Abstract
Objective This longitudinal study compared emerging adults with and without type 1 diabetes on life path decisions, health behaviors, and psychological well-being during the transition out of high school. Methods Administered questionnaires during the senior year of high school and 1 year later to 117 emerging adults with diabetes and 122 emerging adults without diabetes. Comparisons were conducted with respect to health status, sex, and school status. Results Those with and without diabetes chose similar life paths and engaged in similar levels of risky behaviors, but disturbed sleep increased for males with diabetes only. Having diabetes was not associated with depressive symptoms, loneliness, or bulimic symptoms, but was associated with lower life satisfaction and lower life purpose over time. Conclusions Emerging adults with and without diabetes fare similarly on most dimensions studied during the first year out of high school.
Keywords: emerging adulthood, health behavior, lifestyle, type 1 diabetes, well-being
Introduction
The developmental period from ages 18–25 years has been labeled “emerging adulthood” (Arnett, 2000). Emerging adulthood is the period of life during which the possibilities for the future are the most numerous, and identity exploration is at its lifetime peak. Arnett (2000) describes the first phase of emerging adulthood as a time when individuals are both excited about their new freedom but also uncertain because of the unsettled nature of their lives, as they explore the possibilities for their futures with respect to residential status, school status, vocation, romantic relationships, and identity. Adjustment to new responsibilities that arise during the first phase of emerging adulthood occurs rapidly with little structure and supervision, especially for those who move out of the house to live on their own for the first time or to attend college. The heightened freedom and reduced parental monitoring associated with emerging adulthood are coupled with an environment especially conducive to identity and lifestyle exploration, thus creating opportunities for risky behavior (Arnett, 2000; White et al., 2006). These circumstances also result in potential for social isolation and uncertainty about the future, which could diminish psychological well-being. Researchers who have examined risk behavior patterns during emerging adulthood have speculated that poor health behaviors established during emerging adulthood may persist into later stages of adulthood (Laska, Pasch, Lust, Story, & Ehlinger, 2009; Nelson, Story, Larson, Neumark-Sztainer, & Lytle, 2008). Diminished psychological well-being during emerging adulthood is an important concern in and of itself and may predict future declines in psychological well-being. Despite these potential risks, relatively few studies have focused on the health and well-being of emerging adults.
The transition to emerging adulthood may pose a special challenge to those with childhood chronic diseases, such as type 1 diabetes. The demands of managing a complicated illness like diabetes must be integrated into the normative changes in vocation, education, relationships, and living situations that accompany emerging adulthood (Weissberg-Benchell, Wolpert, & Anderson, 2007). In addition to the new responsibilities and freedoms that most emerging adults share, those managing diabetes become increasingly responsible for their self-care, with daily requirements such as blood glucose monitoring and assessment and insulin dose adjustments, and periodic activities such as scheduling physician appointments, ensuring availability of adequate supplies, and caring for themselves when sick. All of these activities are likely to have been monitored at least partially by parents during adolescence. In addition, some of the risky behaviors that occur during emerging adulthood, such as lack of physical activity and smoking, are predictive of long-term health detriments, such as vascular complications, for which those with type 1diabetes are particularly vulnerable (Bishop et al., 2009).
Despite the challenges faced by emerging adults with diabetes, little research has compared the transition experiences of those with and without diabetes. It is possible that those who are coping with diabetes may experience the years of emerging adulthood differently because of potential diabetes-related limitations to their exploration of future possibilities. Thus, the goal of this study was to compare individuals with and without diabetes during the transition out of high school in terms of the following: (1) life path decisions regarding education, vocation, and living situation; (2) health behaviors; and (3) psychological well-being. Below, we briefly review what is known about how individuals with diabetes compare with those without diabetes in each of these three domains during emerging adulthood.
Life Path Decisions
Of the many considerations facing youth during the initial stages of emerging adulthood, those regarding education, vocation, and living situation are likely the most deliberated because of their monumental influence on future outcomes. Research conducted before the Diabetes Control and Complications Trial (DCCT; Diabetes Control and Complications Research Group, 1994) found high school students with diabetes had similar intentions to work or pursue college but were more likely to plan to attend community college and had less career support from parents than control subjects (Myers, 1992). More recent research found that emerging adults with chronic illnesses (cancer, heart disease, epilepsy, type 1 diabetes) had lower college graduation rates, higher unemployment rates, higher probability of receiving public assistance, and lower incomes than those without chronic illness (Maslow, Haydon, McRee, Ford, & Halpern, 2011). However, that study did not examine those with diabetes separately from other chronic illnesses. The effect of health status on the pursuit of higher education is important because a college degree is associated with higher earning potential and job stability and mobility (Montgomery & Côté, 2003). Health status differences in the type of education pursued also is important because retention and degree completion rates are lower among community college students than among those enrolled in 4-year institutions (National Center for Education Statistics, 2008a).
Only a few studies have examined whether having diabetes impacts the decision for an emerging adult to leave home. In 2008, 36% of college students aged 19–23 years lived at home (National Center for Education Statistics, 2008b). One older study found that youth with diabetes (aged 17–22 years) were more likely to live at home (66%) than control subjects (33%), despite no health status differences in the distance of college from home (Myers, 1992). Another older study found a high rate of emerging adults with diabetes (aged 18–22 years) to be living at home (65%), but there was no comparison with emerging adults without diabetes (Wysocki, Hough, Ward, & Green, 1992). Given the drastic diabetes care improvements post-DCCT, it is unclear whether differences in educational and vocational decisions and living situations persist between today’s emerging adults with and without diabetes. If those with diabetes are found to choose colleges closer to home, on average, than control subjects, it may be an indication that these individuals are intentionally limiting their options for higher education, which, in turn, could lead to differences in income, quality of life, and life satisfaction both during the college years and beyond. If lifestyle differences are no longer found between the groups, it may indicate that post-DCCT improvements have mitigated some real or perceived lifestyle limitations for those with diabetes that existed in past decades. Encouragingly, one recent study found evidence that diabetes self-management was not associated with whether emerging adults with type 1 diabetes were living independently of their parents (Hanna et al., 2012).
