Abstract
At the start of the HIV epidemic, 50% of new infections were among injection drug users (IDUs) in New York City. While HIV has declined among IDUs since the mid 1990s, parenteral transmission continues to overburden blacks/Hispanic IDUs. Individual risk behaviors do not explain the distribution of HIV/AIDS among IDUs. Social and/or structural factors are likely fueling racial disparities creating a high-risk socio-environmental context. While increased access to structural interventions (i.e. syringe exchange and pharmacy syringe access) are needed, it may not be sufficient to eliminate HIV/AIDS disparities among IDUs. Research on incorporating structural factors into intervention strategies is needed.
Keywords: risk behaviors, racial disparities, structural factors, structural interventions, disease burden
Introduction
One of the greatest achievements in the field of HIV prevention during the last few years is the significant decrease in crude HIV prevalence rates among injection drug users (IDUs) in New York City (NYC), one of the U.S. cities with the highest AIDS case rate, more than three times the U.S. average with 1.2% of the population in NYC living with HIV/AIDS. New HIV diagnoses have decreased among IDUs in NYC since the mid 1990’s. This is likely due to prevention programs aimed at decreasing injection risk practices by providing safe, legal access to sterile syringes such as syringe exchange programs (SEP), where used syringes are exchanged for new ones free of charge, and the New York State Expanded Syringe Access Program (ESAP), which allows pharmacies to sell syringes without a prescription. Rates of injection/sexual risk behaviors have decreased (despite using drugs) since these prevention programs were implemented in NYC; IDUs in NYC report lower injection risk behaviors when compared to previous years (before 1995) when syringe exchange and ESAP programs were not available, largely because of the availability of sterile syringes (Institute of Medicine, 2006; Des Jarlais et al., 2009).
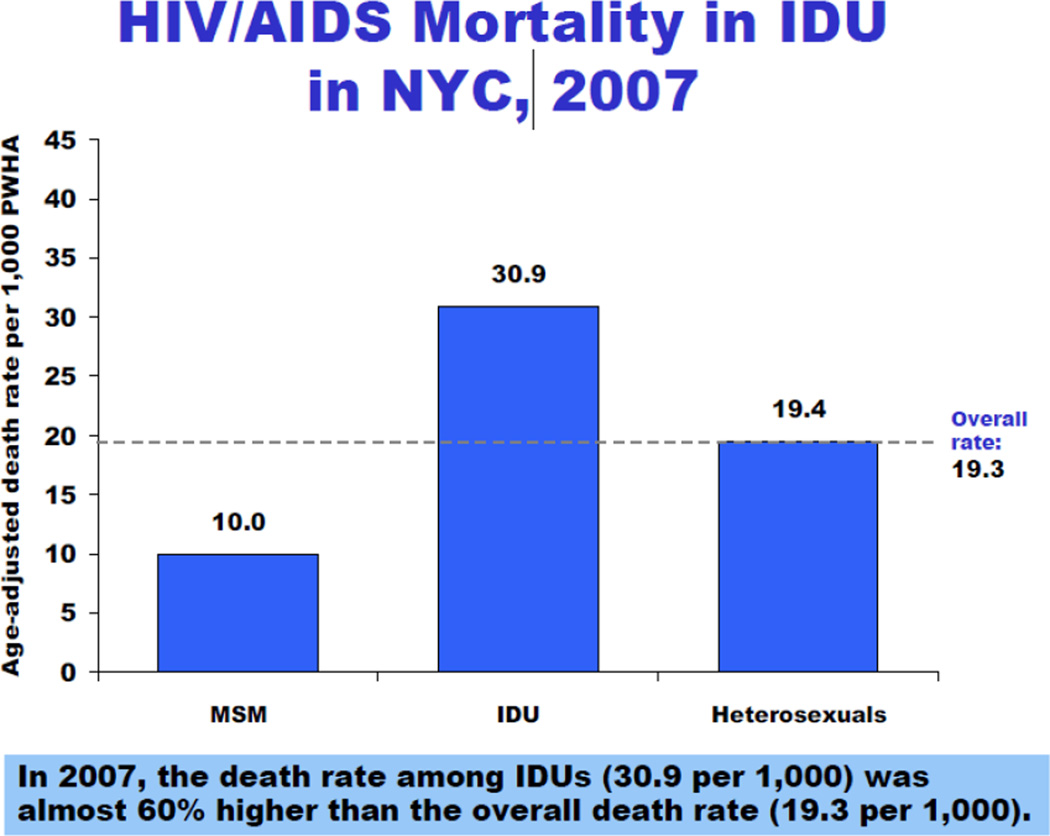
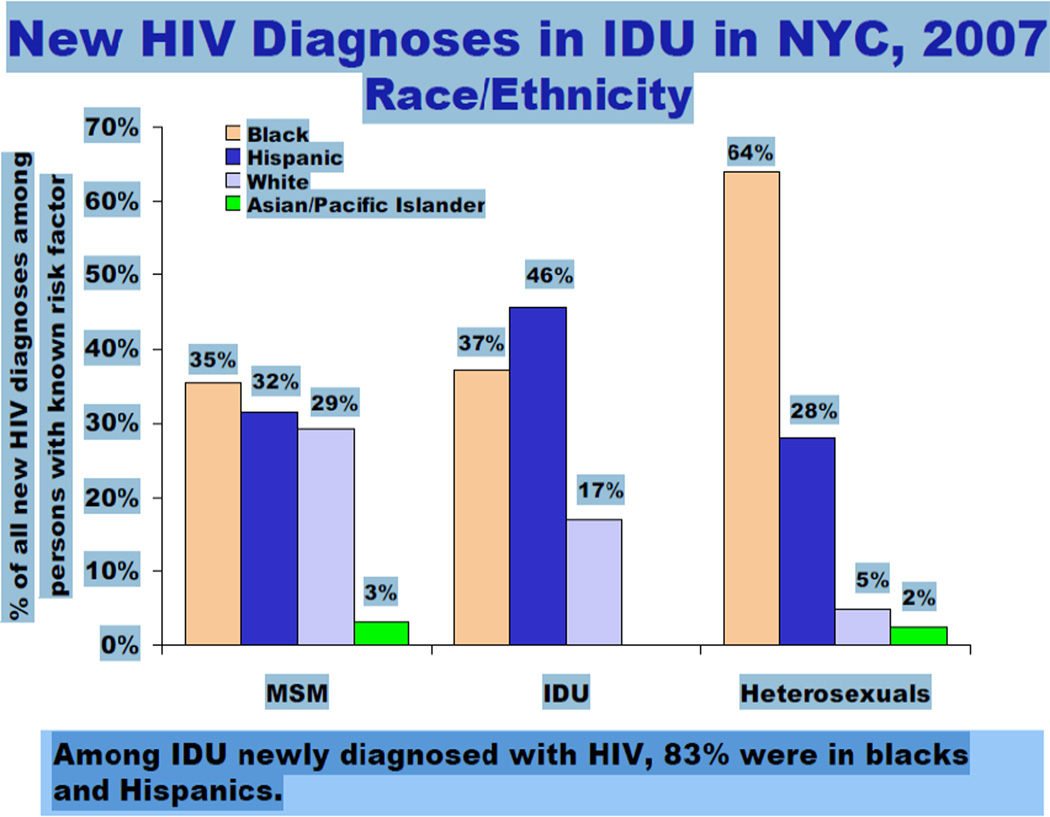
Despite the progress that has been accomplished in this area, HIV continues to disproportionately affect black and Hispanic IDUs in NYC and racial/ethnic disparities in HIV among IDUs continue to be profound. Within these communities, IDUs have been excessively burdened with, and at high risk of HIV/AIDS morbidity and mortality [Figure 1] with blacks and Hispanics representing the largest percentage of HIV/AIDS cases in the IDU category (NYC DOHMH, 2009). While IDUs constitute only 6.5% of new HIV cases of known transmission category in NYC in 2007, 83% of newly diagnosed HIV cases in the IDU category were among blacks and Hispanics [Figure 2] (NYC DOHMH, 2009). The