Abstract
Objectives
Animal-assisted therapy using dogs trained to be calm and provide comfort to strangers has been used as a complementary therapy for a range of medical conditions. This study was designed to evaluate the effects of brief therapy dog visits for fibromyalgia patients attending a tertiary outpatient pain management facility compared with time spent in a waiting room.
Design
Open-label with waiting room control
Setting
Tertiary care, university-based, outpatient pain management clinic
Subjects
A convenience sample of fibromyalgia patients was obtained through advertisements posted in the clinic.
Interventions
Participants were able to spend clinic waiting time with a certified therapy dog instead of waiting in the outpatient waiting area. When the therapy dog was not available, individuals remained in the waiting area.
Outcome measures
Self-reported pain, fatigue, and emotional distress were recorded using 11-point numeric rating scales before and after the therapy dog visit or waiting room time.
Results
Data were evaluated from 106 therapy dog visits and 49 waiting room controls, with no significant between-group demographic differences in participants. Average intervention duration was 12 minutes for the therapy dog visit and 17 minutes for the waiting room control. Significant improvements were reported for pain, mood, and other measures of distress among patients after the therapy dog visit but not the waiting room control. Clinically meaningful pain relief (≥2 points pain severity reduction) occurred in 34% after the therapy dog visit and 4% in the waiting room control. Outcome was not affected by the presence of comorbid anxiety or depression.
Conclusions
Brief therapy dog visits may provide a valuable complementary therapy for fibromyalgia outpatients.
Keywords: clinically meaningful pain relief, complementary therapy, mood, satisfaction, therapy dog, waiting room
Introduction
Animal-assisted therapy is a complementary intervention using animals, usually dogs trained to be obedient, calm, and comforting, for therapeutic benefit across a broad range of medical conditions [1–3]. Published data are available investigating the impact of therapeutic animal visits for mixed medical and surgical patients and patients with pervasive developmental disorders, cerebral palsy, speech disorders, cardiovascular disease, depression, schizophrenia, Alzheimer’s disease, cancer, and spinal cord injuries, as well as people living in rehabilitation facilities and nursing homes [2–3]. Therapy dog visits are provided through volunteer services, with no additional cost, staff time, or equipment required for caregivers implementing this therapeutic service. A literature review provided Class IIa-IIb evidence (shown to be acceptable and useful) for recommending animal-assisted therapy to optimize healing environments [4]. Animal-assisted therapy with dogs has been documented to produce objective health changes, with reductions in measures of cardiovascular stress [5.6], improvements in neurophysiological stress markers (e.g., cortisol) [7.8], increases in endorphins [7], and enhancement of immune factors [9]. Interestingly, pre-study attitude toward pets measured using the Pet Attitude Scale has been shown to be independent of physiological benefit [9]. Despite the potential feasibility of animal-assisted therapy as a complementary intervention, data on effectiveness are limited by the use of anecdotal reports, small sample sizes, mixed study populations, and uncontrolled studies, which have limited the ability to provide strong supportive evidence [10]. Additional studies are needed to better understand the impact of animal-assisted interventions on specific patient populations [11].
A previous study demonstrated significant improvement for chronic pain patients attending a tertiary pain management clinic who received brief therapy dog visits [12]. In that study, pain and other measures of distress were compared between a mixed group of chronic pain patients opting to participate in a brief therapy dog visit during clinic waiting time (N=295) compared with patients surveyed after spending similar time in the clinic waiting room (N=96). Pain, fatigue, stress, and mood were significantly improved after the therapy dog visit but not the waiting room control. The current study was designed to expand on this earlier study by focusing on a specific chronic pain patient population, selecting fibromyalgia because of their typically high acceptance of complementary therapies. Fibromyalgia is an often disabling widespread chronic pain condition affecting about 2–3% of adults in the Americas and Europe, with no currently available curative treatment [13–17]. Benefits from approved drug therapies are typically modest [18–20]. Symptoms are generally managed with a combination of non-drug and drug therapies, with complementary and alternative therapies used by a majority of fibromyalgia patients, most commonly exercise, spiritual healing, massage, chiropractic treatment, and supplements [21]. A recent systematic review of controlled trials evaluating benefits from complementary and alternative treatments for fibromyalgia concluded that more research is needed to provide convincing evidence for the efficacy of many of these therapies [22]. The strongest evidence provided from controlled trials supports hydrotherapy and mind-body interventions [22]. Benefits have also been shown for fibromyalgia with acupuncture, homeopathy, massage, Tai chi, and yoga [23–25]. Recommendations from clinicians to patients for selecting among complementary and alternative treatments may be limited due to lack of knowledge by referring healthcare providers, perceived legal barriers, and cost and availability constraints [26–28]. Although cost issues would not limit access to animal-assisted interventions, limited data in a fibromyalgia population is a significant barrier to utilization of this therapy.
