Abstract
Introduction
Informing children of their own HIV status is an important aspect of long-term disease management, yet there is little evidence of how and when this type of disclosure takes place in resource-limited settings and its impact.
Methods
MEDLINE, EMBASE and Cochrane Databases were searched for the terms hiv AND disclos* AND (child* OR adolesc*). We reviewed 934 article citations and the references of relevant articles to find articles describing disclosure to children and adolescents in resource-limited settings. Data were extracted regarding prevalence of disclosure, factors influencing disclosure, process of disclosure and impact of disclosure on children and caregivers.
Results
Thirty-two articles met the inclusion criteria, with 16 reporting prevalence of disclosure. Of these 16 studies, proportions of disclosed children ranged from 0 to 69.2%. Important factors influencing disclosure included the child's age and perceived ability to understand the meaning of HIV infection and factors related to caregivers, such as education level, openness about their own HIV status and beliefs about children's capacities. Common barriers to disclosure were fear that the child would disclose HIV status to others, fear of stigma and concerns for children's emotional or physical health. Disclosure was mostly led by caregivers and conceptualized as a one-time event, while others described it as a gradual process. Few studies measured the impact of disclosure on children. Findings suggested adherence to antiretroviral therapy (ART) improved post-disclosure but the emotional and psychological effects of disclosure were variable.
Conclusions
Most studies show that a minority of HIV-infected children in resource-limited settings know his/her HIV status. While caregivers identify many factors that influence disclosure, studies suggest both positive and negative effects for children. More research is needed to implement age- and culture-appropriate disclosure in resource-limited settings.
Keywords: HIV, disclosure, children, resource-limited settings, systematic review
Introduction
Of the 3.4 million children under the age of 15 years living with HIV worldwide [1], almost 90% live in sub-Saharan Africa [2]. Increasing numbers of these children have access to antiretroviral therapy (ART) and improved prognoses for survival [3]. This requires healthcare systems in resource-limited settings to address challenges, such as maintaining medication adherence, responding to the psychosocial implications of HIV infection, life-skills training and supporting long-term disease management. As more of these children reach adolescence and adulthood, another important challenge is determining how and when to inform children about their HIV status [4,5].
One definition of disclosure refers to a child gaining knowledge of his/her HIV status [6]. For the purposes of this review, we focus on this type of disclosure, while acknowledging paediatric disclosure can also refer to disclosure of caregivers’ HIV status to children [7,8] or a child's disclosure of their own HIV status to others [9,10]. Recommendations for disclosure in the United States endorse a gradual process of giving children age-appropriate information regarding their illness, leading to full disclosure when the child has the cognitive and emotional maturity to process this information [4,6,11,12].
The effects of disclosure are not well studied. While some studies from resource-rich settings show that disclosure is associated with higher self-esteem, fewer symptoms of depression, improved adherence and higher CD4 counts [13–17], other studies do not [18–21]. Furthermore, many studies to date have utilized cross-sectional designs and cannot adequately assess the impact of disclosure on clinical or psychosocial characteristics [6]. Other studies suggest that HIV-infected children who know their status may be better able to seek social support, have improved coping skills [11,22] and practice safer sexual practices to prevent secondary transmission [23,24].
Disclosure is crucial to long-term disease management [12], yet how and when caregivers and healthcare professionals in resource-limited settings disclose to children are not well-characterized and the number of children that know their status is generally thought to be low. Moreover, many of these settings currently lack standardized, culturally appropriate guidelines and resources for undertaking disclosure [25]. While organizations such as the World Health Organization and Médecins Sans Frontières have published recommendations for disclosure of HIV status to children, they do not have a broad evidence base and are not context-specific with considerations of different cultural views on age, maturity and psychosocial development [26–28]. This systematic review aims to estimate the prevalence of HIV disclosure among children in low- and middle-income countries, to examine factors influencing paediatric disclosure, including barriers to and advantages of disclosure, and to assess the impact of disclosure on children's physical and emotional health in these settings.
Methods
We searched several bibliographic databases, including MEDLINE (January 1, 1966–November 23, 2011), EMBASE (Inception–October 30, 2011), Cochrane Central Register of Controlled Trials (CENTRAL) (Inception–November 23, 2011) and Cochrane Database of Systematic Reviews (Inception–November 23, 2011). We used the search strategy: hiv AND disclos* AND (child* OR adolesc*). Two authors (RCV and AMG) reviewed the titles of all returned articles to determine which studies examined HIV status disclosure to children in resource-limited settings. A structured data extraction tool was used to evaluate all articles. Search terms were only entered in English; articles written in English, French, Spanish, or Portuguese were reviewed. Articles were immediately excluded if they did not involve HIV disclosure, children or adolescents, were not conducted in a resource-limited setting, or were not in English, French, Spanish, or Portuguese. We also searched the bibliographies of the retrieved studies and relevant review articles.
Two authors (RCV and AMG) independently reviewed the articles to determine inclusion. Disagreements were resolved by consensus. For inclusion, the study needed to describe disclosure of HIV status to HIV-infected children or adolescents aged 18 years or less. In addition, the studies needed to be conducted in a resource-limited setting, defined as a low- or middle-income country using the World Bank classification [29]. Studies describing populations of HIV-infected individuals over 18 years of age were included if they also had data on individuals younger than 18 years. Studies that focused only on disclosure of the parent's HIV status to children were excluded, as were studies that focused on disclosure of a child's HIV status to community members, schools, or other individuals, without disclosure to the child. Each article was analyzed to determine the sample characteristics, study setting, definition of and prevalence of disclosure, reasons for and against disclosure, outcomes of disclosure, and the process and method of disclosure.
Results
Studies of paediatric HIV disclosure in resource-limited settings
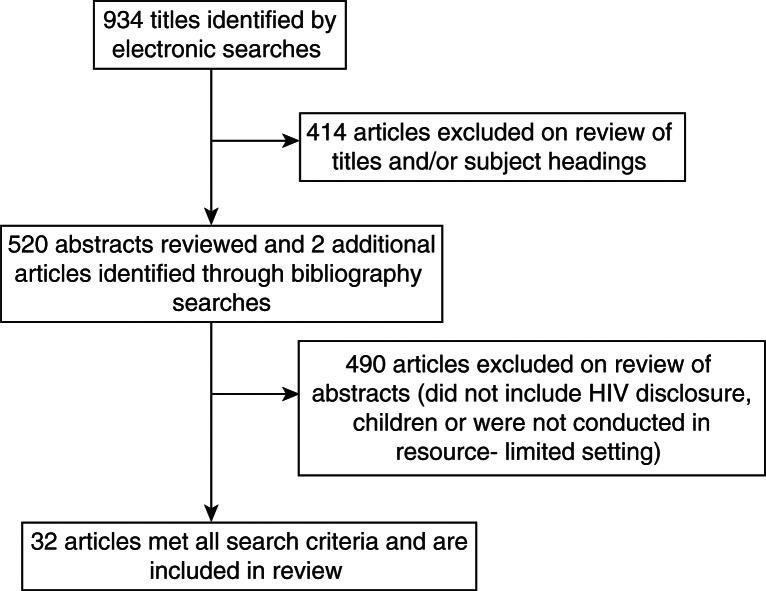
The systematic literature search identified 934 articles (Figure 1). Once articles whose titles alone indicated that they did not address disclosure to HIV-infected children were excluded, 520 articles remained, for which abstracts and then full-text articles were reviewed. Two additional studies were identified through searches of bibliographies [30,31]. Thirty-two articles met all search criteria and were included in this systematic review.