question remains as to why, despite all successes in HIV prevention programs among IDUs, we continue to have persistent racial/ethnic disparities in HIV among IDUs. In this paper, we set forth to first, describe the epidemiology of HIV among IDUs in NYC with a specific focus on race/ethnicity; second, describe individual, socio-cultural, and structural factors that have helped explain racial/ethnic disparities in HIV among IDUs; and third, provide an overview of empirically-based intervention research that has targeted black and/or Hispanic IDUs or has provided evidence of having potential to reduce racial disparities in HIV among IDUs. Throughout this report, we provide recommendations for critical next steps to eliminate racial disparities in HIV among IDUs in NYC and other similar urban environments in the U.S.
Figure 1.
(HIV Epidemiology and Field Services Program, New York City Department of Health and Mental Hygiene. HIV/AIDS in New York City, 2007: Injection Drug Users. Available at http://www.nyc.gov/html/doh/html/dires/epi_surveillance.shtml. Accessed September 28, 2009.
Figure 2.
(HIV Epidemiology and Field Services Program, New York City Department of Health and Mental Hygiene. HIV/AIDS in New York City, 2007: Injection Drug Users. Available at http://www.nyc.gov/html/doh/html/dires/epi_surveillance.shtml. Accessed September 28, 2009.
Epidemiology of HIV among IDUs in NYC and role of race/ethnicity
At the start of the HIV epidemic, close to half of all new infections were among IDUs in northeastern cities (Holmberg, 1996). The geographic distribution of HIV prevalence and incidence has closely followed heroin and cocaine epidemics across the U.S. with the northeastern cities representing the heaviest drug markets (NIDA, 2000). Given the concentrated drug markets that have historically targeted many urban, minority communities, it is not surprising that throughout the epidemic, black and Hispanic IDUs have been disproportionately burdened by HIV and AIDS.
Recent New York City Department of Health (NYCDOH) statistics reveal that the NYC neighborhoods most affected by HIV/AIDS include Upper Manhattan (East and Central Harlem), the South Bronx, and Central Brooklyn, communities where a large percentage of the population are black and/or Hispanic. These neighborhoods help illustrate the profound racial/ethnic disparities in HIV among black/Hispanic IDUs. For example, 2007 data shows that while only 10.3% of the new HIV diagnoses of known transmission category were among IDUs in East Harlem, the prevalence pool of HIV/AIDS is largest among IDUs (29.5%) and blacks/Hispanics (91.8%) in East Harlem. Additionally, among people living with HIV/AIDS (PLWHA) in East Harlem, IDUs accounted for the greatest number of deaths (37.3%) in 2007 (NYC DOHMH, 2009).