The current open-label study replicates the design used in the previously published animal-assisted study, applying treatment to a population of treatment-seeking fibromyalgia patients at a tertiary care chronic pain clinic. This study was designed as a open-label study to determine potential benefit from brief animal-assisted therapy delivered to a fibromyalgia population.
Methods
This open-label study was conducted in an outpatient, tertiary care, interdisciplinary pain management clinic from June 1, 2011 to December 2, 2011. The study protocol was approved by a local Institutional Review Board as an exempt study not requiring informed consent from participants. The study was conducted as a survey study, which minimized disruption to clinic flow. Randomly assigning interested candidates to therapy dog visits vs the waiting room control would have required a consenting process that would have exceeded the time spent with the typical therapy dog visit. In addition, there was a concern that the consenting process itself might provide information about anticipated potential therapy dog benefits that might have encouraged participants to report more favorable responses than they experienced.
Subjects
Study participants were recruited through advertisements placed in patient waiting areas and on the room occupied by the therapy dog, which stated: “Therapy Dog Research Project. This research asks how you might spend time before your visit waiting in a room with a therapy dog. Please complete the front page of the research survey before coming in to see the dog.” The therapy dog intervention was available for about 2 hours on one or two days each week, while the waiting room survey was available when the therapy dog was not present in the clinic. Therapy dog visit times were selected to coincide with times when fibromyalgia patients were likely to be scheduled to be evaluated by the clinicians and times that were convenient for the dog handler. Some sessions were offered during morning hours and others during afternoon hour, depending on clinic’s patient scheduling.
Adults ≥18 years old who had been diagnosed with fibromyalgia were eligible to participate. The fibromyalgia diagnosis was confirmed by each patient’s treating clinician, based on American College of Rheumatology criteria including a tender point examination [29].
The current study population includes those patients with fibromyalgia from the previously published analysis (n=32 receiving therapy dog visits and n=15 waiting room controls) [12] plus additional patients with fibromyalgia recruited during the five months after the initial study population was closed. Most participants in this study were not included in the earlier sample.
Survey
Participants completed a screening survey immediately prior to the intervention. The one-page survey asked for demographic information and included the validated 4-question Patient Health Questionnaire (PHQ-4), a standardized, ultra-brief mood disorder screening tool that provides three measures: PHQ-4, PHQ-2 depression screener, and Generalized Anxiety Disorder (GAD)-2 anxiety screener (possible range 0–6), using recommended cut-offs of ≥3 with PHQ-2 and GAD-2 scores for potential depression and anxiety, respectively [30.31]. Screening was performed for mood disorders because they are the most common psychiatric conditions identified in fibromyalgia patients and they have been shown to be linked with worsen pain severity [32]. Subjects also rated current symptom severity on an 11-point scale for 10 factors: pain, fatigue, stress level, aggravation, anxiety or worry, sadness or depression, irritability or frustration, calmness, pleasantness, and cheerfulness. Following completion of the form, participants noted the time on their surveys and began either the therapy dog or waiting room control intervention.
Participants were permitted to complete only one survey on any given day. Additional surveys could be completed on other days that occurred at least 1 week after the previously completed survey, with a notation made on the survey when previous participation in that intervention had occurred.
Therapy dog intervention
A certified therapy dog (5-year-old, 40-pound, male soft-coated wheaten terrier) and his handler were available to meet in a designated room. The dog and handler were an experienced team who were evaluated and certified annually through Therapy Dogs International. This therapy dog-handler team had made regular therapy visits for 4 years, completing over 175 visits at the time of this study, with the dog having been awarded the American Kennel Club Therapy Dog title. Similar to the previously published study [12], a single therapy dog was used in this study for feasibility and to avoid introducing an additional confounding variable that might have required additional analyses, as dog size has been shown to affect patients’ perceptions of therapy dog visits [33].
After completing their survey, therapy dog participants were provided with a chair in a designated room and introduced to the dog, which they were invited to pet. The dog was trained to stand or sit next to the chair for the duration of the participant’s visit and accept handling. More than one participant could interact with the dog at the same time. Conversations between participants and the dog’s handler were directed to focus on the dog (breed, age, training, etc.) and pet-related topics. Discussion of health issues with the handler was discouraged. Participants were informed that they could spend as much time with the dog as they preferred or until the patient was notified that his/her appointment was ready to begin. A variable time for the therapy dog visit was used for this study to accommodate clinic flow so that patients would not be detained from appointments once their clinician was available. Also, this permitted participants an opportunity to choose how much time they preferred to spend, as would be consistent with typical therapy dog visits.
After completing the therapy dog visit, participants again rated their current symptoms on an 11-point scale. Participants were also asked to rate their satisfaction with the therapy dog interaction on a 5-point scale from strongly disagree to strongly agree by reacting to statements that they enjoyed the visit, that the dog made them happy, and that they would like to visit the dog again. Duration between completing the pre- and post-intervention surveys was noted.