Figure 1.
Flow diagram of phases of paediatric disclosure systematic review.
From the thirty-two articles describing HIV disclosure to paediatric patients in resource-limited settings, we extracted data on the location, setting, sample size, study design, population characteristics and prevalence of disclosure (Table 1). Two articles described the same study population [32,33] and therefore were considered a single-study population for this review; however, we make reference to both articles where appropriate due to unique findings. Twenty-one of the studies were conducted in Africa [30,32,34–51] with the remaining primarily from Asia and South America. Most studies relied on small samples, with the largest two studies including 492 HIV-infected children and adolescents [48] and 390 caregivers [44]. Eighteen studies used a qualitative study design including interviews or focus groups [30,32,34,35,37,39–43,47,49,51–56]. Six studies included only children and adolescents [17,31,48,50,53,57] and eight studies included only caregivers (parents or guardians) [25,37,38,42,45,51,55,58]. Ten studies included children and caregivers [30,36,40,41,44,49,52,54,56,59], while seven studies also included healthcare professionals [32,34,35,39,43,46,47].
Table 1.
Study characteristics
| Study | Title | Location | Setting | Study design | Population | Sample size (N) | Children's age range and/or mean or median age (SD) | Proportions of disclosed children |
|---|---|---|---|---|---|---|---|---|
| Abadia-Barrero and Larusso, 2006 | The disclosure model versus a developmental illness experience model for children and adolescents living with HIV/AIDS in Sao Paulo, Brazil | Sao Paulo, Brazil | Home | Qualitative | Children | 36 | 1–15 years | N/A |
| Arun et al., 2009 | Disclosure of the HIV infection status in children | New Delhi, India | Hospital | Qualitative | Caregivers | 50 | Mean: 8.98 (0.42) | 14% |
| Bhattacharya et al., 2010 | Patterns of diagnosis disclosure and its correlates in HIV-infected North Indian children | Northern India | Hospital | Cross-sectional | Caregiver-child dyads | 290 (145 children, 145 caregivers) | >5 years; mean: 9.1 (2.5) | 41.4% |
| Biadgilign et al., 2009 | Barriers and facilitators to antiretroviral medication adherence among HIV-infected paediatric patients in Ethiopia: a qualitative study | Addis Ababa, Ethiopia | Hospital | Qualitative | Caregivers, health professionals | 26 (12 caregivers, 14 health professionals) | 1–14 years; mean: 8.52 (2.97) | N/A |
| Biadgilign et al., 2011 | Factors associated with HIV/AIDS diagnostic disclosure to HIV infected children receiving HAART: a multi-center study in Addis Ababa, Ethiopia | Addis Ababa, Ethiopia | Hospital | Cross-sectional | Caregiver-child dyads | 780 (390 children, 390 caregivers) | 1–14 years; mean: 8.52 (2.97) | 17.4% (by age: 5.9% 0–5 years, 41.2% 6–9 years, 52.9% 10–14 years) |
| Bikaako-Kajura et al., 2006 | Disclosure of HIV status and adherence to daily drugs regimens among HIV-infected children in Uganda | Kampala, Uganda | Clinic | Qualitative | Caregiver-child dyads | 84 (42 children and 42 caregivers) | 5–17 years; median: 12 | 29% complete parental disclosure, 38% partial disclosure |
| Boon-Yashidi et al., 2005 | Diagnosis disclosure in HIV-infected Thai Children | Bangkok, Thailand | Hospital | Qualitative | Children and caregivers | 115 (19 children, 96 caregivers) | 5–15 years; mean: 9.6 | 19.8% (in sample of 96 children. Only disclosed sample – 19 children – were included in qualitative analysis) |
| Brown et al., 2011 | Disclosure of HIV status to infected children in a Nigerian HIV care programme | Ibadan, Nigeria | Clinic | Cross-sectional | Caregivers | 96 | 6–14 years; mean: 8.8 (2.2) | 13.5% |
| *Corneli et al., 2009 | The role of disclosure in relation to assent to participate in HIV-related research among HIV-infected youth: a formative study | Kinshasa, DRC | Clinic | Qualitative | Children, caregivers, health professionals | 72 (19 children, 36 caregivers, 17 health professionals) | 11–21 years; median: 16 | N/A |
| De Baets et al., 2008 | HIV disclosure and discussions about grief with Shona children: a comparison between healthcare workers and community members in Eastern Zimbabwe | Eastern Zimbabwe | Hospital and clinic | Qualitative | Health professionals, community members | 195 (64 health professionals, 131 community members) | Not reported | N/A |
| Demmer, 2011 | Experiences of families caring for an HIV-infected child in KwaZulu-Natal, South Africa: an exploratory study | KwaZulu-Natal, South Africa | Clinic and home | Qualitative | Caregivers, health professionals | 25 (13 caregivers, 12 health professionals) | Not reported | N/A |
| Feinstein et al., 2010 | Effect of disclosure on HIV status to children receiving ART on six-month virologic suppression | Soweto, South Africa | Unspecified | Prospective cohort | Children | 492 | 4–18 years | 3% (children aged 4–6 years); 17% (children aged 7–10 years); 77% (children ≥11 years) |
| Ferris et al., 2007 | The influence of disclosure of HIV diagnosis on time to disease progression in a cohort of Romanian children and teens | Constanta, Romania | Clinic | Retrospective cohort | Children | 325 | 5–17 years; mean: 13.5 (1.5) | 69.2% |
| Fetzer et al., 2011 | Barriers to and facilitators of adherence to pediatric antiretroviral therapy in a sub-Saharan setting: insights from a qualitative study | Kinshasa, DRC | Hospital | Qualitative | Caregiver-child dyads | 40 (20 children, 20 caregivers) | 9–17 years; median: 14 | 20.0% |
| Haberer et al., 2011 | Excellent adherence to antiretrovirals in HIV+ Zambian children is compromised by disrupted routine, HIV nondisclosure, and paradoxical income effects | Lusaka, Zambia | Clinic and home | Prospective cohort | Children | 96 | Median 6 (IQR 2, 9) | 2.0% |
| Hejoaka, 2009 | Care and secrecy: being a mother of children living with HIV in Burkina Faso | Burkina Faso | Hospital | Qualitative | Children, caregivers, health professionals | 57 (15 children, 20 caregivers, 22 health professionals) | 8–18 years | N/A |
| Kallem et al., 2010 | Prevalence and pattern of disclosure of HIV status in HIV-infected children in Ghana | Accra, Ghana | Hospital | Cross-sectional | Caregiver-child dyads | 142 (71 children, 71 caregivers) | 8–14 years; mean: 10.42 (1.72) | 21% |
| Kouyoumdjiam et al., 2005 | Barriers to disclosure to children with HIV | Soweto, South Africa | Clinic | Qualitative | Caregivers | 17 | Not reported | N/A |
| Lee and Oberdorfer, 2009 | Risk-taking behaviors among vertically HIV-infected adolescents in northern Thailand | Northern Thailand | Hospital | Qualitative | Children | 54 | ≥ 13 years; median 14.6 (IQR 13.8, 16.1) | N/A |
| Marques et al., 2006 | Disclosure of HIV infection from the perspective of adolescents living with HIV/AIDS and their parents and caregivers | Sao Paulo and Santos, Brazil | Clinic | Qualitative | Children, caregivers | 46 (22 children, 24 caregivers) | 10–20 years | N/A |
| Menon et al., 2007 | Mental health and disclosure of HIV status in Zambian adolescents with HIV Infection | Lusaka, Zambia | Hospital and clinic | Cross-sectional | Children | 127 | 11–15 years; Mean 12.4 (1.4) | 37.8% |
| Moodley et al., 2006 | Paediatric HIV disclosure in South Africa – caregivers’ perspectives on discussing HIV with infection children | Cape Town, South Africa | Hospital | Qualitative | Caregivers | 174 | 0–11 years; median: 3.3 | 9% overall; 26% in children older than 6 years |
| Myer et al., 2006 | Healthcare providers’ perspectives on discussing HIV status with infected children | Cape Town, South Africa | Hospital | Qualitative | Health professionals | 40 | Not reported | N/A |