In Central Harlem, where blacks and Hispanics accounted for 92.2% of new HIV cases, 6.1% of HIV cases of known transmission category were among IDUs in 2007. Nearly one quarter of IDUs were burdened with HIV/AIDS and 40% of HIV/AIDS mortality was attributed to injection drug use. While Central Harlem was identified as having the second highest rate of HIV diagnoses in Manhattan, a slight decrease has been observed from 2006 to 2007; however, the proportion of those diagnosed with HIV that were attributed to injection drug use remained unchanged (NYC DOHMH, 2009).
The South Bronx area of NYC also experiences one of the highest rates of HIV transmission attributed to injection drug use. In the Hunts Point-Mott Haven neighborhood of the South Bronx, IDUs represent 16.8% of newly diagnosed HIV cases of known transmission category and 31.8% of PLWHA. Nearly half (44.8%) of HIV/AIDS deaths were among IDUs in this neighborhood (NYC DOHMH, 2009)
In Brooklyn 30.5% of people live with HIV/AIDS and 7.4% of new HIV cases of known transmission category in 2007 were IDUs. Central Brooklyn has more than twice the death rate from HIV relative to NYC. In this neighborhood, 35% of HIV diagnoses have already progressed to AIDS (NYC DOHMH, 2009).
Data from each of these communities clearly describe the increased morbidity and mortality of HIV/AIDS in black and Hispanic neighborhoods, which is a stark contrast to neighborhoods with IDU communities that are predominantly white. For example in 2007, 56.2% of PLWHA in the Chelsea-Clinton neighborhood of Manhattan were white and of those, 14.4% were IDUs. In this lower Manhattan neighborhood, less than 3.9% of new HIV cases were among IDUs (2007) and less than 11.2% of those diagnosed with HIV had progressed to AIDS. In contrast, blacks and Hispanics make up 54.2% of the PLWHA population in the Lower East Side neighborhood, where 27% of PLWHA in 2007 were IDUs and 8.8% of new HIV cases of known transmission category were attributed to injection drug use. More than 55.3% of HIV/AIDS mortality in the Lower East Side was among IDUs (NYC DOHMH, 2009). In the upcoming section, we describe reasons for this variation in HIV/AIDS prevalence, morbidity and mortality which should be more carefully and strategically considered with attempting to dismantle the problem of disparities in the U.S.
Explaining Racial/Ethnic Disparities among IDUs in NYC
The reason for the observed racial/ethnic disparities in HIV/AIDS among IDUs is not entirely understood, however researchers have identified potential factors that point to mechanisms that are both multifactorial and multilevel when trying to account for this serious public health problem. For example, individual (risk behaviors, socioeconomic status, HIV knowledge), social contextual (high risk networks, socio-cultural factors), and structural factors (poverty, neighborhood factors, health care access, access to HIV prevention services, incarceration) are key categories of risk that have been examined and provide the foundation for explaining disproportionate risk and burden of HIV experienced by black and Hispanic IDUs.
Individual risk behaviors and black/Hispanic IDUs
Individual risk behaviors (injection and sexual) have not explained the racial/ethnic differences found in HIV prevalence (Kottiri et al., 2002, Des Jarlais et al., 2009). In a recent study comparing injection and sexual risk behaviors among IDUs during pre- and post-syringe exchange programs in NYC, pre-exchange individual risk behaviors were found to be similar across racial/ethnic groups, and were significantly lower (receptive syringe sharing, unprotected sex, and passing on a used syringe to someone else) for blacks in the post exchange group (Des Jarlais et al., 2009). White drug users start to inject earlier and have a higher lifetime prevalence of injection drug use, while black drug users are drug addicted/dependent for longer periods and are more likely to relapse after treatment (CDC, 2002; Broz & Ouellet, 2008). However, this alone would not explain the profound racial disparities that were observed, especially when other injecting risk behaviors are similar or lower among blacks when compared to whites. Puerto Rican-born IDUs (who predominantly make up the Hispanic IDU population in NYC) or those recently arriving to NYC from Puerto Rico tend to have higher rates of injection drug use and are more likely to report higher injection risk behaviors than both black and white IDUs (Absalon et al., 2006; Kottiri et al., 2002), with few exceptions, (CDC, 2002; Broz & Ouellet, 2008), and this may help explain some of the racial/ethnic differences between Hispanic and white IDUs.
Two specific marginalized subgroups of black and Hispanic IDUs that have shown to be at increased HIV risk through both individual high risk behaviors and high risk sexual networks include men who have sex with men (MSM) and women who have sex with women (WSW). Injection risk behaviors among black MSM IDUs are found to be lower when compared to whites (Harawa et al., 2004). In general, MSM IDUs are at elevated HIV risk mostly from sexual risk behaviors and not injection behaviors (Diaz et al., 2001). These reports are further supported by others, one of which found that drug-using MSM carried the highest HIV prevalence when compared to heterosexual men, heterosexual women, and WSW, regardless of injection status (Absalon et al., 2006). A second report noted that HIV risk was higher among non-injection drug-using MSM, when compared to IDU MSM in NYC (Ompad et al., 2004), and among a similarly recruited MSM drug-using study sample, no association was found between injection drug use and HIV status (Fuller et al., 2005). Even though HIV risk in black/Hispanic MSM is mainly associated with high sexual risk behaviors, there is data suggesting that HIV positive black and Hispanic MSM engage in lower risk sexual behaviors compared with HIV negatives which could be due to changes in behavior after receiving an HIV diagnosis (Des Jarlais et al., 2004, Fuller et al., 2005, Robles et al., 1996; Sinclair et al., 2004). Drug-using MSM reported similar levels of condom use, multiple sexual partners, casual partners, and HIV-infected partners compared to heterosexual men, heterosexual women, and WSW (Absalon et al., 2006; Fuller et al., 2005). This suggests other social and/or structural factors, unmeasured here and in previous studies, may be accounting for racial disparities in HIV among both injecting and non-injecting MSM. Such factors might include homophobia, stigma, discrimination, and inability to access services that may create high risk sexual networks and social settings where exposure is more likely to occur functioning as a mediator or modifier of the relationship between HIV and behavioral risk (Fuller et al., 2004).
