Abstract
Background
Despite evidence of a positive effect of collaborative patient-provider communication on patient outcomes, our understanding of this relationship is unclear.
Purpose
To determine whether racial composition of the relationship modified the association between ratings of provider communication and medication adherence.
Methods
Effect modification of the communication-adherence association, by racial composition of the relationship, was evaluated using general linear mixed models while adjusting for selected covariates.
Results
390 patients were in race-concordant (black patient, black provider) relationships, while 207 were in race-discordant (black patient, white provider) relationships. The communication-adherence association was significantly modified in race-discordant relationships (p=0.04). Communication rated as more collaborative in race-discordant relationships was associated with better adherence, while communication rated as less collaborative was associated with poor adherence. There was no significant association between adherence and communication in race-concordant relationships (p=0.24).
Conclusions
Collaborative patient-provider communication may play an influential role in black patients’ adherence behaviors when receiving care from white providers.
Keywords: hypertension, medication adherence, communication, race concordance
INTRODUCTION
The quality of patient-provider communication has been identified as an important and potentially modifiable factor associated with improved patient outcomes. Patient-provider communication that is characterized by shared-decision making and patient-centeredness is associated with better self-reported adherence in patients with chronic diseases (1–12). In our previous work, we demonstrated that provider communication rated by patients as collaborative was associated with better adherence to antihypertensive medications in low-income hypertensive black patients (13). Despite the mounting evidence of the positive relationship between collaborative patient-provider communication and medication adherence, particularly in minority populations (1, 2, 5, 8–10, 13), the basis of this association has not been well-studied.
Race-concordant relationships (i.e., when patient and provider belong to the same racial background) may contribute to the higher rates of medication adherence noted in collaborative patient-provider interactions. Specifically, patients’ views about satisfaction, trust, and feeling respected during the medical encounter have emerged as important outcomes that differ by patient race (14–17). Race-concordant patient-provider relationships, as opposed to race-discordant, have been found to result in longer medical visits with higher ratings of positive affect, shared-decision making, and satisfaction (14, 18, 19). Although the effect of race-concordant relationships on improved processes of care (i.e., patient satisfaction and healthcare utilization) (14, 16–18, 20–22) has been clearly documented, the effect on patient outcomes such as medication adherence is unclear (23–28). Recent studies have found no association between racial composition of the relationship and health outcomes, including medication adherence, treatment intensification, and blood pressure control (24, 25). However, these studies did not assess factors that may contribute to this relationship, limiting the ability to understand the potential reasons for the lack of association.
The aim of this study was to determine whether there is a differential association between patient ratings of provider communication and medication adherence by the racial composition of the patient-provider relationship, in 597 hypertensive black patients followed in urban community health centers. We hypothesized that provider communication rated as less collaborative would be associated with worse adherence and that this association would be stronger for patients in race-discordant relationships compared to those in race-concordant relationships. Examining whether the association between communication and medication adherence is influenced by the racial composition of the patient-provider relationship is an important next step to identifying the circumstances under which interpersonal processes affect hypertension-related health outcomes,(24, 29) one of the major chronic diseases contributing to the racial mortality gap between blacks and whites.(30)
METHODS
Study Design and Participants
This study was conducted as part of a randomized clinical trial, Counseling African Americans to Control Hypertension (CAATCH), in 30 community health centers in the New York metropolitan area. The purpose of CAATCH was to evaluate the effectiveness of a multi-level intervention in improving blood pressure control among black patients with uncontrolled hypertension. The CAATCH intervention was comprised of a number of evidence-based components and targets both patients and providers to promote patient self-management skills and provider adherence to established guidelines for hypertension treatment. All questionnaires for this cross-sectional study were administered at the baseline visit before patients were randomized to the intervention or control conditions, thus eliminating any influence the intervention may have had on the present study’s measures.
Eligibility criteria for the CAATCH trial include: a) self-identification as black/African American; b) having a diagnosis of hypertension (defined as an average blood pressure ≥140/90 mmHg on at least two previous visits in the previous year); c) uncontrolled blood pressure at the eligibility visit (BP ≥140/90 mmHg or ≥130/80 mmHg for those with kidney disease or diabetes) based on the mean of the final 2 of the 3 measurements using a validated automated blood pressure monitor (BPTru) (31); d) taking at least 1 antihypertensive medication; and e) being 18 years or older; and f) English-speaking (32). For the present study, eligible patients were limited to those who received care from a black or white healthcare provider (n = 691). Patients identified their current provider during the enrollment visit. Of these, an additional 94 were excluded due to incomplete data, yielding a final sample of 597 patients (86%). Other than having a higher proportion of patients with low income (69% vs. 80%, respectively, p < 0.001), excluded patients did not differ significantly from those in the final sample in terms of age, sex, educational level, insurance status, baseline systolic and diastolic blood pressure, or comorbidity. Providers were enrolled in the CAATCH trial if they were: a) a provider (i.e., physician, nurse practitioner) in the participating sites, and b) providing care to at least 5 patients with uncontrolled blood pressure. Of the 97 providers participating in CAATCH, 69 (71%) were eligible to participate in the present study because they self-identified as white or black. Ineligible providers included those that self-identified as Latino (8.2%), Asian (11.3%), East Indian (4.3%), and as Other (5.2%). Patients were more likely to report receiving care for less than 5 years with ineligible providers as compared to eligible providers (36% vs. 29%, respectively, p = 0.004); otherwise provider characteristics were similar for both groups.
The final sample comprised 597 patients and 69 providers (27 white and 42 black), yielding 207 race-discordant relationships and 390 race-concordant relationships. All participants provided written informed consent approved by the Columbia University and New York University Medical Center Institutional Review Boards.
Study Measures
Patient-provider relationships were grouped into 2 categories: a) Race-concordant relationship, defined as a dyad where the patient and provider belong to the same race (black provider and black patient), and b) Race-discordant relationship, defined as a dyad where the patient is black and the provider is white.