Health Behavior
Emerging adulthood is associated with an array of poor health behaviors, including alcohol use, smoking, lack of physical activity, and disturbed sleeping patterns. For example, emerging adults have the highest rate of alcohol use (Substance Abuse and Mental Health Services Administration, 2011), especially for those who attend college (White, Labouvie, & Papadaratsakis, 2005). Drinking poses a more severe risk to individuals with diabetes than to peers without diabetes owing to impaired judgment that could negatively impact self-care (Ahmed, Karter, & Liu, 2006) and increased risk for hypoglycemia (Franz et al., 2002). Smoking is common in early adulthood; 20.1% of adults between the ages of 18–24 years smoked regularly in 2010 (Center for Disease Control and Prevention, 2011). In addition, 90% of smokers begin the habit before the age of 21 years (Mowery, Brick, & Farrelly, 2000), and early initiation of smoking is related to becoming a heavier smoker and to smoking for longer durations (Elders, Perry, Eriksen, & Giovino, 1994). Because individuals with diabetes have heightened risk for heart and kidney disease, and smoking exacerbates the risk for both (Bishop et al., 2009; Muehlhauser, Sawicki, & Berger, 1986), smoking is potentially more detrimental to the health of those with diabetes than those without. Declining physical activity after high school, especially for college students, typically results in freshman year weight gain (Butler, Black, Blue, & Gretebeck, 2004). Physical activity is especially important for those with diabetes because it helps to achieve good glycemic control and may decrease risk for complications (Chimen et al., 2012). Finally, disturbed sleep is common among college students (Lund, Reider, Whiting, & Prichard, 2010), and poor sleep quality is associated with poorer health (Katz & McHorney, 2002). Because poor sleep and poor glycemic control are believed to be reciprocally related (Barone & Menna-Barreto, 2011), disturbed sleep may be more disruptive to college students with diabetes than those without diabetes. In this study, we examined potential differences between emerging adults with and without diabetes in all of these health behaviors. Because youth with diabetes may be more conscious of their health and the increased risk that many of these behaviors pose, we hypothesize lower levels of risk behavior among youth with than without diabetes.
Psychological Well-Being
Depressive symptoms increase during adolescence, peak in young adulthood, and then decline throughout the rest of the life span (Arnett, 2004; Kessler, Mickelson, Walters, Zhao, & Hamilton, 2004). A meta-analytic review revealed that youth with diabetes experience more depression than those without diabetes (Reynolds & Helgeson, 2011). The overall effect sizes were small to medium, and smaller in more recent studies. Adults with type 1 diabetes experience more depressive symptoms and are more likely to use antidepressants than peers (Gendelman et al., 2009). Two meta-analytic reviews based largely on cross-sectional studies found that depressive symptoms are an important risk factor for diabetes health because of links to poor glycemic control (Lustman et al., 2000) and diabetes-related complications (de Groot, Anderson, Freedland, Clouse, & Lustman, 2001).
Another index of psychological well-being especially relevant to emerging adulthood is loneliness. Loneliness tends to peak during emerging adulthood (Rokach, 2000). Lonely people experience more disturbed sleep and higher cardiovascular reactivity than those who are not lonely (Cacioppo et al., 2002) and is associated with poor glycemic control (Barone & Menna-Barreto, 2011). Cardiovascular reactivity is linked to long-term cardiovascular complications (Matthews, Zhu, Tucker, & Whooley, 2006). We know of no data comparing the levels of loneliness between emerging adults with and without diabetes.
An aspect of psychological health especially relevant to diabetes is disturbed eating behavior. People with diabetes—especially females—are at greater risk for eating disorders compared with people without diabetes (Jones, Lawson, Daneman, Olmsted, & Rodin, 2000), and disturbed eating behaviors are linked to diabetes-related complications (Rydall, Rodin, Olmsted, Devenyi, & Daneman, 1997). Typically emerging in early adolescence, eating disturbances increase during the transition to college (Vohs, Heatherton, & Herrin, 2001), a trend at least partially attributed to the college environment’s high stress, changing roles, and achievement orientation (Striegel-Moore, Silberstein, Grunberg, & Rodin, 1990). Given their strong implications for diabetes-related complications, it is important to examine health status differences in eating behaviors during emerging adulthood.
Finally, one of the primary tasks of emerging adulthood is the exploration and establishment of identity, defined as the extent to which one has explored goal alternatives and committed to life choices (Luyckx et al., 2008). Emerging adults with diabetes with stronger senses of identity experience fewer diabetes-related problems and have lower levels of depressive symptoms than those with weaker senses of identity (Luyckx et al., 2008). Identity exploration is lower in emerging adults with diabetes than in comparison peers (Luyckx et al., 2008). Although we did not include a measure of identity exploration, we examined life purpose and life satisfaction as potential outcomes of the identity exploration process. Emerging adults with diabetes may have more difficulties establishing an independent identity than their peers owing to the greater likelihood of continuing parent involvement and oversight with respect to diabetes self-care that may bleed into other life aspects, resulting in a lower sense of life purpose and/or life satisfaction during early emerging adulthood.
The Present Study
Using Arnett’s (2000) theory of emerging adulthood, we examined the life domains that are critical to this stage of development, that are undergoing tremendous change at this time, and that have implications for future well-being—specifically, lifestyle decisions such as going to college and leaving home, health behaviors such as alcohol consumption and smoking, and psychological well-being such as depressive symptoms and loneliness. Few studies have compared these domains among emerging adults with and without type 1 diabetes, and most of the ones that exist are decades old. If emerging adults with type 1diabetes are somehow disadvantaged in comparison with those without diabetes, this sets forth a disadvantage that will influence the course of their futures and suggests intervention efforts may be prudent. Even if those with diabetes are found to engage in the same level of risk behavior as those without diabetes, they may be putting themselves in danger with respect to their health because these health risk behaviors have more severe consequences for those with than those without diabetes.
We compared youth with and without diabetes in their senior year of high school and 1 year later with respect to life path decisions, health behaviors, and psychological well-being. Because of technological advances in the treatment of diabetes, we did not hypothesize health status differences in life path decisions. However, we did hypothesize that those with diabetes would report better health behavior than those without diabetes owing to the stronger health implications of health behaviors. Given past research, we cautiously hypothesized that those with diabetes would report lower psychological well-being than those without diabetes. Because psychological well-being and health behaviors frequently differ by sex, we also compared males and females and explored the interaction between sex and health status (i.e., participants with vs. without diabetes). Because attending college may have implications for risk behavior and psychological well-being (Blanco et al., 2008; O’Malley & Johnston, 2002), we also examined the impact of attending college on health behaviors and psychological well-being.
Materials and Methods
Participants
Participants were 239 youth (122 without diabetes, 117 with diabetes) who were in their last semester of high school at baseline. Demographic data are shown in Table I.
Table I.
Participant Demographics at Baseline (T1)
| Diabetes (n = 117) | Control (n = 122) | |
|---|---|---|
| Agea | 18.15 (.41) | 18.02 (.49) |
| BMI*,a | 25.68 (4.03) | 24.12 (4.72) |
| Social status (Hollingshead)*,a | 42.61 (11.08) | 46.58 (13.70) |
| Maleb | 47.0% (58) | 46.3% (56) |
| Household structure | ||
| Lives with | ||
| Mother and fatherb | 66.7% (78) | 68.9% (84) |
| Otherb | 20.5% (24) | 24.6% (30) |
| Declined to answerb | 12.8% (15) | 6.5% (8) |
| Race | ||
| Whiteb | 92.3% (108) | 93.4% (114) |
| Otherb | 7.7% (9) | 6.6% (8) |
| Ethnicity | ||
| Hispanicb | 1.7% (2) | 3.3% (4) |
| Not Hispanicb | 95.7% (112) | 95.9% (117) |
| No answerb | 2.6% (3) | 0.8% (1) |
| Pump | 57.50% | |
| Time since diagnosis (years)c | 11.12 (3.10, 5.75–17.74) | |
| HbA1c (%)c | 8.90 (1.75, 6.2–13.7) |
Note. Birthdate, sex, household structure, race/ethnicity, and social status were collected for a previous study (Helgeson et al., 2007); all remaining data were collected at T1.
aMean (SD).
bMean (n).
cMean (SD, range).