In the substance use literature where there are sufficient samples of women, WSW tend to have either the highest HIV prevalence rate or the second highest (MSM being highest) compared with other IDU groups (heterosexual males, MSM, heterosexual females). In one of our recent community IDU studies among Latino IDUs, nearly half of the WSW were HIV infected and the risk behaviors that were significantly associated with HIV transmission were both injection and sexually-related, involving individual and social network risk characteristics (Diaz et al., 2001). Women who identify as WSW have higher sexual risk behaviors with men, and higher injection risk behaviors overall suggesting that having sex with the same sex, in the case of WSW, is not related to their HIV risk. Other studies in NYC found high-risk sexual behaviors higher in men than in women; however, it is important to note that women in these studies had higher rates of HIV when compared to heterosexual men. One explanation for this is that women engage less in high risk sexual behaviors but have riskier sexual partners (Absalon et al., 2006). For example, reports have noted drug-using WSW to be more likely to report sexual partnerships with MSM than heterosexual women (Absalon et al., 2006; Ompad et al., 2004). Additional research is needed to further explore sexual partnerships and sexual networks of drug-using WSW to help inform more targeted interventions.
In summary, these reports do not provide evidence to support the possibility of increased individual risk behaviors as an explanation for racial disparities in HIV, but consistently highlight the importance of the social environment within which individual behavior occurs. Thus, targeting the social environment should be more prominently considered in current HIV prevention and intervention strategies.
Social Contextual Factors
High Risk Networks
A growing body of evidence suggests that persistent racial differences in HIV incidence are likely fueled by the differential burden of HIV disease among across various community and social environments (Friedman et al, 2000, Kottiri et al., 2002). For example, there has been a strong research focus on social networks and the social norms within these networks that influence individual behavior and the social setting within which risk behavior occurs. Studies have found significant associations between risky social networks and HIV seroprevalence among IDUs in NYC (Friedman et al., 1997; Neaigus et al., 1996). Within urban samples of predominantly black IDUs, those with riskier social networks were more likely to engage in risky syringe sharing and sexual norms (Latkin et al., 2009). This becomes the more prominent issue to contend with, particularly in situations where individual injecting and sexual risk behaviors are low or moderate. Given the importance of the social environment, particularly those directly impacting and/or defining socioeconomic status, it is critical to include further discussion of the role of structural factors that impact individuals, particularly in drug-using environments (Sumartojo, 2000).
Socio-cultural factors
Researchers have also examined socio-cultural factors to help explain racial disparities, particularly among Hispanic drug users. Puerto Ricans carry the overwhelming majority of HIV/AIDS cases acquired through injection drug use. In 2007, 40% of AIDS cases (nationwide) among island-born Puerto Ricans were among IDUs (CDC, 2007). Despite the paucity of substance use research among Hispanic subgroups, acculturation into the U.S. has been hypothesized as one explanation for the high levels of drug use and heightened HIV risk among Hispanics, particularly Puerto Ricans migrating to New York. For example, acculturation has been found to be significantly associated with syringe sharing among Puerto Rican IDUs in Western Massachusetts (Delgado et al., 2008). Recent data has shown that Puerto Rican IDUs who have recently migrated to NYC from Puerto Rico (and who are less acculturated) have a higher likelihood of sharing needles and paraphernalia, using dirty needles, buying used needles, attending shooting galleries, not cleaning syringes, not using condoms, and exchanging sex for drugs/money when compared with Puerto Rican IDUs who have been in the US for a longer period of time (Deren et al., 2003; Deren et al., 2007; Estrada, 2005; Freeman, Williams, & Saunders, 1999). This suggests that earlier periods of acculturation are riskier than the later periods. The relationship between recent arrival to NYC and HIV risk has been shown in a number of studies (Deren et al., 2003; Deren et al., 2007) and stresses the need for prioritizing prevention programs targeting Puerto Rican IDUs who have recently arrived to NYC. It is also important to investigate other Hispanic non-US born IDU migrants (e.g., Mexican, Cuban), a population that is typically faced with limited access to information and services, are more affected by poverty, unemployment, lack of access to sterile needles, and have high availability of drugs in impoverished neighborhoods (Freeman, Williams, & Saunders, 1999).
There is a more limited body of research documenting a relationship between cultural factors and behavioral risk among Non-Hispanic, black IDUs in the U.S. Friedman and colleagues suggest that certain social norms and values within black culture—struggle, propriety, and survival—have shaped individual HIV risk behaviors (Friedman, Cooper, & Osborne, 2009). More evidence is needed to further examine these cultural associations among IDUs, the necessary conditions for them to operate and how these factors may contribute to a higher risk and burden of HIV, above and beyond individual risk behavior.