Waiting room control
After completing the one-page survey, waiting room control participants were asked to wait for 15 minutes with no particular directions about what to do while waiting. Magazines and a television were available for patients to use during this time. After about 15 minutes, the participants completed a second survey rating current symptoms on an 11-point scale.
Data analysis
Demographics, mood assessments, and satisfaction questions were evaluated using descriptive statistics. Changes in mean pre- and post-intervention symptom scores were calculated and differences evaluated with paired t-tests, with significance set at <0.05. The percentage of participants achieving clinically meaningful pain relief (defined as a reduction on the pain severity scale of ≥2 points [34–36]) and those scoring ≥8 for calm, pleasant, or cheerful pre- and post-intervention were noted. Subanalyses were performed to determine if baseline potential depression or anxiety identified through screeners or visit duration influenced outcome, with paired t-tests used to evaluate changes in numeric rating scale measures from pre- to post-intervention.
Results
Subjects
A total of 133 individuals participated in this study, with 84 meeting with the therapy dog and 49 completing the waiting room survey (Table 1). There were no significant between-groups differences in demographics. Several individuals met with the therapy dog for 2 or 3 visits, for a total of 106 therapy dog visits. No subject completed more than one visit during the same week. Mean visit duration (range) with the therapy dog was 12.1 ± 5.7 minutes (2–32 minutes). No subjects completed the waiting room survey more than once. The mean time for the waiting room survey between pre- and post-survey completion was 17.1 ± 6.2 minutes (5–35 minutes).
Table 1.
Participant characteristics
| Characteristic | Therapy dog visitors N=84 |
Waiting room control N=49 |
|---|---|---|
|
| ||
| Age, mean years (SD) | 48.0 (11.5) | 47.8 (14.4) |
|
| ||
| Gender, n (%) | ||
| Male | 2 (2.4) | 2 (4.1) |
| Female | 82 (97.6) | 47 (95.9) |
|
| ||
| PHQ4, mean (SD) | 5.96 (3.52) | 6.86 (3.63) |
|
| ||
| PHQ2 | ||
| Mean (SD) | 2.79 (2.00) | 3.37 (1.92) |
| Positive depression screening, n (%)* | 40 (47.6) | 29 (59.2) |
|
| ||
| GAD2 | ||
| Mean (SD) | 3.18 (1.88) | 3.49 (2.07) |
| Positive anxiety screening, n (%)* | 48 (57.1) | 30 (61.2) |
Patients scoring ≥3
A number of subjects returned to the therapy dog room after completing their clinical appointments to spend additional time with the therapy dog. Subjects were permitted to spend as much time with the dog as they preferred, however, no additional surveys were completed or data recorded for visits when >1 visit occurred on the same day.
Therapy dog visit vs. waiting room
Pre- and post-intervention data showed significant improvements in all numeric scales for therapy dog visits (Table 2). Changes in mean scores for patients completing the waiting room survey were generally not significant. Significant worsening was noted among waiting room participants for cheerfulness, with a trend toward significant worsening for fatigue. Clinically meaningful pain relief was achieved after 36 therapy dog visits (34.0% of visits) and after 2 waiting room control surveys (4.1%).
Table 2.
Pre- and post-intervention values (SE)
| Symptom | Therapy dog visits | Waiting room controls | ||||
|---|---|---|---|---|---|---|
| Pre | Post | P-value* | Pre | Post | P-value* | |
| Pain | 7.14 (0.21) | 5.95 (0.23) | <0.001 | 7.02 (0.33) | 7.29 (0.30) | 0.074 |
| Fatigue | 6.75 (0.26) | 5.45 (0.24) | <0.001 | 6.53 (0.39) | 7.00 (0.36) | 0.059 |
| Stress | 6.14 (0.27) | 3.80 (0.25) | <0.001 | 5.69 (0.36) | 5.71 (0.37) | 0.931 |
| Aggravation | 4.96 (0.31) | 2.91 (0.26) | <0.001 | 4.39 (0.44) | 4.71 (0.45) | 0.146 |
| Anxiety | 5.86 (0.28) | 3.35 (0.27) | <0.001 | 5.20 (0.41) | 5.10 (0.42) | 0.682 |
| Sadness | 4.91 (0.31) | 2.96 (0.28) | <0.001 | 4.59 (0.42) | 4.51 (0.41) | 0.684 |
| Irritability | 5.17 (0.29) | 2.69 (0.26) | <0.001 | 4.80 (0.45) | 4.86 (0.46) | 0.766 |
| Calm | 4.55 (0.29) | 7.19 (0.26) | <0.001 | 4.82 (0.41) | 4.47 (0.43) | 0.299 |
| Pleasant | 5.44 (0.27) | 7.61 (0.24) | <0.001 | 4.94 (0.36) | 4.88 (0.39) | 0.685 |
| Cheerful | 5.03 (0.29) | 7.57 (0.23) | <0.001 | 4.88 (0.37) | 4.55 (0.39) | 0.031 |
Each item was scored from 0 (symptom is absent) to 10 (symptom is extreme).