Medication adherence was assessed with the well-validated Morisky scale, a self-report measure that asks patients to respond “yes” or “no” to the following questions: a) Have you ever forgotten to take your medicine? b) Are you sometimes careless in regards to your medicine? c) Do you skip your medicine when you are feeling well? and d) When you feel badly due to the medicine, do you skip it? (33) The scale was coded such that patients received a score of “1” for each negative response, with higher scores indicating better adherence (range: 0 – 4). The Cronbach’s alpha for this sample was 0.67, which is consistent with the estimate of Morisky et al.(33) To provide a more objective assessment of the effectiveness of the medication adherence measure, patient’s adherence level was compared to their baseline blood pressure readings. The association between better medication adherence and lower diastolic blood pressure was significant (p = 0.003).
Patient rating of provider communication was assessed with a measure adapted from a study of the effect of physician communication style on beliefs and medication-taking behaviors of patients with depression (3). This scale assesses the extent to which patients felt the provider encouraged their participation in treatment decisions and monitored their medication use. In the original 13-item scale, 2 items required categorical (yes/no) responses and ask whether the patient was given written information about the medication and if a follow-up appointment was scheduled. Given that different metrics (e.g., categorical) were used for these items, they were dropped to form an 11-item scale for this study. Responses for the first eleven questions range from 1 = not at all to 4 = very much. Individual items are summed to form a total continuous score (range: 11–44), with higher scores signifying more collaborative communication. Sample questions include “To what degree is your doctor: 1) friendly during the visit, and 2) asking about your concerns. Responses were scored from not at all to very much. Because scores were substantially negatively skewed, the scale was reverse-scored and then log transformed prior to data analysis. As a result, lower scores on the log-transformed scale are indicative of more collaborative communication, and the parameter estimates in the regression models indicate the amount of adherence for a 1-unit change on the log-transformed poor communication scale (range: 1 – 4). The properties of the 11-item measure were reevaluated and found to be satisfactory with a Cronbach alpha of 0.92 in our sample compared to an alpha of 0.84 reported by Bultman and Svarstad (3).
Covariates included comorbidity, provider exposure to cultural competency training, and demographic variables. Comorbidity was assessed at the patient’s baseline visit with the Charlson Comorbidity Index (34), a weighted index of the longitudinal risk of mortality attributable to comorbid disease. For this self-report measure, patients respond “yes” or “no” to 19 categories of comorbidity (e.g., diabetes, stroke). The total comorbidity risk score reflects the cumulative increased likelihood of one-year mortality; the higher the total score, the more severe the burden of comorbidity. An assessment of provider’s exposure to cultural competency training was included in this study to adjust for the potential confounding effects increased cultural sensitivity may have on the quality of communication across the dyad types. Self-reported cultural competency training was assessed using a modified version of the medical training subscale of the Clinical Cultural Competency Questionnaire (35). The Clinical Cultural Competency Questionnaire was developed as a tool to measure clinician’s knowledge, skills, and attitudes relating to the provision of culturally competent healthcare to diverse patient populations (36). As part of the questionnaire, clinicians rate the amount of cultural diversity training they have been exposed to during four time periods over their medical education and training: a) in college, b) during postgraduate studies, c) during medical training, and d) as a faculty member. Responses are based on a Likert-type scale ranging from 1 = none, to 5 = a lot. Total scores for each provider were calculated by summing responses across all four time periods. The measure’s Cronbach’s alpha was 0.82 in a sample of primary care providers in healthcare centers across the United States (36).
Demographic data collected at the patient-level included age, sex, place of birth, marital status, employment status, educational and income level, insurance status, length of relationship with current provider, number of antihypertensive medications, mean systolic and diastolic blood pressure. Patient blood pressure was measured by trained research assistants with a validated automated blood pressure device following standard American Heart Association guidelines (31, 37). Provider-level demographic data collected included age, sex, place of birth, duration of practice at the site, type of provider (i.e., physician, nurse practitioner) and specialty.
Statistical Analyses
Descriptive statistics were used to describe all patient and provider-level variables. The demographics of the two categories of patient-provider dyads were compared using chi-square for categorical variables and independent t-tests for continuous variables. Regression analyses were used to test the effects of racial composition of the relationship and patient’s ratings of provider communication on medication adherence. Patient- and provider-level variables were included in the multivariate models if they were associated with the racial composition of the relationship at p < 0.10 in bivariate analyses; or there was evidence from the literature that the variables were potential confounders of medication adherence or patient-provider communication (i.e., patient age as a confounder of medication adherence and length of patient-provider relationship as a confounder of communication).
Due to the mixed sample of physicians and non-physicians, it may be argued that the true effect of race concordance on perceived communication and medication adherence in this study will be confounded by provider type. That is, nurse practitioners as well as physician assistants are typically trained under a more holistic approach in which there is greater emphasis on relationship building and cultural competence. This hypothesis was tested with an ANOVA and resulted in no significant relationship between provider type and patients’ perceived communication score (F (2, 67) = 1.82, p = .16). Further, a Tukey follow-up test indicated that the nurse practitioners’ communication score were not significantly higher (M = 2.69; SD = 0.38) than both the physician (M = 2.87; SD = 0.39, p = 0.16) and physician assistant (M = 2.91; SD = 0.38, p = 0.20) groups. Despite this non-significance, provider type was controlled for in all adjusted models.
Given the nested nature of the data (patients within providers within sites), all analyses were conducted using generalized linear mixed models (GLMM). Providers were modeled as the random effect to adjust for potential nesting caused by multiple patients seeing the same provider. All independent variables were modeled as fixed effects, including patient demographics and provider characteristics. Two GLMM models were conducted to determine whether the association between patients’ ratings of provider communication and medication adherence was modified by racial composition of the relationship. In the first model, independent associations between the two main factors (communication and racial composition) and the dependent variable (medication adherence) were assessed, while adjusting for selected patient- and provider-level covariates. In Model 2, the product term between racial composition of the relationship and provider communication was added to Model 1. The procedures described in Bauer and Curran (38) were used to interpret the nature of the racial composition x communication interaction on medication adherence in post hoc analyses. Specifically the simple linear slopes of the regression of medication adherence onto communication for the race-concordant and race-discordant relationships were evaluated. SPSS version 18 (39) was used for all analyses and significance levels were set at p ≤ 0.05.