Structural factors
For the purposes of this paper, which focuses on HIV prevention and interventions, “structural” factors relate to the impact that economic, social, policy, and systems has on individual behavior. For example, some of our earlier work noted that when taking neighborhood context into account, black drug users from highly disadvantaged neighborhoods were more likely to initiate injection drug use during adolescence than white drug users (Fuller et al., 2005). When the context of the neighborhood or social environment had not been taken into account, the contrary had been consistently reported, that is, white drug users initiating injection at a younger age (Ellickson & Morton, 1999; Fuller et al., 2001; Fuller et al., 2002; Golub & Johnson, 2001; Kral, Lorvick, & Edlin, 2000). These neighborhood-level data provide support for further investigation to include an emphasis on neighborhoods and socioeconomic factors, which have been shown to have a more detrimental impact on individuals from black communities compared with their white counterparts (Sampson & Wilson, 1995).
As previously noted, migration is an important structural factor driving the HIV epidemic among Hispanic IDUs. Whether immigrants (primarily from Mexico) or migrants (in the case of U.S. territory-Puerto Rico), these individuals are typically burdened by a myriad of socioeconomic problems (Freeman, Williams, & Saunders, 1999). It has been suggested that Puerto Rican drug users migrating to the U.S., and specifically to NYC are drawn by greater availability of prevention programs such as syringe exchange and methadone programs in NYC, and thus the reason why drug users travel from Puerto Rico (PR) to NYC. Puerto Rican IDUs who recently arrived to NYC may face obstacles accessing services due to lack of knowledge of services and language barriers upon arrival to NYC. The relationship between recent arrival to NYC and HIV risk has been shown in a number of studies (Deren et al., 2003; Deren et al., 2007; Freeman, Williams, & Saunders,1999) and the high rates of injection risk behaviors and HIV among this Puerto Rican IDU subgroup (the NYC-PR “airbridge”) (Deren et al., 2003; Deren et al., 2007) is an essential reason to prioritize prevention programs among this mobile population and design interventions that directly target the social context of migration.
Although, not necessarily evident, access to services and its relationship to HIV prevention and intervention strategies may also impact HIV risk among black/Hispanic IDUs. For example, while IDUs have a long history of poor access to health care, even those with health insurance have low rates of health care utilization (Cronquist et al., 2001). Lower levels of access to HIV testing and antiretroviral therapy has been observed among minorities, women, drug users, individuals of lower socioeconomic status, and those who lack insurance; a considerable literature has documented the delay in HIV care and services as well (Andersen et al., 2000; Andrulis et al., 1992; Celentano et al., 1998; Celentano et al., 2001; Mauskopf et al., 1994; Moore et al., 1994; Solomon et al., 1991; Stein et al., 1991; Strathdee et al., 1998;Turner et al., 1994a; Turner et al., 1994b). There are two important issues to consider when thinking about the relationship between limited access to services and HIV risk. First, lack of access to services may be a significant obstacle to confidential HIV testing and services in clinical settings. Being tested for HIV is a critical first step in access to treatment and in HIV prevention (CDC, 2006). One of the HIV prevention strategies outlined by the CDC in recent years has been an emphasis on routine HIV testing; a large proportion of HIV cases in general remain undiagnosed, and those unaware of having HIV may inadvertently infect others. Data suggests those diagnosed with HIV tend to adopt safer behaviors (Des Jarlais, 2004; Robles et al., 1996; Sinclair et al., 2004) reinforcing the importance of HIV testing. Second, HIV care and antiretroviral (ART) treatment reduces viral load in those who are HIV positive, thereby decreasing viremia and consequently the risk of HIV transmission. Thus, having limited access to HIV services may deepen racial disparities in HIV among black/Hispanic IDUs, and their communities. Therefore, lack of consideration of access to care and services when determining effective HIV prevention strategies will likely lead to suboptimal results.
Syringe exchange programs (SEPs) have overwhelmingly demonstrated effectiveness in reducing HIV transmission among IDUs, and are largely responsible for the overall decline in HIV prevalence among IDUs in NYC. Access to SEPs has also been associated with reduced drug use (Vlahov & Junge, 1998; Watters et al., 1994), decreased incidence and prevalence of HIV and other blood-borne infections (Des Jarlais, et al. 2000; Des Jarlais, et al., 2009; MacDonald & Law, 2003), improved access to HIV prevention programs, lower rates of criminal activity, less needle sharing and other high risk injection behaviors, (Des Jarlais et al., 1996; Groseclose et al., 1995) and greater entry and retention in drug user treatment programs (Strathdee, 2006). While successful in driving down the HIV epidemic among IDUs, there have been barriers identified that directly relate to the inability of SEPs to close the racial gap in HIV. For example, consistent reports from other urban centers in the northeast and west coast have identified structural barriers accessing SEPs such as police harassment, and criminal arrests (Bluthenthal et al., 1997; Cooper et al., 2009b; Rich et al., 1999). Given the disproportionate rates of arrest and incarceration experienced by blacks and Hispanics, these subgroups are likely to be most affected by these types of structural barriers (Galea & Vlahov, 2002), and therefore likely to perpetuate HIV disparities. Thus, structural intervention strategies that include targeting the police force with education and training on the legality of harm reduction programs for IDUs (namely, syringe access programs), and addressing the inappropriateness of criminalizing drug use and misuse as opposed to treating it as a public health problem may have a direct and positive impact on access to SEPs in the black and Hispanic community.