Significance of pre- to post-intervention change
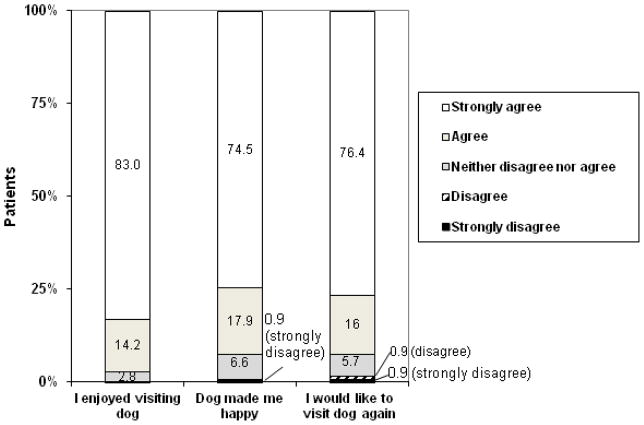
Changes in positive feelings are shown in Figure 1. Self-perceptions of high levels of calmness, pleasantness, and cheerfulness increased after meeting with the therapy dog, without substantial changes when completing the waiting room survey. Pre-intervention percentage reporting high levels of pleasantness was numerically lower among waiting room participants compared with those opting to participate in the therapy dog visit.
Figure 1.
Calm, pleasant, and cheerful feelings (identified when patients scored item ≥8). Significant pre- to post-intervention changes: ***P<0.001
Subgroup analyses
Twenty-two therapy dog visits were made by individuals visiting the dog on more than one occasion. Analyzing data from only the first visit from each participant did not affect any outcome. Furthermore, among the 84 patients participating in their first therapy dog visit, 30 experienced clinically meaningful pain relief (35.7%). Among the 22 repeat visits, clinically meaningful pain relief was achieved after 6 visits (27.3%).
Among individuals visiting the therapy dog, significant changes occurred in all numeric ratings for individuals scoring positive or negative on the depression screener, with no significant changes among waiting room controls for either those screening positive or negative for depressed symptoms. A clinically meaningful reduction in pain occurred for 32.7% of individuals screening positive for depressed symptoms and 35.2% of non-depressed individuals meeting with the therapy dog compared with 3.4% of positive depressed screener and 5.0% of non-depressed individuals completing the waiting room survey.
Changes in all numeric rating scales were likewise significant for individuals meeting with the therapy dog who screened positive or negative for anxiety symptoms. There only significant changes in patients completing the waiting room survey were significant worsening with fatigue (from 6.00 [standard error (SE) 0.56] to 6.42 [0.53], P=0.042) in patients screening negative for anxiety and significant worsening in cheerfulness (from 4.27 [0.50] to 3.80 [0.52], P=0.017) in patients screening positive for anxiety. Clinically meaningful pain relief occurred in 36.7% of positive anxious screener patients and 30.4% of non-anxious patients meeting with the therapy dog and 3.3% of positive anxious screener and 5.3% of non-anxious patients in the waiting room control.
Most therapy dog visits lasted ≥10 minutes (67.9% of visits), with 32.1% lasting <10 minutes. Pre- to post-intervention changes in all numeric variables were significant for both shorter and longer duration visits. Most waiting room controls lasted ≥10 minutes (93.9%). Clinically meaningful pain relief occurred for 23.5% of patients visiting the therapy dog for <10 minutes and 38.9% visiting ≥10 minutes. None of the 3 patients spending <10 minutes completing the waiting room survey reported relief; 4.3% spending ≥10 minutes reported meaningful pain relief with the control.
A number of participants meeting with the therapy dog visit spontaneously verbalized at the start of the visit that they disliked or were intimidated by some dogs or would prefer to visit with a different type of animal, such as a cat or rabbit. These participants generally stated they were opting to participate in the visit in order to try something different, because another animal was not an option, or to help improve comfort levels around dogs. In general, participant responses did not appear to be different for these individuals verbalizing an initially negative perception of dogs compared with the group as a whole. Information about pet attitude was not requested or recorded as part of this project and, therefore, could not be analyzed.
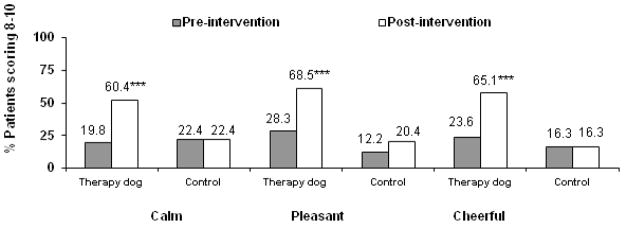
Satisfaction
The vast majority of patients meeting with the therapy dog had a positive impression of the visit and endorsed a desire to have future therapy dog visits (Figure 2). Patients reporting negative perceptions of the visits generally verbalized that spending time with the therapy dog made them miss a pet that they had recently lost or a concern that their own pet would be upset with them for having spent time with another dog.
