Abstract
Background
The current study was carried out to examine the gastroprotective effects of Parkia speciosa against ethanol-induced gastric mucosa injury in rats.
Methodology/Principal Findings
Sprague Dawley rats were separated into 7 groups. Groups 1–2 were orally challenged with carboxymethylcellulose (CMC); group 3 received 20 mg/kg omeprazole and groups 4–7 received 50, 100, 200 and 400 mg/kg of ethanolic leaf extract, respectively. After 1 h, CMC or absolute ethanol was given orally to groups 2–7. The rats were sacrificed after 1 h. Then, the injuries to the gastric mucosa were estimated through assessment of the gastric wall mucus, the gross appearance of ulcer areas, histology, immunohistochemistry and enzymatic assays. Group 2 exhibited significant mucosal injuries, with reduced gastric wall mucus and severe damage to the gastric mucosa, whereas reductions in mucosal injury were observed for groups 4–7. Groups 3–7 demonstrated a reversal in the decrease in Periodic acid-Schiff (PAS) staining induced by ethanol. No symptoms of toxicity or death were observed during the acute toxicity tests.
Conclusion
Treatment with the extract led to the upregulation of heat-shock protein 70 (HSP70) and the downregulation of the pro-apoptotic protein BAX. Significant increases in the levels of the antioxidant defense enzymes glutathione (GSH) and superoxide dismutase (SOD) in the gastric mucosal homogenate were observed, whereas that of a lipid peroxidation marker (MDA) was significantly decreased. Significance was defined as p<0.05 compared to the ulcer control group (Group 2).
Introduction
Peptic ulcers, which are characterized by the presence of mucosal damage, are predominantly caused by infection with Helicobacter pylori, antiplatelet agents such as acetylsalicylic acid [1], non-steroidal anti-inflammatory drugs (NSAIDs) such as oral bisphosphonates, potassium chloride, immunosuppressive medications [2], serotonin reuptake inhibitors [3], alcohol consumption and cigarette smoking [4]. These factors can cause submucosal erosion and inhibit cyclooxygenase, thus disturbing the protection of the gastric mucosal layer [5]. Anatomically, peptic ulcers occur mostly in the stomach and proximal duodenum. Peptic ulcers are caused by an imbalance between the defensive (mucus secretion, mucosal barrier, blood flow, cellular regeneration and endogenous protective agents) and destructive (acid and pepsin secretion) functions of the gastric system [6]. Alcohol-induced gastric lesions impair gastric defense factors such as mucus secretion and mucosal circulation [7]. Ethanol causes necrotic lesions in the gastric mucosa through multiple pathways, directly producing necrotic lesions, which in turn reduces defensive factors, bicarbonate secretion and mucus production [8]. The gastric wall mucus is thought to play an important role as a defensive barrier against gastrointestinal damage [9]. Mucus secretion is considered to be a crucial defensive factor that protects the gastric mucosa from lesions [10]. The level of gastric wall mucus has been evaluated previously and is used as an indicator of gastric mucus secretion [11]. Researchers have reported a large number of medicinal plants with antiulcer properties [12]–[14]. Plant-based medicines represent a vast untapped resource that has shown enormous therapeutic potential. Parkia speciosa is also known as stink bean or “petai.” It bears long, flat bean pods with green seeds. These beans are popular in Southeastern Asia, including Malaysia and Northeastern India. The beans are sold in the pods or as seeds that are already separated from the pods. The beans may are be jarred in brine and exported. In addition, P. speciosa is believed by the local residents to possess medicinal properties [15] and has been reported to exhibit hypoglycemic, antibacterial, anticancer and antioxidant activity [16]. The present study was performed to establish the antioxidant and antiulcer activity of Parkia speciosa ethanol leaf extract against ethanol-induced gastric ulcers in rats.
Materials and Methods
Materials and Reagents
All materials and reagents were obtained from Sigma (Sigma Aldrich, Germany), and the MDA, SOD and GSH activity measurement kits were purchased from Cayman Chemical Company (Cayman, USA). Omeprazole was used as a reference antiulcer drug and was obtained from the University of Malaya Medical Centre (UMMC). The drug was dissolved in 0.5% (w/v) carboxymethylcellulose (CMC) and orally administered to the rats at a dosage of 20 mg/kg body weight (5 ml/kg) according to Mahmood et al [17].
Plant Material and Preparation of the Crude Extract
Fresh Parkia speciosa leaves were obtained from Ethno Resources (Selangor, Malaysia). The identity of the plant was confirmed at the Rimba Ilmu Herbarium, Institute of Biological Sciences, University of Malaya through a comparison with the voucher specimen. Fresh leaves were hung upside down in a warm, dry place (away from direct sunlight) with good air circulation for two weeks to dry. Then, using an electrical blender, the dried leaves were converted to a fine powder. A quantity of 100 g of the powder was soaked for 3 days in a flask that contained 500 ml of 95% ethanol. The mixture was filtered using a fine muslin cloth and filter paper (Whatman No. 1). The filtered mixture was distilled using a rotary evaporator (Eyela, USA) and yielded nearly 17.4% dried mass. The dried extract was diluted in CMC and orally administered to the rats at a dose of 50, 100, 200 or 400 mg/kg body weight (in 0.5% CMC, 5 ml/kg body weight), in accord with earlier reports [18].
Acute Toxicity
Healthy male and female Sprague Dawley rats (6–8 weeks old) were obtained from the animal house (University of Malaya, Ethics No. PM/07/05/2010/1111/MAA/R). The rats weighed between 180–200 g. The animals were given standard rat pellets and tap water ad libitum and were individually placed in separate cages with wide-mesh wire bottoms to prevent coprophagy during the experiment. An acute toxicity study was performed to determine a safe dose for the P. speciosa extract. A total of 48 rats (24 males and 24 females) were equally divided into 4 groups that received the vehicle (0.5% CMC, 5 ml/kg) or 1, 3 or 5 g/kg of leaf extract (5 ml/kg). The animals were fasted overnight (but allowed water) prior to dosing. Food was withheld for a further 3 to 4 h after dosing. The animals were observed for 48 hours after the administration of the powder for the onset of clinical or toxicological symptoms. Mortality, if any, was observed over a period of 2 weeks. The animals were sacrificed by an overdose of xylazine and ketamine anesthesia on the 15th day. Histological, hematological and serum biochemical parameters were determined according to standard methods [19]. The ethics committee for animal experimentation of the Faculty of Medicine, University of Malaya, approved the experiment. Throughout the experiments, all animals were treated humanely according to the criteria outlined in the “Guide for the Care and Use of Laboratory Animals” [20].