RESULTS
Patient and Provider Characteristics
The majority of patients were female, unemployed, and reported a household income of less than $20,000/year (Table 1). Mean blood pressure was 151/91 mmHg, with about a third reporting a comorbidity score of ≥ 3. Most (88%) of the patients reported receiving care from their current provider for at least one year. The mean medication adherence score was 2.86 (SD 1.23; range: 0 – 4, higher scores indicate better adherence) with a non-adherence rate of 59% (patient responded ‘yes’ to any question on the Morisky scale). The mean score on communication scale (represented as the raw mean prior to log-transformation) was 1.75 (SD 0.73; range: 1 – 4, lower scores are indicative of more collaborative communication). The majority of providers were female and internists, with a mean age of 49 years and practice duration of 8.55 years (Table 2). Of the patients enrolled in the study, white providers saw an average of 7.6 (5.56) patients while black providers provided care to an average of 9.29 (7.87) patients. White providers worked at their clinics significantly longer than black providers (9.96 years vs. 7.65 years, p = 0.03); were more likely to be nurse practitioners (15% vs. 2%, p = 0.05) and report being born in the United States. (67% vs. 46% p = 0.08; Table 2).
Table 1.
Comparison of Patient Characteristics by Racial Composition of the Patient-Provider Relationship (N = 597)*
| Patient Characteristics** | All Patients (N = 597) | Race-Concordant Relationship† (n = 390) | Race-Discordant Relationship‡ (n = 207) | p* |
|---|---|---|---|---|
| Mean age (± SD) Range: 24–89 years | 57.3 (12.3) | 57.4 (12.7) | 58.6 (13.4) | 0.30 |
| Female: n (%) | 411 (69) | 262 (67) | 149 (72) | 0.26 |
| Marital status: n (%)* | ||||
| Single | 155 (26) | 92 (24) | 63 (30) | |
| Married | 145 (24) | 104 (27) | 41 (20) | 0.05 |
| Divorced/Separated | 173 (29) | 115 (30) | 58 (28) | |
| Widowed | 85 (14) | 48 (12) | 37 (18) | |
| Education: n (%) | ||||
| < High school | 227 (38) | 148 (38) | 79 (38) | 0.89 |
| High school | 199 (33) | 128 (33) | 71 (34) | |
| Some college | 171 (29) | 114 (29) | 57 (28) | |
| Unemployed: n (%) | 378 (63) | 240 (62) | 138 (67) | 0.24 |
| Income (%) | ||||
| ≤ $20,000 | 398 (67) | 261 (67) | 137 (66) | 0.41 |
| Insurance status: n (%) | ||||
| None | 53 (9) | 37 (10) | 16 (8) | |
| HMO/Private | 108 (18) | 65 (17) | 43 (21) | |
| Medicare | 158 (26) | 103 (26) | 55 (27) | 0.56 |
| Medicaid | 242 (41) | 164 (42) | 78 (38) | |
| Comorbidity score: n (%) | ||||
| 0 | 107 (18) | 74 (19) | 33 (16) | |
| 1 | 128 (21) | 79 (20) | 49 (24) | 0.61 |
| 2 | 133 (22) | 89 (23) | 44 (21) | |
| 3 or more | 206 (35) | 131 (34) | 75 (36) | |
| Comorbity: n (%) | ||||
| Congestive Heart Failure | 76 (13) | 49 (13) | 27 (13) | 0.97 |
| Stroke | 57 (10) | 31 (8) | 26 (13) | 0.09 |
| Myocardial Infarction | 51 (9) | 35 (9) | 16 (8) | 0.54 |
| Diabetes | 185 (31) | 110 (28) | 75 (36) | 0.07 |
| Mean blood pressure (± SD) | ||||
| Systolic BP (Range: 114–211mm Hg) | 151 (15.7) | 151 (15.3) | 151 (16.3) | 0.36 |
| Diastolic BP (Range: 67–141mm Hg) | 91 (10.9) | 91 (10.9) | 90 (10.9) | 0.86 |
| Mean N of meds (± SD) Range: 1–5 | 1.94 (0.9) | 1.88 (0.89) | 2.05 (1.04) | 0.09 |
| Seeing current provider ≥ 1 yr: n (%) | 526 (88) | 345 (89) | 181 (87) | 0.71 |
| Raw mean communication score¥ Range: 1–4 | 1.75 (0.73) | 1.81 (0.75) | 1.63 (0.67) | 0.007 |
| Mean adherence score Range: 0 – 4 | 2.86 (1.23) | 2.88 (1.22) | 2.81 (1.26) | 0.36 |
| % non-adherent | 59.0 | 58.3 | 60.0 | 0.38 |
p values for t-tests for continuous variables and chi-square for categorical variables
Values for marital status, insurance status, and comorbidity score do not add to the total sample size for each column due to missing data
Black patient and black provider
Black patient and white provider
Lower scores are indicative of more collaborative provider communication
Table 2.
