential regression to the mean (Twisk JW, 2003), as well as HIV status and insurance status, which were statistically different (p<0.05) between conditions at baseline. All analyses were based on the intent-to-treat assumption regardless of number of sessions attended. These analyses were conducted using Stata 10 (StataCorp, 2007).
Results
A total of 188 AA MSM participants screened behaviorally eligible and completed the baseline visit (Figure 1). Non-randomized participants did not significantly differ from the randomized participants in terms of demographics or number of sex partners. A total of 147 participants were randomized between the intervention (n=75) and control conditions (n=72). Retention was high, as 96% of participants in the intervention condition (n=73) and control condition (n=71) completed the follow-up assessment.
Table 2 presents the baseline characteristics of 147 randomized participants. A majority of the sample identified as homosexual (61%), 31% as bisexual, and 8% as straight. Most had a 12th grade, GED or higher education (80%) and were not working (76%). There were no differences between the intervention (n=75) and control conditions (n=72) on most of the baseline characteristics, except HIV status (p=0.03) and health insurance (p=0.05).
Table 2.
Sample characteristics of randomized participants at baseline, UND study, Baltimore, Maryland (n=147)
| Variable | Total Sample N=147 N (%) |
Intervention Condition N=75 N (%) |
Control Condition N=72 N (%) |
p-value |
|---|---|---|---|---|
| Educational level | ||||
| Grade 11 or less | 29 (20) | 16 (21) | 13 (18) | |
| 12th grade or GED | 59 (40) | 30 (40) | 29 (40) | |
| Some college or higher | 59 (40) | 29 (39) | 30 (42) | 0.87 |
| Mean Age(SD) | 38.9 (10.2) | 38.4 (10.8) | 39.5 (9.6) | 0.53 |
| Employment status | ||||
| Not working | 50 (34) | 25 (33) | 25 (35) | |
| Disabled | 61 (42) | 33 (44) | 28 (39) | |
| Working (full or part-time) | 36 (24) | 17 (23) | 19 (26) | 0.80 |
| Currently have health insurance | 107 (73) | 60 (80) | 47 (65) | 0.05 |
| History of incarceration | ||||
| Never in lifetime | 43 (29) | 21 (28) | 22 (31) | |
| Lifetime, not in past 3 months | 85 (58) | 41 (55) | 44 (61) | |
| In the past 3 months | 19 (13) | 13 (17) | 6 (8) | 0.27 |
| Homeless in past 3 months | 18 (12) | 11 (15) | 7 (10) | 0.45 |
| Sexual identity | ||||
| Gay, same gender loving, homosexual | 87 (61) | 44 (60) | 43 (61) | |
| Bisexual | 45(31) | 20(28) | 25(36) | |
| Straight, heterosexual | 11 (8) | 9 (12) | 2 (3) | |
| Other, unsure | 4 (3) | 2 (3) | 2 (3) | 0.18 |
| HIV status | ||||
| Negative/unknown | 73 (50) | 44 (59) | 29 (40) | |
| Positive | 74 (50) | 31 (41) | 43 (60) | 0.03 |
| Injected drugs in the past 3 months | 17 (12) | 11 (15) | 6 (8) | 0.23 |
| Used heroin in the past 3 months | 30 (20) | 18 (24) | 12 (17) | 0.31 |
| Used crack in the past 3 months | 59 (40) | 30 (40) | 29 (40) | 1.00 |
| Used cocaine in the past 3 months | 38 (26) | 18 (24) | 20 (28) | 0.71 |
| Used amphetamine in the past 3 months | 6 (4) | 4 (5) | 2 (3) | 0.68 |
| Used club drugs in the past 3 months | 12 (8) | 4 (5) | 8 (11) | 0.68 |
Table 3 presents model estimates after adjusting for baseline outcome, participant’s HIV status and current insurance status. The intervention condition was associated with increased odds of reporting fewer male partners at follow-up (AOR=3.03; 95%CI=1.26–7.28 for zero versus two or more). Among participants who reported having a sex partner at follow-up (n=64), the intervention condition was associated with marginally greater odds of reporting 100% condom use with male partners (AOR=2.64; 95%CI=0.95–7.36) and HIV negative/unknown status partners (AOR=3.19; 5%CI=0.98–10.4).