Animal Stock
Healthy adult Sprague Dawley rats (6–8 weeks old), each weighing between 200–220 g, were obtained from the animal house at the University of Malaya (Ethic No. PM/12/05/2010/MAA/R). The rats were randomly divided into 7 groups of 6 rats each and received a standard pellet diet and tap water ad libitum. The rats were individually placed in separate cages with wide-mesh wire bottoms to prevent coprophagy during the experiment.
Gastric Ulcer Induction by Ethanol
The animals were fasted for 24 h prior to the experiment [17]. Groups 1 and 2 received vehicle (0.5% CMC) orally. Group 3 received an oral dose of 20 mg/kg omeprazole in 0.5% CMC (5 ml/kg), and groups 4–7 received ethanolic extract of Parkia speciosa at doses of 50, 100, 200 or 400 mg/kg as a pretreatment. At 1 h after pretreatment, the vehicle or absolute ethanol was orally administered to groups 2–7 [12]. One hour later, the rats were euthanized, and their stomachs were dissected.
Measurement of Gastric Juice Acidity
The animals were sacrificed, and their stomachs were removed. The stomach contents were collected, measured, centrifuged, and subjected to analysis for titratable acidity against 0.01 N NaOH to pH 7 [21].
Determination of Gastric Wall Mucus (GWM)
The modified procedure of Piper et al. was used to analyze the gastric wall mucus. The glandular segments from the stomachs of the control and treated rats were removed and weighed. Each segment was transferred immediately to 1% Alcian blue (in sucrose solution, buffered with sodium acetate, pH 5), and the excess dye was removed by rinsing with sucrose solution. The dye in complex with the gastric wall mucus was extracted with magnesium chloride. A 4 ml sample of the blue extract was then shaken with an equal volume of diethyl ether. The resulting emulsion was centrifuged, and the absorbance of the aqueous layer was measured at 580 nm. The quantity of Alcian blue extracted per gram (net) of glandular tissue was then calculated [22].
Macroscopic Gastric Lesion Evaluation
The rat stomachs were examined under a stereomicroscope. The length and width (mm) of each individual hemorrhagic lesion was measured by a planimeter (10 × 10 mm2 = ulcer area) under a dissecting microscope (1.8×). The ulcer area (UA) was calculated using the sum of the areas of all lesions for each stomach according to a previously published protocol [23]. The UA was calculated using the following formula:
Inhibition percentage (I%) was calculated as follows:
Antioxidant Activity
Preparation of homogenate
Gastric tissue homogenate 10% (w/v) was prepared in ice-cold 50 mM phosphate buffer (pH 7.4) containing a mammalian protease inhibitor cocktail and then centrifuged at 4,000 rpm for 10 minutes (4°C).
Measurement of superoxide dismutase (SOD) activity
The SOD activity was measured according to the protocol of Sun et al [24]. The enzymatic activity was evaluated by measuring the enzyme’s capacity to inhibit the photochemical reduction of nitro-blue tetrazolium (NBT). In this assay, the photochemical reduction of riboflavin generates O2−; this reduces the NBT to produce a formazan salt that absorbs light at a wavelength of 560 nm. In the presence of SOD, NBT reduction is inhibited because the enzyme converts the superoxide radical to peroxide. The results are expressed as the quantity of SOD necessary to inhibit the rate of NBT reduction by 50% in units of enzyme per gram of protein. The supernatants of the homogenates were centrifuged a second time (20 min, 12,000 rpm, 4°C), and the resulting supernatant was assayed. In a dark chamber, 1 ml of the reactant (50 mM phosphate buffer, 100 nM EDTA and 13 mM l-methionine, pH 7.8) was mixed with 30 µL of the sample, 150 µL of 75 µM NBT and 300 µL of 2 µM riboflavin. The solution was then exposed to fluorescent light (15 W) for 15 min and read using a spectrophotometer at 560 nm.
Measurement of lipid peroxidation (MDA)
Tissue malondialdehyde (MDA) (mmol/L) was determined using the double heating method of Draper and Hadley [25]. A reaction mixture containing 8.1% sodium dodecyl sulfate, 20% acetate buffer (pH 3.5) and 0.8% thiobarbituric acid (TBA) was mixed well with 0.2 ml of stomach tissue homogenate for 3 min and then incubated at 95°C for 60 min. After chilling, the TBA-reactive substance (MDA) was extracted with 1 ml of H2O and 2.5 ml of an n-butanol:pyridine mixture (15∶1, v/v). The upper organic layer containing the MDA, which was produced by lipid peroxidation, was measured at 532 nm.
Determination of total glutathione (GSH)
The gastric mucosa was weighed, minced with scissors and homogenized at 48°C in phosphate-buffered saline (PBS). The homogenate was immediately precipitated with 0.1 ml 25% trichloroacetic acid, and the precipitate was removed by centrifugation at 4200 rpm for 40 min at 4°C. The supernatant was used in a 5,5′-dithiobis(2-nitrobenzoic acid) assay to determine GSH. Absorbance was measured at 412 nm using a spectrophotometer [26].
Histological Examination of the Gastric Mucosa
The gastric wall specimens were fixed in 10% buffered formalin for 24 h prior to paraffin tissue processing (Leica, Germany). The stomach tissues were sectioned at a thickness of 5 µm and stained with hematoxylin and eosin to evaluate histological degeneration [27].
Study of Mucosal Glycoproteins
The sections of the glandular portion of the rat stomach were stained with Periodic acid-Schiff (PAS) as described by McManus et al [28].
Immunohistochemical Staining
Immunohistochemical staining for HSP70 and BAX proteins was conducted according to the manufacturer’s protocol (DakoCytomation, USA).
Statistical Analysis
All values are reported as the mean ± S.E.M. and were analyzed by one-way ANOVA followed by Tukey’s post-hoc test for multiple comparisons using the Statistical Package for the Social Sciences software (SPSS 18). The differences between means were considered statistically significant when the p value was less than 0.05.
Results
Acute Toxicity Study
No death or significant toxicity was observed in the control or treatment groups (extract doses of 1, 3 or 5 g/kg for 14 days), as evaluated based on clinical and histopathological observations.