*Health status difference at p < .05.
Procedure
This study was approved by the appropriate institutional review boards. Participants were recruited from a previous study that explored the transition to adolescence (Helgeson, Snyder, Escobar, Siminerio, & Becker, 2007). Briefly, participants originally were recruited from the local Children’s Hospital, when they were aged 12 years on average (response rate 77%). Control subjects were recruited from area malls (n = 70) and physicians’ offices (n = 61) from the same geographic region (response rate 66%). Of the 132 participants with diabetes and the 131 control subjects, 121 (91.7%) with diabetes and 123 (93.9%) without diabetes agreed to be contacted for this new study that explored their transition into emerging adulthood.
Consent forms were mailed to participants. Once signed consent forms were received, youth were emailed an online questionnaire to complete during the spring of their senior year of high school (Time 1 [T1]) and 1 year later (Time 2 [T2]). Participants without online access were sent a questionnaire by mail to complete by hand (T1: 11.9%; T2: 11.5%). The majority of both groups completed both assessments (diabetes n = 117 [97%]; control n = 122 [99%]).
Participants from the original study who did not participate in the present study (n = 24) were compared with those who completed the current study (n = 239) with respect to the demographic and disease-related variables shown in Table I. Only two differences were found: (a) participants who dropped out of the diabetes group had a higher average body mass index (BMI; 24.72) than those who stayed in the study, (21.80), t(132) = −2.16, p = .03, and (b) control participants who did not participate in the current study were more likely to be non-white (37.5%; n = 3) than those who did participate, (7.3%; n = 9), X2(131) = 8.22, p = .004.
Measures
Demographics
Birthdate, sex, household structure, race/ethnicity, and social status (Hollingshead, 1975) were collected from the previous study (see Helgeson, Snyder, Esobar, Siminerio, & Becker, 2007). The other demographic information shown in Table I was collected at T1.
Life Path Decisions
At T2, participants indicated whether they were enrolled in college and/or working and where they lived. Names of colleges were obtained to examine institutional information (e.g., selectivity, size) from the 29th edition of Barron’s Profiles of American Colleges (College Division of Barron’s Educational Series, 2011).
Health Behaviors
Five health behaviors were examined using standardized questionnaires. Questions regarding alcohol consumption in the past 30 days, binge drinking in the past two weeks, and smoking in the past 12 months were taken from the Monitoring the Future Study (Johnston, 2010) and were represented as dichotomous variables indicating whether the participant had engaged in each behavior (i.e., any alcohol consumption, at least one binge, any smoking). Physical activity was measured with the Paffenberger Physical Activity Questionnaire (Paffenbarger, Hyde, Wing, & Hsieh, 1986) as weekly energy expenditure (kcal) per week in sports, leisure, and recreational activities. Five questions from the Pittsburgh Sleep Quality Index (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989) were used to measure sleep: typical bed time, typical wake time, number of minutes to fall asleep, number of hours typically slept at night, and sleep quality. This information was used to calculate four components of sleep (quality, duration, latency, and efficiency) on a scale from 0 (very good) to 3 (very poor), which were summed to create a sleep index. Higher numbers indicated worse sleep. Reliability statistics are not reported for the health behavior measures because all are either dichotomous or standardized scoring schemes and thus are not amenable to standard reliability calculations.
Psychological Well-Being
Depressive symptoms were measured with the Center for Epidemiological Studies Depression Scale (Radloff, 1977), which consists of 20 summed items, each of which is rated on a 0 (none of the time) to 3 (most of the time) scale during the past week (T1: α = .89; T2: α = .93). Loneliness was measured with the eight-item UCLA Loneliness Scale (Russell, 1996) in which participants rated how often they felt as described (i.e., “I lack companionship,” “I feel left out.”) on a 1 (never) to 4 (often) scale. Items were averaged to create a loneliness index (T1: α = .84; T2: α = .86).
Two subscales from the Eating Disorders Inventory (Garner, Olmstead, & Polivy, 1983; Steel, Young, Lloyd, & Macintyre, 1989) were used to measure disturbed eating behavior: drive for thinness (four items; T1: α = .91, T2: α = .91) and bulimic symptoms (seven items; T1: α = .82; T2: α = .85). Three items of the original drive for thinness subscale were removed because typical diabetes care artificially inflates their presence (Steel et al., 1989). Participants rated each item on a 1 (never) to 5 (very often) scale, and items for each subscale were averaged.
The seven-item purpose in life subscale from Ryff’s Six Dimensions of Psychological Well-Being (Ryff & Keyes, 1995) was used to measure life purpose. Participants rated their agreement with items on a scale from 1 (strongly disagree) to 6 (strongly agree), and ratings were averaged to create an index in which higher numbers indicated a stronger sense of life purpose (T1: α = .73; T2: α = .77). Life satisfaction was measured with the five-item Life Satisfaction Inventory (Diener, Emmons, Larsen, & Griffin, 1985). Items were rated on a 1 (strongly disagree) to 7 (strongly agree) scale, and the average was taken (T1: α = .90; T2: α = .92).
Statistical Analysis
The t-tests and chi-square analyses were used to examine health status differences in demographic variables (see Table I) and life path decisions (see Table II). Then, 2 (sex: male, female) × 2 (health status: control, diabetes) × 2 (school status: full-time college student, not full-time college student) × 2 (time: T1, T2) mixed Analysis of Covariance was used to examine continuous measures of health behaviors and psychological well-being. Because there were health status differences in BMI, t(238) = −2.94, p = .004, d = −.38, and social status, t(242) = 2.50, p = .01, d = 0.32, these two variables were statistically controlled in all analyses.
Table II.
Participants Enrolled in College and/or Working at T2
| Diabetes (n = 117) | Control (n = 122) | |
|---|---|---|
| School | ||
| Full-time | 75.2% (88) | 74.6% (91) |
| Part-time | 2.6% (3) | 1.6% (2) |
| Not in school | 22.2% (26) | 23.8% (29) |
| Working | ||
| Yes | 52.1% (61) | 52.5% (64) |
| No | 47.9% (56) | 47.5% (58) |
| Work/School combinations | ||
| College only | 46.2% (54) | 47.6% (58) |
| Other school only | 1.7% (2) | 0.0% (0) |
| Work only | 17.1% (20) | 13.9% (17) |
| Work and college | 30.7% (36) | 27.1% (33) |
| Work and other school | 0.0% (0) | 1.6% (2) |
| Military | 0.0% (0) | 4.1% (5) |
| Other | 4.3% (5) | 5.7% (7) |
The analysis of dichotomous health behaviors (alcohol use, binge drinking, smoking) was more complicated. We used logistic regression analysis to predict T1 outcomes, with sex and health status as predictors. For prediction of these behaviors at T2, the respective T1 behavior was statistically controlled, and health status, sex, school status, and their associated interactions were tested as predictors. Analyses only included student status as a predictor of T2 health behaviors because college status was only applicable to this wave of measurement. Because neither of these analyses tests the changes in health behavior over time, we used chi-square analyses to examine overall differences in the dichotomous health behaviors between T1 and T2.