Figure 2.
Satisfaction with therapy dog visit
Discussion
This study expands on previously published data evaluating a brief therapy dog intervention in chronic pain patients by focusing on fibromyalgia outpatients. Similar to the response in a mixed group of chronic pain patients [12], fibromyalgia outpatients in the current study experienced significant improvements in pain and distress following a brief therapy dog visit, with no significant improvements noted for patients in the waiting room control condition. Overall, pain severity was significantly reduced after a brief therapy dog visit, with clinically meaningful pain relief reported in 34% of fibromyalgia patients after the dog visit vs 4% in the waiting room control. Effects did not appear to be substantially influenced by coexisting mood disorder symptoms.
Average therapy dog visit duration was 12 minutes, with clinically meaningful pain relief reported by 24% of patients visiting with the dog for <10 minutes and 39% visiting for ≥10 minutes. Because patients were permitted to choose how long they spent with the therapy dog to avoid disruption of clinic flow rather than an assigned visit duration requirement, this study cannot determine if a longer visit was necessary for achieving better pain relief or patients experiencing greater pain reduction were more likely to spend a longer duration of time with the dog. Published studies evaluating benefits of therapy dog visits suggest that 10–15 minutes provide optimal benefits to those visited by the dog [37]. Previous studies have shown significant improvement in pain relief after therapy dog visits lasting for an average of 10 minutes in a study of adult medical and surgical hospitalized patients [38] and in two studies of hospitalized pediatric patients in which therapy dog interactions were scheduled to last for 11–20 minutes [39,40]. A pilot study likewise showed significantly reduced anxiety among adults waiting for an MRI after spending 15 minutes with a therapy dog [41]. Future studies, therefore, may wish to have patients spend at least 10 minutes with the dog or use a standard 10–15 minute intervention time for all fibromyalgia participants.
A subanalysis of first visits only showed significant improvement in all measures among patients during their first visit to help ensure benefits were not a reflection of repeat visits by high responders. Interestingly, clinically meaningful pain relief occurred more frequently among the first visit only population. Conditioning experiments suggest that placebo analgesia is enhanced after experiencing successful pain relief from initial exposure [42]. Because surveys were completed anonymously, comparisons cannot be made to determine if individual patients responded better at their first visit or if repeat visits were made by patients who were more likely to make several visits to the clinic during the assessment period, suggesting that they might have had more recalcitrant symptoms warranting more intensive care than patients with less frequent visits. Patients completing therapy dog visits were not asked if they had previously completed a waiting room survey on a separate visit. Because surveys were anonymous, it was not possible to compare responses if the same patient had completed a survey for each visit type.
Changes among patients in the regular waiting area were generally small and did not achieve statistical significance, with the exception of a small worsening of cheerfulness after time in the waiting room that was statistically significant; this change was numerically small and not necessarily clinically meaningful. While one might postulate that time waiting would increase stress, aggravation, and negative emotional symptoms, the changes that did occur were small. These data suggest that short periods of time (e.g., 17 minutes on average in the waiting room), in and of themselves, were not likely to substantially affect symptoms or distress among fibromyalgia patients.
This study did not investigate potential mechanisms for why benefits might have occurred with therapy dog visits. As noted previously, published data have linked brief therapy dog visits with reductions in stress hormones, such as epinephrine and norepinephrine, as well as increases in endorphin levels [7,8]. Medications that affect neurotransmitters, like norepinephrine, have proven efficacy for reducing fibromyalgia symptoms [43]. Oxytocin also offers anti-stress effects and increases pain threshold [44] and oxytocin levels have been shown to increase following therapy dog visits [45,46]. Furthermore, current mood symptoms have been linked with pain severity in fibromyalgia patients [32], so that pain improvement may have been a secondary consequence of reductions in anxious and depressed symptoms.