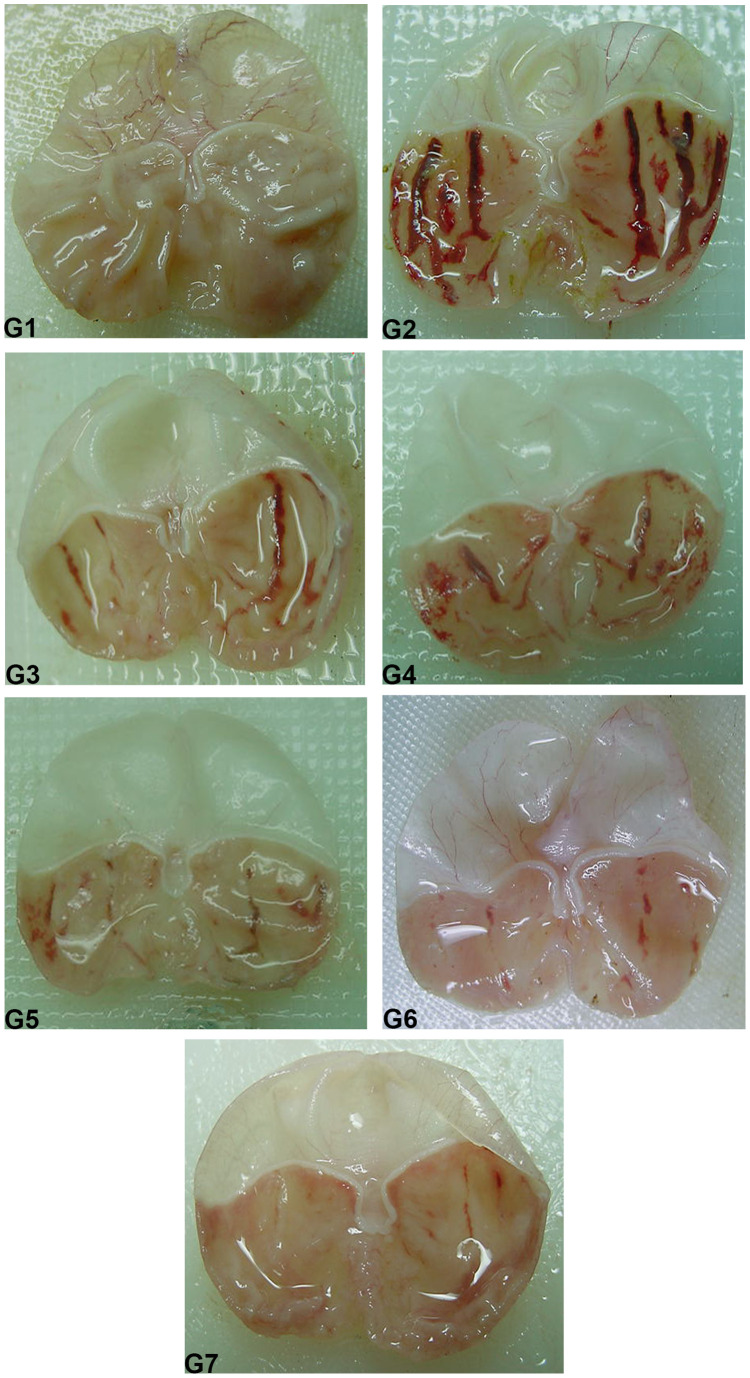
Gross Evaluation of Gastric Lesions
The antiulcer activity of the Parkia speciosa leaf extract in the ethanol-induced gastric lesion model is shown in Table 1. The results demonstrated that rats pretreated with omeprazole or Parkia speciosa extracts prior to treatment with absolute ethanol (groups 3–7) exhibited significantly smaller areas of gastric ulceration than did group 2 (Figure 1). Absolute ethanol produced extensive and visible hemorrhagic lesions in the gastric mucosa. Parkia speciosa extract significantly inhibited the ulcer formation induced by absolute ethanol and obviously decreased the gastric mucosal damage in a dose-dependent manner, i.e., the Parkia speciosa extract significantly suppressed the formation of ulcers. Intriguingly, a flattening of the gastric mucosal folds was observed in group 7. The protection of the gastric mucosa was also the most prominent in group 7 (Table 1 and Figure 1). The inhibition of gastric ulcer formation in group 6 was significant and comparable to that observed in the omeprazole treatment group (group 3) (Table 1 and Figure 1).
Table 1. The effect of Parkia speciosa ethanolic extract on gastric content pH, gastric ulcer area and the inhibition of ethanol-induced gastric mucosal lesions in rats.
| Experimental Group | pH | Ulcer Area | Inhibition(%) |
| CMC (vehicle) | 6.57±0.21 | 0 | 0 |
| CMC (control) | 3.43±0.26 | 877.45±29.99 | 0 |
| Omeprazole | 5.43±0.21** | 209.46±12.78** | 76 |
| P. speciosa (50 mg/kg) | 4.24±0.20 | 373.04±22.23** | 57 |
| P. speciosa (100 mg/kg) | 4.75±0.34* | 215.09±23.43** | 75 |
| P. speciosa (200 mg/kg) | 5.36±0.20** | 102.37±7.59** | 88 |
| P. speciosa (400 mg/kg) | 6.04±0.27** | 39.18±3.55** | 95 |
Rats pretreated with Parkia speciosa (100, 200, and 400 mg/kg) extracts had significantly reduced gastric ulcer areas and gastric content pH. All values are expressed as the mean ± standard error of the mean; differences between means were considered significant at p0.05 or p0.001 levels. The data were analyzed by one-way ANOVA using the Statistical Package for the Social Sciences software (SPSS 18).
Figure 1. The effect of P. speciosa on the macroscopic appearance of the gastric mucosa in ethanol-induced gastric mucosal lesions in rats.
(G1) (Normal control group); (G2) (Ulcer control group); (G3) (Omeprazole); (G4) (50 mg/kg), (G5) (100 mg/kg), (G6) (200 mg/kg), (G7) (400 mg/kg) Parkia speciosa extract.
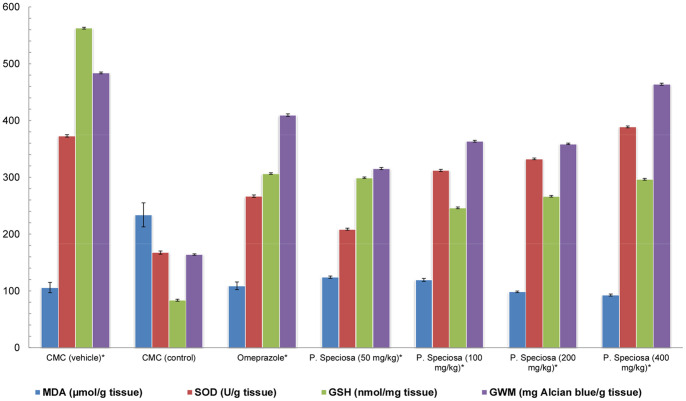
The Effect of Parkia Speciosa on GWM, SOD, MDA, and GSH
The effects of P. speciosa on the gastric wall mucus in ethanol-induced gastric mucosal lesions in rats were examined. Group 2 exhibited a significant decrease in the Alcian blue binding capacity of the gastric wall mucus, whereas groups 4–7 demonstrated a significant enhancement in the Alcian blue binding capacity of the gastric mucosa. Similarly, in group 2, ethanol reduced the SOD activity, while groups 4–7 exhibited a significant increase in SOD enzyme activity compared with group 2. The MDA activity was significantly higher in group 2 than in group 1, while groups 4–7 demonstrated significantly decreased MDA activity. In addition, the effect of the Parkia speciosa extract on the total GSH in gastric mucosal homogenates was assessed. Ethanol treatment caused a significant depletion of GSH in group 2 compared to group 1. In contrast, groups 47 exhibited significantly augmented GSH content (Figure 2).