Comparison of Characteristics by Provider Race (N = 69)
| Characteristics | All Providers (N = 69) | Black Providers (n = 42) | White Providers (n = 27) | p* |
|---|---|---|---|---|
| Mean Age (± SD) Range: 26 – 81 years | 49.28 (10.74) | 48.51 (9.33) | 50.48 (12.74) | 0.17 |
| Female: n (%) | 39 (57) | 23 (55) | 16 (59) | 0.59 |
| Type of Provider: n (%) | ||||
| Physician | 59 (86) | 38 (90) | 21 (78) | |
| Nurse Practitioner | 5 (7) | 1 (2) | 4 (15) | 0.05 |
| Physician Assistant | 5 (7) | 3 (8) | 2 (7) | |
| Specialty: n (%) | ||||
| Internal Medicine | 41 (60) | 25 (60) | 16 (60) | 0.25 |
| Born in United States: n (%) | 36 (55) | 18 (46) | 18 (67) | 0.08 |
| Mean Cultural Competency Training (± SD) Range: 1 – 5 | 2.75 (0.99) | 2.64 (1.02) | 2.91 (0.93) | 0.43 |
| Mean years providing care at site (± SD) Range: 3 months – 27 years | 8.55 (6.58) | 7.65 (5.64) | 9.96 (7.74) | 0.03 |
p values for t-tests for continuous variables and chi-square for categorical variables
Comparisons of patient characteristics by racial composition of the relationship are also shown in Table 1. Patients in race-discordant relationships were more likely to report being single and/or widowed (p = 0.05), prescribed more antihypertensive medications (2.05 vs. 1.88 p = 0.09), have comorbid diabetes (37% vs. 28% p = 0.07) and stroke (13% vs. 8% p = 0.09) than those in race-concordant relationships. On average, patients in race-discordant relationships rated their provider as more likely to listen to them, provide clear instructions on how to take their medications, talk about things that could help the patient feel better, and help solve problems than patients in race-concordant relationships (Table 3). Because of the significant relationship between patient’s marital status, comorbid diabetes and stroke, and antihypertensive medications; as well as type of provider, place of birth, and years at their site; these variables were included as covariates in the multivariate analysis.
Table 3.
Association between Race Composition of the Relationship and Components of Collaborative Communication
| Scale Item* (range: 1 – 4) | Raw Mean Score (SD)†
|
p | |
|---|---|---|---|
| Race-Concordant Relationship (n = 390)‡ | Race-Discordant Relationship (n = 207)¥ | ||
| Asked if had questions or concerns | 2.08 (1.05) | 1.99 (0.99) | 0.30 |
| Helped with concerns related to the use of medication | 1.91 (0.99) | 1.84 (0.97) | 0.75 |
| Friendly during the visit | 1.41 (0.68) | 1.34 (0.61) | 0.08 |
| Gave clear instructions on how to take medication | 1.60 (0.86) | 1.40 (0.72) | 0.001 |
| Listened to you | 1.48 (0.74) | 1.36 (0.61) | 0.001 |
| Gave clear explanation about how medication would affect you | 1.88 (1.04) | 1.68 (0.96) | 0.14 |
| Talked about things that you could do to help you feel better | 1.82 (1.01) | 1.59 (0.86) | 0.003 |
| Encourages expression of problems | 1.99 (1.08) | 1.73 (0.97) | 0.11 |
| Asks about concerns | 2.01 (1.12) | 1.69 (0.98) | 0.08 |
| Listens to your concerns | 1.72 (0.90) | 1.53 (0.86) | 0.43 |
| Helped solve problems | 2.03 (1.11) | 1.76 (0.94) | 0.006 |
Lower scores are indicative of more collaborative provider communication
Items reflect raw mean score on untransformed communication scale
Black patient and black provider
Black patient and white provider
Race, Patient-Provider Communication, and Medication Adherence
After adjusting for selected patient (age, gender, marital status, insurance status, comorbidity, number of medications, and length of patient-provider relationship) and provider characteristics (place of birth, type of provider, cultural competency training, and years at site), there was a significant main effect of patient-provider communication on medication adherence in Model 1 (B = −0.46, p = 0.04) such that provider communication rated as more collaborative was associated with better medication adherence (Table 4). Racial composition of the relationship was not associated with medication adherence (p = 0.39). The interaction term was added to Model 1 to determine whether racial composition modified the association between patient-provider communication and medication adherence (Model 2). As shown in Table 4, there was a significant effect modification of the association between patient-provider communication and medication adherence by racial composition of the relationship (B = 0.95, p = 0.04). Post hoc analysis of the interaction effect indicates that the simple slope for race-discordant relationships is significantly different from zero (t(216) = 2.99, p = 0.003). That is, as ratings of white providers’ communication progress from collaborative to non-collaborative, black patients are significantly more likely to report poor medication adherence. However, the test of the simple slope is non-significant in race-concordant relationships indicating that there is no relationship between communication and adherence in patient-provider relationships (t(216) = 0.11, p = 0.91). Figure 1 displays the results of Model 2.
Table 4.
Results of GLMM Testing the Effect Modification of the Association between Patient-Provider Communication and Medication Adherence by Racial Composition of the Relationship (N = 597)*†
| Model 1
|
Model 2
|
|||||||
|---|---|---|---|---|---|---|---|---|
| df | F | B (SE) | p | df | F | B (SE) | p | |
| Patient age | 1 | 3.12 | 0.01 (0.01) | 0.08 | ||||
| Patient gender Male | 1 | 0.15 | −0.07 (0.17) | 0.70 | ||||
| Marital Status | 3 | 0.62 | 0.61 | |||||
| Insurance status | 3 | 0.45 | 0.72 | |||||
| Diabetes | 1 | 0.88 | 0.16 (0.17) | 0.35 | ||||
| Stroke | 1 | 5.10 | −0.69 (0.31) | 0.03 | ||||
| # hypertension meds | 1 | 0.54 | 0.06 (0.08) | 0.46 | ||||
| Length of relationship ≥1 year | 1 | 3.65 | 0.52 (0.27) | 0.06 | ||||
| Provider birthplace U.S. | 1 | 4.15 | −0.35 (0.17) | 0.04 | ||||
| Type of provider Physician | 1 | 2.59 | 0.42 (0.26) | 0.11 | ||||
| Cultural competency training | 1 | 1.64 | −0.10 (0.08) | 0.20 | ||||
| Years at clinic | 1 | 0.01 | 0.001 (0.01) | 0.93 | ||||
| Communication | 1 | 4.46 | −0.46 (0.22) | 0.04 | 1 | 8.25 | −1.11 (0.39) | 0.005 |
| Dyad type | 1 | 0.75 | 0.17 (0.20) | 0.39 | 1 | 1.38 | 0.23 (0.20) | 0.24 |
| CommunicationxDyad | 1 | 4.14 | 0.95 (0.47) | 0.04 | ||||
Controlling for clustering by providers
Regression coefficients are only reported for those constructs represented by single variables
Figure 1.