This study is limited by a variety of factors, including an open-label, non-randomized design and the use of a convenience sample collected through participant self-selection rather than consecutive patient sampling. For example, individuals choosing to meet with the therapy dog may have been more likely to have a more positive perception of pets and been more likely to benefit from interactions. This study did not query participants about current relationships with or attitudes about pets. In a previously published study, benefits were not linked to pet attitude, suggesting benefits may be independent of previous or current relationships or attitudes toward pets [9]. While administering the Pet Attitude Scale would have been too time-consuming for the current study, this measure or brief questions asking about attitude and current relationships with pets should be included in future studies. Another limitation was the inability to blind participants to intervention type, which may have inadvertently encouraged participants to respond more favorably to questions about the therapy dog visit. Limited availability of the therapy dog in the clinic also restricted the ability of fibromyalgia patients to opt to participate and this may have also resulted in a more restricted sample. Unlike a service dog that has been trained to provide ongoing service throughout the day, therapy dogs are limited in providing visits as engaging repetitively with strangers has been shown to be stressful and tiring for therapy dogs, with negative physiological changes increasing as the number of visits per month and hours per visit increase [47]. Restrictions on visit times resulted in the dog being available for only a limited amount of time such that all fibromyalgia patients who might have been interested in a visit would not have had the opportunity. In order to offer visits to all patients, a substantial number of dog-handler teams would have been needed. In addition, the design of this study did not permit indepth evaluation and classification of pain symptoms and psychological/psychiatric comorbidity. Due to the nature of this study, using symptom self-report, mood disorders were screened for using the validated PHQ-4. The PHQ-4 does not confirm a diagnosis of depression or anxiety, but is a screening tool suggesting when additional detailed evaluations for mood disorders might be indicated. More extensive tools, such as the Mini International Neuropsychiatric Interview, would have provided a more robust description of potential psychiatric comorbidities among study subjects. Furthermore, 11-point severity scales were used for all symptoms because patients are familiar with this type of rating and this scale captures current symptoms rather than changes over times (e.g., the PHQ-4 asks about symptoms over the preceding two weeks). This type of brief assessment, however, cannot compare to more indepth evaluations of emotional distress symptoms that might be uncovered using more extensive questionnaires or patient interviews. Although previously published studies have likewise employed a similar waiting room control as was used in the current study [12,41,48], future studies may wish to compare outcome of the therapy dog visit against other established alternative therapy options. A comparative complementary intervention was not utilized as a control in the current study due to feasibility issues and the inability for most complementary therapies with proven efficacy in fibromyalgia to be delivered within the 10–15 minutes that is typically utilized for a therapy dog visit. In addition, data are not available to determine whether benefits from the therapy dog interaction in the current study persisted. Future studies should incorporate a more rigorous design, such as randomizing participants to a therapy dog intervention vs usual treatment or a comparable treatment control, with outcome measured using non-self report assessments obtained weeks to months post-intervention to determine persistent impact [49]. Although randomized studies should provide more rigorous data, a meta-analysis evaluating outcome from animal-assisted therapy found that comparable outcomes had been reported by nonrandomized and uncontrolled studies compared with well-designed, controlled [50]. These data highlight that, while more rigorous designs are ideal in providing robust data, animal-assisted therapy outcomes from less rigorous designs can also be meaningful. When data from less rigorous studies are available, future studies in that patient population should adopt a more rigorous study design to confirm outcome. Because of the noted baseline differences in distress between patients opting to participate in therapy dog visits and those completing waiting room assessments in the current study, future studies should include methods, such as randomization or stratification based on psychological comorbidity, that might allow comparison of patients with more similar baseline characteristics.
Conclusions
The positive data obtained in this study support that therapy dog visits may provide valuable complementary treatment to fibromyalgia outpatients, with significant reductions in pain and distress. These symptomatic improvements prior to assessment/treatment appointments may help prepare patients for a more successful clinic visit encounter.
Acknowledgments