In 2000, New York State legislators recently passed a law allowing syringes to be obtained without a prescription either through pharmacies or healthcare providers known as the New York State Expanded Syringe Access Program or ESAP. Research has consistently shown low rates of pharmacy syringe access among black and Hispanic IDUs (Bluthenthal et al., 1998; Cooper et al., 2009b, Cotton-Oldenburg et al., 2001; Valleroy et al., 1995). Our recent work found that these racial/ethnic disparities in pharmacy use were likely explained by social factors other than one’s race/ethnicity (Center for Urban Epidemiologic Studies, 2003), namely various types of and social settings within which discrimination occurred. For example, past experience of any type of discrimination or within any setting where one perceived being discriminated against based on race was independently associated with a lack of pharmacy use. Given that ESAP legislation prohibits pharmacists from advertising syringe sales in their pharmacies through ESAP, it is likely that pharmacists’ participation status is unknown to an IDU syringe customer until they enter the pharmacy and ask to purchase a syringe without a prescription. This structural barrier may decrease pharmacy use particularly among black/Hispanic drug users who may not feel comfortable engaging a pharmacist due to fear of mistreatment or stigmatization, particularly if they had been discriminated against in the past. There is no evidence that would indicate that pharmacists have mistreated drug users who have attempted to purchase syringes or that such mistreatment can be distinguished by race/ethnicity (Valleroy et al., 1995), and in this particular study no significant interactions persisted with respect to race/ethnicity and race discrimination; however further investigation is needed to more confidently explore these potential plausible interactions.
This same analysis also documented a positive association between police discrimination and higher likelihood of pharmacy use. While at face value paradoxical, this is consistent with previously documented behavior patterns. Rich and colleagues found that one of the major obstacles to participation in SEPs was fear of being identified as an IDU and fear of police harassment (Rich et al., 1999). Since participation in SEPs draws attention to and identifies individuals as IDUs, it is plausible that a subgroup of IDUs who had previous negative experiences with police would be more likely to obtain syringes through pharmacies since entering and exiting a pharmacy is not likely to identify someone as an IDU. However, this explanation has not been empirically shown and therefore warrants further investigation. All in all, what is most important about these findings is the clear importance of social structural factors that are directly or indirectly related to one’s race/ethnicity and therefore taking one’s social context into account may be what is needed to eliminate the problem of racial disparities.
HIV Intervention Strategies to Eliminate Racial Disparities in HIV among IDUs
Early in the epidemic, many (mostly behavioral) interventions have been suggested and targeted to IDUs (Friedman et al.,1992), surprisingly few have included sufficient numbers of black and Hispanic IDUs and/or showed empirical evidence of effectiveness in eliminating racial disparities in HIV.
Individual/behavioral interventions
An intervention conducted by Sterk and colleagues, targeted black, HIV negative, IDU women with a 3-arm trial: (1) enhanced motivation intervention (MI), (2) enhanced negotiation intervention (NI), and (3) NIDA standard intervention (Sterk et al., 2003). The two intervention arms (MI and NI) were grounded in theory and based on in-depth formative research. The trial was successful in reducing both sexual and injection risk behaviors. This intervention was also conducted among a majority black IDU population, was culturally appropriate and gender-tailored, and included issues related to the impact of race and gender on HIV risk behaviors. Three interventions have targeted Puerto Rican IDUs living in Puerto Rico and/or in the mainland United States. Among Puerto Rican IDUs in Hartford, Dushay and colleagues implemented a two-arm intervention: (1) a control arm which consisted of a standard NIDA intervention and (2) an enhanced arm which used Puerto Rican staff to address HIV/AIDS and its relation with family and gender roles in the Puerto Rican community (Dushay et al., 2001). Although there were no significant differences between the two arms in HIV risk behaviors, injection and sexual risk behaviors did decrease over time. In a second large-scale randomized controlled trial (RCT) of IDUs in Puerto Rico (n=1866), participants in the enhanced intervention attended three educational group sessions on HIV risk, compared to a standard community outreach program (Colon et al.,1993). Participants reduced risk behavior; however, levels of risk reduction did not significantly differ across arms. The third Hispanic-targeted two-arm RCT was conducted by Robles and colleagues in Puerto Rico. Their successful enhanced intervention consisted of combined counseling, case management, and motivational interviewing to encourage IDUs to reduce risk and/or enter drug treatment (Robles et al., 2004). Participants in the enhanced intervention were significantly less likely to continue drug injection and share syringes and more likely to enter drug user treatment. It is noteworthy that promoting entrance addresses a structural factor (drug user treatment access); however, the intervention did not “target” drug user treatment facilities and can therefore not be considered a structural intervention.
Socio contextual interventions
One of the few interventions that have targeted black or Hispanic IDUs or demonstrated impact specifically among black or Hispanic IDUs includes a social network-based intervention conducted by Latkin and colleagues (Latkin, Sherman, & Knowlton, 2003). Using a peer outreach model, the authors trained IDUs to be peer AIDS outreach educators and during their training, individual risk, sexual partner risk, and community risk were emphasized. Trained peer outreach educators were assessed on the risk reduction conversations which they had with other drug users, sex partners, friends and family. Those in the intervention arm were 3 times more likely to report injection risk reduction and 4 times more likely to report sexual risk reduction. In addition to the program effectiveness, the intervention targeted a majority black IDU population.
Weeks and colleagues conducted a similar social network-based intervention using “Peer Health Advocates” (PHAs) to deliver a modular HIV, hepatitis, and STI prevention intervention to primarily black and Hispanic IDUs and crack cocaine users (Weeks et al., 2009). Comparing baseline to 6-month follow-up demonstrated risk reduction among all study participants associated with health advocacy action delivered by PHAs as well as a significant relationship between exposure to the PHA-delivered intervention activities and risk reduction. While this intervention was absent of a randomized design and a control group, this study provided additional evidence of the utility of social networks (particularly informational supportive networks) and its effectiveness in potentially reducing racial disparities in highly burdened communities.