| Oberdorfer et al., 2006 | Disclosure of HIV/AIDS diagnosis to HIV-infected children in Thailand | Northern Thailand | Hospital | Cross-sectional | Caregivers | 103 | 6–16 years; mean: 9.5 | 30% |
| Petersen et al., 2010 | Psychosocial challenges and protective influences for socio-emotional coping of HIV+ adolescents in South Africa: a qualitative investigation | Durban, South Africa | Hospital | Qualitative | Children, caregivers | 40 (25 children, 15 caregivers) | 14–16 years | N/A |
| Punpanich et al., 2008 | Understanding the psychosocial needs of HIV-infected children and families: a qualitative study | Bangkok, Thailand | Hospital | Qualitative | Children, caregivers | 69 (34 children, 35 caregivers) | 8–16 years; mean: 12.5 (2.2) | N/A |
| Schaurich, 2011 | Disclosure of AIDS diagnosis to children from the family members’ perspective | Porto Alegre, Brazil | Clinic | Qualitative | Caregivers | 7 | Not reported | N/A |
| *Vaz et al., 2008 | The process of HIV status disclosure to HIV-positive youth in Kinshasa, DRC | Kinshasa, DRC | Clinic | Qualitative | Children, caregivers | 40 (19 children, 21 caregivers) | 10–21 years; mean: 16.1 | N/A |
| Vaz et al., 2010 | Telling children they have HIV: lessons learned from findings of a qualitative study in Sub-Saharan Africa | Kinshasa, DRC | Clinic | Qualitative | Caregiver-child dyads | 16 (7 children, 9 caregivers) | 8–17 years | In recruitment, screened 259 children and 8 (3%) had been told their HIV status |
| Vaz et al., 2011 | Patterns of Diagnosis Disclosure of HIV Status to Infected Children in a Sub-Saharan African Setting | Kinshasa, DRC | Clinic | Qualitative | Caregivers | 201 | 5–17 years; median: 8 | N/A |
| Vreeman et al., 2010 | The perceived impact of disclosure of pediatric HIV status on pediatric antiretroviral therapy adherence, child well-being, and social relationships in a resource-limited setting | Western Kenya | Hospital | Qualitative | Caregivers | 120 | 0–14 years; mean: 6.8 | 1.7% |
| Yeap et al., 2010 | Factors influencing uptake of HIV care and treatment among children in South Africa – a qualitative study of caregivers and clinic staff | Gauteng Province, South Africa | Clinic | Qualitative | Caregivers, health professionals | 42 (21 caregivers, 21 health professionals) | Not reported | N/A |
Articles describe the same study population.
Some studies defined disclosure generally, using some variant of the concept of children knowing their HIV status [25,34,46,51,56–58], while other studies used a more stringent definition, considering disclosure to have occurred only if there was confirmation that the terms “HIV” or “AIDS” had been used with or specifically mentioned by the child [17,30,32,36,41,45,54,59]. Six studies required a child to have been informed of their status before participating in the study [32,35,40,41,56,57], ensuring that 100% of the sample had been disclosed to, but eliminating the possibility of providing an estimate of disclosure prevalence. Sixteen studies reported proportions of disclosed children for their study population [17,25,30,31,34,36,38,45,48–52,54,58,59], ranging from 0 to 69.2%. Few studies included appropriate sampling methods and scientific design to estimate disclosure prevalence and were not designed to evaluate the impact of disclosure. Most studies reporting disclosure prevalence were cross-sectional in design and employed non-randomized, small, convenience samples of various age ranges of children and adolescents.
Factors influencing paediatric HIV disclosure
Studies identified multiple factors influencing whether disclosure occurred, many of which were described through qualitative inquiry. Most factors shaping disclosure were at the level of the child or the caregiver (Table 2). Child characteristics considered important to disclosure included the child's age [17,25,31–33,36–42,44,45,51,53,54,58], gender [46], education level [36,39,42,59], medication responsibilities [36], whether the child asks questions [35,37,41,42,51,55,56], and their perceived ability to understand their diagnosis [37,39,40,44,46,47,51,53,54]. The prevalence of disclosure varied most dramatically based on the age of the population, with most children not knowing their HIV status until older ages. For example, in a sample of 492 HIV-infected children in South Africa, 3% of four- to six-year olds knew their status, compared to 17% of seven- to ten-year olds and 77% of those aged 11 years and older [48]. The child's clinical status [32] also influenced disclosure. Receiving ART [31,59], a longer duration of enrolment in clinic or on ART [36,59] and the child having a lower CD4 count [25] were associated with a greater likelihood of disclosure.
Table 2.
Child and caregiver factors influencing disclosure
| Characteristics of the child influencing disclosure | Description of child-related factors |
|---|---|
| Child's age |
|
| Child's level of maturity/awareness |
|
| Child asks questions about health, disease or HIV | Child's inquisitive or persistent questions makes disclosure more likely (Hejoaka, 2009; Kouyoumdjiam et al., 2005; Marques et al., 2006; Schaurich, 2011; Vaz et al., 2010; Vaz et al., 2011; Vreeman et al., 2010). |
| Child's family situation |
|
| Education/school factors |
Child going to school given as a reason causing caregivers to think more about disclosing (Vaz et al., 2011). |
| Health-related factors |
|
| Feel worried about or unprepared for disclosure |
|
| Fear negative effects of disclosure |
|
| Belief in keeping HIV concealed/private |
|
| Other caregiver/family-related factors |
|
The characteristics and beliefs of the caregiver further shaped whether and how disclosure took place (Table 2). Caregivers were more likely to disclose if they had a higher level of education [44,46,59] or were more open about their own HIV infection [31,38,40,53]. Caregivers with financial problems [25] and caregivers who were not the father or who were parenting in a context where the father had died [25,36] were also more likely to have disclosed. The caregiver's beliefs about children's ability to understand or about the impact of disclosure further influenced disclosure [32,37,41,43,44,53,56,58]. Variations in disclosure patterns by children's gender were not reported in studies identified in this review.
Studies described both barriers preventing the disclosure of HIV status to children in resource-limited settings and potential advantages to disclosure (Table 3). Numerous fears on the part of caregivers and healthcare providers were cited as barriers to disclosure. These included fear the child would disclose to others [25,32,35–38,42,44,45,49,51–55,59], fear of subsequent stigma or negative effects from others knowing the diagnosis [25,32,35,37,44,47,49,51,52,54–56,59], concerns for worsening the child's emotional or physical health [25,32,36,38,41–45,47,51,53–56,59], believing the child is unready or too young [25,35–37,39,43–45,47,51–55,59], feeling unprepared for questions or the disclosure process [43,53–56] and fear of the children's resentment [25,45,53,54,56,59]. In a survey of Nigerian caregivers’ reasons for non-disclosure, caregivers reported fears of the child subsequently telling other children (41%) or family and friends (33.7%), concerns the child was too young to understand (63%), fears the parents would be blamed (26.5%) and fears of psychological disturbance for the child (31%) [45]. Caregivers more often expressed fears of stigma and the child telling others, whereas healthcare providers focused more on children's emotional or physical health and age.