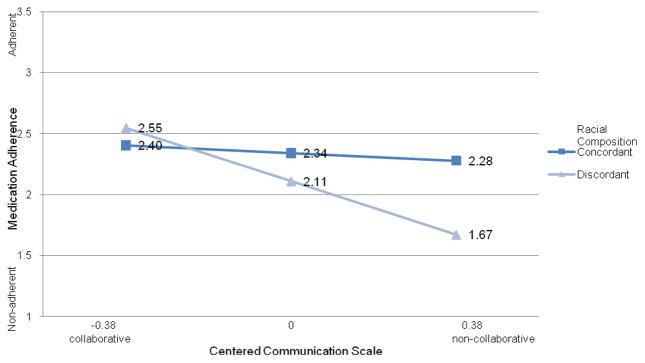
Effect Modification of the Communication-Adherence Association by Racial Composition of the Patient-Provider Relationship
DISCUSSION
Our study shows that black hypertensive patients in race-discordant relationships who rated communication as collaborative reported better medication adherence, with levels similar to those reported by patients in race-concordant relationship. Conversely, white providers’ communication that was rated as less collaborative was associated with poor adherence. There was no significant association between medication adherence and ratings of provider communication in race-concordant relationships.
Although our findings corroborate a growing body of research documenting the effect of patient-provider communication on patient outcomes (7, 11, 12, 40), this appears to be the first study to evaluate the role of racial composition of the relationship as an effect modifier of the association between quality of communication and medication adherence. To date, four studies have assessed the effect of race concordance on medication adherence (24,27,28, 41). Using data from the Piedmont Health Survey of the Elderly, Howard et al. (41) and Konrad et al. (28) found that race concordance had little effect on whether elderly hypertensive patients take their antihypertensive medications. Rather, black patients overall were more likely to be prescribed antihypertensive medications and report taking them as compared to their white counterparts, regardless of provider race (38). King et al. (27) found that black HIV+ patients in race-discordant relationships reported receiving protease inhibitors later in the course of their care than black patients in race-concordant relationships (461 vs. 353 days, respectively; p = 0.002) (27). Finally, Traylor et al. (24) found that race concordance was marginally associated with good adherence to medications (combination of diabetes, cholesterol and hypertension medications) among black patients in Kaiser Permanente’s North Carolina Diabetes Registry compared to white, Asian and Hispanic patients (24). Taken together, these studies suggest that racial composition of the relationship may play a role in medication adherence for black patients. However, factors that could potentially explain the associations in these studies were largely unexplored.
A major strength of this study was the inclusion of a measure of patient-provider communication to elucidate how racial composition of the relationship influences patient outcomes. By testing the moderating effect of racial composition of the relationship on the communication-adherence association, this study was able to identify circumstances under which race-discordant patient-provider relationships can either enhance or hinder patients’ medication adherence. Our findings indicate that black patients’ level of adherence was a function of the perceived quality of communication with their white providers. Specifically, the effect of being in a race-discordant relationship had little impact on patients’ medication adherence when communication was rated as collaborative. In fact, levels of adherence were comparable to being in a race-concordant relationship. On the contrary, the effect of race discordance on medication adherence was substantially heightened when the provider’s communication was rated as non-collaborative. While the factors driving patients’ divergent perceptions about their white providers’ communication skills and the provider characteristics that may contribute to these differences remain unclear, these findings offer important implications for patients and providers who are in race-discordant relationships.
Effective interpersonal communication is a dynamic and ongoing process that requires both patients and providers to find common ground through cooperation, coordination, and understanding of one another’s perspectives.(42) An essential component of this process is the provider’s ability to interact with the patient in a caring and sensitive manner in order to engender trust in the medical relationship. (43) The primary way to build trust and understanding in a relationship is through consistent, collaborative communication.(44) Providers who foster collaborative communication in the medical relationship by actively listening to and eliciting patients’ concerns and expectations for treatment, as well as providing clear and thorough explanations have patients who report better medication adherence.(43, 45, 46) However, if a patient feels they are not communicating with their provider or are not being properly cared for they are less likely to trust the provider(47) and as a result, more likely to discontinue their medication use (48, 49).
Studies have shown that the majority of patients, irrespective of their racial/ethnic backgrounds, prefer providers who exhibit the fundamental communication skills of collaboration, patient-centeredness, empathetic understanding, and active listening.(43, 50, 51) More importantly, these core skills are viewed as the basis of human respect (52), which is considered by many patients to be central to providing culturally competent care.(51) Thus, effective cross-cultural communication is likely to be achieved when white providers are able to fully attend to the minority patient’s needs and incorporates their unique experiences, beliefs, and preferences into the interaction.(53) The ability of the patient and physician to accomplish this has the potential to decrease the degree of ambiguity and conflicting messages that disrupt communication in race-discordant relationships.
While it may seem surprising that patient ratings of provider communication were unrelated to medication adherence in race-concordant relationships, previous studies have also failed to find a clear relationship between race concordance and quality of the patient-provider relationship. In an analysis of 252 audio-taped medical interactions in 16 urban primary care practices, Cooper et al. (20) found that the quality of communication did not explain the higher ratings of positive affect, patient satisfaction, and participatory decision-making documented in race-concordant relationships. Using data from the Commonwealth Fund’s Health Care Quality Survey, Saha et al. (16) reported that race concordance was not associated with black respondent’s satisfaction or use of healthcare services. Moreover, in this survey, only white respondents overtly preferred to be in a race-concordant relationship as compared to the black, Hispanic, and Asian respondents (16).