Structural Interventions
Schilling and colleagues conducted a non-RCT street outreach intervention targeting black and Hispanic IDUs in high-risk neighborhoods of the South Bronx (Schilling et al., 2000). In addition to standard HIV prevention street outreach, intervention neighborhoods were provided with referral specialists who made appointments to drug treatment services and accompanied IDUs to their first visit lending to a more direct structural intervention strategy. However, injection and sexual risk behaviors decreased among IDUs in both intervention and control communities, with no significant effect in intervention neighborhoods. These findings do not necessarily negate the importance of structural factors but simply fall short when addressing issues related to drug user treatment and lack of retention and successful treatment outcomes observed among black drug users compared to their white counterparts.
Finally, our research team implemented a community-based intervention among primarily black and Hispanic IDUs in East and Central Harlem (referred to as “Harlem” hereafter) with the specific goal of addressing racial disparities in pharmacy syringe access (Fuller et al., 2007). Using a community-based participatory research approach, a multilevel pre-/post- intervention design was implemented in Harlem at three levels: IDUs (individual), pharmacists (individual and structural), and community residents (individual and structural) using the South Bronx as the comparison community. For each target population, educational materials detailing the importance of syringe access in reducing HIV risk in the community were disseminated. This intervention was based on the premise that by creating a more positive and socially accepting environment for syringe access that increased pharmacy use, particularly black drug users who demonstrated the lowest rates of use, would result. Among pharmacists and community residents, an increase in positive attitudes and a decrease in negative attitudes toward drug users and syringe access were observed in the intervention community with no change in the comparison community. Among IDUs, a decrease in syringe re-use was observed and specifically among black IDUs, an increase in pharmacy use was observed in the intervention community with no change in the comparison community.
Conclusion
One of the most important lessons we have learned from the available HIV prevention research is that racial/ethnic disparities in HIV prevalence among IDUs are not explained by individual risk behaviors, thus interventions that focus on reducing risk behaviors will not have an impact on reducing the racial/ethnic HIV disparities. Each of the previously reported successful intervention strategies incorporated either social networks and/or structural factors in order to have an impact on individual risk behavior. However, additional intervention research is needed that tests other multilevel and/or structural interventions aimed at those who continue to be at high risk because of the risk attributed to their social environment. While high HIV/AIDS mortality among black and Hispanic IDUs continues to persist, there is still opportunity to prevent new HIV infection among black and Hispanic IDUs and increase access to HIV prevention, care and treatment services to help decrease risk of transmission as well as save and extend the lives of those currently infected.
Glossary
- disease burden
the impact of a health problem in an area measured by financial cost, mortality, morbidity, or other indicators
- risk behaviors
behaviors that increase an individual’s risk for a negative health outcome
- racial disparities
inequality or difference between two or more races
- structural factors
economic, social, policy, and systems factors that impact individual behavior
- structural interventions
interventions that address structural factors
Biographies

Silvia Amesty is a family physician at the New York Presbyterian Hospital, on faculty at Columbia University, College of Physicians and Surgeons, Mailman School of Public Health, and a research fellow with the Center of Urban Epidemiologic Studies at the New York Academy of Medicine. She was educated at the University of Pennsylvania (BA, MSEd), Temple University (MD), and Columbia University (MPH). She is a board certified Family Medicine physician, and received residency training at Beth Israel Medical Center/The Institute for Urban Family Health in New York City. She has worked in the Washington Heights and Harlem communities for several years as a clinician, and has been a primary care HIV provider; after completing her fellowship training in academic family medicine.

Alexis Rivera is a Research Coordinator with the Center for Urban Epidemiologic Studies at the New York Academy of Medicine. She obtained her master's degree in the Department of Epidemiology at the Mailman School of Public Health at Columbia University. Her research interests include HIV prevention interventions, racial disparities, Latino health, and urban health

Crystal Fuller is an Associate Professor of Clinical Epidemiology at Columbia University, Mailman School of Public Health and an infectious disease epidemiologist with Center for Urban Epidemiologic Studies at the New York Academy of Medicine. She completed her MPH at Tulane University School of Public Health and her Ph.D. at Johns Hopkins University, School of Public Health in the Infectious Disease Epidemiology Program. Her research focuses on the effect of high-risk behavior (particularly social networks), and other social determinants (individual and contextual) on initiation of injection drug use, subsequent risk behavior, and early transmission of blood-borne pathogens among drug users in New York City.