Table 3.
Barriers and advantages of disclosure
| Barriers to disclosure | Fear child will tell others | Subsequent stigma | Concern for child's emotional or physical health | Believing child unready or too young | Unpreparedness for questions or disclosure process |
|---|---|---|---|---|---|
| Studies | Abadia-Barrero and Larusso, 2006* | Bhattacharya et al., 2010 | Abadia-Barrero and Larusso, 2006* | Abadia-Barrero and Larusso, 2006* | Abadia-Barrero and Larusso, 2006* |
| Bhattacharya et al., 2010 | Biadgilign et al., 2011 | Bhattacharya et al., 2010 | Bhattacharya et al., 2010 | Boon-Yashidi et al., 2005* | |
| Biadgilign et al., 2011 | Boon-Yashidi et al., 2005* | Biadgilign et al., 2011 | Biadgilign et al., 2011 | Demmer, 2011* | |
| Boon-Yashidi et al., 2005* | Corneli et al., 2009; Vaz et al. *2008 | Boon-Yashidi et al., 2005* | Boon-Yashidi et al., 2005* | Kouyoumdjiam et al., 2005* | |
| Brown et al., 2011 | Demmer, 2011* | Brown et al., 2011 | Brown et al., 2011 | Marques et al., 2006* | |
| Corneli et al., 2009; Vaz et al., 2008* | Fetzer et al., 2011* | Corneli et al., 2009; Vaz et al., *2008 | Demmer, 2011* | Punpanich et al., 2008* | |
| Fetzer et al., 2011* | Hejoaka, 2009* | Demmer, 2011* | Hejoaka, 2009* | Schaurich, 2011* | |
| Hejoaka, 2009* | Kouyoumdjiam et al., 2005* | Kallem et al., 2010 | Kallem et al., 2010 | Yeap et al., 2010* | |
| Kallem et al., 2010 | Marques et al., 2006* | Marques et al., 2006* | Kouyoumdjiam et al., 2005* | ||
| Kouyoumdjiam et al., 2005* | Oberdorfer et al., 2006 | Moodley et al., 2006* | Myer et al., 2006* | ||
| Moodley et al., 2006* | Punpanich et al., 2008* | Oberdorfer et al., 2006 | Oberdorfer et al., 2006 | ||
| Oberdorfer et al., 2006 | *Schaurich, 2011* | Schaurich, 2011* | Punpanich et al., 2008* | ||
| Punpanich et al., 2008* | Vreeman et al., 2010** | Vaz et al., 2010* | Schaurich, 2011* | ||
| Schaurich, 2011* | Vaz et al., 2011* | Vreeman et al., 2010* | |||
| Vaz et al., 2011* | Vreeman et al., 2010* | Yeap et al., 2010* | |||
| Vreeman et al., 2010* | Yeap et al., 2010* | ||||
| Advantages of disclosure | Improving adherence | Improving child's care or treatment | Providing answers to child's questions | Fulfilling child's right to know | Child being able to protect themselves or others |
| Studies | Bhattacharya et al., 2010 | Bhattacharya et al., 2010 | Bhattacharya et al., 2010 | Bhattacharya et al., 2010 | Bhattacharya et al., 2010 |
| Biadgilign et al., 2009 | Biadgilign et al., 2009* | Boon-Yashidi et al., 2005* | Corneli et al., 2009; Vaz et al., *2008 | Boon-Yashidi et al., 2005* | |
| Bikaako-Kajura et * al., 2006 | Boon-Yashidi et al., 2005* | Brown et al., 2011 | Moodley et al., 2006* | Kallem et al., 2010 | |
| Brown et al., 2011 | Corneli et al., 2009; Vaz et al., *2008 | Hejoaka, 2009* | Marques et al., 2006* | ||
| Corneli et al., 2009; Vaz et al., *2008 | Ferris et al., 2007 | Kallem et al., 2010 | Vaz et al., 2010* | ||
| Fetzer et al., 2011* | Hejoaka, 2009* | Kouyoumdjiam et al., 2005* | Vaz et al., 2011* | ||
| Haberer et al., 2011 | Kallem et al., 2010 | Marques et al., 2006* | |||
| Kallem et al., 2010 | Marques et al., 2006* | Punpanich et al., 2008* | |||
| Marques et al., 2006* | Moodley et al., 2006* | Vaz et al., 2010* | |||
| Oberdorfer et al., 2006 | Oberdorfer et al., 2006 | ||||
| Punpanich et al., 2008* | Punpanich et al., 2008* | ||||
| Vaz et al., 2010* | Vaz et al., 2010* | ||||
| Vaz et al., 2011* | Vaz et al., 2011* | ||||
| Vreeman et al., 2010* | Vreeman et al., 2010* | ||||
Denotes qualitative study design.
The most common reasons cited as advantages to disclosure were potential improvements in medication adherence [25,30,32,34,36,41,42,45,49–52,56,59] and improving the child's care or treatment [17,25,32,34–36,38,41,42,51,52,54,56,59]. The child's increasing age [32,33,36,39,41,42,54,58,59], being able to answer the child's questions [35–37,41,45,52,54,56,59], fulfilling the child's right to know [32,38,59] and equipping the child to protect others or themselves [36,41,42,54,56,59] were also cited by caregivers as reasons to disclose to children.
Process of paediatric HIV disclosure in resource-limited settings
While some studies described disclosure as a one-time event, during which a child was told the reason they were taking medicines or was told the name of their diagnosis [25,41,44,53,58,59], other studies described children experiencing partial disclosure before being told they had HIV [30,42,46,55,56]. In several studies, caregivers reported lying to the children about the reason for taking their medicines until after full disclosure [25,42,51,58,59]. This contrasted with the emphasis from disclosed adolescents in Brazil on the importance of children's receiving accurate and complete information about HIV [56]. Vaz et al. included a more detailed description of the disclosure process for children in the Democratic Republic of Congo (DRC), where disclosure included giving minimal information about the illness itself, but featured discussion of the medications [33,41]. While caregivers typically conceptualized disclosure as a process, children described disclosure as a discrete event rather than a process, with limited conversations with caregivers and healthcare providers before, during or after disclosure [41]. Parents also described preparatory activities around the day of disclosure, including preparing the child's favourite foods, offering gifts and making sure the child felt loved [33]. In Thailand, caregivers reported that most disclosure events occurred when children were sick and alone with caregivers (89.2%) [25].
Studies endorsed involving both healthcare professionals and the child's parents or caregivers in disclosure. In a majority of studies, caregivers were thought to be the best people to carry out the disclosure process or were reported as the primary discloser [25,30,36–39,41,45,54,58,59]; however, some caregivers wanted healthcare providers to lead disclosure [36,44,57] or preferred that healthcare providers partnered with the child's caregiver [38,39]. In a study from Zimbabwe, 51.3% of caregivers wanted healthcare workers involved with disclosure and 42.3% wanted help from another family member such as a sister or parent [46]. Marques et al. reported several instances in which healthcare providers disclosed to children without prior consultation with caregivers who believed their child was not ready or that disclosure by providers was conducted inappropriately [56].
