Abstract
Background
Survival statistics commonly reflect survival from the time of diagnosis but do not take into account survival already achieved after a diagnosis. The objective of this study was to provide conditional survival estimates for brain tumor patients as a more accurate measure of survival for those who have already survived for a specified amount of time after diagnosis.
Methods
Data on primary malignant and nonmalignant brain tumor cases diagnosed from 1985–2005 from selected SEER state cancer registries were obtained. Relative survival up to 15 years postdiagnosis and varying relative conditional survival rates were computed using the life-table method.
Results
The overall 1-year relative survival estimate derived from time of diagnosis was 67.8% compared to the 6-month relative conditional survival rate of 85.7% for 6-month survivors (the probability of surviving to 1 year given survival to 6 months). The 10-year overall relative survival rate was 49.5% from time of diagnosis compared to the 8-year relative conditional survival rate of 79.2% for 2-year survivors. Conditional survival estimates and standard survival estimates varied by histology, behavior, and age at diagnosis. The 5-year relative survival estimate derived from time of diagnosis for glioblastoma was 3.6% compared to the 3-year relative conditional survival rate of 36.4% for 2-year survivors. For most nonmalignant tumors, the difference between relative survival and the corresponding conditional survival estimates were minimal. Older age groups had greater numeric gains in survival but lower conditional survival estimates than other age groups. Similar findings were seen for other conditional survival intervals.
Conclusions
Conditional survival is a useful disease surveillance measure for clinicians and brain tumor survivors to provide them with better ‘real-time’ estimates and hope.
Key Words: Brain tumor, primary; Brain tumor, malignant; Brain tumor, nonmalignant; Survival; Conditional probability
Introduction
The most commonly reported cancer survival statistics reflect survival from the time of diagnosis but are not as informative for patients who have survived for some time postdiagnosis. The clinical usefulness of these relative survival rates to estimate future prognosis is diminished for patients who have lived some time after a cancer diagnosis because the probability of survival changes as patients continue to survive. As a result, prognosis for survivors differs from that of newly diagnosed patients. Conditional survival provides modified survival estimates that are a more accurate measure for those patients who have already survived for a specified amount of time after diagnosis [1].
Little has been published regarding conditional survival rates for primary brain tumor patients. Estimates for malignant brain tumors were first reported by Davis et al. [2] in a US study for a patient cohort diagnosed from 1979–1993. Subsequent studies from Taiwan reported estimates for a subgroup of malignant tumors [3, 4]. To date, there are no published estimates for nonmalignant tumors. Given that state cancer registries in the US are now required to collect nonmalignant brain tumor data [5], reporting of these estimates is warranted. The objective of this study was to obtain conditional survival estimates, overall and by histology and age, for primary malignant and nonmalignant brain tumor survivors.
Materials and Methods
Survival data for this study included information on primary malignant and nonmalignant brain tumor cases diagnosed from 1985–2005 with follow-up through December 2006. Tumors were selected for inclusion using the following International Classification of Diseases for Oncology (ICD-O-3) primary site codes: brain and other central nervous system (CNS; C70.0–C72.9), pituitary and pineal glands (C75.1–C75.3) and olfactory tumors of the nasal cavity (C30: 9522–9523) [5]. Data for malignant cases were obtained from five Surveillance, Epidemiology, and End Results (SEER) program state cancer registries (CT, HI, IA, NM, UT) included in the SEER research dataset [6]. Data for nonmalignant cases were obtained from two Central Brain Tumor Registry of the United States (CBTRUS) collaborating SEER state cancer registries, (CT, UT). Both data sources are nationally recognized; SEER as the gold standard for population-based cancer statistics for all cancer sites [7], and CBTRUS as the leader for reporting population-based incidence data on all primary brain tumors since 1991 [5]. The exclusion criteria varied due to differences in data structure between malignant and nonmalignant cases. For analyses of malignant and nonmalignant data, cases were excluded if patients were alive but follow-up time could not be calculated. For analyses of malignant cases only, patients diagnosed at autopsy or death certificate only, and second or later primary tumors, were excluded. While second or later primary brain tumors were excluded from nonmalignant cases, the dataset may contain brain tumors that were second or later primaries after a primary from another cancer site. All tumors of the brain and CNS were included, whether or not they were microscopically confirmed.
All data were compiled using SAS software, version 9.2 [8] and all survival estimates were generated using the life-table method in SEER*Stat 6.6.2 software [9]. Patients who were still alive at the end of the cutoff date of December 2006 were right censored at the date of last contact. Relative survival rates were presented for all estimates, defined as observed survival divided by expected survival, with adjustment for age, gender, race, and calendar year. Survival rates were estimated in 1-year intervals up to a period of 15 years after diagnosis. Cumulative survival estimates were used to derive conditional survival estimates. Conditional survival, CS(y | x) is the probability of surviving an additional y years, given that the patient has already survived x years after diagnosis [1], and can be expressed as:
S(t) represents the traditional life-table survival at time t. To compute 3-year conditional survival (probability of surviving an additional 3 years) for a patient that has already survived 2 years, the survival at 2 + 3 years, S(5), was divided by the survival at 2 years, S(2). Conditional survival rates were calculated similarly for other time intervals. Conditional survival estimates were calculated and reported for all primary brain tumors and for selected histologies as defined by CBTRUS [5], pediatric (all tumors diagnosed before the age of 20); and adult (tumors diagnosed between the ages of 20–44, 45–64, or 65+). For the purposes of this study, pilocytic astrocytoma was considered a tumor of nonmalignant behavior. Survival estimates were not computed for groups with less than 16 cases. The 95% confidence intervals (95% CI) were calculated around the relative survival rate and the conditional survival rates [9].