Figure 2. The effects of P. speciosa on SOD, MDA, GSH and GWM in the gastric mucosa homogenate of ethanol-induced gastric mucosal lesions in rats.
All values are expressed as the mean ± standard error of the mean. All P. speciosa-treated groups were significantly different from the control groups at p0.05. The data were analyzed by one-way ANOVA using the Statistical Package for the Social Sciences software (SPSS 18).
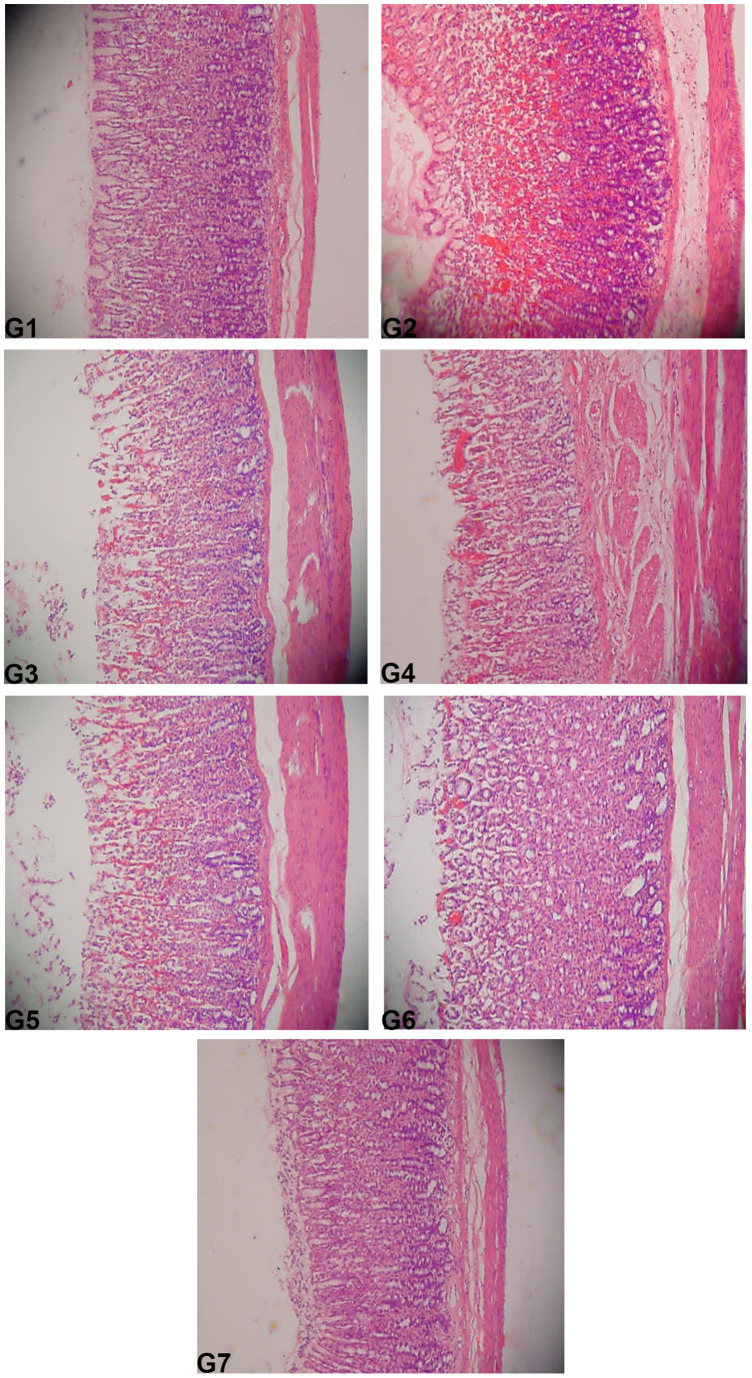
Histological Evaluation of Gastric Lesions
Histological observations of group 1 indicated that there was no disruption of the surface epithelium, while the histological examination showed extensive damage to the gastric mucosa in group 2, with necrotic lesions penetrating deeply into the mucosa accompanied by extensive edema and leucocyte infiltration of the submucosal layer (Figure 3). Group 4 exhibited moderate disruption of the surface epithelium, with edema and leucocyte infiltration of the submucosal layer, and group 5 showed a mild disruption of the surface epithelium with edema and leucocyte infiltration into the submucosal layer. Group 6 showed mild disruption of the surface epithelium with edema and leucocyte infiltration of the submucosal layer. Group 7 showed mild edema and leucocyte infiltration of the submucosal layer, but no disruption of the surface epithelium. Group 3 exhibited a mild disruption of the surface epithelium, with submucosal edema and leucocyte infiltration. These results demonstrated that the plant extracts exerted cytoprotective effects in a dose-dependent manner (Figure 3).
Figure 3. The effect of P. speciosa on the histology of ethanol-induced gastric mucosal damage in rats.
(G1) (Normal control group); (G2) (Ulcer control group); (G3) (Omeprazole); (G4) (50 mg/kg), (G5) (100 mg/kg), (G6) (200 mg/kg), (G7) (400 mg/kg) Parkia speciosa extract. The rats in groups 4–7 demonstrated comparatively better protection of the gastric mucosa, as shown by a reduction in or absence of the ulcer area, submucosal edema and leucocyte infiltration (H&E staining, 20×).