Opinions about the optimal age for disclosure varied. In one study from South Africa, healthcare providers believed six years was appropriate for a general discussion about health issues and ten years was appropriate for HIV-specific disclosure [39]. Caregivers from South Africa endorsed older ages for both events – 11 years for a general discussion and 12 years for HIV-specific information [38]. In Zimbabwe, community members preferred full disclosure at 14–15 years, with partial disclosure at 10–11 years, but healthcare providers preferred younger ages [46]. The caregivers’ preferences generally matched the age at which disclosure was actually done. In Thailand, one study found that being over 10 years was associated with knowing your HIV status [25], and in a small study from the DRC, the median age for disclosure was 15 years, with no children under ten years having been informed of their status; however, only 19 children were included in the study [33]. Two studies reported on caregivers’ and healthcare providers’ desire for protocols, materials or specific guidelines to direct disclosure [37,39].
Impact of disclosure on children and caregivers
Fourteen studies discussed the impact of disclosure on HIV-infected children; however, no studies evaluated children pre- and post-disclosure [17,25,30–32,35,40,41,43,45,49,50,56,57] (Table 4). The experience of disclosure on children in resource-limited settings was reported through qualitative or descriptive studies, in which disclosure was described as a positive event among the majority of those who went through it [32,56,57]. In Brazil, adolescents characterized disclosure as an essential step in adapting to a “normal” life with HIV and thought disclosure should be done as soon as possible [56]. Among Thai youth aged 13–16 years, 33.3% reported wishing they had been told sooner or much sooner, and 79.6% were satisfied with disclosure process; however, 18.5% wished they had not been told of the diagnosis at all [57].
Table 4.
Impact of disclosure
| Study | Impact of disclosure on children |
|---|---|
| Bikaako-Kajura et al., 2006* | Described improved adherence; disclosure believed to be motivating factor because child understood importance of medication; more positive attitude towards treatment; developed own adherence strategies and/or shared responsibility for treatment. |
| Brown et al., 2011 | Caregivers reported improved adherence in 66% of children. |
| Corneli et al., 2009; Vaz 2008* | Improved adherence; knowledge of diagnosis improved adherent behaviours; better able to protect themselves and others; some youths expressed emotional difficulties from disclosure, including sadness, discouragement and fear. |
| Ferris et al., 2007 | Significantly more frequent CD4 counts; significantly less likely to experience disease progression and death. |
| Fetzer et al., 2011* | Less frustration with medication-taking; disclosure as a motivating factor for adherent behaviours. |
| Haberer et al., 2011 | Significantly fewer missed ART days (compared to undisclosed children). |
| Hejoaka, 2009* | Improved adherence; children maintained concealment strategies and secrecy. |
| Lee and Oberdorfer, 2009* | Majority viewed disclosure as a positive event. |
| Marques et al., 2006* | Majority viewed disclosure as a positive event; adolescents felt disclosure had positive long-term psychological impacts and allowed for better self-care and treatment. |
| Menon et al., 2007 | Significantly fewer emotional difficulties (compared to undisclosed children). |
| Oberdorfer et al., 2006 | Majority of children accepted diagnosis; some reported sadness, anger and rebellion. |
| Petersen et al., 2010* | Negative effects and emotional difficulties included: distress, fear, perceived stigma, internalized stigma, withdrawal from peers, and perceived shortened future. Accepting family social support helped to address these challenges. |
| Vaz et al., 2010* | Negative effects and emotional difficulties included: sadness, worry and perceived stigma; some children reported relief after disclosure and felt disclosure was important. |
Denotes qualitative study design.
The combined evidence from this review suggests that disclosure may play an important role in improving medication adherence and HIV-related outcomes. Four qualitative studies reported adherence improved post-disclosure [30,32,35,49]. In Burkina Faso, youth reported that disclosure enabled them to maintain their HIV treatment, including their ability to conceal the diagnosis from others [35]. As one youth in the DRC described regarding improved adherence: “Having heard explanations made it easy for me to take the medicines. I was told what medicines do in my body. That is why I take them” [49]. Two studies attempted to quantify changes in adherence post-disclosure [45,50]. In a study from Nigeria, among caregivers who had disclosed to children, 64% felt that adherence had improved post-disclosure [45]. A study of paediatric ART adherence in Zambia found that the average number of missed ART days was 38% lower among children who knew their status (p=0.001) [50]. Though knowledge of HIV status was strongly associated with age, it remained an independent predictor for adherence when adjusted for age [50]. A study of 325 HIV-infected children in Romania found that disclosed children were less likely to experience disease progression (p=0.03), as measured by CD4 count or death [17].
Evidence on the emotional and psychological impact of disclosure was more limited. In the only study identified that quantified the psychological differences between disclosed and non-disclosed children, univariate analysis of 127 children in Zambia found non-disclosed children were more than twice as likely to experience concerning levels of emotional difficulty (OR=2.62, 95% CI: 1.11–6.26) [31]. In qualitative studies, many youth reported initial emotional difficulties, some of which were mitigated over time. In a qualitative study of 25 South African adolescents, almost all found disclosure to be emotionally difficult [40]. In Brazil and the DRC, children reported feeling sadness, grief, and worry upon learning about their HIV infection, but these negative feelings were followed by some feelings of relief [33,41,56]. Congolese children reported feeling calmer after disclosure because knowing their HIV status removed some of the uncertainty surrounding their illness [32]. Despite the negative emotions of sadness and worry, a number of studies reported that children felt that knowing HIV status was important and necessary [33,41,56].
Completing child disclosure also impacted caregivers differently. Some caregivers reported feeling relieved and happy with their decision to disclose [32,56]. Caregivers appreciated sharing the responsibilities of adherence with the child after disclosure [30], and described having less frustration with adherence [49]. Other caregivers reported negative emotional effects after disclosing, such as feeling unprepared for answering children's continuing questions and fear that social stigmatization might result if the child told others [41,56]. No studies measured actual experiences of stigma, discrimination, or social rejection post-disclosure for caregivers or their children. The systematic review found no studies that reported on the impact of disclosure on adolescent sexual behaviours or risk reduction for secondary transmission.
Discussion
In resource-limited settings, the prevalence of HIV disclosure to children is generally low, even among adolescents. Significant factors influencing disclosure include the child's age, the child's persistent questioning and caregivers’ perceptions of the child's ability to understand and cope up with HIV. Caregivers identify many barriers to disclosure within these settings, the most prominent being fear of stigma and of negative consequences for children's emotional and social well-being. In the midst of caregivers’ worries about disclosure and low prevalence of disclosure, there is only limited evidence to suggest how disclosure will impact children. Some studies assessing children who know their HIV status describe possible improvements in children's medication adherence and emotional health, but other studies describe negative effects. Because the impact of disclosure on children has rarely been assessed quantitatively, research to evaluate how disclosure impacts children's physical, emotional, mental, and social outcomes would improve implementation of age- and culture-appropriate disclosure.
Much of the work assessing disclosure to HIV-infected children in resource-limited settings is qualitative in nature and provides a useful body of literature describing important cultural concepts shaping when, how, and whether children are informed of their HIV status. Reasons given by caregivers for and against disclosure are similar across resource-limited and resource-rich settings with potential benefits weighted against potential harms of disclosure. While the child's age, developmental maturity, and concerns about medication adherence can drive parents and caregivers towards telling the child about their HIV diagnosis, deep-seated fears of the child telling others about the diagnosis and of potential negative emotional consequences for the child also shape caregivers’ decisions about disclosure. As HIV care programmes attempt to engage in disclosure for their growing populations of children, caregivers’ fears of stigma and negative psychosocial effects need to be addressed with appropriate disclosure protocols and procedures.