Results
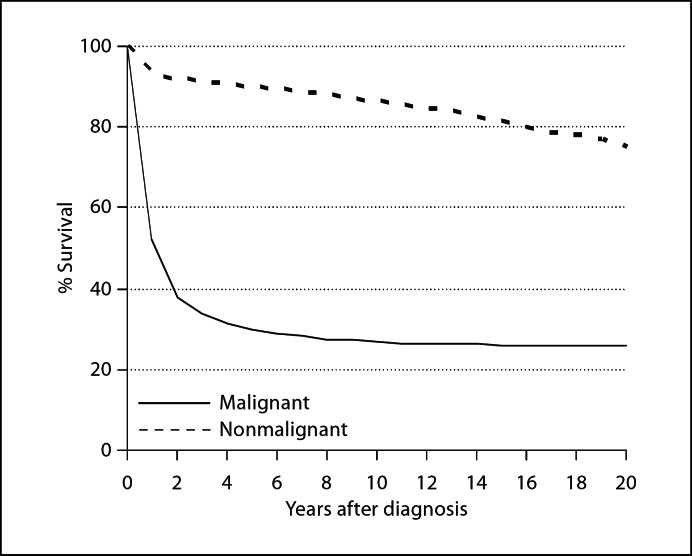
Distinctive patterns in relative survival rates (0 years to 15-year survival) for the 22,974 malignant and nonmalignant tumors were apparent (fig. 1). Relative survival rates for malignant tumors declined rapidly in the first 2 years after diagnosis, then plateaued at less than 30 percent. However, relative survival rates for nonmalignant tumors declined slightly in the 1st year after diagnosis, then continued to slowly decline, but remained over 80% at 15 years.
Fig. 1.
Relative survival estimates of patients with primary brain tumors at time of diagnosis.
The overall 1-, 2-, 5-, 10-, and 15-year relative survival rates were 67.8, 58.6, 52.6, 49.5, and 47.2%, respectively (table 1). One-year relative survival rates were similar for glioblastoma (30.3%) and neoplasm, unspecified (35.5%) but dramatically differed as years since diagnosis progressed. Relative survival rates for nerve sheath tumors and other cranial/spinal nerves remained constant for all survival years (range: 97.4–98.4%). Long-term relative survival rates for all histologies remained above 25% at 10 and 15 years except anaplastic astrocytoma (10 years: 21.8%; 15 years: 19.8%), glioblastoma (10 years: 2.9%; 15 years: 2.8%), and lymphoma (10 years: 15.7%; 15 years: 13.0%). For many histologies, 10-year relative survival rates did not differ much from 15-year relative survival rates.
Table 1.
1-, 1.5-, 2-, 3-, 5-, 10-, and 15-year relative survival rates with 95% confidence intervals for all primary brain tumors: 1985–2005
| Category | Cases n | Relative survival, % |
||||||
|---|---|---|---|---|---|---|---|---|
| 1 year | 1.5 years | 2 years | 3 years | 5 years | 10 years | 15 years | ||
| All brain tumors | 22,974 | 67.8 (67.2–68.4) | 61.6 (61.0–62.3) | 58.6 (57.9–59.2) | 55.7 (55.0–56.4) | 52.6 (51.9–53.4) | 49.5 (48.6–50.4) | 47.2 (46.1–48.4) |
| Tumor behavior | ||||||||
| Malignant | 14,119 | 52.3 (51.4–53.1) | 42.5 (41.7–43.3) | 37.8 (37.0–38.6) | 33.7 (32.8–34.5) | 29.8 (28.9–30.6) | 26.9 (25.9–27.8) | 26.1 (25.0–27.2) |
| Nonmalignant | 8,855 | 92.8 (92.2–93.4) | 92.5 (91.8–93.1) | 92.1 (91.4–92.8) | 91.6 (90.8–92.3) | 90.0 (89.0–90.9) | 86.5 (85.0–87.9) | 81.5 (79.2–83.6) |
| Specified histologic subtypes | ||||||||
| Primarily malignant | ||||||||
| Diffuse astrocytoma | 342 | 68.2 (62.8–72.9) | 57.9 (52.3–63.1) | 53.6 (47.9–58.8) | 46.8 (41.2–52.2) | 39.1 (33.5–44.7) | 30.7 (24.9–36.6) | 27.6 (21.4–34.1) |
| Anaplastic astrocytoma | 859 | 61.2 (57.8–64.4) | 51.9 (48.5–55.3) | 44.4 (40.9–47.8) | 37.1 (33.7–40.5) | 27.9 (24.7–31.2) | 21.8 (18.6–25.2) | 19.8 (16.4–23.5) |
| Glioblastoma | 5,991 | 30.3 (29.1–31.5) | 15.9 (15.0–16.9) | 9.5 (8.7–10.3) | 5.4 (4.8–6.0) | 3.6 (3.1–4.2) | 2.9 (2.4–3.5) | 2.8 (2.2–3.5) |
| Oligodendroglioma | 785 | 93.4 (91.3–95.0) | 90.3 (87.9–92.3) | 89.1 (86.6–91.2) | 84.6 (81.6–87.1) | 78.2 (74.7–81.3) | 61.9 (57.2–66.3) | 51.0 (45.0–56.6) |
| Anaplastic oligodendroglioma | 205 | 77.8 (71.4–83.0) | 70.7 (63.8–76.6) | 62.5 (55.2–69.0) | 57.4 (49.9–64.2) | 45.1 (37.2–52.6) | 35.4 (26.1–44.8) | 35.4 (26.1–44.8) |
| Mixed glioma | 293 | 84.7 (80.0–88.5) | 78.3 (73.0–82.7) | 71.6 (65.8–76.5) | 64.7 (58.6–70.1) | 55.3 (48.8–61.4) | 44.3 (37.1–51.3) | 38.9 (31.0–46.8) |
| Astrocytoma (NOS) | 1,722 | 64.5 (62.1–66.8) | 57.0 (54.6–59.4) | 53.5 (51.0–55.9) | 49.3 (46.8–51.7) | 42.9 (40.4–45.4) | 38.3 (35.6–41.0) | 36.9 (33.9–39.9) |
| Glioma, malignant (NOS) | 829 | 53.9 (50.4–57.3) | 46.1 (42.5–49.6) | 42.9 (39.4–46.4) | 40.2 (36.7–43.8) | 37.3 (33.6–41.0) | 36.5 (32.7–40.2) | 35.1 (30.2–40.0) |
| Embryonal/primitive medulloblastoma | 542 | 81.7 (78.1–84.7) | 75.3 (71.4–78.8) | 73.0 (69.1–76.6) | 68.1 (63.9–71.9) | 61.9 (57.5–66.0) | 54.0 (49.2–58.6) | 49.8 (44.4–55.0) |
| Lymphoma | 886 | 45.9 (42.5–49.2) | 38.5 (35.2–41.8) | 34.5 (31.3–37.8) | 28.6 (25.4–31.8) | 21.3 (18.3–24.5) | 15.7 (12.5–19.2) | 13.0 (9.3–17.4) |