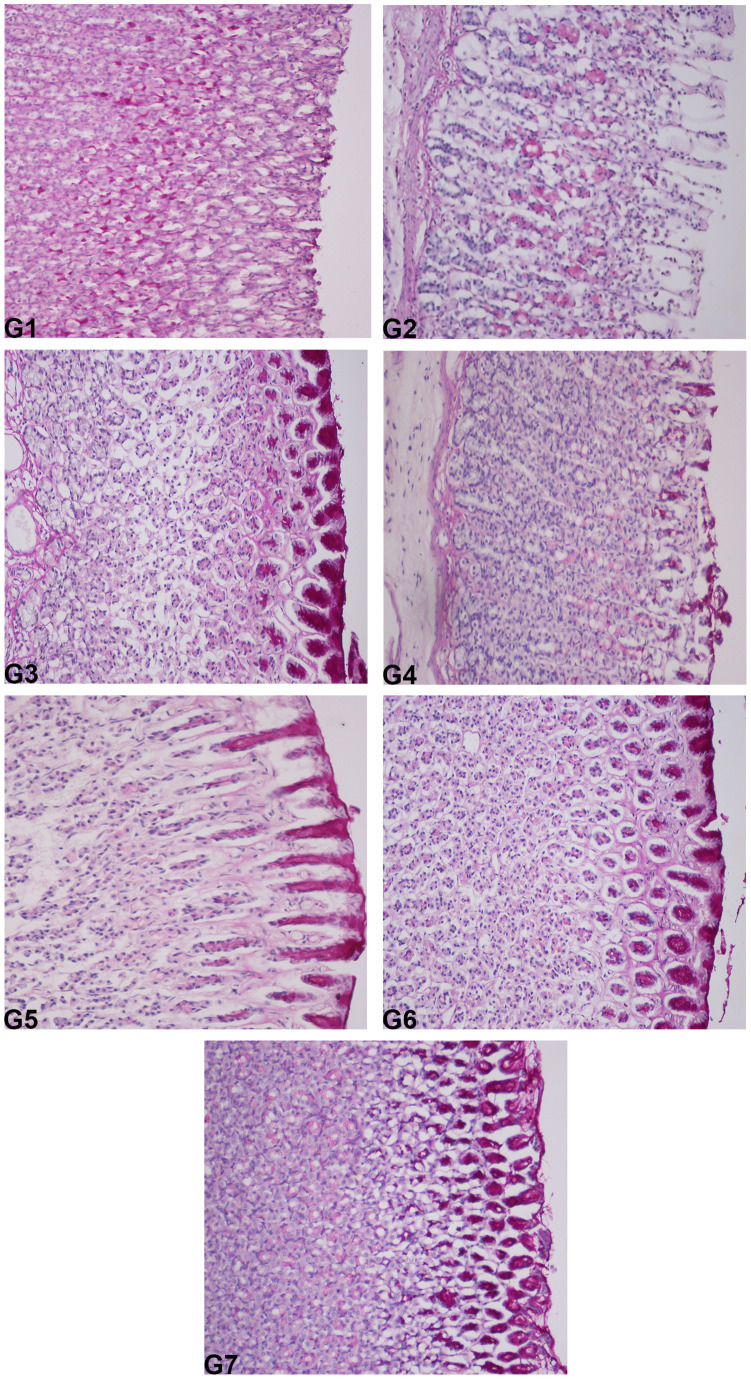
Periodic Acid-Schiff (PAS)
The gastric mucosa in animals pretreated with Parkia speciosa extract or omeprazole (group 3–7) displayed increased PAS staining intensity compared to the rats in group 2, indicating an increase in the glycoprotein content of gastric mucosa in pretreated rats (Figure 4).
Figure 4. The effect of Parkia speciosa on gastric tissue glycoprotein-PAS staining in ethanol-induced gastric ulcers in rats.
(G1) (Normal control group); (G2) (Ulcer control group); (G3) (Omeprazole); (G4) (50 mg/kg), (G5) (100 mg/kg), (G6) (200 mg/kg), (G7) (400 mg/kg) Parkia speciosa extract (PAS stain 20×). Figure 4G1 is excluded from this article's CC BY license. See the accompanying retraction notice for more information.
Immunohistochemistry
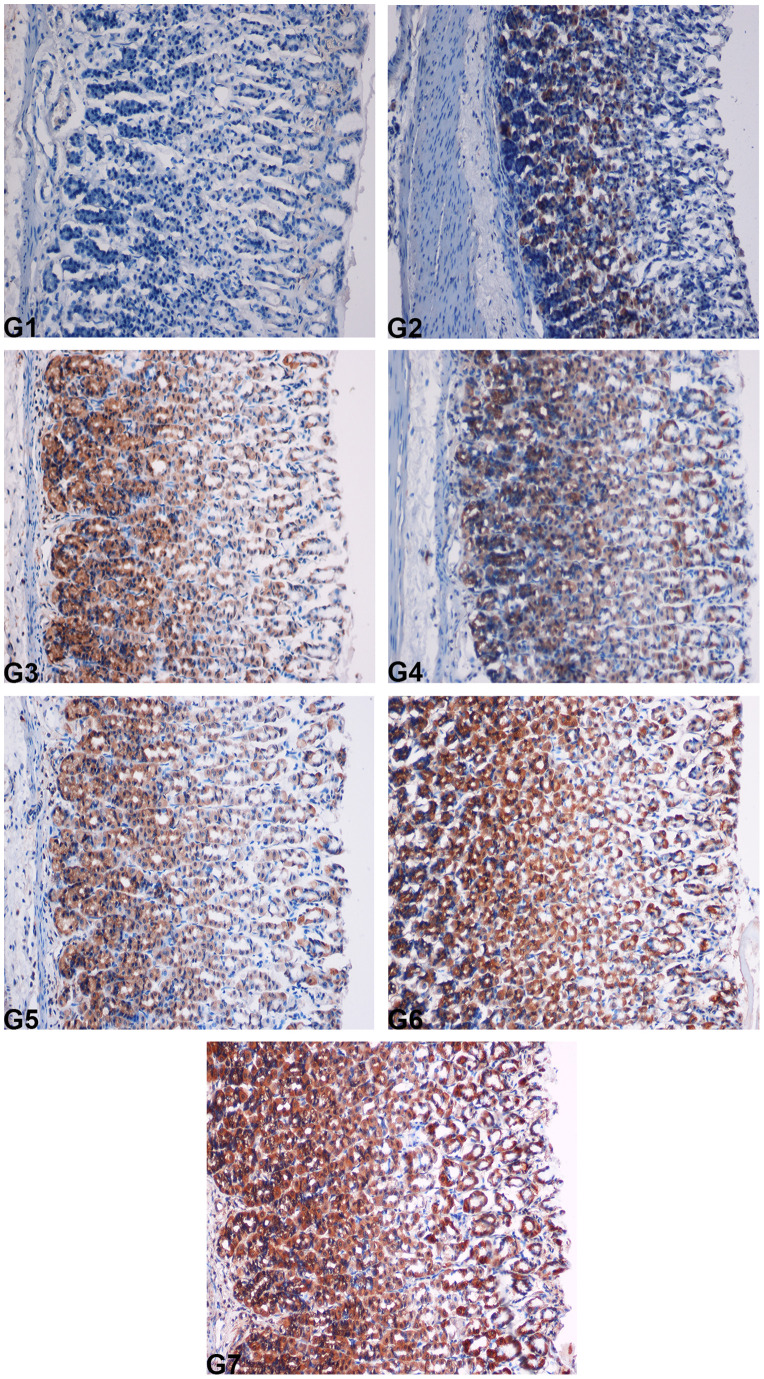
The expression of the HSP70 protein in the gastric mucosa was downregulated in group 2 but upregulated in group 3–7 (Figure 5).
Figure 5. Immunohistochemical analysis of HSP70 expression in the gastric mucosa of rats.