Learning about their HIV status is clearly an emotional and pivotal point in a child's life. Children describe reacting with sadness and grief, as well as anxiety and worry about what their diagnosis means for the future. In addition, children share their caregivers’ worries about the negative social repercussions that may result if their HIV status is revealed to others. No studies investigated whether fears of stigma translated into actual discrimination post-disclosure. In qualitative studies, disclosure is often described as a positive event, and at least one quantitative study suggested that, despite the immediate burden of learning one's HIV diagnosis, disclosed children actually have better emotional health outcomes compared to their non-disclosed counterparts. Limited evidence also suggests disclosure is associated with better adherence to ART and HIV-related health outcomes, although the effect of disclosure on adherence could not be evaluated.
The compiled evidence of this review suggests that there may be both positive and negative effects from disclosure. Additional qualitative and quantitative studies are needed to investigate how disclosure impacts children, particularly their adherence to ART, and physical, emotional, and social outcomes. Providing appropriate resources and support to caregivers and children through the disclosure process may mitigate any potential negative effects of disclosure. Furthermore, effective strategies to assess and monitor children's clinical and psychosocial well-being throughout the process will also help ensure that children and caregivers receive necessary services. While a number of web-based resources for disclosure exists [28,60,61], their impact has not been evaluated rigorously and merits attention. Investigating how the existing disclosure protocols and procedures may be cross-culturally adapted also deserves further consideration.
There are several limitations to this systematic review that warrant consideration. We may have failed to identify publications from non-traditional or non-Western literature sites, but we attempted to follow the most inclusive and systematic methodology readily available. Few non-English, French, Spanish or Portuguese studies were identified. Publication bias could be a concern; however, we were encouraged by the recent increase in studies from low- and middle-income countries, with all included studies having been published since 2004. In addition, we opted to include only published studies, as the quality of the existing studies was already fraught with limitations. While few studies measured the prevalence of disclosure or the quantitative impact of disclosure, the current understanding of disclosure in these settings is such that qualitative work is critically needed to understand cultural phenomena. The studies were heterogeneous, with inconsistent definitions or processes for disclosure, and few quantitative data about factors related to disclosure. Thus, we could not conduct a meta-analysis at this time for factors related to disclosure or a pooled estimate for the impact of disclosure. Key factors shaping the disclosure process may still be missing from these compiled data. For example, government policies and guidelines in different countries may have legal implications for disclosure. The studies that we summarized did not specifically include discussions of national laws and policies regulating disclosure in particular settings, which may influence the age for disclosure and who can be involved. Studies were also heterogeneous in the ages of study participants, with some studies including only children, others only adolescents, and many including both children and adolescents. Important differences in how disclosure takes place as well as its impact on clinical, emotional, and social outcomes for children and adolescents may be present; however, this review did not investigate this aspect of disclosure because of the limited body of data. Similarly, differences in disclosure patterns by gender could not be assessed in this review. Finally, we excluded studies reporting only on parents’ disclosure of their own HIV status to children or on youth disclosure of their own status to other people. Although these types of disclosure also merit careful consideration, the motivations and potential impacts may be different.
Conclusions
This systematic review revealed the paucity of data related to disclosure of HIV status to children in low- and middle-income countries. While specific evidence-based recommendations for how and when disclosure should take place are premature, the findings of this review and from the more robust literature available from the United States allow us to make preliminary recommendations for disclosure to children in resource-limited settings and directions for future research. First, disclosure needs to be addressed thoughtfully and proactively as part of long-term disease management. This includes consideration of cultural views about a child's age, maturity level and emotional health and addressing families’ widespread fears about potential HIV-related stigma and discrimination if their child's status is revealed to others. These concerns suggest that improved psychosocial support services in these settings could aid in the disclosure process. Second, there is a need for structured, evidence-based protocols, materials and guidelines for paediatric HIV disclosure that have been rigorously evaluated and incorporate both preparation and on-going communication among children, caregivers and health providers. Existing materials on disclosure should be made available for adaptation, evaluation and broader implementation. Finally, additional research is needed on effective strategies for disclosure and the clinical, emotional and social impact of disclosure on HIV-infected children in resource-limited settings. Longitudinal studies that follow children through the disclosure process will be better able to assess the impact of disclosure and allow clinicians and other providers to deliver appropriate services and support to children and caregivers.
Competing interests
The authors of this review have no competing interests to report.
Authors' contributions
RCV designed the systematic review, contributed significantly to the systematic search and review of articles and was the primary writer of the manuscript. AMG contributed significantly to the design and conduct of the systematic search and review of articles, extraction and analysis of data, and preparation of the manuscript. POG contributed to the systematic search and review of articles and the preparation and writing of the manuscript. MLS contributed to the review of articles, extraction and analysis of data, and contributed significantly to the preparation and writing of the manuscript. WMN contributed to the systematic review of articles and the preparation and writing of the manuscript. All authors have read and approved the final manuscript.
Funding
This research was supported in part by a grant (K23MH087225 and 5R01MH099747-01) to Dr. Vreeman from the NIMH and by the USAID-AMPATH Partnership from the United States Agency for International Development as part of the President's Emergency Plan for AIDS Relief (PEPFAR).
Disclaimer