Our findings, and those of other investigators, raise the question of whether focusing on race as a self-identified characteristic is the correct approach to understanding the role that race concordance (or discordance) plays in explaining differential health outcomes between black and white patients. Rather, the role of race concordance is confounded by a combination of patient and provider characteristics and cultural norms, which include racial/ethnic identity, socioeconomic status, experiences with discrimination, attitudes, beliefs, and behaviors surrounding preferred approaches to care (54–56). For example, the white providers in our study may not be representative of those in typical managed-care organizations and private practices. Providers who work with underserved patients typically prefer to take a biopsychosocial approach to patient care in their medical practice, and are particularly motivated by issues of social justice and equity in healthcare.(57, 58) Moreover, these providers report a feeling of genuine fondness for their patients and continually strive to improve their interpersonal relationship during interactions.(57) As a result, these providers may be more culturally sensitive to the needs of minority patients and exhibit more collaborative communication, which has the potential to significantly affect adherence behaviors by engendering higher levels of patient trust and satisfaction (57). In support of this premise, recent evidence suggests that race concordance plays only a minor role, if patients and providers have a shared understanding of the goals and structure of the medical visit, ultimately leading to higher levels of patient satisfaction, trust, and intentions to adhere to treatment recommendations (56). In all, these findings suggests that, when examining the role of racial composition of the patient-provider relationship on patient outcomes, future studies should treat race as a heterogeneous as well as subjective variable, recognizing that greater variation can occur within minority populations than across groups (59).
Several limitations of this study should be noted. First, the cross-sectional design precludes any causal inference between ratings of communication and medication adherence. Second, this was an observational study thus; we did not randomize patients to race-concordant vs. discordant providers. Furthermore, we did not assess whether patients preferentially chose their provider. Previous studies have shown that the ability to choose one’s provider in terms of race explains a significant portion of variance between race concordance and satisfaction with healthcare (60), use of preventive services (17), and rating provider care as excellent (61). It is hypothesized that if minority patients have the freedom to select their provider and further, tend to choose a provider of their own race then the results of this study might simply reflect the patient satisfaction from having found a physician they prefer rather than the racial composition of the relationship (62). Although a question assessing choice of provider was not included in this study, the characteristics of the patient population impede upon fulfilling such preferences. All patients participating in this study received care at community health center sites, which are often characterized by high turnover rates and an inadequate number of providers for the community’s healthcare needs.(63) Moreover, as opposed to previous race concordance studies, over one-third of this patient population has Medicaid, which confines patients to a select and declining number of providers who accept their health insurance.(26) While the majority of patients participating in the current study were on Medicaid and earned less than $20,000 per year, the findings of this study may not be generalizable to patients that live in extreme poverty (e.g., had less than $10,000 annual income). Future studies should utilize targeted strategies to reach this high-risk group as they are not only at greater risk for non-adherence to medications but also least likely to engage in a collaborative relationship with a single provider as a consequence of episodic and discontinuous care.(9, 64)
Third, this study was embedded within a larger trial that was limited to African American/black patients thus, the impact of racial composition and communication on medication adherence could not be compared to white patient-provider dyads. The current study was also limited to black and white providers thus; we did not systematically collect data on providers of other racial/ethnic categories. Future research is needed to determine whether the relationship between quality of communication and medication adherence identified in this study also applies to black patients in race-discordant relationships with providers of other racial/ethnic groups.
Fourth, medication adherence was assessed with a self-report measure, which lacks a time frame for patients to refer to when responding to each of the questions. This may have led to an overestimation of adherence levels due to patient recall bias. However, our data show a non-adherence rate of 59%, which is similar to the estimated 50 to 70% non-adherence rates in the literature (24). Moreover, the Morisky scale was found to have a sensitivity of 72% with a specificity of 74% for adherence to at least 80% of prescribed antihypertensive medications(33) and was associated with better blood pressure control in hypertensive patients.(33, 65) Future studies would benefit from also utilizing a more objective measure of adherence to assess the relationship between patient-provider communication and medication adherence. Finally, provider communication was assessed as patients’ self-reported perception of the interaction; thus, scores may reflect characteristics specific to the patient (i.e., personality traits), rather than the actual dialogue. Despite this limitation, the importance of understanding the patient’s perspective of the patient-provider relationship cannot be understated.
In conclusion, we found significant effect modification between a patient’s ratings of provider communication and medication adherence among black hypertensive patients in race-discordant relationships followed in urban community-based clinics. Medication adherence was not associated with quality of provider communication in race-concordant relationships. These findings reinforce the clinical importance of improving collaborative cross-cultural communication among providers. With increasing evidence that communication skills are amenable to change and these changes endure (66, 67), medical schools should continually strive to systematically incorporate communication skills training during the course of medical school and residency. Training in cultural humility should also be included in the curricula to assist medical students in developing the skills needed to effectively communicate with diverse patient populations. As opposed to traditional models of multicultural medical education, cultural humility views cultural competency as a lifelong commitment to continuous and active engagement in self-reflection and self-critique.(53) Providers are taught the importance of remaining humble and bringing one’s genuine self into the relationship in order to be mindful of the unique biases, experiences, and values they bring into the interaction. In line with this study’s findings, students should also be taught the role that patient-provider relationships that are characterized by mutual respect, collaboration, and understanding may play in enabling providers to bridge sociocultural gaps between patient and provider, regardless of the racial composition of the relationship. More importantly, healthcare providers-in-training need to understand that such relationships can lead to greater patient engagement in treatment decisions, improvements in patient satisfaction, and better health outcomes. Finally, future research should address how cultural and other sociodemographic factors influence interpersonal processes within the patient-provider relationship. Such data will inform the development of tailored interventions, directed at both the patient and provider, to improve the quality of patient-provider communication in minority patients with chronic diseases.
Acknowledgments
We gratefully acknowledge Johnathan N. Tobin PhD, Marleny Diaz-Gloster MPH, Andrea Cassells MPH and Chamanara Khalida MD (Clinical Directors Network) for all of their help with project and data management.
Funding/Support: This study was supported by F31 HL081926-01, K23 HL 098564-01 and R01 HL 078566, and from the National Heart, Lung, and Blood Institute.
Footnotes
Conflict of Interest Statement: The authors have no conflict of interest to disclose.