(G1) (Normal control group); (G2) (Ulcer control group); (G3) (Omeprazole); (G4) (50 mg/kg), (G5) (100 mg/kg), (G6) (200 mg/kg), (G7) (400 mg/kg) Parkia speciosa extract. HSP70 protein expression was upregulated in rats pretreated with Parkia speciosa (magnification 20×).
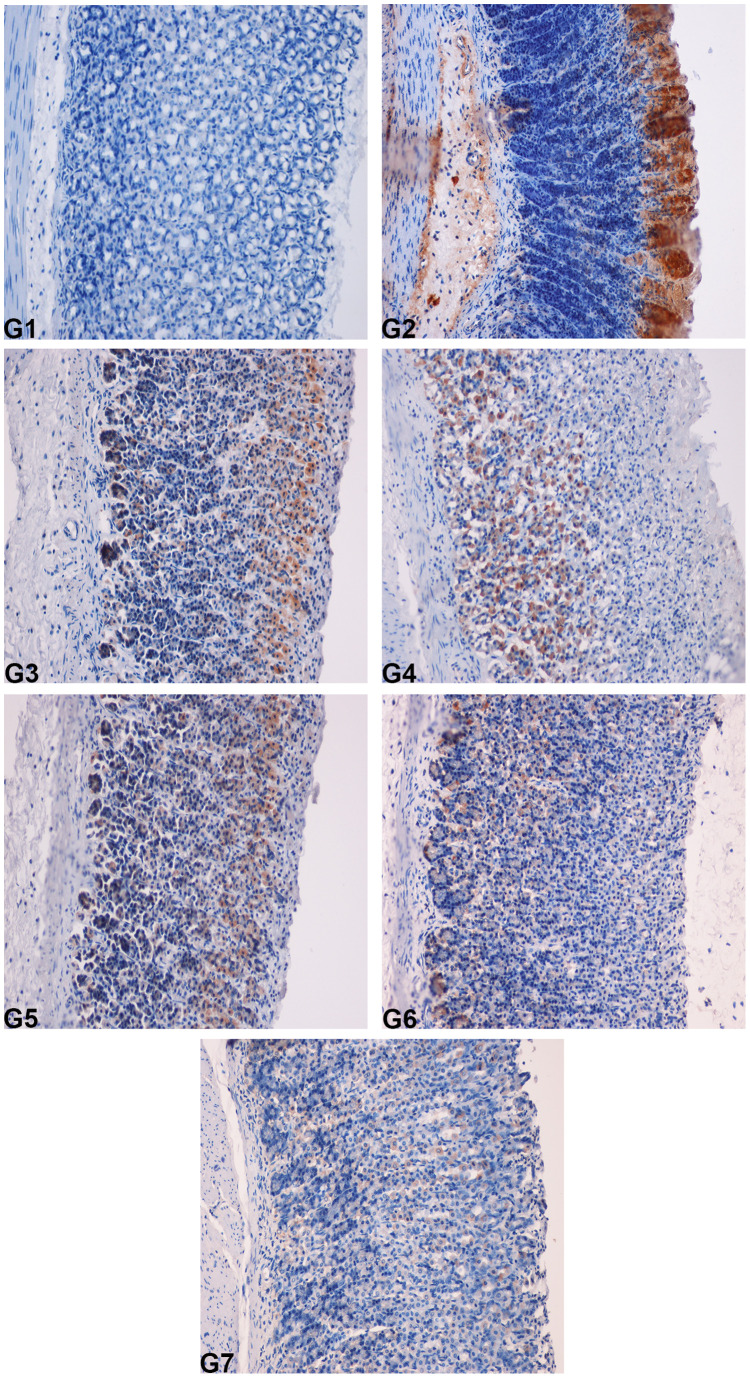
Immunohistochemical staining of the gastric mucosa of rats pretreated with Parkia speciosa extract or omeprazole demonstrated a downregulation of the BAX protein (Figure 6). In addition, the levels of BAX protein in group 2 rats were higher than those of groups 3–7 (Figure 6).
Figure 6. Immunohistochemical analysis of the expression of the BAX protein in the gastric mucosa of rats.
(G1) (Normal control group); (G2) (Ulcer control group); (G3) (Omeprazole); (G4) (50 mg/kg), (G5) (100 mg/kg), (G6) (200 mg/kg), (G7) (400 mg/kg) Parkia speciosa extract. BAX protein expression was downregulated in rats pretreated with Parkia speciosa (magnification 20×).
Discussion
The acute toxicity test did not suggest any toxicity or mortality in the P. speciosa-treated rats. This test revealed that the plant is safe and has no toxicity when administered orally up to 5 g/kg. Certain antiulcer drugs have been reported to increase the amount of gastric mucus secretion in the gastric mucosa [29]. Pretreatment with Parkia speciosa extract significantly increased the gastric mucus content in rats with ethanol-induced ulcers, indicating that the gastroprotective effect of Parkia speciosa is mediated partly by preservation of the gastric wall mucus. This mucus consists of mucin-type glycoproteins, which can be detected by Alcian blue [30]; the increase in Alcian blue staining demonstrates the protective effect of orally administered Parkia speciosa, which may be mediated by the formation of protective complexes between Parkia speciosa and the mucus that acts as a barrier against necrotizing agents introduced to the stomach [31]. Here, the Parkia speciosa extract prevented the decrease in the concentration of gastric wall mucus upon treatment with ethanol. Thus, one possible mechanism by which the gastric mucosa is protected by Parkia speciosa involves the reinforcement of the mucosal barrier resistance, generated by a protective coating. It is likely that the protective effect of Parkia speciosa is due at least in part to the preservation of the mucus layer in the gastric mucosa; Parkia speciosa was observed to prevent ethanol-induced gastric wall mucus depletion. The results of the present study demonstrated that Parkia speciosa extract has an effective antiulcer activity against ethanol-induced gastric mucosal injury. The plant extract increased the mucus content of the gastric wall, which is consistent with results reported by Thirunavukkarasu et al. [32].
Our results revealed the protection of the gastric mucosa and inhibition of leucocyte infiltration into the gastric wall in rats pretreated with Parkia speciosa extract. The activation and infiltration of neutrophils appear to be involved in the initial processes that form these lesions. Similarly, Abdulla et al. [12] demonstrated that the reduction of neutrophil infiltration into ulcerated gastric tissues helped to prevent gastric ulcers in rats. Wasman et al. [33] showed that the oral administration of plant extract prior to ethanol administration significantly decreased neutrophil infiltration into the gastric mucosa. Ethanol causes extensive damage to the gastric mucosa and leads to increased neutrophil infiltration into this tissue.