The project described was supported by the National Institutes of Health through Grant Numbers UL1 RR024153 and UL1TR000005.
Footnotes
Author Conflict of Interest/Disclosure Statement
Dawn A. Marcus, MD: no conflicts to disclose; no competing financial interests exist
Cheryl D. Bernstein, MD: no conflicts to disclose; no competing financial interests exist
Janet M. Constantin, RN, BSN, Esq: no conflicts to disclose; no competing financial interests exist
Frank A. Kunkel, MD: no conflicts to disclose; no competing financial interests exist
Paula Breuer, BS: no conflicts to disclose; no competing financial interests exist
Raymond B. Hanlon, MS: no conflicts to disclose; no competing financial interests exist
References
- 1.Muñoz Lasa G, Ferriero G, Brigatti E, Valero R, Franchignoni F. Animal-assisted interventions in internal and rehabilitation medicine: a review of the recent literature. Panminerva Med. 2011;53:129–36. [PubMed] [Google Scholar]
- 2.Kniseley JS, Barker SB, Barker RT. Research on benefits of canine-assisted therapy for adults in nonmilitary settings. US Army Med Dep J. 2012 Apr-Jun;:30–7. [PubMed] [Google Scholar]
- 3.Marcus DA. Complementary medicine in cancer care: adding a therapy dog to the team. Curr Pain Headache Rep. doi: 10.1007/s11916-012-0264-0. (in press) [DOI] [PubMed] [Google Scholar]
- 4.Halm MA. The healing power of the human-animal connection. Am J Crit Care. 2008;17:373–76. [PubMed] [Google Scholar]
- 5.Allen K, Shykoff BE, Izzo JL. Pet ownership, but not ACE inhibitor therapy, blunts home blood pressure responses to mental stress. Hypertension. 2001;38:815–20. [PubMed] [Google Scholar]
- 6.Allen K, Blascovich J, Mendes WB. Cardiovascular reactivity and the presence of pets, friends, and spouses: the truth about cats and dogs. Psychosomatic Med. 2002;64:727–39. doi: 10.1097/01.psy.0000024236.11538.41. [DOI] [PubMed] [Google Scholar]
- 7.Odendaal JJ, Meintjes RA. Neurophysiological correlates of affiliative behaviour between humans and dogs. Vet J. 2003;165:296–301. doi: 10.1016/s1090-0233(02)00237-x. [DOI] [PubMed] [Google Scholar]
- 8.Barker SB, Knisely JS, McCain NL, Best AM. Measuring stress and immune response in healthcare professionals following interaction with a therapy dog: a pilot study. Psychol Rep. 2005;96:713–29. doi: 10.2466/pr0.96.3.713-729. [DOI] [PubMed] [Google Scholar]
- 9.Charnetski CJ, Riggers S, Brennan FX. Effect of petting a dog on immune system function. Psychological Rep. 2004;95:1087–91. doi: 10.2466/pr0.95.3f.1087-1091. [DOI] [PubMed] [Google Scholar]
- 10.Palley LS, O’Rourke PP, Niemi AM. Mainstreaming animal-assisted therapy. ILAR J. 2010;51:199–207. doi: 10.1093/ilar.51.3.199. [DOI] [PubMed] [Google Scholar]
- 11.Lima M, Silva K, Amaral I, de Sousa L. Finding an ally: can dogs help therapists promote communication in individuals with profound intellectual and multiple disabilities? J Altern Complement Med. 2012;18:2–3. doi: 10.1089/acm.2011.0461. [DOI] [PubMed] [Google Scholar]
- 12.Marcus DA, Bernstein CD, Constantin JM, Kunkel FA, Breuer P, Hanlon RB. Animal-assisted therapy at an outpatient pain management clinic. Pain Med. 2012;13:45–57. doi: 10.1111/j.1526-4637.2011.01294.x. [DOI] [PubMed] [Google Scholar]
- 13.Senna ER, De Barros AL, Silva EO, et al. Prevalence of rheumatic diseases in Brazil: a study using the COPCORD approach. J Rheumatol. 2004;31:594–7. [PubMed] [Google Scholar]
- 14.Marcus DA. Fibromyalgia: diagnosis and treatment options. Gender Medicine. 2009;6:139–51. doi: 10.1016/j.genm.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Lawrence RC, Fleson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McNally JD, Matheson DA, Bakowsky VS. The epidemiology of self-reported fibromyalgia in Canada. Chronic Dis Can. 2006;27:9–16. [PubMed] [Google Scholar]
- 17.Branco JC, Bannwarth B, Failde I, et al. Prevalence of fibromyalgia: a survey of five European countries. Semin Arthritis Rheumat. 2010;39:448–53. doi: 10.1016/j.semarthrit.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 18.Häuser W, Wolfe F, Tölle T, Uçeyler N, Sommer C. The role of antidepressants in the management of fibromyalgia syndrome: a systematic review and meta-analysis. CNS Drugs. 2012;26:297–307. doi: 10.2165/11598970-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Smith MT, Moore BJ. Pregabalin for the treatment of fibromyalgia. Expert Opin Pharmacother. 2012;13:1527–33. doi: 10.1517/14656566.2012.687373. [DOI] [PubMed] [Google Scholar]
- 20.Nüesch E, Häuser W, Bernardy K, Barth J, Jüni P. Comparative efficacy of pharmacological and non-pharmacological interventions in fibromyalgia syndrome: network meta-analysis. Ann Rheum Dis. doi: 10.1136/annrheumdis-2011-201249. in press. [DOI] [PubMed] [Google Scholar]
- 21.Wahner-Roedler DL, Elkin PL, Vincent A, et al. Use of complementary and alternative medical therapies by patients referred to a fibromyalgia treatment program at a tertiary care center. Mayo Clin Proc. 2005;80:55–60. doi: 10.1016/S0025-6196(11)62958-3. [DOI] [PubMed] [Google Scholar]
- 22.Terhorst L, Schneider MJ, Kim KH, Goodzdich LM, Stilley CS. Complementary and alternative medicine in the treatment of pain in fibromyalgia: a systematic review of randomized controlled trials. J Manipulative Physiol Ther. 2011;34:483–96. doi: 10.1016/j.jmpt.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 23.Terry R, Perry R, Ernst E. An overview of systematic reviews of complementary and alternative medicine for fibromyalgia. Clin Rheumatol. 2012;31:55–66. doi: 10.1007/s10067-011-1783-5. [DOI] [PubMed] [Google Scholar]