Table 3.
Intervention effects on sexual risk outcomes, UND Study (n=147), Baltimore, Maryland
| Outcomes | Baseline | 3 months | AOR (95%CI)1 | ||
|---|---|---|---|---|---|
| Intervention (N=73) | Control (N=71) | Intervention (N=73) | Control (71) | ||
| n (%) | n (%) | n (%) | n (%) | ||
| 100% condom use with all partners (ref: Less than 100%)2 | 5 (7) | 5 (7) | 14 (31) | 12 (23) | 1.73 (0.62–4.79) |
| 100% condom use with male partners (ref: less than 100%) 3 | 9 (13) | 5 (8) | 17 (39) | 13 (25) | 2.64 (0.95–7.36)§ |
| 100% condom use with HIV+ partner (ref: Less than 100%) 4 | 50(71) | 45(65) | 40 (83) | 37 (70) | 1.24 (0.33–4.71) |
| 100% condom use with HIV unknown/negative partner (ref: Less than 100%)5 | 18 (25) | 19 (31) | 23 (52) | 23 (43) | 3.19 (0.98–10.38)§ |
| Alcohol use during last sex (ref: no last sex under alcohol influence or does not have partner) | 35(48) | 39(55) | 21 (44) | 27 (48) | 0.98 (0.36–2.69) |
| Drug use during last sex (ref: no last sex under drug influence) | 31(43) | 33(47) | 12 (25) | 23 (41) | 0.38 (0.10–1.37) |
| Baseline | 3 months6 | ||||
| Intervention (N=73) | Control (N=71) | Intervention (N=73) | Control (N=71) | AOR (95%CI)1 | |
| n (%) | n (%) | n (%) | n (%) | ||
| Number of male partners (ref: 2 or more) | |||||
| None | 0 (0) | 0 (0) | 25 (34) | 15 (21) | 3.03 (1.26–7.28)* |
| One | 10 (14) | 8 (11) | 23 (32) | 17 (24) | 2.39 (1.00–5.72)§ |
| Number of female partners (ref: 2 or more) | |||||
| None | 47(64) | 46(65) | 47 (64) | 52 (73) | 0.80 (0.15–4.34) |
| One | 7 (10) | 9 (13) | 15 (21) | 7 (10) | 2.28 (0.50–10.35) |
p<0.10;
p<0.05;
p<0.01
Adjusted for baseline status of the outcome, HIV status and insurance at baseline
Adjusted odds ratio estimated among a subsample of respondents who reported having partners at baseline and follow-up (n=45 intervention condition; n=52 control condition)
Adjusted odds ratio estimated among a subsample of respondents who reported having male partners at baseline and follow-up (n=44 intervention condition; n=52 control condition)
Adjusted odds ratio estimated among a subsample of respondents who reported HIV+ partners at baseline(n=48 intervention condition; n=53 control condition)
Adjusted odds ratio estimated among a subsample of respondents who reported HIV−/unknown partners at baseline(n=44 intervention condition; n=54 control condition)
Data presented includes full sample
Table 4 presents frequencies on HIV communication efficacy. Across all topics assessed, participants indicated feeling confident that they could talk about using condoms and getting tested. There were marginally significant differences between groups on the item, “I have a difficult time talking to my partner about using condoms” at baseline. These proportions did not change over time for either condition.
Table 4.