| Meningioma, malignant | 228 | 86.0 (80.1–90.3) | 82.3 (75.8–87.2) | 80.2 (73.3–85.5) | 74.6 (67.2–80.6) | 67.3 (58.6–74.6) | 53.5 (42.5–63.3) | 36.9 (23.2–50.8) |
| Neoplasm, unspecified | 666 | 35.5 (31.7–39.3) | 32.2 (28.5–36.0) | 30.4 (26.6–34.2) | 27.9 (24.2–31.8) | 27.7 (23.8–31.7) | 27.7 (23.8–31.7) | 27.7 (23.8–31.7) |
| Ependymoma | 532 | 92.8 (92.2–93.4) | 90.4 (87.4–92.7) | 88.7 (85.4–91.2) | 84.3 (80.6–87.4) | 81.5 (77.4–84.9) | 75.4 (70.4–79.7) | 69.9 (62.8–75.9) |
| Germ cell tumor | 172 | 91.4 (86.0–94.7) | 88.5 (82.6–92.5) | 86.1 (79.9–90.6) | 85.6 (79.3–90.1) | 82.9 (76.1–88.0) | 79.5 (71.6–85.5) | 73.1 (61.7–81.6) |
| Primarily nonmalignant | ||||||||
| Pilocytic astrocytoma | 663 | 96.5 (94.8–97.7) | 96.3 (94.5–97.5) | 95.8 (93.9–97.2) | 95.1 (93.1–96.6) | 92.7 (90.2–94.6) | 92.0 (89.3–94.0) | 89.8 (85.3–93.0) |
| Hemangioblastoma/hemangioma | 224 | 94.0 (89.6–96.5) | 93.6 (89.0–96.3) | 93.6 (89.0–96.3) | 93.1 (87.9–96.1) | 90.4 (84.0–94.3) | 88.3 (79.4–93.5) | 80.4 (67.2–88.7) |
| Craniopharyngioma | 135 | 93.0 (86.8–96.4) | 90.4 (83.4–94.5) | 89.2 (81.8–93.7) | 88.9 (81.2–93.6) | 84.8 (75.7–90.6) | 73.8 (62.7–82.0) | 70.1 (55.7–80.6) |
| Meningioma, nonmalignant | 4,535 | 91.9 (90.9–92.7) | 91.4 (90.4–92.4) | 91.0 (89.9–92.0) | 90.4 (89.1–91.5) | 88.7 (87.1–90.1) | 82.8 (80.2–85.0) | 77.3 (73.4–80.7) |
| Nerve sheath and other cranial/spinal nerve tumor | 1,125 | 98.4 (97.1–99.1) | 98.0 (96.6–98.9) | 97.7 (96.1–98.7) | 97.5 (95.7–98.6) | 97.5 (95.7–98.6) | 97.4 (92.2–99.1) | 97.4 (92.2–99.1) |
| Pituitary tumor | 1,609 | 97.2 (96.0–98.0) | 97.2 (96.0–98.0) | 96.8 (95.4–97.8) | 96.3 (94.6–97.5) | 93.7 (91.4–95.3) | 90.2 (86.8–92.7) | 81.6 (76.7–85.5) |
| 73.8 (66.3–79.9) | 68.6 (58.6–76.7) | |||||||
| Neuronal/glial, nonmalignant and malignant | 254 | 91.6 (87.3–94.5) | 86.8 (81.7–90.5) | 85.2 (79.9–89.1) | 84.0 (78.6–88.2) | 78.2 (71.7–83.3) | ||
| All other brain tumors | 334 | 82.3 (77.6–86.1) | 78.3 (73.3–82.5) | 75.7 (70.5–80.2) | 72.3 (66.8–77.1) | 66.2 (60.2–71.6) | 61.6 (54.6–67.8) | 57.7 (49.1–65.3) |
NOS = Not otherwise specified.
Surviving for even a short period of time resulted in more favorable conditional survival rates than the corresponding relative survival rates (t able 2). The overall 6-month relative conditional survival estimates for 0.5-, 1-, and 1.5-year survivors were 85.7, 90.6, and 94.7%, respectively. Primarily malignant histologies followed this incremental upward trend except for oligodendroglioma, anaplastic oligodendroglioma, mixed glioma, ependymoma, and germ cell tumor, whose rates remained virtually unchanged. As expected, the overall probability of surviving to 2 years was greater if the patient had already survived 18 months [94.7% (95% CI: 93.5–95.7)] compared to having already survived12 months [85.8% (95% CI: 84.6–86.9)] but varied among histologies. Except for neuronal/glial tumors, relative conditional survival estimates for primarily nonmalignant tumors remained constant nearing 100% regardless of the length of time patients had survived.
Long-term relative conditional survival estimates given that the patient has already survived a specified number of years after diagnosis are depicted in table 3. The overall 8-year relative conditional survival rate for 2-year survivors (i.e. the probability of surviving to 10 years given survival to 2 years) was 79.2% (95% CI: 77.9–80.5), which was more favorable than the 10-year relative survival rate of 49.5% (95% CI: 48.6–50.4) derived from time at diagnosis. Overall, the probability of surviving to 10 years was greater for those who had already survived 5 years [90.1% (95% CI: 88.8–91.3)] compared to those who had already survived 2 years [79.2% (95% CI: 77.9–80.5)]. Identical trends were seen for most other tumor groups and for 15-year survival conditioned on having survived 5 and 10 years since diagnosis.
Table 3.