The views expressed in this article are those of the authors and do not necessarily represent the view of the Indiana University School of Medicine or the Moi University School of Medicine. The authors have no conflicts of interest to disclose. The primary author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.World Health Organization. Geneva: World Health Organization; 2011. Global HIV/AIDS response: epidemic update and health sector progress towards universal access—progress report 2011. [Google Scholar]
- 2.UNAIDS. The Joint United Nations Programme on HIV/AIDS (UNAIDS). Geneva. 2010. 2010 report on the global AIDS epidemic. [Google Scholar]
- 3.World Health Organization. Geneva, Switzerland: World Health Organization; 2010. Antiretroviral therapy for HIV infection in infants and children: towards universal access. [PubMed] [Google Scholar]
- 4.American Academy of Pediatrics Committee on Pediatric AIDS. Disclosure of illness status to children and adolescents with HIV infection. American Academy of Pediatrics Committee on Pediatrics AIDS. Pediatrics. 1999;103(1):164–6. doi: 10.1542/peds.103.1.164. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Switzerland: World Health Organization; 2006. Progress on global access to HIV antiretroviral therapy: a report on “3 by 5” and beyond. [Google Scholar]
- 6.Wiener L, Mellins CA, Marhefka S, Battles HB. Disclosure of an HIV diagnosis to children: history, current research, and future directions. J Dev Behav Pediatr. 2007;28(2):155–66. doi: 10.1097/01.DBP.0000267570.87564.cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Armistead L, Forehand R. For whom the bell tolls: parenting decisions and challenges faced by mothers who are HIV seropositive. Clin Psychol: Sci Pract. 1995;2(3):239–50. [Google Scholar]
- 8.Rwemisisi J, Wolff B, Coutinho A, Grosskurth H, Whitworth J. What if they ask how I got it?’ Dilemmas of disclosing parental HIV status and testing children for HIV in Uganda. Health Policy Plan. 2008;23(1):36–42. doi: 10.1093/heapol/czm040. [DOI] [PubMed] [Google Scholar]
- 9.Hogwood J, Campbell T, Butler S. I wish I could tell you but I can't: adolescents with perinatally acquired HIV and their dilemmas around self-disclosure. Clin Child Psychol Psychiatry. 2012;18(1):44–60. doi: 10.1177/1359104511433195. [DOI] [PubMed] [Google Scholar]
- 10.Sherman BF, Bonanno GA, Wiener LS, Battles HB. When children tell their friends they have AIDS: possible consequences for psychological well-being and disease progression. Psychosom Med. 2000;62(2):238–47. doi: 10.1097/00006842-200003000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Gerson AC, Joyner M, Fosarelli P, Butz A, Wissow L, Lee S, et al. Disclosure of HIV diagnosis to children: when, where, why, and how. J Pediatr Health Care. 2001;15(4):161–7. doi: 10.1067/mph.2001.114835. [DOI] [PubMed] [Google Scholar]
- 12.Lesch A, Swartz L, Kagee A, Moodley K, Kafaar Z, Myer L, et al. Paediatric HIV/AIDS disclosure: towards a developmental and process-oriented approach. AIDS Care. 2007;19(6):811–6. doi: 10.1080/09540120601129301. [DOI] [PubMed] [Google Scholar]
- 13.Bachanas PJ, Kullgren KA, Schwartz KS, Lanier B, McDaniel JS, Smith J, et al. Predictors of psychological adjustment in school-age children infected with HIV. J Pediatr Psychol. 2001;26(6):343–52. doi: 10.1093/jpepsy/26.6.343. [DOI] [PubMed] [Google Scholar]
- 14.Riekert KA, Wiener L, Battles HB. Prediction of psychological distress in school-age children with HIV. Child Health Care. 1999;28:201–20. [Google Scholar]
- 15.Blasini I, Chantry C, Cruz C, Ortiz L, Salabarria I, Scalley N, et al. Disclosure model for pediatric patients living with HIV in Puerto Rico: design, implementation, and evaluation. J Dev Behav Pediatr. 2004;25(3):181–9. doi: 10.1097/00004703-200406000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Hammami N, Nostlinger C, Hoeree T, Lefevre P, Jonckheer T, Kolsteren P. Integrating adherence to highly active antiretroviral therapy into children's daily lives: a qualitative study. Pediatr. 2004;114(5):e591–7. doi: 10.1542/peds.2004-0085. [DOI] [PubMed] [Google Scholar]
- 17.Ferris M, Burau K, Schweitzer AM, Mihale S, Murray N, Preda A, et al. The influence of disclosure of HIV diagnosis on time to disease progression in a cohort of Romanian children and teens. AIDS Care. 2007;19(9):1088–94. doi: 10.1080/09540120701367124. [DOI] [PubMed] [Google Scholar]
- 18.Mellins CA, Brackis-Cott E, Dolezal C, Rchards A, Nicholas SW, Abrams EJ. Patterns of HIV status disclosure to perinatally HIV-infected children and subsequent mental health outcomes. Clin Child Psychol Psychiatry. 2002;7(1):101–14. [Google Scholar]
- 19.Lester P, Chesney M, Cooke M, Weiss R, Whalley P, Perez B, et al. When the time comes to talk about HIV: factors associated with diagnostic disclosure and emotional distress in HIV-infected children. J Acquir Immune Defic Syndr. 2002;31(3):309–17. doi: 10.1097/00126334-200211010-00006. [DOI] [PubMed] [Google Scholar]
- 20.Marhefka SL, Tepper VJ, Brown JL, Farley JJ. Caregiver psychosocial characteristics and children's adherence to antiretroviral therapy. AIDS Patient Care STDS. 2006;20(6):429–37. doi: 10.1089/apc.2006.20.429. [DOI] [PubMed] [Google Scholar]
- 21.Mellins CA, Brackis-Cott E, Dolezal C, Abrams EJ. The role of psychosocial and family factors in adherence to antiretroviral treatment in human immunodeficiency virus-infected children. Pediatr Infect Dis J. 2004;23(11):1035–41. doi: 10.1097/01.inf.0000143646.15240.ac. [DOI] [PubMed] [Google Scholar]
- 22.Sopena S, Evangeli M, Dodge J, Melvin D. Coping and psychological adjustment in adolescents with vertically acquired HIV. AIDS Care. 2010;22(10):1252–8. doi: 10.1080/09540121003668110. [DOI] [PubMed] [Google Scholar]
- 23.Michaud PA, Suris JC, Thomas LR, Kahlert C, Rudin C, Cheseaux JJ. To say or not to say: a qualitative study on the disclosure of their condition by human immunodeficiency virus-positive adolescents. J Adolesc Health. 2009;44(4):356–62. doi: 10.1016/j.jadohealth.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 24.Relf MV, Bishop TL, Lachat MF, Schiavone DB, Pawlowski L, Bialko MF, et al. A qualitative analysis of partner selection, HIV serostatus disclosure, and sexual behaviors among HIV-positive urban men. AIDS Educ Prev. 2009;21(3):280–97. doi: 10.1521/aeap.2009.21.3.280. [DOI] [PubMed] [Google Scholar]
- 25.Oberdorfer P, Puthanakit T, Louthrenoo O, Charnsil C, Sirisanthana V, Sirisanthana T. Disclosure of HIV/AIDS diagnosis to HIV-infected children in Thailand. J Paediatr Child Health. 2006;42(5):283–8. doi: 10.1111/j.1440-1754.2006.00855.x. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Geneva: World Health Organization; 2011. Guideline on HIV disclosure counselling for children up to 12 years of age. [PubMed] [Google Scholar]
- 27.Chazal E. Paris: Medecins Sans Frontieres; 2005. Therapeutic education: recommendations regarding disclosure of HIV status to children under ARV in MSF projects. [Google Scholar]
- 28.South to South. Bellville, South Africa: South to South, Faculty of Health Sciences, Stellenbosch University, USAID; 2010. Disclosure process for children and adolescents living with HIV: practical guide. [Google Scholar]
- 29.Bank W. Country and lending groups. 2011. [cited 2011 Oct 10]. Available from: http://data.worldbank.org/about/country-classifications/country-and-lending-groups#Low_income.