The present study established that pretreatment with Parkia speciosa reduced neutrophil infiltration into ulcerated tissue. We also observed a flattening of the mucosal folds, which suggests that the gastroprotective effect of the Parkia speciosa leaf extract might be attributed to a decrease in gastric motility. Changes in gastric motility have been implicated in the development and prevention of experimental gastric lesions. The relaxation of the circular muscles may protect the gastric mucosa through a flattening of the folds. This flattening increases the mucosal area exposed to necrotizing agents and reduces the volume of the gastric irritants that come into contact with the rugal crest [12], [33].
Gastric tissue homogenate prepared from the groups that were pretreated with plant extract exhibited significant antioxidant activity, with decreased levels of MDA and elevated levels of GSH and SOD, in response to oxidative stress due to ethanol treatment. SOD converts superoxide to hydrogen peroxide (H2O2), which is transformed into water by catalase in the lysosomes or by glutathione peroxidase in the mitochondria [34]. MDA is the final product of lipid peroxidation and is used to determine lipid peroxidation levels [35]. Lipid peroxidation causes a loss of membrane fluidity, impaired ion transport and membrane integrity and ultimately a loss of cellular function.
Our experimental results indicate that Parkia speciosa ethanolic extract significantly inhibited the negative effects of ethanol on gastric GSH levels at all doses used. The gastric GSH level was highest for the 400 mg/kg dose and lowest for the 50 mg/kg dose, while the GSH level was decreased in the ulcer control group. The current results and previously published articles indicate that there is an important relationship between gastric GSH levels and ulcer severity. GSH and GSH-related enzymes are known as important tissue protective agents due to their antioxidant properties [36], [37].
The periodic acid-Schiff (PAS) histochemical method produces a characteristic carmine staining in stomach regions that secrete mucopolysaccharides. Tissue sections from the group of rats that was treated with 400 mg/kg plant extract showed intense staining reflecting mucus secretion in the gastric glands. Mucus production is one of the major mechanisms of local gastric mucosal defense [38].
BAX promotes apoptosis [39], while BCL-2 inhibits this process. Apoptosis may be caused by an imbalance in the expression of BCL-2 family antiapoptotic proteins and apoptotic BAX proteins in stress ulcers [40]. HSP70 is a 70 kDa protein from the HSP family that is expressed in mammalian cells. These proteins are responsible for protecting cellular homeostatic processes from environmental and physiologic injuries by preserving the structure of normal proteins and repairing or removing damaged proteins [41], and the study of this protein can thus provide interesting data for the elucidation of possible mechanisms of action. HSP70 defends cells from oxidative stress or heat shock. Ethanol-generated reactive oxygen species (ROS) normally act to inhibit the expression of HSP70 and increase the expression of BAX. HSP70 prevents these partially denatured proteins from aggregating and allows them to refold. The upregulation of HSP70 that was observed in this study suggests that the Parkia speciosa extract protected the gastric tissues through the upregulation of HSP70. Additionally, HSP70 has been suggested to exert its cytoprotective activity by protecting mitochondria and interfering with the stress-induced apoptotic program. Immunohistochemical staining showed that BAX protein expression was downregulated in rats pretreated with Parkia speciosa extract.
Conclusion
In conclusion, P. speciosa extract was clearly demonstrated to function as an antiulcer agent. The results suggest that the P. speciosa extract may act by enhancing the gastric mucosal defense and/or by inhibiting leukotriene synthesis. The plant extract protected the gastric tissues through the upregulation of the HSP70 and downregulation of the BAX protein. Parkia speciosa reversed the decrease in PAS staining induced by ethanol, significantly increased the GSH and SOD activities, and decreased the level of lipid peroxidation (MDA) in the P. speciosa-pretreated groups.
Acknowledgments
The authors are thankful to the staff of Faculty of Medicine, and Animal House for the care and supply of rats and to others who participated in this work.
Funding Statement
The authors express gratitude to the University of Malaya for the financial support of UM/MOHE High Impact Research Grant (HIR Grant No. F000009-21001). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Yeomans ND, Hawkey CJ, Brailsford W, Næsdal J (2009) Gastroduodenal toxicity of low-dose acetylsalicylic acid: a comparison with non-steroidal anti-inflammatory drugs. Current Medical Research & Opinion 25: 2785–2793. [DOI] [PubMed] [Google Scholar]
- 2.Yuan L, Wang JH, Sun TM (2010) Total synthesis and anticancer activity studies of the stereoisomers of asperphenamate and patriscabratine. Chinese Chemical Letters 21: 155–158. [Google Scholar]
- 3.Itatsu T, Nagahara A, Hojo M, Miyazaki A, Murai T, et al. (2011) Use of selective serotonin reuptake inhibitors and upper gastrointestinal disease. Internal Medicine 50: 713–717. [DOI] [PubMed] [Google Scholar]
- 4.Søberg T, Hofstad B, Sandvik L, Johansen M, Lygren I (2010) Risk factors for peptic ulcer bleeding. Tidsskrift for den Norske Laegeforening: Tidsskrift for Praktisk Medicin, ny Raekke 130: 1135–1139. [DOI] [PubMed] [Google Scholar]
- 5.Lanas A (2009) Nonsteroidal antiinflammatory drugs and cyclooxygenase inhibition in the gastrointestinal tract: a trip from peptic ulcer to colon cancer. The American Journal of the Medical Sciences 338: 96. [DOI] [PubMed] [Google Scholar]
- 6.Maity P, Biswas K, Roy S, Banerjee RK, Bandyopadhyay U (2003) Smoking and the pathogenesis of gastroduodenal ulcer–recent mechanistic update. Molecular and Cellular Biochemistry 253: 329–338. [DOI] [PubMed] [Google Scholar]
- 7.Kushima H, Hiruma-Lima CA, Santos MA, Viana E, Coelho-Ferreira M, et al. (2005) Gastroprotective activity of Pradosia huberi on experimentally induced gastric lesions in rodents: Role of endogenous sulphydryls and nitric oxide. Journal of Ethnopharmacology 101: 61–67. [DOI] [PubMed] [Google Scholar]