Baseline measures of HIV communication self-efficacy, UND study, Baltimore, Maryland
| Variable | Total Sample N=108* |
Intervention Condition N=53 |
Control Condition N=55 |
p-value | Intervention Condition N=54 |
Control Condition N=51 |
p-value |
|---|---|---|---|---|---|---|---|
| I have a difficult time talking to my partner about using condoms | |||||||
| Disagree | 72 (67) | 41 (77) | 31 (56) | 35 (69) | 40 (74) | ||
| Neither agree nor disagree | 11 (10) | 4 (8) | 7 (13) | 8 (16) | 4 (7) | ||
| Agree | 25 (23) | 8 (15) | 17 (31) | 0.07 | 8 (16) | 10 (19) | 0.41 |
| How sure are you that you can have a conversation about using condoms with your sex partner? | |||||||
| Very Sure | 76 (70) | 37 (70) | 39 (71) | 45 (88) | 40 (74) | ||
| Somewhat sure-not sure | 32 (30) | 16 (30) | 16 (29) | 1.00 | 6 (12) | 14 (26) | 0.07 |
| How sure are you that you can ask your partner to get tested with you? | |||||||
| Very Sure | 72 (67) | 37 (70) | 35 (64) | 37 (73) | 32 (59) | ||
| Somewhat sure-not sure | 36 (33) | 16 (30) | 20 (36) | 0.54 | 14 (27) | 22 (41) | 0.15 |
| How sure are you that you can ask a new partner to use a condom before you have sex for the first time? | |||||||
| Very Sure | 74 (69) | 37 (70) | 37 (67) | 35 (69) | 35 (65) | ||
| Somewhat sure-not sure | 34 (31) | 16 (30) | 18 (33) | 0.84 | 16 (31) | 19 (35) | 0.68 |
Questions added to survey after enrollment began, therefore n=108 participants provided data.
Discussion
Results from this randomized clinical trial with a sample of behaviorally risky AA MSM indicate efficacy in decreasing the number of male sex partners and marginal effects on condom use with male partners and with partners with HIV negative or unknown serostatus. These results contribute to the limited number of culturally appropriate interventions available for African American men who have sex with men (Centers for Disease Control and Prevention, 2010a; Centers for Disease Control and Prevention, 2010b; Scott, Bernstein, Raymond, Kohn, & Klausner, 2010). Content of both conditions promoted a range of risk reduction strategies including abstinence, reducing the number of sexual partners, condom use and HIV testing which may explain the reductions in risk behavior in the control condition. The intervention condition was exposed to a greater dose and activities were structured to enable the opportunity to practice risk reduction skills and results suggest the importance of developing interventions that are interactive with multiple sessions.
Interventions that increase consistent and proper condom use with all partners are an important way to intervene on both STI and HIV transmission (Lyles et al., 2007) UND was designed with numerous activities and opportunities for participants to practice handling and properly using condoms. Intervention participants were provided with a variety of condoms and lubricants and encouraged to talk to their social network members and distribute condoms to them. Among participants who had a sexual partner at follow-up we observed a marginally significant trend of increased condom use with male and HIV negative/unknown. These findings are promising, though limited by low sample size and power.
One-third of the sample (34%) reported having at least one female sex partner at baseline. No intervention effects were found on number of female partners over time or condom use. The lack of effect on condom use and number of female partners may be due to floor effects or indicate partner-specific resistance to condom use. AA MSM may seek relationships with women for numerous reasons. For example, in addition to avoiding stigma of MSM identity, women may offer financial security and opportunities to have children (Martinez & Hosek, 2005). Men who have sex with men and women are a unique sub-group that have been described in the literature as potential bridges for HIV and STI transmission and would benefit from further research that focus on risk reduction with different sex partners (Latkin et al., 2011).
HIV communication efficacy was high in both conditions and did not change over the 3 month follow-up. Given that a majority reported less than 100% condom use with current sex partners, it may be that comfort or self-efficacy in having conversations about condom use is not a core factor in affecting actual condom use. Factors such as relationship dynamics (Wolitski et al., 2003) and substance use (Koblin et al., 2006; McKirnan, Vanable, Ostrow, & Hope, 2001) have been identified as barriers to condom use. These findings imply that intervention efforts should focus on skills for initiating actual conversations in relevant social contexts versus increasing self-efficacy to have conversations. Use of role-plays or video vignettes of initiating conversations in real situations may be one approach to train participants in these skills.
Limitations of the study should be noted. This study used a convenience sample that were predominately older men who were not currently working full-time, which limits generalizability to younger men and those who were unable to commit to attending two sessions a week in the afternoon. The outcomes were based only on self-reports and the measures included in this analysis did not differentiate by partner type or insertive versus receptive anal sex. There was insufficient power to examine intervention effects on network member condom use. Though the control condition received high quality risk reduction counseling during the baseline visit, this condition was not equal attention and the experimental condition received more renumeration for their session attendance (up to $140) as compared to $20 for one session. We did not assess potential contamination between conditions, which may explain the limited effects of the intervention. Additionally, the 3-month follow-up period to assess behavior change limits our ability to determine sustainability of effects.