- 30.Bikaako-Kajura W, Luyirika E, Purcell DW, Downing J, Kaharuza F, Mermin J, et al. Disclosure of HIV status and adherence to daily drug regimens among HIV-infected children in Uganda. AIDS Behav. 2006;10(Suppl 4):S85–93. doi: 10.1007/s10461-006-9141-3. [DOI] [PubMed] [Google Scholar]
- 31.Menon A, Glazebrook C, Campain N, Ngoma M. Mental health and disclosure of HIV status in Zambian adolescents with HIV infection: implications for peer-support programs. J Acquir Immune Defic Syndr. 2007;26(3):349–54. doi: 10.1097/QAI.0b013e3181565df0. [DOI] [PubMed] [Google Scholar]
- 32.Corneli A, Vaz L, Dulyx J, Omba S, Rennie S, Behets F. The role of disclosure in relation to assent to participate in HIV-related research among HIV-infected youth: a formative study. J Int AIDS Soc. 2009;12(1):17. doi: 10.1186/1758-2652-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vaz L, Corneli A, Dulyx J, Rennie S, Omba S, Kitetele F, et al. The process of HIV status disclosure to HIV-positive youth in Kinshasa, Democratic Republic of the Congo. AIDS Care. 2008;20(7):842–52. doi: 10.1080/09540120701742276. [DOI] [PubMed] [Google Scholar]
- 34.Biadgilign S, Deribew A, Amberbir A, Deribe K. Barriers and facilitators to antiretroviral medication adherence among HIV-infected paediatric patients in Ethiopia: a qualitative study. Sahara J. 2009;6(4):148–54. doi: 10.1080/17290376.2009.9724943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hejoaka F. Care and secrecy: being a mother of children living with HIV in Burkina Faso. Soc Sci Med. 2009;69(6):869–76. doi: 10.1016/j.socscimed.2009.05.041. [DOI] [PubMed] [Google Scholar]
- 36.Kallem S, Renner L, Ghebremichael M, Paintsil E. Prevalence and pattern of disclosure of HIV status in HIV-infected children in Ghana. AIDS Behav. 2011;15(6):1121–7. doi: 10.1007/s10461-010-9741-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kouyoumdjian FG, Meyers T, Mtshizana S. Barriers to disclosure to children with HIV. J Trop Pediatr. 2005;51(5):285–7. doi: 10.1093/tropej/fmi014. [DOI] [PubMed] [Google Scholar]
- 38.Moodley K, Myer L. Paediatric HIV disclosure in South Africa – caregivers’ perspectives on discussing HIV with infected children. S Afr Med J. 2006;96(3):201–4. [PubMed] [Google Scholar]
- 39.Myer L, Moodley K, Hendricks F, Cotton M. Healthcare providers’ perspectives on discussing HIV status with infected children. J Trop Pediatr. 2006;52(4):293–5. doi: 10.1093/tropej/fml004. [DOI] [PubMed] [Google Scholar]
- 40.Petersen I, Bhana A, Myeza N, Alicea S, John S, Holst H, et al. Psychosocial challenges and protective influences for socio-emotional coping of HIV+ adolescents in South Africa: a qualitative investigation. AIDS Care. 2010;22(8):970–8. doi: 10.1080/09540121003623693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vaz L, Eng E, Maman S, Tshikandu T, Behets F. Telling children they have HIV: lessons learned from findings of a qualitative study in sub-Saharan Africa. AIDS Patient Care STDS. 2010;24(4):247–56. doi: 10.1089/apc.2009.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vaz LM, Maman S, Eng E, Barbarin OA, Tshikandu T, Behets F. J Dev Behav Pediatr. 2011. Patterns of disclosure of HIV status to infected children in a Sub-Saharan African setting. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yeap AD, Hamilton R, Charalambous S, Dwadwa T, Churchyard GJ, Geissler PW, et al. Factors influencing uptake of HIV care and treatment among children in South Africa—a qualitative study of caregivers and clinic staff. AIDS Care. 2010;22(9):1101–7. doi: 10.1080/09540121003602218. [DOI] [PubMed] [Google Scholar]
- 44.Biadgilign S, Deribew A, Amberbir A, Escudero HR, Deribe K. Factors associated with HIV/AIDS diagnostic disclosure to HIV infected children receiving HAART: a multi-center study in Addis Ababa, Ethiopia. PLoS One. 2011;6(3):e17572. doi: 10.1371/journal.pone.0017572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brown BJ, Oladokun RE, Osinusi K, Ochigbo S, Adewole IF, Kanki P. Disclosure of HIV status to infected children in a Nigerian HIV care programme. AIDS Care. 2011;23(9):1053–8. doi: 10.1080/09540121.2011.554523. [DOI] [PubMed] [Google Scholar]
- 46.De Baets AJ, Sifovo S, Parsons R, Pazvakavambwa IE. HIV disclosure and discussions about grief with Shona children: a comparison between health care workers and community members in Eastern Zimbabwe. Soc Sci Med. 2008;66(2):479–91. doi: 10.1016/j.socscimed.2007.08.028. [DOI] [PubMed] [Google Scholar]
- 47.Demmer C. Experiences of families caring for an HIV-infected child in KwaZulu-Natal, South Africa: an exploratory study. AIDS Care. 2011;23(7):873–9. doi: 10.1080/09540121.2010.542123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Feinstein L, Moultrie H, Myers T, Rie A. Effect of disclosure on HIV status to children receiving ART on six-month virologic suppression. Am J Epidemiol. 2010;171(Suppl):538–S. [Google Scholar]
- 49.Fetzer BC, Mupenda B, Lusiama J, Kitetele F, Golin C, Behets F. Barriers to and facilitators of adherence to pediatric antiretroviral therapy in a sub-Saharan setting: insights from a qualitative study. AIDS Patient Care STDS. 2011;25(10):611–21. doi: 10.1089/apc.2011.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haberer JE, Cook A, Walker AS, Ngambi M, Ferrier A, Mulenga V, et al. Excellent adherence to antiretrovirals in HIV+ Zambian children is compromised by disrupted routine, HIV nondisclosure, and paradoxical income effects. PLoS One. 2011;6(4):e18505. doi: 10.1371/journal.pone.0018505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vreeman RC, Nyandiko WM, Ayaya SO, Walumbe EG, Marrero DG, Inui TS. The perceived impact of disclosure of pediatric HIV status on pediatric antiretroviral therapy adherence, child well-being, and social relationships in a resource-limited setting. AIDS Patient Care STDS. 2010;24(10):639–49. doi: 10.1089/apc.2010.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Punpanich W, Detels R, Gorbach PM, Leowsrisook P. Understanding the psychosocial needs of HIV-infected children and families: a qualitative study. J Med Assoc Thai. 2008;91(Suppl 3):S76–84. [PMC free article] [PubMed] [Google Scholar]
- 53.Abadia-Barrero CE, Larusso MD. The disclosure model versus a developmental illness experience model for children and adolescents living with HIV/AIDS in Sao Paulo, Brazil. AIDS Patient Care STDS. 2006;20(1):36–43. doi: 10.1089/apc.2006.20.36. [DOI] [PubMed] [Google Scholar]
- 54.Boon-Yasidhi V, Kottapat U, Durier Y, Plipat N, Phongsamart W, Chokephaibulkit K, et al. Diagnosis disclosure in HIV-infected Thai children. J Med Assoc Thai. 2005;88(Suppl 8):S100–5. [PubMed] [Google Scholar]
- 55.Schaurich D. Disclosure of aids diagnosis to children from the family members’ perspective. Rev Esc Enferm USP. 2011;45(2):480–6. doi: 10.1590/s0080-62342011000200025. [DOI] [PubMed] [Google Scholar]
- 56.Marques HH, Silva NG, Gutierrez PL, Lacerda R, Ayres JR, Dellanegra M, et al. Disclosure of HIV infection from the perspective of adolescents living with HIV/AIDS and their parents and caregivers. Cad Saude Publica. 2006;22(3):619–29. doi: 10.1590/s0102-311x2006000300017. [DOI] [PubMed] [Google Scholar]
- 57.Lee B, Oberdorfer P. Risk-taking behaviors among vertically HIV-infected adolescents in Northern Thailand. J Int Assoc Physicians AIDS Care. 2009;8(4):221–8. doi: 10.1177/1545109709341082. [DOI] [PubMed] [Google Scholar]
- 58.Arun S, Singh AK, Lodha R, Kabra SK. Disclosure of the HIV infection status in children. Indian J Pediatr. 2009;76(8):805–8. doi: 10.1007/s12098-009-0177-z. [DOI] [PubMed] [Google Scholar]
- 59.Bhattacharya M, Dubey AP, Sharma M. Patterns of diagnosis disclosure and its correlates in HIV-infected North Indian children. J Trop Pediatr. 2010;57(6):405–11. doi: 10.1093/tropej/fmq115. [DOI] [PubMed] [Google Scholar]
- 60.World Health Organization. Gevena: World Health Organization; 2011. Guideline on HIV disclosure counselling for children up to 12 years of age. [PubMed] [Google Scholar]
- 61.Close K. Houston, TX: Baylor International Pediatric AIDS Initiative; 2010. Psychosocial aspects of HIV/AIDS: children and adolescents HIV curriculum; pp. 319–33. [Google Scholar]