Long-term relative conditional survival (%) based on varying conditioning points with 95% confidence intervals for all primary brain tumors: 1985–2005
| 3-year CS upon 2 years | 8-year CS upon 2 years | 5-year CS upon 5 years | 10-year CS upon 5 years | 5-year CS upon 10 years | |
|---|---|---|---|---|---|
| Years since diagnosis | 5 years | 10 years | 10 years | 15 years | 15 years |
| All brain tumors | 87.8 (87.0–88.5) | 79.2 (77.9–80.5) | 90.1 (88.8–91.3) | 82.1 (80.1–84.0) | 90.8 (87.8–93.1) |
| Tumor behavior | |||||
| Malignant | 75.4 (74.0–76.7) | 62.8 (60.7–64.7) | 82.6 (79.2–85.5) | 72.7 (68.9–76.1) | 87.4 (81.7–91.5) |
| Nonmalignant | 96.9 (96.0–97.5) | 92.0 (90.3–93.4) | 94.9 (92.5–96.6) | 88.6 (85.3–91.2) | 92.9 (88.2–95.8) |
| Specified histologic subtypes | |||||
| Primarily malignant | |||||
| Diffuse astrocytoma | 71.5 (63.6–77.9) | 53.6 (42.9–63.2) | 73.7 (59.6–83.6) | 61.7 (45.0–74.7) | 83.6 (43.5–96.2) |
| Anaplastic astrocytoma | 61.0 (55.4–66.1) | 45.4 (38.2–52.3) | 73.6 (62.7–81.8) | 62.4 (49.5–72.9) | 84.3 (55.3–95.2) |
| Glioblastoma | 36.4 (31.8–41.0) | 26.2 (20.6–32.1) | 70.4 (55.6–81.2) | 59.7 (42.5–73.3) | 84.0 (38.9–96.8) |
| Oligodendroglioma | 87.4 (84.2–90.0) | 68.6 (63.1–73.5) | 78.5 (72.5–83.3) | 63.9 (55.3–71.3) | 81.3 (64.8–90.6) |
| Anaplastic oligodendroglioma | 70.8 (60.3–79.0) | 53.7 (37.8–67.2) | 75.6 (51.2–89.0) | 75.6 (41.7–91.4) | –a |
| Mixed glioma | 76.7 (69.3–82.5) | 60.5 (49.7–69.7) | 79.0 (64.9–87.9) | 68.0 (50.4–80.5) | 85.1 (45.6–96.7) |
| Astrocytoma (NOS) | 77.6 (74.5–80.3) | 65.2 (60.7–69.2) | 83.5 (78.4–87.4) | 74.6 (68.3–79.9) | 89.1 (78.2–94.7) |
| Glioma malignant (NOS) | 82.3 (77.0–86.4) | 74.2 (66.0–80.8) | 90.0 (79.6–95.2) | 79.8 (66.4–88.3) | 88.1 (63.5–96.5) |
| Embryonal/primitive medulloblastoma | 84.8 (80.5–88.3) | 74.0 (67.2–79.5) | 87.0 (79.4–91.9) | 80.2 (69.9–87.2) | 92.1 (69.3–98.2) |
| Lymphoma | 61.0 (53.8–67.4) | 43.8 (34.0–53.3) | 71.2 (54.9–82.5) | 57.7 (36.5–74.1) | 78.6 (27.9–95.6) |
| Meningioma, malignant | 82.2 (73.1–88.5) | 63.6 (49.3–74.9) | 76.5 (59.1–87.3) | 50.3 (28.9–68.4) | 64.5 (23.6–87.6) |
| Neoplasm, unspecified | 84.8 (77.3–90.0) | 80.4 (66.2–89.1) | 91.2 (72.4–97.4) | 78.4 (57.9–89.7) | 85.6 (48.6–96.7) |
| Ependymoma | 91.8 (88.2–94.3) | 84.8 (78.7–89.2) | 92.3 (81.6–96.9) | 85.2 (72.6–92.3) | 91.3 (68.1–97.9) |
| Germ cell tumor | 96.2 (90.5–98.5) | 92.0 (82.2–96.5) | 95.7 (73.2–99.4) | 87.7 (67.4–95.8) | 91.7 (50.6–98.9) |
| Primarily nonmalignant | |||||
| Pilocytic astrocytoma | 96.7 (94.6–98.0) | 95.9 (92.6–97.8) | 99.2 (91.6–99.9) | 96.8 (89.5–99.0) | 96.7 (85.3–99.3) |
| Hemangioblastoma/hemangioma | 96.1 (89.7–98.5) | 93.9 (80.5–98.2) | 97.6 (69.3–99.8) | 88.8 (68.7–96.3) | 92.9 (45.9–99.3) |
| Craniopharyngioma | 95.0 (85.6–98.3) | 82.5 (68.9–90.6) | 86.4 (72.8–93.5) | 81.1 (59.1–92.0) | 91.9 (28.7–99.4) |
| Meningioma, nonmalignant | 96.4 (95.0–97.5) | 88.7 (85.8–91.1) | 92.0 (89.2–94.1) | 85.1 (80.0–88.9) | 91.6 (83.3–95.8) |
| Nerve sheath and other cranial/spinal nerve tumor | 99.7 (98.4–99.9) | 99.3 (52.8–100) | 99.1 (50.6–100) | 99.1 (19.8–100) | 99.1 (0–100) |
| Pituitary tumor | 96.5 (94.5–97.8) | 92.6 (88.6–95.2) | 95.9 (89.0–98.5) | 86.5 (79.7–91.2) | 90.5 (80.3–95.5) |
| Neuronal/glial, nonmalignant and malignant | 91.6 (85.4–95.2) | 86.3 (76.2–92.4) | 94.4 (69.7–99.1) | 87.7 (65.8–96.0) | 92.5 (46.1–99.2) |
| All other brain tumors | 86.9 (81.0–91.1) | 80.1 (70.2–87.1) | 92.0 (69.6–98.1) | 85.2 (63.8–94.4) | 93.1 (36.9–99.5) |
a The overall sample size was less than 16 cases.
CS = Conditional survival; NOS = not otherwise specified.