Conclusions
Racial disparities in HIV among MSM persist and there is no evidence to support that this is due to individual level risk behavior (Millett, Peterson, Wolitski, & Stall, 2006). There has been increased attention to the role of culture as a contributing factor to the disproportionate rates of HIV among AA MSM. As such, there has been an increased effort to develop interventions that are culturally tailored as one approach for addressing the disparities. These culturally tailored interventions explicitly acknowledge the role of homophobia, stigma and discrimination in shaping behavior for AA MSM. The present study contributes to the limited number of rigorously tested culturally tailored interventions currently available for this study population and may aide health educators to recognize issues that are important for inclusion in an intervention for AA MSM.
Implications for practice
UND was a multiple session, multiple component program that included numerous opportunities for the participants to build self-efficacy in HIV risk reduction skills and reinforce skills. Allowing ample time for practice and feedback from peers was an important component for participants to integrate the content with their personal experiences. While brief individual interventions hold promise, programs that include small group formats is of particular value especially for individuals who have been stigmatized and report social isolation. This format provides an opportunity for social support, peer modeling, peer influence and to promote changes in social norms.
Much has been written about the benefits of community-based participatory approaches (Operario et al., 2010; Strathdee et al., 2006; Strong et al., 2009). UND relied on a panel of community stake-holders to provide feedback and suggestions for content, as have most other interventions designed for AA MSM (Rhodes et al., 2011). While, we did not develop UND using all of the principles of CBPR, the process of engaging with the IAB was productive in terms of developing intervention content that resonated with study participants. Development of future interventions should prioritize inclusion of “voices from the community”, whether it be in the form of a true CBPR partnership or in terms of advisory boards. We recommend extending the involvement of the stakeholder by obtaining their perspectives of the partnerships so that the process of community engagement can be improved and sustained.
Dissemination and implementation of efficacious interventions within community-based settings is a challenge within the health education and public health field. Many community-based organizations and AIDS service organizations may lack the capacity (e.g. staffing, space, materials) to implement a multiple session intervention such as UND. This underscores the value of early and consistent partnerships with agencies in the community so that the interventions that are developed are more readily able to be implemented in the field. As efforts continue to develop interventions that are culturally-sensitive and tailored for AA MSM, considerations of community context and resources will be key.
References
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, N.J: Prentice-Hall; 1986. [Google Scholar]
- Brooks R, Rotheram-Borus MJ, Bing EG, Ayala G, Henry CL. HIV and AIDS among men of color who have sex with men and men of color who have sex with men and women: An epidemiological profile. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education. 2003;15(1 Suppl A):1–6. doi: 10.1521/aeap.15.1.5.1.23607. [DOI] [PubMed] [Google Scholar]
- Carpiano RM, Kelly BC, Easterbrook A, Parsons JT. Community and drug use among gay men: the role of neighborhoods and networks. J Health Soc Behav. 2011 Mar;52(1):74–90. doi: 10.1177/0022146510395026. [DOI] [PubMed] [Google Scholar]
- Catania JA, Osmond D, Stall RD, Pollack L, Paul JP, Blower S, Coates TJ. The continuing HIV epidemic among men who have sex with men. American Journal of Public Health. 2001;91(6):907–914. doi: 10.2105/ajph.91.6.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celentano DD, Sifakis F, Hylton J, Torian LV, Guillin V, Koblin BA. Race/ethnic differences in HIV prevalence and risks among adolescent and young adult men who have sex with men. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2005;82(4):610–621. doi: 10.1093/jurban/jti124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. From the centers for disease control and prevention. HIV/STD risks in young men who have sex with men who do not disclose their sexual orientation--six U.S. cities, 1994–2000. JAMA: The Journal of the American Medical Association. 2003;289(8):975–977. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV surveillance report, 2008. 20. Atlanta: U.S. Department of Health and Human Services; 2010a. [Google Scholar]