Results
Life Path Decisions
As shown in Table II, there were no health status differences in college attendance or work status. Three-quarters of both groups were attending college full-time, and about half of each group was working. Comparable percentages of each group combined college and work. Overall, living situations were comparable. Of those attending college, about one-quarter of each group was living at home (diabetes: 26.4%; control: 25.3%); of those not in college, roughly 70% were living at home (diabetes: 71.4%; control: 70.0%).
Among those attending college, there were no health status differences in most college characteristics: two-year vs. four-year, private vs. public, size, distance from home, or average in-state tuition. However, control participants attended colleges with significantly higher competitiveness ratings (M = 2.71, SD = 1.09) than those with diabetes (M = 2.32, SD = 1.08), t(133) = −2.11, p = .04, d = .37. There were no health status differences in self-reported grade point average at the end of the first semester in college.
Health Behaviors
There were no main effects or interactions involving health status, sex, or school status on alcohol consumption at either wave of data collection. However, more participants reported consuming alcohol at T2 (50.9%) than at T1 (31.7%), X2(1, 230) = 25.63, p < .001.
There were no effects of health status, sex, or school status on binge drinking at T1, but there was a sex by student status interaction at T2. Male participants were more likely to report binge drinking than females, and this was particularly true among full-time college students (males full-time: 50.0%; females full-time: 38.8%; males not full-time: 5.0%; female not full-time: 6.2%; odds ratio 6.15; 95% confidence interval 1.03–36.54, p = .046). In addition, more participants reported binge drinking at T2 (33.5%) than at T1 (15.9%), X2(1, 233) = 22.96, p < .001.
There were no effects of health status or school status on smoking behavior at T1, but there was a main effect of sex. Logistic regression indicated that males were 2.23 times more likely than females to smoke at T1 (Odds Ratio 2.23; 95% confidence interval 1.08–4.60, p = .03). There were no effects of health status, sex, or student status at T2. There was a main effect of time such that more participants smoked at T2 (36.6%) than at T1 (28.4%), X2(1, 232) = 86.64, p < .001.
Returning to the repeated-measures analyses of variances for continuous health behavior outcomes, there was a main effect of sex, but not of health status, school status, or time, on physical activity. Males reported more physical activity (M = 3983.59, SE = 343.59) than females (M = 2848.61, SE = 362.17), F(1, 224) = 5.18, p = .02,  = .02.
= .02.
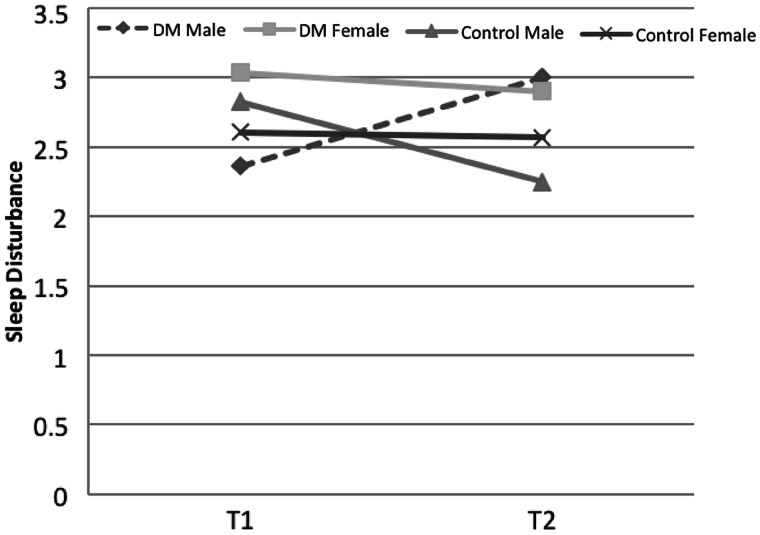
There were no main effects of any of the predictor variables on sleep, but a three-way health status by sex by time interaction emerged, F(1, 224) = 5.75, p = .02,  = .03, as shown in Figure 1. Among control participants, males’ sleep disturbance declined from T1 (M = 2.83, SE = 0.26) to T2 (M = 2.25, SE = 0.28), whereas females’ sleep disturbance remained constant between T1 (M = 2.61, SE = 0.27) and T2 (M = 2.57, SE = 0.29). In contrast, among the diabetes group, male participants’ sleep disturbance increased from T1 (M = 2.36, SE = 0.27) to T2 (M = 3.00, SE = 0.29), but females’ sleep disturbance remained unchanged between T1 (M = 3.04, SE = 0.28) and T2 (M = 2.90, SE = 0.30).
= .03, as shown in Figure 1. Among control participants, males’ sleep disturbance declined from T1 (M = 2.83, SE = 0.26) to T2 (M = 2.25, SE = 0.28), whereas females’ sleep disturbance remained constant between T1 (M = 2.61, SE = 0.27) and T2 (M = 2.57, SE = 0.29). In contrast, among the diabetes group, male participants’ sleep disturbance increased from T1 (M = 2.36, SE = 0.27) to T2 (M = 3.00, SE = 0.29), but females’ sleep disturbance remained unchanged between T1 (M = 3.04, SE = 0.28) and T2 (M = 2.90, SE = 0.30).
Figure 1.
Health status by sex by time interaction predicting sleep disturbance. Among control participants, males’ sleep disturbance declined from T1 to T2, whereas females’ sleep disturbance remained the same. Among those with diabetes, males’ sleep disturbance increased, but females’ sleep disturbance remained unchanged between T1 and T2 (p = .02).
Psychological Well-Being
There was a main effect of sex on depressive symptoms such that males reported fewer depressive symptoms (M = 1.54, SD = 0.05) than females (M = 1.85, SD = 0.05), F(1, 224) = 18.40, p < .001,  = .08, but this main effect was qualified by an interaction with school status, F(1, 224) = 4.04, p = .05,
= .08, but this main effect was qualified by an interaction with school status, F(1, 224) = 4.04, p = .05,  = .02. Male’s depressive symptoms were similar, regardless of school status (full-time: M = 1.57, SD = 0.05; not full-time: M = 1.51, SD = 0.08), whereas females who were not enrolled in college reported more depressive symptoms than females who were full-time students (full-time: M = 1.74, SD = 0.05; not full-time: M = 1.96, SD = 0.09). There were no other effects on depressive symptoms. None of our predictor variables predicted loneliness.
= .02. Male’s depressive symptoms were similar, regardless of school status (full-time: M = 1.57, SD = 0.05; not full-time: M = 1.51, SD = 0.08), whereas females who were not enrolled in college reported more depressive symptoms than females who were full-time students (full-time: M = 1.74, SD = 0.05; not full-time: M = 1.96, SD = 0.09). There were no other effects on depressive symptoms. None of our predictor variables predicted loneliness.