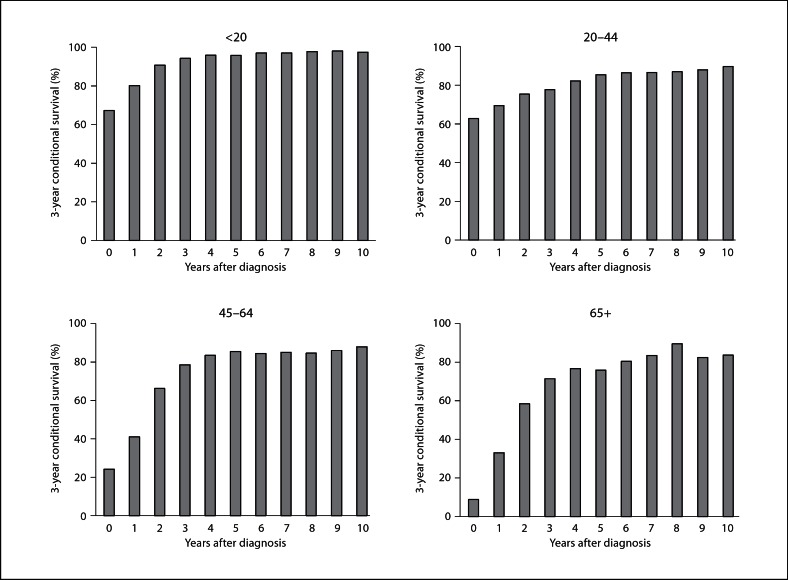
Among malignant tumor patients who had survived up to 10 years postdiagnosis, numeric gains in 3-year relative conditional survival were greater for the older age groups when compared with the younger age groups, and were thus more favorable (fig. 2). The 3-year relative conditional survival for 65+ year olds was 8.8% at time of diagnosis (time 0); if they survived an additional year the probability of surviving 3 additional years (to year 4) increased to 33.1%; and surviving yet another year increased the probability of surviving 3 additional years (to year 5) to 58.4%. For all age groups, conditional survival leveled off after 5 years postdiagnosis, indicating that the probability of surviving 3 additional years was similar regardless if survival was estimated after surviving up to 5 years or 10 years.
Fig. 2.
Relative probability of surviving 3 additional years in patients with primary malignant brain tumor (including those that were not confirmed microscopically) aged <20, 20–44, 45–64, and 65+ years conditional on having survived for up to 10 years postdiagnosis. Time 0 reflects the year of diagnosis.
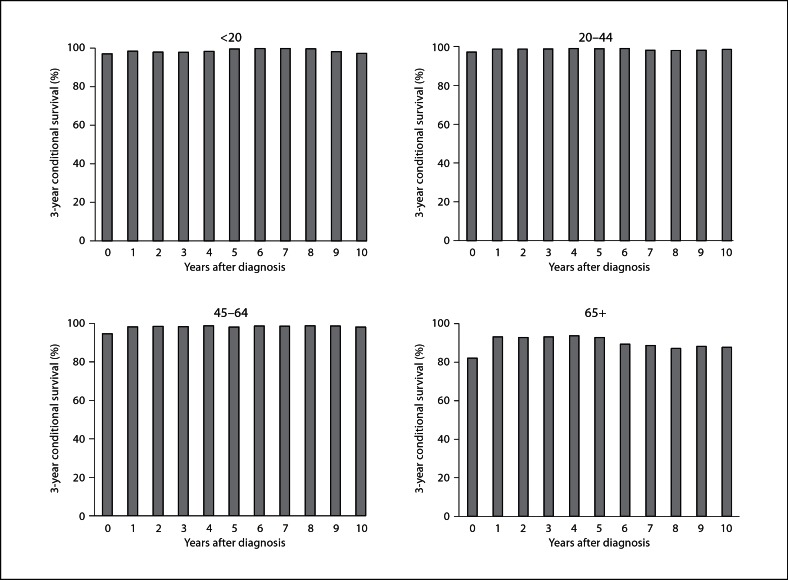
In contrast to the malignant tumor patterns, gains in 3-year relative conditional survival for survivors with nonmalignant tumors were only seen for the oldest age group (fig. 3). For these patients, results revealed modest gains in 3-year relative conditional survival during the first year postdiagnosis that plateaued up to year 5 (range: 92.9–93.7%) before slightly decreasing during years 6 through 10 postdiagnosis (range: 87.1–89.3%). For patients diagnosed up to age 64 years, 3-year relative conditional survival approached 100% regardless of the length of time survived postdiagnosis and remained constant thereafter.
Fig. 3.
Relative probability of surviving 3 additional years in patients with primary nonmalignant brain tumor (including those that were not confirmed microscopically) aged <20, 20–44, 45–64, and 65+ years conditional on having survived for up to 10 years postdiagnosis. Time 0 reflects the year of diagnosis.
Expanding on 3-year conditional survival rates presented in table 2, we stratified rates by age groups (table 4). In general, the pediatric group had the greatest probability of surviving 3 additional years to 5 years while the oldest age group had the lowest. However, the probability of surviving 3 additional years given survival to 2 years was more than 90% for nonmalignant tumors across all age groups. Contrary to other age groups, the lowest 3-year conditional survival for the oldest age group was diffuse astrocytoma [9.3% (95% CI: 0.5–34.0)] rather than glioblastoma [24.5% (95% CI: 14.0–36.5)]. A finding of lower 3-year conditional survival for >20-year-olds compared to the eldest age group among those with nerve sheath and other cranial/spinal nerve tumors was likely due to the small number of subjects in the >20 year old group (n = 21), which resulted in a very large confidence interval.
Table 2.