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance, 2009. Atlanta: U.S. Department of Health and Human Services; 2010b. [Google Scholar]
- Davey-Rothwell MA, Tobin K, Yang C, Sun CJ, Latkin CA. Results of a randomized controlled trial of a peer mentor HIV/STI prevention intervention for women over an 18 month follow-up. AIDS and Behavior. 2011 doi: 10.1007/s10461-011-9943-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2006;25(4):462–473. doi: 10.1037/0278-6133.25.4.462. [DOI] [PubMed] [Google Scholar]
- German D, Sifakis F, Maulsby C, Towe VL, Flynn CP, Latkin CA, Holtgrave DR. Persistently high prevalence and unrecognized HIV infection among men who have sex with men in Baltimore: The BESURE study. Journal of Acquired Immune Deficiency Syndromes (1999) 2011 doi: 10.1097/QAI.0b013e318211b41e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghanem KG, Hutton HE, Zenilman JM, Zimba R, Erbelding EJ. Audio computer assisted self interview and face to face interview modes in assessing response bias among STD clinic patients. Sexually Transmitted Infections. 2005;81(5):421–425. doi: 10.1136/sti.2004.013193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harawa NT, Greenland S, Bingham TA, Johnson DF, Cochran SD, Cunningham WE, Valleroy LA. Associations of race/ethnicity with HIV prevalence and HIV-related behaviors among young men who have sex with men in 7 urban centers in the United States. Journal of Acquired Immune Deficiency Syndromes (1999) 2004;35(5):526–536. doi: 10.1097/00126334-200404150-00011. [DOI] [PubMed] [Google Scholar]
- Jimenez AD. Triple jeopardy: Targeting older men of color who have sex with men. Journal of Acquired Immune Deficiency Syndromes (1999) 2003;33(Suppl 2):S222–5. [PubMed] [Google Scholar]
- Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, McClellan WM. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database of Systematic Reviews (Online) 2008;3:CD001230. doi: 10.1002/14651858.CD001230.pub2. [DOI] [PubMed] [Google Scholar]
- Jones KT, Gray P, Whiteside YO, Wang T, Bost D, Dunbar E, Johnson WD. Evaluation of an HIV prevention intervention adapted for black men who have sex with men. American Journal of Public Health. 2008;98(6):1043–1050. doi: 10.2105/AJPH.2007.120337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, Buchbinder S. Risk factors for HIV infection among men who have sex with men. AIDS (London, England) 2006;20(5):731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- Koblin BA, Torian LV, Guilin V, Ren L, MacKellar DA, Valleroy LA. High prevalence of HIV infection among young men who have sex with men in New York City. AIDS (London, England) 2000;14(12):1793–1800. doi: 10.1097/00002030-200008180-00015. [DOI] [PubMed] [Google Scholar]
- Latkin C, Yang C, Tobin K, Penniman T, Patterson J, Spikes P. Differences in the social networks of African American men who have sex with men only and those who have sex with men and women. American Journal of Public Health. 2011;101(10):e18–23. doi: 10.2105/AJPH.2011.300281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: Outcome of a network-oriented peer outreach intervention. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2003;22(4):332–339. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- Lyles CM, Kay LS, Crepaz N, Herbst JH, Passin WF, Kim AS HIV/AIDS Prevention Research Synthesis Team. Best-evidence interventions: Findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000–2004. American Journal of Public Health. 2007;97(1):133–143. doi: 10.2105/AJPH.2005.076182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macalino GE, Celentano DD, Latkin C, Strathdee SA, Vlahov D. Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-seronegative injection drug users. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education. 2002;14(5):367–378. doi: 10.1521/aeap.14.6.367.24075. [DOI] [PubMed] [Google Scholar]
- Martinez J, Hosek SG. An exploration of the down-low identity: Nongay-identified young African-American men who have sex with men. Journal of the National Medical Association. 2005;97(8):1103–1112. [PMC free article] [PubMed] [Google Scholar]