References
- 1.Beach MC, Duggan PS, Moore RD. Is patients’ preferred involvement in health decisions related to outcomes for patients with HIV? J Gen Intern Med. 2007;22:1119–24. doi: 10.1007/s11606-007-0241-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beach MC, Keruly J, Moore RD. Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? J Gen Intern Med. 2006;21:661–5. doi: 10.1111/j.1525-1497.2006.00399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bultman DC, Svarstad BL. Effects of physician communication style on client medication beliefs and adherence with antidepressant treatment. Patient Educ Couns. 2000;40:173–85. doi: 10.1016/s0738-3991(99)00083-x. [DOI] [PubMed] [Google Scholar]
- 4.Fuertes JN, Mislowack A, Bennett J, Paul L, Gilbert TC, Fontan G, et al. The physician-patient working alliance. Patient Educ Couns. 2007;66:29–36. doi: 10.1016/j.pec.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17:243–52. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007;42:1443–63. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–27. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 8.Kjellgren KI, Svensson S, Ahlner J, Saljo R. Antihypertensive medication in clinical encounters. Int J Cardiol. 1998;64:161–9. doi: 10.1016/s0167-5273(98)00038-2. [DOI] [PubMed] [Google Scholar]
- 9.Piette JD, Schillinger D, Potter MB, Heisler M. Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. J Gen Intern Med. 2003;18:624–33. doi: 10.1046/j.1525-1497.2003.31968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schneider J, Kaplan SH, Greenfield S, Li W, Wilson IB. Better physician-patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. J Gen Intern Med. 2004;19:1096–103. doi: 10.1111/j.1525-1497.2004.30418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- 12.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 13.Schoenthaler A, Chaplin WF, Allegrante JP, Fernandez S, Diaz-Gloster M, Tobin JN, et al. Provider communication effects medication adherence in hypertensive African Americans. Patient Educ Couns. 2009;75:185–91. doi: 10.1016/j.pec.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–9. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 15.Beach MC, Sugarman J, Johnson RL, Arbelaez JJ, Duggan PS, Cooper LA. Do patients treated with dignity report higher satisfaction, adherence, and receipt of preventive care? Ann Fam Med. 2005;3:331–8. doi: 10.1370/afm.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saha S, Arbelaez JJ, Cooper LA. Patient-physician relationships and racial disparities in the quality of health care. Am J Public Health. 2003;93:1713–9. doi: 10.2105/ajph.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159:997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- 18.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94:2084–90. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roter DL, Stewart M, Putnam SM, Lipkin M, Jr, Stiles W, Inui TS. Communication patterns of primary care physicians. JAMA. 1997;277:350–6. [PubMed] [Google Scholar]
- 20.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139:907–15. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 21.LaVeist TA, Carroll T. Race of physician and satisfaction with care among African–American patients. J Natl Med Assoc. 2002;94:937–43. [PMC free article] [PubMed] [Google Scholar]
- 22.LaVeist TA, Nuru-Jeter A, Jones KE. The association of doctor-patient race concordance with health services utilization. J Public Health Policy. 2003;24:312–23. [PubMed] [Google Scholar]
- 23.Meghani SH, Brooks JM, Gipson-Jones T, Waite R, Whitfield-Harris L, Deatrick JA. Patient-provider race-concordance: does it matter in improving minority patients’ health outcomes? Ethn Health. 2009;14:107–30. doi: 10.1080/13557850802227031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2011;25:1172–7. doi: 10.1007/s11606-010-1424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Traylor AH, Subramanian U, Uratsu CS, Mangione CM, Selby JV, Schmittdiel JA. Patient race/ethnicity and patient-physician race/ethnicity concordance in the management of cardiovascular disease risk factors for patients with diabetes. Diabetes Care. 2011;33:520–5. doi: 10.2337/dc09-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Howard DL, Konrad TL, Stevens C, Porter CQ. Physician-patient racial matching, effectiveness of care, use of services, and patient satisfaction. Research on Aging. 2001;23:83–108. [Google Scholar]
- 27.King WD, Wong MD, Shapiro MF, Landon BE, Cunningham WE. Does racial concordance between HIV-positive patients and their physicians affect the time to receipt of protease inhibitors? J Gen Intern Med. 2004;19:1146–53. doi: 10.1111/j.1525-1497.2004.30443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Konrad TR, Howard DL, Edwards LJ, Ivanova A, Carey TS. Physician-patient racial concordance, continuity of care, and patterns of care for hypertension. Am J Public Health. 2005;95:2186–90. doi: 10.2105/AJPH.2004.046177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ogedegbe G, Schoenthaler A. A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens (Greenwich) 2006;8:174–80. doi: 10.1111/j.1524-6175.2006.04872.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002;347:1585–92. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 31.Wright JM, Mattu GS, Perry TL, Jr, Gelferc ME, Strange KD, Zorn A, et al. Validation of a new algorithm for the BPM-100 electronic oscillometric office blood pressure monitor. Blood Press Monit. 2001;6:161–5. doi: 10.1097/00126097-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Ogedegbe G, Tobin JN, Fernandez S, Gerin W, Diaz-Gloster M, Cassells A, et al. Counseling African Americans to Control Hypertension (CAATCH) trial: a multi-level intervention to improve blood pressure control in hypertensive blacks. Circ Cardiovasc Qual Outcomes. 2009;2:249–56. doi: 10.1161/CIRCOUTCOMES.109.849976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 35.Ogedegbe G, Chaplin W, Schoenthaler A, Statman D, Berger D, Richardson T, et al. A Practice-Based Trial of Motivational Interviewing and Adherence in Hypertensive African Americans. Am J Hypertens. 2008;21:1137–1143. doi: 10.1038/ajh.2008.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Like RC. Culturally competent family medicine: transforming clinical practice and ourselves. Am Fam Physician. 2005;72:2189–90. [PubMed] [Google Scholar]