Short-term relative conditional survival (%) based on varying conditioning points with 95% confidence intervals for all primary brain tumors: 1985–2005
| 6-mo CS upon 0.5 year | 6-mo CS upon 1 year | 1-year CS upon 1 year | 6-mo CS upon 1.5 years | 1-year CS upon 2 years | |
|---|---|---|---|---|---|
| Years since diagnosis | 1 year | 1.5 years | 2 years | 2 years | 3 years |
| All brain tumors | 85.7 (84.9–86.5) | 90.6 (89.5–91.5) | 85.8 (84.6–86.9) | 94.7 (93.5–95.7) | 94.4 (92.9–95.6) |
| Tumor behavior | |||||
| Malignant | 74.9 (73.7–76.1) | 80.9 (79.2–82.4) | 71.6 (69.6–73.4) | 88.4 (86.3–90.2) | 87.8 (85.0–90.1) |
| Nonmalignant | 98.7 (97.9–99.2) | 99.5 (98.0–99.9) | 99.0 (97.7–99.6) | 99.5 (97.8–99.9) | 99.0 (97.5–99.7) |
| Specified histologic subtypes | |||||
| Primarily malignant | |||||
| Diffuse astrocytoma | 83.3 (78.3–87.2) | 84.7 (76.8–90.1) | 78.2 (67.7–85.6) | 92.2 (78.6–97.3) | 86.7 (70.5–94.4) |
| Anaplastic astrocytoma | 79.8 (76.5–82.7) | 84.6 (79.4–88.6) | 72.1 (65.3–77.8) | 85.1 (78.3–89.9) | 82.8 (72.6–89.4) |
| Glioblastoma | 52.9 (51.2–54.6) | 52.1 (49.2–55.0) | 30.9 (27.6–34.2) | 59.1 (54.3–63.6) | 56.0 (48.1–63.1) |
| Oligodendroglioma | 97.3 (95.8–98.3) | 96.7 (94.3–98.1) | 95.3 (91.9–97.3) | 98.6 (93.8–99.7) | 94.8 (90.5–97.1) |
| Anaplastic oligodendroglioma | 89.6 (84.0–93.4) | 90.7 (81.5–95.5) | 80.0 (67.6–88.1) | 88.2 (76.3–94.3) | 91.3 (65.6–98.1) |
| Mixed glioma | 92.0 (88.0–94.7) | 92.3 (85.9–95.9) | 84.2 (75.2–90.2) | 91.3 (82.8–95.7) | 90.2 (76.3–96.1) |
| Astrocytoma (NOS) | 82.0 (79.8–84.0) | 88.0 (84.7–90.7) | 82.2 (77.9–85.7) | 93.3 (88.7–96.1) | 91.1 (85.0–94.8) |
| Glioma, malignant (NOS) | 78.6 (74.9–81.8) | 84.8 (78.9–89.1) | 78.3 (70.8–84.1) | 92.3 (83.1–96.6) | 92.1 (78.1–97.3) |
| Embryonal/primitive medulloblastoma | 89.5 (86.5–91.9) | 92.2 (87.4–95.2) | 89.4 (83.2–93.4) | 97.0 (87.7–99.3) | 93.3 (84.4–97.2) |
| Lymphoma | 77.3 (73.3–80.7) | 83.8 (77.5–88.6) | 75.0 (66.8–81.5) | 89.4 (80.1–94.5) | 82.4 (70.4–89.9) |
| Meningioma, malignant | 94.9 (90.1–97.4) | 95.4 (87.0–98.4) | 92.7 (81.2–97.3) | 97.1 (80.2–99.6) | 92.7 (77.9–97.7) |
| Neoplasm, unspecified | 80.6 (75.3–84.9) | 89.5 (80.2–94.6) | 83.1 (71.7–90.3) | 92.8 (78.6–97.7) | 89.2 (71.6–96.1) |
| Ependymoma | 98.1 (96.2–99.0) | 97.4 (94.4–98.7) | 95.4 (91.1–97.7) | 98.0 (93.3–99.4) | 95.1 (89.5–97.7) |
| Germ cell tumor | 99.4 (95.5–99.9) | 96.8 (91.8–98.8) | 94.2 (85.6–97.7) | 97.3 (88.3–99.4) | 99.3 (0–100) |
| Primarily nonmalignant | |||||
| Pilocytic astrocytoma | 99.0 (97.8–99.5) | 99.7 (92.0–100) | 99.3 (95.8–99.9) | 99.5 (95.3–100) | 99.2 (94.7 99.9) |
| Hemangioblastoma/hemangioma | 98.8 (95.5–99.7) | 99.4 (79.1–100) | 99.4 (62.1–100) | 100a | 99.0 (79.9–100) |
| Craniopharyngioma | 99.4 (92.1–100) | 96.9 (90.3–99.0) | 95.7 (83.7–98.9) | 98.6 (71.9–99.9) | 99.7 (0–100) |
| Meningioma, nonmalignant | 98.4 (97.8–98.8) | 99.4 (98.2–99.8) | 98.8 (97.3–99.5) | 99.4 (97.8–99.8) | 98.9 (96.8–99.6) |
| Nerve sheath and other cranial/spinal nerve tumor | 99.9 (85.7–100) | 99.6 (97.3–100) | 99.3 (95.7–99.9) | 99.6 (96.1–100) | 99.7 (81.9–100) |
| Pituitary tumor | 99.5 (98.7–99.8) | 99.8 (92.8–100) | 99.4 (96.2–99.9) | 99.6 (96.8–100) | 99.4 (94.7–99.9) |
| Neuronal/glial, nonmalignant and malignant | 95.2 (91.4–97.3) | 4.7 (88.7–97.6) | 93.0 (84.6–96.9) | 98.2 (78.8–99.9) | 98.6 (30.2–100) |
| All other brain tumors | 93.1 (89.4–95.5) | 95.0 (88.8–97.8) | 91.9 (83.8–96.0) | 96.7 (86.3–99.2) | 95.3 (81.4–98.9) |
a Confidence interval undefined.
CS = Conditional survival; NOS = not otherwise specified.
Table 4.