There was a main effect of sex on drive for thinness such that females reported a stronger drive for thinness (M = 2.35, SD = 0.10) than males (M = 1.34, SD = 0.09), F(1, 224) = 57.68, p < .001,  = .21. In addition, there was a health status by school status × time interaction, F(1, 224) = 4.51, p = .04,
= .21. In addition, there was a health status by school status × time interaction, F(1, 224) = 4.51, p = .04,  = .02. Full-time students in both the control and diabetes groups reported no change in drive for thinness between T1 (control: M = 1.79, SE = 0.11; diabetes: M = 1.85, SE = 0.11) and T2 (control: M = 1.70, SE = 0.10; diabetes: M = 1.79, SE = 0.10). Among those not enrolled in full-time college, drive for thinness increased between T1 (M = 1.77, SE = 0.19) and T2 (M = 1.91, SE = 0.17) for control subjects and decreased between T1 (M = 2.13, SE = 0.19) and T2 (M = 1.81, SE = 0.18) for those with diabetes.
= .02. Full-time students in both the control and diabetes groups reported no change in drive for thinness between T1 (control: M = 1.79, SE = 0.11; diabetes: M = 1.85, SE = 0.11) and T2 (control: M = 1.70, SE = 0.10; diabetes: M = 1.79, SE = 0.10). Among those not enrolled in full-time college, drive for thinness increased between T1 (M = 1.77, SE = 0.19) and T2 (M = 1.91, SE = 0.17) for control subjects and decreased between T1 (M = 2.13, SE = 0.19) and T2 (M = 1.81, SE = 0.18) for those with diabetes.
There was a main effect only of sex on bulimic symptoms. Females reported higher levels of bulimic symptoms (M = 1.61, SD = 0.06) than males (M = 1.33, SD = 0.06), F(1, 224) = 10.98, p < .001,  = .05.
= .05.
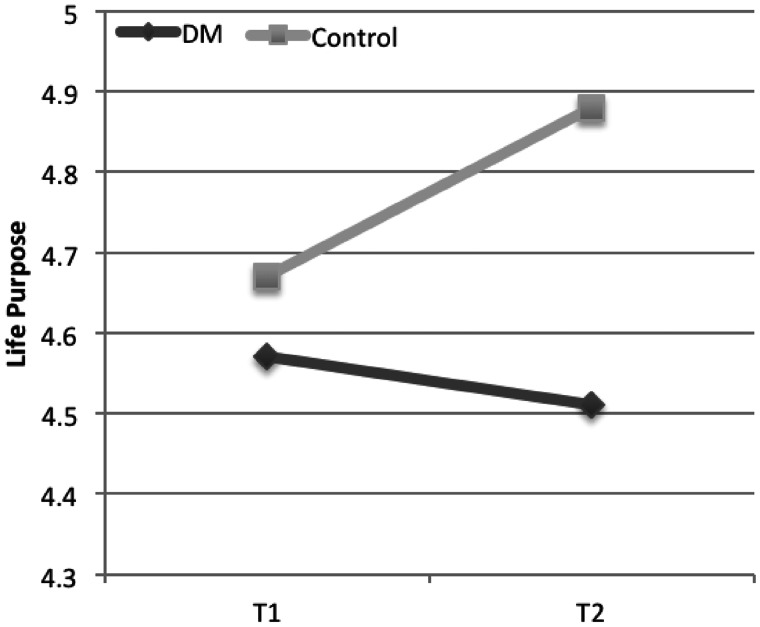
For life purpose, there was main a effect of sex such that females reported higher life purpose (M = 4.76, SD = 0.07) than males (M = 4.56, SD = 0.07), F(1, 224) = 4.26, p = .04,  = .02, and a main effect of health status, F(1, 224) = 6.39, p = .01,
= .02, and a main effect of health status, F(1, 224) = 6.39, p = .01,  = .03, which was qualified by an interaction with time, F(1, 224) = 6.06, p = .02,
= .03, which was qualified by an interaction with time, F(1, 224) = 6.06, p = .02,  = .03. As shown in Figure 2, there were no health status differences in life purpose at T1 (control: M = 4.67, SE = 0.08; diabetes: M = 4.57, SE = 0.08), but life purpose increased among the control group by T2 (M = 4.88, SE = 0.08) and remained the same among the diabetes group by T2 (M = 4.51, SE = 0.08).
= .03. As shown in Figure 2, there were no health status differences in life purpose at T1 (control: M = 4.67, SE = 0.08; diabetes: M = 4.57, SE = 0.08), but life purpose increased among the control group by T2 (M = 4.88, SE = 0.08) and remained the same among the diabetes group by T2 (M = 4.51, SE = 0.08).
Figure 2.
Health status by time interaction predicting life purpose. Both groups reported similar life purpose at T1, but life purpose increased only for the control group between T1 and T2. (p = .02).
There were main effects of health status and school status on life satisfaction. Control participants scored higher in life satisfaction (M = 5.40, SE = 0.12) than those with diabetes (M = 4.88, SE = 0.12), F(1, 224) = 9.36, p = .002,  = .04. Those enrolled in school full-time expressed greater life satisfaction (M = 5.42, SD = 0.09) than those who were not (M = 4.86, SD = 0.15), F(1, 224) = 9.77, p = .002,
= .04. Those enrolled in school full-time expressed greater life satisfaction (M = 5.42, SD = 0.09) than those who were not (M = 4.86, SD = 0.15), F(1, 224) = 9.77, p = .002,  = .04.
= .04.
Conclusions
These findings indicate that life path decisions are similar for those with and without diabetes. Although older research reported that youth with diabetes were more likely to attend a community college and live at home compared with those without diabetes (Myers, 1992), we found that those with diabetes were equally likely to attend college, to attend similar colleges, and to live at home as comparison peers. Previous health status differences may have disappeared as a result of advances in diabetes-related technology and education. These advances have increased the flexibility of diabetes self-care and the probability of optimal glycemic control and diabetes-related health outcomes. The only difference detected between the two groups was that colleges attended by the control group had higher competitiveness ratings than those attended by those with diabetes. This difference could indicate lower levels of academic ambition by those with diabetes or perhaps a difference in academic interests between the groups. However, it is important to emphasize that the colleges chosen by those with and those without diabetes were the same in all other respects, including average Scholastic Aptitude Test score, distance from home, and in-state tuition. Therefore, it is unclear that any substantive difference exists in colleges attended by those with and those without diabetes in this study.
In terms of health behavior, it was hypothesized that those with diabetes would engage in less risky behavior than those without diabetes because these behaviors posed more hazards to health for those with diabetes. We found no support for this hypothesis in terms of alcohol consumption, binge drinking, smoking, or physical activity. In fact, the only health behavior that was associated with health status was disturbed sleep. We observed an increase in sleep disturbance over time for males with diabetes that was not apparent among females with diabetes or control subjects. We could postulate that the transition into emerging adulthood and the increase in risk behavior observed during this period has something to do with the increased sleep disturbance, but we cannot explain why transition difficulties would be linked to sleep disturbance for males with diabetes alone. Future research should replicate this finding and continue to explore sleep disturbances because it is an area of research that has been frequently linked to health outcomes (Barone & Menna-Barreto, 2011; Katz & McHorney, 2002).