- 24.Wang C, Schmid CH, Rones R, et al. A randomized trial of tai chi for fibromyalgia. N Engl J Med. 2010;363:743–54. doi: 10.1056/NEJMoa0912611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carson JW, Carson KM, Jones KD, et al. A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain. 2010;151:530–9. doi: 10.1016/j.pain.2010.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Connor EL, White KM. Intentions and willingness to use complementary and alternative medicines: what potential patients believe about CAMs. Complement Ther Clin Pract. 2009;15:136–40. doi: 10.1016/j.ctcp.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 27.Ruggio M, DeSantis-Then L. Complementary and alternative medicine: longstanding legal obstacles to cutting edge treatment. J Health Life Sci Law. 2009;2:137–70. [PubMed] [Google Scholar]
- 28.Wong LY, Toh MP, Kong KH. Barriers to patient referral for complementary and alternative medicines and its implications on interventions. Complement Ther Med. 2010;18:135–42. doi: 10.1016/j.ctim.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 29.Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheumat. 1990;33:160–72. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 30.Kroenke K, Spitzer RL, Williams JW, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50:613–21. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 31.Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 32.Consoli G, Marazziti D, Ciapparelli A, et al. The impact of mood, anxiety, and sleep disorders on fibromyalgia. Compr Psychiatry. 2012;53:962–7. doi: 10.1016/j.comppsych.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 33.Marx MS, Cohen-Mansfield J, Regier NG, et al. The impact of different dog-related stimuli on engagement of persons with dementia. Am J Alzheimers Dis Other Demen. 2010;25:37–45. doi: 10.1177/1533317508326976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Farrar JY, Portenoy RK, Berlin JA, Kinman JL, Strom BL. Defining the clinically important difference in pain outcome measures. Pain. 2000;88:287–94. doi: 10.1016/S0304-3959(00)00339-0. [DOI] [PubMed] [Google Scholar]
- 35.Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–58. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 36.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine. 2008;33:90–4. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 37.Marcus DA. The Power of Wagging Tails: A Doctor’s Guide to Dog Therapy and Healing. New York, NY: Demos Health; 2011. [Google Scholar]
- 38.Coakley AB, Mahoney EK. Creating a therapeutic and healing environment with a pet therapy program. Complement Ther Clin Pract. 2009;15:141–6. doi: 10.1016/j.ctcp.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Braun C, Stangler T, Narveson J, Pettingell S. Animal-assisted therapy as a pain relief intervention for children. Complement Ther Clin Pract. 2009;15:105–9. doi: 10.1016/j.ctcp.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 40.Sobo EJ, Eng B, Kassity-Krich N. Canine visitation (pet) therapy: pilot data on decreases in child pain perception. J Holist Nurs. 2006;24:51–7. doi: 10.1177/0898010105280112. [DOI] [PubMed] [Google Scholar]
- 41.Ruchman R, Ruchman A, Jaeger J, Durand D, Kelly P. Animal-assisted anxiolysis prior to MRI. Am J Roentgenol. 2001;196:A120–34. [Google Scholar]
- 42.Colloca L, Benedetti F. How prior experience shapes placebo analgesia. Pain. 2006;124:126–33. doi: 10.1016/j.pain.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 43.Mease PJ. Further strategies for treating fibromyalgia: the role of serotonin and norepinephrine reuptake inhibitors. Am J Med. 2009;122(suppl):S44–55. doi: 10.1016/j.amjmed.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 44.Beetz A, Uvnäs-Moberg K, Julius H, Kotrschal K. Psychosocial and psychophysiological effects of human-animal interactions: the possible role of oxytocin. Front Psychol. 2012;3:234. doi: 10.3389/fpsyg.2012.00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miller SC, Kennedy C, Devoe D, et al. An examination of changes in oxytocin levels in men and women before and after interaction with a bonded dog. Anthrozoös. 2009;22:31–42. [Google Scholar]
- 46.Handlin L, Hydbring-Sandberg E, Nilsson A, Ejdebäck M, Jansson A, Uvnäs-Moberg K. Short-term interaction between dogs and their owners – effects on oxytocin, cortisol, insulin and heart rate – an exploratory study. Anthrozoös. 2011;24:301–16. [Google Scholar]
- 47.Haubenhofer DK, Kirchengast S. Physiological arousal for companion dogs working with their owners in animal-assisted activities and animal-assisted therapy. J Appl Anim Welf Sci. 2006;9:165–72. doi: 10.1207/s15327604jaws0902_5. [DOI] [PubMed] [Google Scholar]
- 48.Barker SB, Pandurangi AK, Best AM. Effects of animal-assisted therapy on patients’ anxiety, fear, and depression before ECT. J ECT. 2003;19:38–44. doi: 10.1097/00124509-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 49.Kazdin AE. Establishing the effectiveness of animal-assisted therapies: methodological standards, issues, and strategies. In: McCardle P, McCune S, Griffin JA, Maholmes V, editors. How Animals Affect Us. Washington, DC: American Psychological Association; 2011. pp. 35–51. [Google Scholar]
- 50.Nimer J, Lundahl B. Animal-assisted therapy: a meta-analysis. Anthrozoös. 2007;20:225–38. [Google Scholar]