Three-year conditional survival upon survival (%) for 2 years and 95% confidence intervals for all primary brain tumors by histology and age group
| Category | Age at diagnosis, years | |||
|---|---|---|---|---|
| >20 | 20–44 | 45–64 | 65+ | |
| All brain tumors | 93.5 (92.2–94.5) | 86.2 (84.9–87.3) | 87.8 (86.5–89.0) | 85.9 (83.7–87.9) |
| Tumor behavior | ||||
| Malignant | 90.7 (88.8–92.3) | 75.3 (73.2–77.2) | 66.2 (63.1–69.0) | 58.4 (52.9–63.4) |
| Nonmalignant | 97.9 (96.3–98.8) | 98.7 (97.9–99.2) | 98.5 (97.3–99.2) | 92.9 (90.3–94.8) |
| Specified histologic subtypes | ||||
| Primarily malignant | ||||
| Diffuse astrocytoma | 97.5 (83.0–99.6) | 69.8 (59.0–78.4) | 62.9 (39.5–79.4) | 9.3 (0.5–34.0) |
| Anaplastic astrocytoma | 78.7 (60.4–89.3) | 64.2 (57.2–70.4) | 50.3 (38.4–61.1) | 28.5 (8.6–52.6) |
| Glioblastoma | 70.0 (45.1–85.3) | 46.2 (38.4–53.7) | 28.0 (21.8–34.5) | 24.5 (14.0–36.5) |
| Oligodendroglioma | 98.6 (88.9–99.8) | 88.7 (84.6–91.8) | 80.3 (72.6–86.0) | 81.2 (57.1–92.5) |
| Anaplastic oligodendroglioma | –a | 71.9 (56.8–82.5) | 68.1 (50.7–80.5) | 80.7 (19.1–97.3) |
| Mixed glioma | 95.9 (73.5–99.4) | 74.3 (64.0–82.0) | 69.7 (52.9–81.5) | 74.5 (27.8–93.5) |
| Astrocytoma (NOS) | 96.0 (92.6–97.9) | 72.6 (67.9–76.7) | 68.2 (59.8–75.3) | 45.3 (27.4–61.5) |
| Glioma malignant (NOS) | 93.3 (87.0–96.6) | 79.6 (70.1–86.4) | 71.8 (57.4–82.0) | 57.1 (25.4–79.5) |
| Embryonal/primitive medulloblastoma | 88.8 (84.2–92.2) | 76.2 (65.7–83.9) | 76.7 (40.3–92.6) | –a |
| Lymphoma | –a | 66.9 (51.4–78.5) | 66.8 (55.1–76.1) | 50.1 (38.4–60.8) |
| Meningioma, malignant | –a | 85.3 (60.3–95.1) | 89.2 (75.7–95.4) | 75.8 (59.5–86.2) |
| Neoplasm, unspecified | 93.6 (76.6–98.4) | 88.7 (74.6–95.3) | 92.2 (75.4–97.7) | 70.2 (52.2–82.5) |
| Ependymoma | 85.7 (78.2–90.8) | 95.8 (90.7–98.2) | 95.2 (85.1–98.5) | 85.4 (55.8–95.8) |
| Germ cell tumor | 95.6 (88.2–98.4) | 97.4 (79.4–99.7) | –a | –a |
| Primarily nonmalignant | ||||
| Pilocytic astrocytoma | 97.2 (94.9–98.5) | 95.7 (89.1–98.3) | 93.1 (65.8–98.8) | –a |
| Hemangioblastoma/hemangioma | –a | 100b | 91.2 (78.1–96.6) | 89.1 (46.9–98.3) |
| Craniopharyngioma | 100b | 97.0 (79.4–99.6) | 89.3 (56.7–97.8) | 81.7 (35.2–96.2) |
| Meningioma, nonmalignant | 100b | 98.9 (97.1–99.5) | 98.5 (96.7–99.3) | 93.6 (90.4–95.7) |
| Nerve sheath and other cranial/spinal nerve tumor | 91.7 (53.6–98.8) | 98.7 (94.9–99.7) | 99.4 (96.0–99.9) | 98.8 (92.5–99.8) |
| Pituitary tumor | 100b | 98.7 (96.8–99.5) | 97.7 (93.7–99.1) | 89.2 (82.0–93.7) |
| Neuronal/glial, nonmalignant and malignant | 92.6 (82.8–96.9) | 93.0 (81.2–97.5) | 88.0 (67.5–96.0) | –a |
| All other brain tumors | 93.5 (92.2–94.5) | 86.2 (84.9–87.3) | 87.8 (86.5–89.0) | 85.9 (83.7–87.9) |
a The overall sample size was less than 16 cases.
b Confidence interval undefined.
NOS = Not otherwise specified.
Discussion
Population-based survival statistics are routinely used as prognostic measures at the clinical level. For surviving patients, conditional survival is a better measure of prognosis [1] than survival estimates derived from initial diagnosis. Conditional survival rates vary by histology and age and are generally higher than the corresponding relative survival estimates. Cancers with poor initial survival are most affected by conditional survival [10]. The difference between the 10-year relative survival estimate and 5-year relative conditional survival given survival to 5 years was 55.7% (26.9 vs. 82.6%) for malignant tumors but only 8.4% (86.5 vs. 94.9%) for nonmalignant tumors. Additionally, there is a threshold after which conditional survival rates stabilize as years since diagnosis increased. Despite more favorable conditional survival estimates than relative survival, trends differed by tumor behavior. In contrast to conditional survival estimates for many primarily nonmalignant tumors, conditional survival rates for long-term survivors with primarily malignant tumors still do not reach that of the general population, as these rates would be closer to 100%.
Higher 3-year relative conditional survival estimates given survival to 2 years (i.e. the probability of surviving to 5 years given survival to 2 years) compared with 5-year relative survival estimates was a common finding in the previous malignant brain tumor studies [2, 3, 4] and is consistent with the current study. Given survival to 2 years, our 3-year relative conditional survival estimate of 61.0% for anaplastic astrocytoma was higher than the 52.9% reported by Hwang et al. [3] while estimates for glioblastoma were comparable; albeit slightly lower in the current study (36.4 vs. 40.0%). The 3-year relative conditional survival estimates (given survival to 2 years) for patients with a glioblastoma [36.4% (95% CI: 31.8–41.0) vs. 36.4% (95% CI: 31.9–41.6)] or pilocytic astrocytoma [96.7% (95% CI: 94.6–98.0) vs. 96.4% (95% CI: 93.6–99.1)] were the same regardless of whether the cohort was diagnosed in 1985–2005 as in the current study or in 1979–1993 [2]. Similarities in conditional survival estimates for tumors diagnosed in 1985–2005 versus 1979–1993 suggest that there were no major improvements in the clinical management for many of these tumor histologies between these time periods. Our 3-year relative conditional survival estimates given survival to 2 years were greater than the previous US study [2] for some histologies (oligodendroglioma; anaplastic oligodendroglioma; astrocytoma (NOS), glioma malignant (NOS); embryonal/primitive/medulloblastoma) but lower for others (diffuse astrocytoma; anaplastic astrocytoma; mixed glioma). The general trend of malignant estimates leveling off over time and steeper conditional survival for the two older groups was shared by the current study and the previous report [2]. A greater frequency of gliomas diagnosed at older ages are more anaplastic and aggressive than gliomas diagnosed at younger ages [11, 12], which could account for the differences in slope of the conditional survival curves between age groups. Direct comparison of overall malignant estimates was not possible due to the coding of pilocytic astrocytoma, a pediatric tumor with good prognosis, as nonmalignant in this study but as a malignant tumor in the previous study. However, it is likely that the relative conditional survival for malignant tumors in the current study [75.4% (95% CI: 74.0–76.7)] would have been greater than that for the previous US study [76.2% (95% CI: 74.8–77.6)] had pilocytic astrocytoma been included as a malignant tumor.