It is somewhat elucidating to present our alcohol and smoking rates 1 year after high school graduation in the context of national statistics for adults aged 18–25 years. Compared with alcohol consumption nationwide (48.9%; Substance Abuse and Mental Health Services Administration, 2011), the rate for control subjects (56.3%) was slightly higher than national statistics, and the rate for the diabetes group (47.0%) was comparable, but the rates for our two groups were not statistically different. Binge drinking rates for the control group (37.5%) were comparable with national statistics (40.6%; Substance Abuse and Mental Health Services Administration, 2011), whereas binge drinking rates for the diabetes group (29.9%) were somewhat lower than national rates. As with alcohol consumption, binge drinking rates did not significantly differ between our two groups. In addition, smoking rates reported by our sample 1 year after high school graduation (37.8%) were comparable with national statistics (40.8%; Substance Abuse and Mental Health Services Administration, 2011), and rates of those with (41.0%) and without (34.7%) diabetes were not statistically different. These findings suggest that those with diabetes do not engage in lower rates of risky behavior than those without diabetes. This is somewhat disturbing because the same level of risky behavior could have more severe consequences for those with than those without diabetes. Our findings support previous research (Arnett, 2000) that these risk behaviors increase during the early stages of emerging adulthood; alcohol consumption, binge drinking, and smoking all significantly increased during the course of this study. It will be important to follow these behaviors throughout the college years to examine future trends among the two groups.
In terms of psychological well-being, there were no health status differences in depressive symptoms, loneliness, or bulimic symptoms. The lack of a group difference in depressive symptoms is in contrast to previous studies (Lustman et al., 2000). However, a recent meta-analysis suggested that health status differences in depressive symptoms among youth are smaller in more recent studies (Reynolds & Helgeson, 2011). Again, this may be due to recent advances in technology, such as insulin pumps and continuous glucose monitoring, which have provided a more seamless integration of self-care behavior into an individual’s lifestyle or better clinical monitoring and management of depression in youth with diabetes. Finding that diabetes was not predictive of higher depressive symptoms is encouraging.
There were three psychological well-being indices on which health status differences did appear: life satisfaction, life purpose, and drive for thinness. Emerging adults with diabetes reported a lower level of life satisfaction and life purpose than peers without diabetes. It is possible that the extra responsibilities and restrictions of diabetes self-care while adjusting to college and work life create enough daily hassle to decrease life satisfaction. It also is possible that the increased attention toward the future that accompanies emerging adulthood resulted in a stronger focus on long-term consequences of having diabetes, which could affect life satisfaction and life purpose. The finding that the sense of life purpose increased between T1 and T2 for the control group, but not for those with diabetes, suggests that the extra responsibilities associated with diabetes self-management may interfere with identity exploration, which, in turn, may interfere with feelings of life purpose. Because we did not measure identity exploration directly, however, this interpretation remains speculative and requires future investigation. Because these indices of psychological well-being have not been investigated among emerging adults with diabetes, it remains for future research to replicate these health status differences, to follow youth over time to see whether they persist, and to identify their underlying mechanisms.
The third aspect of psychological well-being that showed differences with respect to health status is drive for thinness. We found that drive for thinness did not change over time among those enrolled in college full-time, regardless of health status, but decreased among those with diabetes and increased among control subjects for those who were not in college. This three-way interaction is difficult to interpret and needs to be replicated.
The majority of emerging adults—both diabetes and controls—were attending college full-time 1 year after high school graduation. Because those who are not in college may face different challenges than those who are enrolled in college, examining effects of school status on these outcomes is an important consideration. We found greater life satisfaction among those who were enrolled in college full-time than those who were not, which is perhaps not surprising given the opportunities for personal growth and optimism for a bright future that higher education provides. We also found that females who were not enrolled in college reported higher depressive symptoms than those in college.
Taken collectively, these findings suggest that there is minimal evidence that having diabetes disrupts patterns of health behavior or well-being proposed by emerging adulthood theory (Arnett, 2000), at least during the first year of this transition period. First, we found little evidence that lifestyle decisions were different for the two groups. Even the characteristics of colleges selected by the two groups were almost identical. Second, health behaviors were comparable across the board. There is no evidence that those with diabetes were limiting their explorations of risk behaviors that are common at this age of development, although it would be preferable for risk behavior to be lower among those with type 1 diabetes to avoid increased risk for complications. We found that control subjects reported higher life satisfaction and life purpose than those with diabetes, and that those with diabetes did not evidence the increase in life purpose over time that control subjects showed. However, it is possible that these effects may dissipate in subsequent years as those with diabetes learn to more readily incorporate their extra health-related responsibilities into their newly acquired adult roles. In short, the small number of health status differences indicates that diabetes was not a serious detriment to overall well-being during the first year of emerging adulthood.
It is important to remind readers that we assessed only the early period of emerging adulthood. It will be important to follow these youth to determine the progression of these patterns. Nationally, 24% of 4-year college freshmen do not return for their sophomore year (The National Center for Higher Education Management Systems, 2010). It is reasonable to expect that a portion of our sample will alter their life path trajectories during the next few years. The question is whether those trajectories are the same for emerging adults with and without diabetes. Parents of emerging adults with diabetes may be particularly concerned about the transition to college, and some may remain involved in their child’s self-care during the first year. In subsequent years, as parents yield increasing levels of responsibility to their youth, risky health behaviors may increase. A related challenge to be faced by emerging adults with diabetes during the next few years is the transition to adult health care services. Although the majority of these participants remained in the pediatric health care system during their first year out of high school, many will transition to adult services during the next few years (Helgeson et al., 2012). The transition from the structured team-based pediatric health care system to the adult health care system has been associated with a host of difficulties, including decreased frequency of physician visits, and poor glycemic control (Allen & Gregory, 2009; Peters & Laffel, 2011).
Before concluding, we note several study limitations. First, participants were largely white and middle-class, limiting our ability to generalize these findings to minority or lower social status populations who may have fewer resources to negotiate the challenges of emerging adulthood. Second, only 25% of our sample was not enrolled in college full-time, limiting our power to detect effects of college status on outcomes and to determine whether college status interacted with health status to predict outcomes, thus increasing the possibility of type 2 error. Therefore, we view all of our findings as in need for replication. The relative paucity of studies comparing emerging adults with and without diabetes on this wide range of important outcomes justifies the presentation of these data.
In conclusion, these data suggest that emerging adults with diabetes and their peers choose similar life paths after high school. Those with and without diabetes engage in similar levels of risky health behavior and experience similar levels of psychological well-being, with a few exceptions. Further investigation will ascertain whether similarities between groups persist throughout emerging adulthood. Given the potential health-related risks associated with the outcomes of this study for those with type 1 diabetes, determining whether these are factors that become increasingly problematic over time will help health care workers to identify those who are at risk for poor health outcomes. Based on the current findings, however, clinicians can be cautiously optimistic that youth with diabetes can achieve similar outcomes to their peers without diabetes during the initial transition into emerging adulthood.