- 8.Marhuenda E, Martin M, Alarcon Lastra C (1993) Antiulcerogenic activity of aescine in different experimental models. Phytotherapy Research 7: 13–16. [Google Scholar]
- 9.Davenport H (1968) Destruction of the gastric mucosal barrier by detergents and urea. Gastroenterology 54: 175. [PubMed] [Google Scholar]
- 10.Jainu M, Mohan KV, Devi CSS (2006) Gastroprotective effect of Cissus quadrangularis extract in rats with experimentally induced ulcer. Indian Journal of Medical Research 123: 799. [PubMed] [Google Scholar]
- 11.Lukie BE, Forstner GG (1972) Synthesis of intestinal clycoproteins inhibition of [1–14C]glucosamine incorporation by sodium salicylate in vitro. Biochimica et Biophysica Acta (BBA) - General Subjects 273: 380–388. [DOI] [PubMed] [Google Scholar]
- 12.Abdulla MA, Ahmed KAA, Al-Bayaty FH, Masood Y (2010) Gastroprotective effect of Phyllanthus niruri leaf extract against ethanol-induced gastric mucosal injury in rats. African Journal of Pharmacy and Pharmacology 4: 226–230. [Google Scholar]
- 13.Abdelwahab SI, Mohan S, Mohamed Elhassan M, Al-Mekhlafi N, Mariod AA, et al.. (2010) Antiapoptotic and antioxidant properties of Orthosiphon stamineus Benth (cat’s whiskers): intervention in the Bcl-2-mediated apoptotic pathway. Evidence-Based Complementary and Alternative Medicine 2011. [DOI] [PMC free article] [PubMed] [Retracted]
- 14.Wasman S, Mahmood A, Suan Chua L, Alshawsh MA, Hamdan S (2011) Antioxidant and gastroprotective activities of Andrographis paniculata (Hempedu Bumi) in Sprague Dawley rats. Indian Journal of Experimental Biology 49: 767. [PubMed] [Google Scholar]
- 15.Gan CY, Latiff AA (2011) Optimisation of the solvent extraction of bioactive compounds from Parkia speciosa pod using response surface methodology. Food Chemistry 124: 1277–1283. [Google Scholar]
- 16.Ching LS, Mohamed S (2001) Alpha-tocopherol content in 62 edible tropical plants. Journal of Agricultural and food Chemistry 49: 3101–3105. [DOI] [PubMed] [Google Scholar]
- 17.Mahmood A, Mariod AA, Al-Bayaty F, Abdel-Wahab SI (2010) Anti-ulcerogenic activity of Gynura procumbens leaf extract against experimentally-induced gastric lesions in rats. J Med Plants Res 4: 685–691. [Google Scholar]
- 18.Mahmood A, Al-Bayaty F, Salmah I, Syuhada ABN, Harita H, et al. (2011) Enhancement of gastric ulcer by Areca catechu nut in ethanol-induced gastric mucosal injuries in rats. Journal of Medicinal Plant Research 5: 2562–2569. [Google Scholar]
- 19.CHEMICALS D (2005) OECD Guideline for testing of chemicals.
- 20.Resources IoLA (1996) Guide for the care and use of laboratory animals: National Academies Press. [PubMed]
- 21.Shay H (1945) A simple method for the uniform production of gastric ulceration in the rat. Gastroenterology 4: 43–61. [Google Scholar]
- 22.Piper D, Whitecross D, Leonard P, Clarke A (1970) Alcian blue binding properties of gastric juice. Gastroenterology 59: 534. [PubMed] [Google Scholar]
- 23.Bardi D, Khan MAS, Sabri S, Kadir F, Mahmood A, et al. (2011) Anti-ulcerogenic activity of Typhonium flagelliforme aqueous leaf extract against ethanol-induced gastric mucosal injury in rats. Scientific Research and Essays 6: 3232–3239. [Google Scholar]
- 24.Sun Y, Oberley LW, Li Y (1988) A simple method for clinical assay of superoxide dismutase. Clinical Chemistry 34: 497–500. [PubMed] [Google Scholar]
- 25.Draper H, Hadley M (1990) Malondialdehyde determination as index of lipid peroxidation. Methods in enzymology 186: 421. [DOI] [PubMed] [Google Scholar]
- 26.Sedlak J, Lindsay RH (1968) Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman’s reagent. Analytical biochemistry 25: 192. [DOI] [PubMed] [Google Scholar]
- 27.Behmer OA (1976) Manual de técnicas para histologia normal e patológica: EDART/USP.
- 28.McManus J (1948) Histological and histochemical uses of periodic acid. Biotechnic & Histochemistry 23: 99–108. [DOI] [PubMed] [Google Scholar]
- 29.Robert A, Böttcher W, Golanska E, Kauffman Jr G (1984) Lack of correlation between mucus gel thickness and gastric cytoprotection in rats. Gastroenterology 86: 670. [PubMed] [Google Scholar]
- 30.Bolton JP, Palmer D, Cohen MM (1978) Stimulation of mucus and nonparietal cell secretion by the E 2 prostaglandins. Digestive Diseases and Sciences 23: 359–364. [DOI] [PubMed] [Google Scholar]
- 31.Clamp J, Allen A, Gibbons R, Roberts G (1978) Chemical aspects of mucus. British medical bulletin 34: 25–41. [DOI] [PubMed] [Google Scholar]
- 33.Wasman S, Mahmood A, Salehhuddin H, Zahra A, Salmah I (2010) Cytoprotective activities of Polygonum minus aqueous leaf extract on ethanol-induced gastric ulcer in rats. J Med Plants Res 4: 2658–2665. [Google Scholar]
- 34.Johansen JS, Harris AK, Rychly DJ, Ergul A (2005) Oxidative stress and the use of antioxidants in diabetes: linking basic science to clinical practice. Cardiovascular Diabetology 4: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dursun H, Bilici M, Albayrak F, Ozturk C, Saglam MB, et al. (2009) Antiulcer activity of fluvoxamine in rats and its effect on oxidant and antioxidant parameters in stomach tissue. BMC gastroenterology 9: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Repetto M, Llesuy S (2002) Antioxidant properties of natural compounds used in popular medicine for gastric ulcers. Brazilian Journal of Medical and Biological Research 35: 523–534. [DOI] [PubMed] [Google Scholar]
- 37.La Casa C, Villegas I, Alarcon de La Lastra C, Motilva V, Martın Calero M (2000) Evidence for protective and antioxidant properties of rutin, a natural flavone, against ethanol induced gastric lesions. Journal of Ethnopharmacology 71: 45–53. [DOI] [PubMed] [Google Scholar]
- 38.Laine L, Takeuchi K, Tarnawski A (2008) Gastric mucosal defense and cytoprotection: bench to bedside. Gastroenterology 135: 41–60. [DOI] [PubMed] [Google Scholar]
- 39.Emily HYAC, Wei MC, Weiler S, Flavell RA, Mak TW, et al. (2001) BCL-2, BCL-XL sequester BH3 domain-only molecules preventing BAX-and BAK-mediated mitochondrial apoptosis. Molecular Cell 8: 705–711. [DOI] [PubMed] [Google Scholar]
- 40.Konturek PC, Brzozowski T, Konturek S, Pajdo R, Konturek J, et al. (1999) Apoptosis in gastric mucosa with stress-induced gastric ulcers. Journal of Physiology and Pharmacology: An Official Journal of the Polish Physiological Society 50: 211. [PubMed] [Google Scholar]
- 41.Tytell1 M, Hooper PL (2001) Heat shock proteins: new keys to the development of cytoprotective therapies. Emerging Therapeutic Targets 5: 267–287. [DOI] [PubMed] [Google Scholar]