This study provides estimates of relative conditional survival for both primary malignant and nonmalignant brain tumors. The analysis of nonmalignant tumors not only enables an assessment of these patterns but also allows comparison of these estimates to malignant tumors. The current study includes longer years of follow-up and more conditioning points than previously reported [2]. Six-month, 1-, 3-, 5-, 8-, and 10-year conditional survival rates were assessed for varying years of survival after diagnosis which provided an expanded observation of prognosis for brain tumor survivors. The number of patients who survived to 5 years in the oldest age group was more robust compared to the previous study [2] which enabled assessment of trends for more histologic types for this patient subgroup.
Our dataset does not contain information on co-morbidities, treatment, risk factors, or other outcomes (i.e. progression, recurrence), which could greatly affect the reported estimates. Estimates were less stable for rare histologies and histologies with poor prognosis. Additionally, there is a potential bias for nonmalignant tumors since there is a possibility that multiple primaries from other cancer sites were included, and this may have resulted in more pessimistic estimates. Finally, as the conditioning points increased, the subset of survivors decreased which may also have led to less stable estimates as well as issues with generalizability. As there are few reports of 15-year survival estimates by histology for brain tumors, it was difficult to gauge whether the relative survival rates presented here are reflective of the larger community of brain tumor patients. In table 1, 3- and 8-year conditional survival rates were based on the percentage of patients who survived to 2 years while 5-year conditional survival for 5- and 10-year survivors were based on a smaller percentage of patients who had already survived to 5 and 10 years, respectively.
Conclusion
A brain tumor diagnosis can be quite devastating and conjure feelings of uncertainty and despair. This analysis confirms that conditional survival provides more relevant and encouraging prognoses for all surviving brain tumor patients than relative survival estimated from the time of diagnosis. These population-level survival estimates, in conjunction with individual patient risk assessment, can serve as an additional disease surveillance measure for clinicians to present current expected prognosis to their surviving brain tumor patients in order to give them hope for the future, particularly to the elderly and patients with malignant tumors.
Acknowledgments and Funding
This work was supported by the Central Brain Tumor Registry of the United States. Kimberly Porter was supported by a NCI predoctoral fellowship through the cancer prevention and control training grant (2 R25 CA057699-18, co-Is Davis, FG and Fitzgibbon, ML). She is currently a post-doctoral research fellow at Kaiser Permanente Southern California, Department of Research and Evaluation.
The authors gratefully acknowledge the collaborators at state registries that provided data for this analysis: Ms. Cathryn Phillips, Connecticut Tumor Registry and Ms. Rosemary Dibble, Utah Cancer Registry.
Disclosure Statement
The authors report no conflicts of interest.
References
- 1.Henson DE, Ries LA. On the estimation of survival. Semin Surg Oncol. 1994;10:2–6. doi: 10.1002/ssu.2980100103. [DOI] [PubMed] [Google Scholar]
- 2.Davis FG, McCarthy BJ, Freels S, Kupelian V, Bondy ML. The conditional probability of survival of patients with primary malignant brain tumors: surveillance, epidemiology, and end results (SEER) data. Cancer. 1999;85:485–491. [PubMed] [Google Scholar]
- 3.Hwang SL, Yang YH, Lieu AS, Chuang MC, Chang SJ, Chang YY, et al. The conditional survival statistics for survivors with primary supratentorial astrocytic tumors. J Neurooncol. 2000;50:257–264. doi: 10.1023/a:1006484220764. [DOI] [PubMed] [Google Scholar]
- 4.Lin CL, Lieu AS, Lee KS, Yang YH, Kuo TH, Hung MH, et al. The conditional probabilities of survival in patients with anaplastic astrocytoma or glioblastoma multiforme. Surg Neurol. 2003;60:402–406. doi: 10.1016/s0090-3019(03)00322-7. discussion 406. [DOI] [PubMed] [Google Scholar]
- 5.Central Brain Tumor Registry of the United States: CBTRUS Statistical Report 2010: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2004–2006. Hinsdale, IL. Available at www.cbtrus.org Accessed on April 1, 2009.
- 6.Surveillance, Epidemiology, and End Results (SEER) Program: Research Data (1973–2006), National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2009, based on the November 2008 submission. Available at www.seer.cancer.gov Accessed on May 15, 2009.
- 7.Surveillance, Epidemiology, and End Results (SEER) Program: www.seer.cancer.gov Accessed January 11, 2010.
- 8.SAS System software. Release 9.2. SAS Institute Inc, Cary, NC; 2004.
- 9.Surveillance Research Program, National Cancer Institute SEER*Stat software version 6.6.2; 2010. Available at www.seer.cancer.gov/seerstat
- 10.Henson DE, Ries LA, Carriaga MT. Conditional survival of 56,268 patients with breast cancer. Cancer. 1995;76:237–242. doi: 10.1002/1097-0142(19950715)76:2<237::aid-cncr2820760213>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 11.Kaloshi G, Psimaras D, Mokhtari K, Dehais C, Houillier C, Marie Y, et al. Supratentorial low-grade gliomas in older patients. Neurology. 2009;73:2093–2098. doi: 10.1212/WNL.0b013e3181c6781e. [DOI] [PubMed] [Google Scholar]
- 12.Belford K. Central nervous system cancers. In: Yarbro C, Frogge M, Goodman M, editors. Cancer Nursing: Principles and Practice. ed 6. Sudbury, Massachusetts: Jones and Bartlett Publishers; 2005. pp. 1089–1136. [Google Scholar]