Funding
This work was supported by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disorders, (grant number R01 DK60586) to V.H.
Conflicts of interest: None declared.
Acknowledgments
The authors appreciate the support of the project manager, Pamela Snyder, and the research assistants Abigail Vaughn and Jamie Vance for their assistance on this project.
References
- Ahmed A T, Karter A J, Liu J. Alcohol consumption is inversely associated with adherence to diabetes self-care behaviours. Diabetic Medicine. 2006;23:795–802. doi: 10.1111/j.1464-5491.2006.01878.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen D, Gregory J. The transition from children’s to adult diabetes services: Understanding the “problem”. Diabetic Medicine. 2009;26:162–166. doi: 10.1111/j.1464-5491.2008.02647.x. [DOI] [PubMed] [Google Scholar]
- Arnett J J. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55:469–480. [PubMed] [Google Scholar]
- Arnett J J. Adolescence and emerging adulthood. Upper Saddle River, NJ: Pearson Prentice Hall; 2004. [Google Scholar]
- Barone M T, Menna-Barreto L. Diabetes and sleep: A complex cause-and-effect relationship. Diabetes Research and Clinical Practice. 2011;91:129–137. doi: 10.1016/j.diabres.2010.07.011. [DOI] [PubMed] [Google Scholar]
- Bishop F K, Maahs D M, Snell-Bergeon J K, Ogden L G, Kinney G L, Rewers M. Lifestyle risk factors for atherosclerosis in adults with type 1 diabetes. Diabetes & Vascular Disease Rresearch. 2009;6(4):269–275. doi: 10.1177/1479164109346359. [DOI] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin D S, Grant B F, Liu S M, Olfson M. Mental health of college students and their non-college-attending peers: Results from the National Epidemiologic Study on Alcohol and Related Conditions. Archives of General Psychiatry. 2008;65(12):1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler S M, Black D R, Blue C L, Gretebeck R J. Change in diet, physical activity, and body weight in female college freshman. American Journal of Health Behavior. 2004;28:24–32. doi: 10.5993/ajhb.28.1.3. [DOI] [PubMed] [Google Scholar]
- Buysse D J, Reynolds C F, Monk T H, Berman S R, Kupfer D J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Cacioppo J T, Hawkley L C, Crawford L E, Ernst J M, Burleson M H, Kowalewski R B, Malarkey W B, Van Cauter E, Berntson G G. Loneliness and health: Potential mechanisms. Psychosomatic Medicine. 2002;64(3):407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. 2011. Vital signs: Current cigarette smoking among adults aged ≥ 18 years - United States, 2005-2010. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6035a5.htm?s_cid=mm6035a5.htm_w#fig1. [Google Scholar]
- Chimen M, Kennedy A, Nirantharakumar K, Pang T, Andrews R, Narendran P. What are the health benefits of physical activity in type 1 diabetes mellitus? A literature review. Diabetologia. 2012;55:542–551. doi: 10.1007/s00125-011-2403-2. [DOI] [PubMed] [Google Scholar]
- College Division of Barron’s Educational Series. 2011 Barron’s Profiles of American Colleges. 29th ed. Hauppauge, NY: Barron's Educational Series; 2011. [Google Scholar]
- De Groot M, Anderson R, Freedland K E, Clouse R E, Lustman P J. Association of depression and diabetes complications: A meta-analysis. Psychosomatic Medicine. 2001;63:619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- Diabetes Control and Complications Research Group. Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus. The Journal of Pediatrics. 1994;125:177–188. doi: 10.1016/s0022-3476(94)70190-3. [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons R A, Larsen R J, Griffin S. The satisfaction with life scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Elders M J, Perry C L, Eriksen M P, Giovino G A. The report of the Surgeon General preventing tobacco use among young people. American Journal of Public Health. 1994;84:543–547. doi: 10.2105/ajph.84.4.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franz M J, Bantle J P, Beebe C A, Brunzell J D, Chiasson J L, Garg A, Holzmeister L A, Hoogwerf B, Mayer-Davis E, Mooradian A D, Purnell J Q, Wheeler M. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2002;25:148–198. doi: 10.2337/diacare.25.1.148. [DOI] [PubMed] [Google Scholar]
- Garner D M, Olmstead M P, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2:15–34. [Google Scholar]
- Gendelman N, Snell-Bergeon J K, McFann K, Kinney G, Paul Wadwa R, Bishop F, Rewers M, Maahs D M. Prevalence and correlates of depression in individuals with and without type 1 diabetes. Diabetes Care. 2009;32:575–579. doi: 10.2337/dc08-1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna K M, Weaver M T, Stump T E, Slaven J E, Fortenberry J D, Dimeglio L A. Readiness for living independently among emerging adults with type 1 diabetes. The Diabetes Educator. 2012;39(1):92–99. doi: 10.1177/0145721712465341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson V, Reynolds K, Snyder P R, Palladino D K, Becker D J, Siminerio L, Escobar O. 2012. Characterizing the transition from paediatric to adult care among emerging adults with Type 1 diabetes. Diabetic Medicine. Retrieved from http://onlinelibrary.wiley.com/doi/10.1111/dme.12067/abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson V S, Snyder P R, Escobar O, Siminerio L, Becker D. Comparison of adolescents with and without diabetes on indices of psychosocial functioning for three years. Journal of Pediatric Psychology. 2007;32:794–806. doi: 10.1093/jpepsy/jsm020. [DOI] [PubMed] [Google Scholar]
- Hollingshead A B. Two factor index of social position. New Haven, CT: Privately printed; 1957. [Google Scholar]
- Hollingshead A D B. Four factor index of social status. Yale Univ., Department of Sociology; 1975. [Google Scholar]
- Johnston L D, O'Malley P M, Bachman J G, Schulenberg J E. Monitoring the future national survey results on drug use, 1975–2008. Volume II: College students and adults ages 19–50. 2009. p. 306. (NIH Publication No. 09-7403). Bethesda, MD: National Institute on Drug Abuse. [Google Scholar]
- Jones J M, Lawson M L, Daneman D, Olmsted M P, Rodin G. Eating disorders in adolescent females with and without type 1 diabetes: cross sectional study. British Medical Journal. 2000;320:1563–1566. [PMC free article] [PubMed] [Google Scholar]
- Katz D A, McHorney C A. The relationship between insomnia and health-related quality of life in patients with chronic illness. Journal of Family Practice. 2002;51:229–236. [PubMed] [Google Scholar]
- Kessler R C, Mickelson K D, Walters E E, Zhao S, Hamilton L. Age and depressionin the MIDUS study. In: Brim O G, Ryff C D, Kessler R C, editors. How healthy are we? A national study of well-being at mid-life. Chicago, IL: The University of Chicago Press; 2004. pp. 227–251. [Google Scholar]