- Mays VM, Cochran SD, Zamudio A. HIV prevention research: Are we meeting the needs of African American men who have sex with men? The Journal of Black Psychology. 2004;30(1):78–105. doi: 10.1177/0095798403260265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKirnan DJ, Vanable PA, Ostrow DG, Hope B. Expectancies of sexual “escape” and sexual risk among drug and alcohol-involved gay and bisexual men. Journal of Substance Abuse. 2001;13(1–2):137–154. doi: 10.1016/s0899-3289(01)00063-3. [DOI] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: A critical literature review. American Journal of Public Health. 2006;96(6):1007–1019. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Smith CD, Arnold E, Kegeles S. The bruthas project: Evaluation of a community-based HIV prevention intervention for African American men who have sex with men and women. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education. 2010;22(1):37–48. doi: 10.1521/aeap.2010.22.1.37. [DOI] [PubMed] [Google Scholar]
- Peterson JL, Bakeman R, Blackshear JH, Jr, Stokes JP. Perceptions of condom use among African American men who have sex with men. Culture, Health and Sexuality. 2003;5(5):409–424. [Google Scholar]
- Peterson JL, Jones KT. HIV prevention for black men who have sex with men in the United States. American Journal of Public Health. 2009;99(6):976–980. doi: 10.2105/AJPH.2008.143214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Vissman AT, Stowers J, Miller C, McCoy TP, Hergenrather KC, Eng E. A CBPR partnership increases HIV testing among men who have sex with men (MSM): Outcome findings from a pilot test of the CyBER/testing internet intervention. Health Education & Behavior: The Official Publication of the Society for Public Health Education. 2011;38(3):311–320. doi: 10.1177/1090198110379572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott HM, Bernstein KT, Raymond HF, Kohn R, Klausner JD. Racial/ethnic and sexual behavior disparities in rates of sexually transmitted infections, San Francisco, 1999–2008. BMC Public Health. 2010;10:315. doi: 10.1186/1471-2458-10-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 10. College Station, TX: 2007. [Google Scholar]
- Strathdee SA, Ricketts EP, Huettner S, Cornelius L, Bishai D, Havens JR, Latkin CA. Facilitating entry into drug treatment among injection drug users referred from a needle exchange program: Results from a community-based behavioral intervention trial. Drug and Alcohol Dependence. 2006;83(3):225–232. doi: 10.1016/j.drugalcdep.2005.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong LL, Israel BA, Schulz AJ, Reyes A, Rowe Z, Weir SS, Poe C. Piloting interventions within a community-based participatory research framework: Lessons learned from the healthy environments partnership. Progress in Community Health Partnerships: Research, Education, and Action. 2009;3(4):327–334. doi: 10.1353/cpr.0.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, Kuramoto SJ, Davey-Rothwell MA, Latkin CA. The STEP into action study: A peer-based, personal risk network-focused HIV prevention intervention with injection drug users in Baltimore, Maryland. Addiction (Abingdon, England) 2011;106(2):366–375. doi: 10.1111/j.1360-0443.2010.03146.x;10.1111/j.1360-0443.2010.03146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twisk JW. Applied longitudinal data analysis for epidemiology: A practical guide. Cambridge, UK: Cambridge University Press; 2003. [Google Scholar]
- Voelker R. Studies illuminate HIV’s inequalities. JAMA: The Journal of the American Medical Association. 2008;299(3):269–275. doi: 10.1001/jama.299.3.269. [DOI] [PubMed] [Google Scholar]
- Williams JK, Wyatt GE, Resell J, Peterson J, Asuan-O’Brien A. Psychosocial issues among gay- and non-gay-identifying HIV-seropositive African American and Latino MSM. Cultural Diversity & Ethnic Minority Psychology. 2004;10(3):268–286. doi: 10.1037/1099-9809.10.3.268. [DOI] [PubMed] [Google Scholar]
- Wilton L, Herbst JH, Coury-Doniger P, Painter TM, English G, Alvarez ME, Carey JW. Efficacy of an HIV/STI prevention intervention for black men who have sex with men: Findings from the many men, many voices (3MV) project. AIDS and Behavior. 2009;13(3):532–544. doi: 10.1007/s10461-009-9529-y. [DOI] [PubMed] [Google Scholar]
- Wolitski RJ, Bailey CJ, O’Leary A, Gomez CA, Parsons JT Seropositive Urban Men’s Study (SUMS) Self-perceived responsibility of HIV-seropositive men who have sex with men for preventing HIV transmission. AIDS and Behavior. 2003;7(4):363–372. doi: 10.1023/b:aibe.0000004728.73443.32. [DOI] [PubMed] [Google Scholar]