- 37.Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, et al. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–70. doi: 10.1161/01.cir.88.5.2460. [DOI] [PubMed] [Google Scholar]
- 38.Bauer DJ, Curran PJ. Probing interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivariate Behavioral Research. 2005;40:373–400. doi: 10.1207/s15327906mbr4003_5. [DOI] [PubMed] [Google Scholar]
- 39.SPSS. 18. Chicago: SPSS, Inc; 2010. [Google Scholar]
- 40.Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002;15:25–38. [PubMed] [Google Scholar]
- 41.Howard DL, Konrad TL, Stevens C, Porter CQ. Physician-patient racial matching, effectiveness of care, use of services, and patient satisfaction. Research on Aging. 2001;23:83–108. [Google Scholar]
- 42.Epstein RM, Street RL., Jr . Promoting Healing and Reducing Suffering. Bethesda, MD: National Cancer Institute; 2007. Patient-centered Communication in Cancer Care. Report No.: NIH Publication No. 07–6225. [Google Scholar]
- 43.DiMatteo MR. Patient adherence to pharmacotherapy: the importance of effective communication. Formulary. 1995;30:596–8. 601–2, 605. [PubMed] [Google Scholar]
- 44.Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians: effects of choice, continuity, and payment method. J Gen Intern Med. 1998;13:681–6. doi: 10.1046/j.1525-1497.1998.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harmon G, Lefante J, Krousel-Wood M. Overcoming barriers: the role of providers in improving patient adherence to antihypertensive medications. Current Opinion in Cardiology. 2006;21:310–5. doi: 10.1097/01.hco.0000231400.10104.e2. [DOI] [PubMed] [Google Scholar]
- 46.Betancourt JR, Carrillo JE, Green AR. Hypertension in multicultural and minority populations: linking communication to compliance. Current Hypertension Reports. 1999;1:482–8. doi: 10.1007/BF03215777. [DOI] [PubMed] [Google Scholar]
- 47.Fiscella K, Meldrum S, Franks P, Shields CG, Duberstein P, McDaniel SH, et al. Patient trust: is it related to patient-centered behavior of primary care physicians? Med Care. 2004;42:1049–55. doi: 10.1097/00005650-200411000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Fiscella K, Holt K. Racial disparity in hypertension control: tallying the death toll. Ann Fam Med. 2008;6:497–502. doi: 10.1370/afm.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, Warnecke RB. Understanding African Americans’ views of the trustworthiness of physicians. J Gen Intern Med. 2006;21:642–7. doi: 10.1111/j.1525-1497.2006.00485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lipkin M., Jr Sisyphus or Pegasus? The physician interviewer in the era of corporatization of care. Annals of Internal Medicine. 1996;124:511–3. doi: 10.7326/0003-4819-124-5-199603010-00010. [DOI] [PubMed] [Google Scholar]
- 51.Teal CR, Street RL. Critical elements of culturally competent communication in the medical encounter: a review and model. Social Science & Medicine. 2009;68:533–43. doi: 10.1016/j.socscimed.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 52.Dickert NW, Kass NE. Understanding respect: learning from patients. Journal of medical ethics. 2009;35:419–23. doi: 10.1136/jme.2008.027235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tervalon M, Murray-Garcia J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. Journal of health care for the poor and underserved. 1998;9:117–25. doi: 10.1353/hpu.2010.0233. [DOI] [PubMed] [Google Scholar]
- 54.Cooper LA, Beach MC, Johnson RL, Inui TS. Delving below the surface. Understanding how race and ethnicity influence relationships in health care. J Gen Intern Med. 2006;21 (Suppl 1):S21–7. doi: 10.1111/j.1525-1497.2006.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Saha S. The relevance of cultural distance between patients and physicians to racial disparities in health care. J Gen Intern Med. 2006;21:203–5. doi: 10.1111/j.1525-1497.2006.0345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Street RL, Jr, O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient- physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6:198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li LB, Williams SD, Scammon DL. Practicing with the urban underserved. A qualitative analysis of motivations, incentives, and disincentives. Arch Fam Med. 1995;4:124–33. doi: 10.1001/archfami.4.2.124. discussion 134. [DOI] [PubMed] [Google Scholar]
- 58.Odom Walker K, Ryan G, Ramey R, Nunez FL, Beltran R, Splawn RG, et al. Recruiting and retaining primary care physicians in urban underserved communities: the importance of having a mission to serve. American Journal of Public Health. 2010;100:2168–75. doi: 10.2105/AJPH.2009.181669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hayward M, Miles T, Crimmins E, Yang Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. American Sociological Review. 2000;65:910–930. [Google Scholar]
- 60.Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43:296–306. [PubMed] [Google Scholar]
- 61.Chen FM, Fryer GE, Jr, Phillips RL, Jr, Wilson E, Pathman DE. Patients’ beliefs about racism, preferences for physician race, and satisfaction with care. Ann Fam Med. 2005;3:138–43. doi: 10.1370/afm.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schnittker J, Liang K. The promise and limits of racial/ethnic concordance in physician-patient interaction. J Health Polit Policy Law. 2006;31:811–38. doi: 10.1215/03616878-2006-004. [DOI] [PubMed] [Google Scholar]
- 63.Safran DG, Kosinski M, Tarlov AR, Rogers WH, Taira DH, Lieberman N, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36:728–39. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 64.Gregg AC, DeHaven M, Meires J, Kane A, Gullison G. Perspectives on Adherence to Recommended Health Behavior among Low-Income Patients. Health Promotion Practice. 2001;2:162–271. [Google Scholar]
- 65.Bosworth HB, Dudley T, Olsen MK, Voils CI, Powers B, Goldstein MK, et al. Racial differences in blood pressure control: potential explanatory factors. Am J Med. 2006;119:70 e9–15. doi: 10.1016/j.amjmed.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 66.Lipkin M., Jr Sisyphus or Pegasus? The physician interviewer in the era of corporatization of care. Annals of Internal Medicine. 1996;124:511–3. doi: 10.7326/0003-4819-124-5-199603010-00010. [DOI] [PubMed] [Google Scholar]
- 67.Fallowfield L, Jenkins V, Farewell V, Saul J, Duffy A, Eves R. Efficacy of a Cancer Research UK communication skills training model for oncologists: a randomised controlled trial. Lancet. 2002;359:650–6. doi: 10.1016/S0140-6736(02)07810-8. [DOI] [PubMed] [Google Scholar]