- Laska M N, Pasch K E, Lust K, Story M, Ehlinger E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prevention Science. 2009;10:376–386. doi: 10.1007/s11121-009-0140-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund H G, Reider B D, Whiting A B, Prichard J R. Sleep patterns and predictors of disturbed sleep in a large population of college students. The Journal of Adolescent Health. 2010;46:124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Lustman P J, Anderson R J, Freedland K E, De Groot M, Carney R M, Clouse R E. Depression and poor glycemic control: A meta-analytic review of the literature. Diabetes Care. 2000;23:934–942. doi: 10.2337/diacare.23.7.934. [DOI] [PubMed] [Google Scholar]
- Luyckx K, Schwartz S J, Berzonsky M D, Soenens B, Vansteenkiste M, Smits I, Goossens L. Capturing ruminative exploration: Extending the four-dimensional model of identity formation in late adolescence. Journal of Research in Personality. 2008;42:58–82. [Google Scholar]
- Maslow G R, Haydon A, McRee A L, Ford C A, Halpern C T. Growing up with a chronic illness: Social success, educational/vocational distress. The Journal of Adolescent Health. 2011;49:206–212. doi: 10.1016/j.jadohealth.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews K A, Zhu S, Tucker D C, Whooley M A. Blood pressure reactivity to psychological stress and coronary calcification in the Coronary Artery Risk Development in Young Adults Study. Hypertension. 2006;47:391–395. doi: 10.1161/01.HYP.0000200713.44895.38. [DOI] [PubMed] [Google Scholar]
- Montgomery M J, Côté J E. College as a transition to adulthood. In: Adams G R, Berzonsky M D, editors. Blackwell Handbook of Adolescence. Oxford, England: Blackwell Publishing; 2003. pp. 149–172. [Google Scholar]
- Mowery P D, Brick F D, Farrelly M C. Legacy first look report 3: Pathways to established smoking: Results from the 1999 National Youth Tobacco Survey. Washington, DC: American Legacy Foundation; 2000. [Google Scholar]
- Muehlhauser I, Sawicki P, Berger M. Cigarette-smoking as a risk factor for macroproteinuria and proliferative retinopathy in Type I (insulin-dependent) diabetes. Diabetologia. 1986;29:500–502. doi: 10.1007/BF00453501. [DOI] [PubMed] [Google Scholar]
- Myers J T. Transition into adulthood with a chornic illness focus: Insulin-dependent diabetes mellitus. Ann Arbor, MI: The University of Michigan; 1992. [Google Scholar]
- National Center for Education Statistics. 2008a. Percentage distribution of first-time undergraduates in 2003-–2004, by persistence or attainment rate, control and type of postsecondary institution, program plans, and attendance status. Retrieved January 5, 2012, from http://nces.ed.gov/programs/coe/analysis/figures/2008-fig18.asp. [Google Scholar]
- National Center for Education Statistics. 2008b. Percentage distribution of undergraduates, by their local residence while enrolled and selected institutional and student characteristics: 2007-–2008. Retrieved January 5, 2012, from http://nces.ed.gov/pubs2010/2010205.pdf. [Google Scholar]
- The National Center for Higher Education Management Systems. 2010. Retention rates: First-time college freshmen returning their second year. Retrieved February 7, 2012, from http://www.higheredinfo.org/dbrowser/index.php?submeasure=223&year=2010&level=nation&mode=data&state=0. [Google Scholar]
- Nelson M C, Story M, Larson N I, Neumark-Sztainer D, Lytle L A. Emerging adulthood and colege-aged youth: An overlooked age for weight-related behavioral change. Obesity. 2008;16:2205–2211. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- O’Malley P M, Johnston L D. Epidemiology of alcohol and other drug use among american college students. Journal of Studies on Alcohol and Drugs. 2002;(Suppl 14):23–29. doi: 10.15288/jsas.2002.s14.23. [DOI] [PubMed] [Google Scholar]
- Paffenbarger R S, Hyde R, Wing A L, Hsieh C. Physical activity, all-cause mortality, and longevity of college alumni. New England Journal of Medicine. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- Peters A, Laffel L. Diabetes care for emerging adults: Recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care. 2011;34:2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reynolds K A, Helgeson V S. Children with diabetes compared to peers: Depressed? Distressed? A meta-analytic review. Annals of Behavioral Medicine. 2011;42:29–41. doi: 10.1007/s12160-011-9262-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rokach A. Perceived causes of loneliness in adulthood. Journal of Social Behavior and Personality. 2000;15:67–84. [Google Scholar]
- Russell D W. UCLA loneliness scale (version 3): Reliability, validity, and factor structure. Journal of Personality Assessment. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Rydall A C, Rodin G M, Olmsted M P, Devenyi R G, Daneman D. Disordered eating behavior and microvascular complications in young women with insulin-dependent diabetes mellitus. New England Journal of Medicine. 1997;336:1849–1854. doi: 10.1056/NEJM199706263362601. [DOI] [PubMed] [Google Scholar]
- Ryff C D, Keyes C L. The structure of psychological well-being revisited. Journal of Personality and Social Psychology. 1995;69:719–727. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- Steel J M, Young R J, Lloyd G G, Macintyre C C. Abnormal eating attitudes in young insulin-dependent diabetics. The British Journal of Psychiatry. 1989;155:515–521. doi: 10.1192/bjp.155.4.515. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore R H, Silberstein L R, Grunberg N E, Rodin J. Competing on all fronts: Achievement orientation and disordered eating. Sex Roles. 1990;23(11):697–702. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. 2011. Results from the 2010 national survey on drug use and health: Summary of national findings. Retrieved January 5, 2012, from http://www.samhsa.gov/data/nsduh/2k10nsduh/2k10results.htm. [Google Scholar]
- Vohs K D, Heatherton T F, Herrin M. Disordered eating and the transition to college: A prospective study. The International Journal of Eating Disorders. 2001;29:280–288. doi: 10.1002/eat.1019. [DOI] [PubMed] [Google Scholar]
- Weissberg-Benchell J, Wolpert H, Anderson B J. Transitioning from pediatric to adult care: A new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care. 2007;30:2441–2446. doi: 10.2337/dc07-1249. [DOI] [PubMed] [Google Scholar]
- White H R, Labouvie E W, Papadaratsakis V. Changes in substance use during the transition to adulthood: A comparison of college students and their non-college age peers. Journal of Drug Issues. 2005;35:281–306. [Google Scholar]
- White H R, McMorris B J, Catalano R F, Fleming C B, Haggerty K P, Abbott R D. Increases in alcohol and marijuana use during the transition out of high school into emerging adulthood: The effects of leaving home, going to college, and high school protective factors. Journal of Studies on Alcohol. 2006;67:810–822. doi: 10.15288/jsa.2006.67.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T, Hough B S, Ward K M, Green L B. Diabetes mellitus in the transition to adulthood: Adjustment, self-care, and health status. Journal of Behavioral Pediatrics. 1992;13:194–201. [PubMed] [Google Scholar]