References
- Absalon J, Fuller CM, Ompad DC, Blaney S, Koblin B, Galea S, Vlahov D. Gender differences in sexual behaviors, sexual partnerships and HIV among drug users in New York City. AIDS & Behavior. 2006;10:707–715. doi: 10.1007/s10461-006-9082-x. [DOI] [PubMed] [Google Scholar]
- Andersen R, Bozzette S, Shapiro M, St CP, Morton S, Crystal S, Goldman D, Wenger N, Gifford A, Leibowitz A, Asch S, Berry S, Nakazono T, Heslin K, Cunningham W. Access of vulnerable groups to antiretroviral therapy among persons in care for HIV disease in the United States. HCSUS Consortium. HIV Cost and Services Utilization Study. Health Services Research. 2000;35:389–416. [PMC free article] [PubMed] [Google Scholar]
- Andrulis DP, Weslowski VB, Hintz E, Spolarich AW. Comparisons of hospital care for patients with AIDS and other HIV-related conditions. Journal of the American Medical Association. 1992;267:2482–2486. [PubMed] [Google Scholar]
- Bluthenthal RN, Kral AH, Erringer EA, Edlin BR. Use of an illegal syringe exchange and injection-related risk behaviors among street-recruited injection drug users in Oakland, California, 1992 to 1995. Journal of Acquired Immune Deficiency Syndrome & Human Retrovirology. 1998;18(5):505–511. doi: 10.1097/00042560-199808150-00013. [DOI] [PubMed] [Google Scholar]
- Bluthenthal RN, Kral AH, Lorvick J, Warters JK. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Medical Anthropology. 1997;18:61–83. doi: 10.1080/01459740.1997.9966150. [DOI] [PubMed] [Google Scholar]
- Broz D, Ouellet LJ. Racial and ethnic changes in heroin injection in the United States: Implications for the HIV/AIDS epidemic. Drug and Alcohol Dependence. 2008;94:221–233. doi: 10.1016/j.drugalcdep.2007.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celentano DD, Munoz A, Cohn S, Vlahov D. Dynamics of behavioral risk factors for HIV/AIDS: a 6-year prospective study of injection drug users. Drug and Alcohol Dependence. 2001;61:315–322. doi: 10.1016/s0376-8716(00)00154-x. [DOI] [PubMed] [Google Scholar]
- Celentano DD, Vlahov D, Cohn S, Shadle VM, Obasanjo O, Moore RD. Self-reported antiretroviral therapy in injection drug users. Journal of the American Medical Association. 1998;280:544–546. doi: 10.1001/jama.280.6.544. [DOI] [PubMed] [Google Scholar]
- Center for Urban Epidemiologic Studies, New York Academy of Medicine. New York State Expanded Syringe Access Demonstration Program Evaluation: Evaluation report to the Governor and the New York State Legislation. New York, NY: New York Academy of Medicine; 2003. [Google Scholar]
- Centers for Disease Control and Prevention. Drug-associated HIV transmission continues in the United States. Atlanta, GA: Center for Disease Control and Prevention, Department of Health and Human Services; 2002. [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report. 2007;Volume 19 [Google Scholar]
- Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. Morbidity and Mortality Weekly Report. 2006;55(14):1–17. [PubMed] [Google Scholar]
- Colon HM, Robles RR, Freeman D, Matos T. Effects of a HIV risk reduction education program among injection drug users in Puerto Rico. Puerto Rico Health Sciences Journal. 1993;12:27–34. [PubMed] [Google Scholar]
- Committee on the Prevention of HIV Infection Among Injection Drug Users in High Risk Countries. Preventing HIV Infection Among Injection Drug Users in High Risk Countries: An Assessment of the Evidence. Washington, DC: Institute of Medicine; 2006. [Google Scholar]
- Cooper HL, Bossak B, Tempalski B, DesJarlais DC, Friedman SR. Geographic approaches to quantifying the risk environment: drug-related law enforcement and access to syringe exchange programmes. International Journal of Drug Policy. 2009a;20(3):217–226. doi: 10.1016/j.drugpo.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Bossak B, Tempalski B, Friedman SR, Des Jarlais DC. Temporal trends in spatial access to pharmacies that sell over-the-counter syringes in New York City health districts: relationship to local racial/ethnic composition and need. Journal of Urban Health. 2009b doi: 10.1007/s11524-009-9399-7. Epub ahead of print. Accessed online on November 23, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotten-Oldenburg NU, Carr P, DeBoer JM, Collison EK, Novotny G. Impact of pharmacy-based syringe access on injection practices among injecting drug users in Minnesota, 1998 to 1999. Journal of Acquired Immune Deficiency Syndrome. 2001;27:183–192. doi: 10.1097/00126334-200106010-00014. [DOI] [PubMed] [Google Scholar]
- Cronquist A, Edwards V, Galea S, Latka M, Vlahov D. Health care utilization among young adult injection drug users in Harlem, New York. Journal of Substance Abuse. 2001;13:17–27. doi: 10.1016/s0899-3289(01)00073-6. [DOI] [PubMed] [Google Scholar]
- Delgado M, Lundgren LM, Deshpande A, Lonsdale J, Purington T. The association between acculturation and needle sharing among Puerto Rican injection drug users. Evaluation and Program Planning. 2008;31:83–91. doi: 10.1016/j.evalprogplan.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Deren S, Kang SY, Colón HM, Andia JF, Robles RR, Oliver-Velez D, Finlinson A. Migration and HIV Risk Behaviors: Puerto Rican Drug Injectors in New York City and Puerto Rico. American Journal of Public Health. 2003;93(5):812–816. doi: 10.2105/ajph.93.5.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deren S, Kang SY, Colon HM, Robles RR. The Puerto Rico-New York airbridge for drug users: Description and relationship to HIV risk behaviors. Journal of Urban Health. 2007;84(2):243–254. doi: 10.1007/s11524-006-9151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Arasteh K, Hagan H, McKnight C, Perlman D, Friedman S. Persistence and change in disparities in HIV infection among injection drug users in New York City after large-scale syringe exchange programs. American Journal of Public Health. 2009;99(Suppl 2):S445–S451. doi: 10.2105/AJPH.2008.159327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Marmor M, Friedmann P, Titus S, Aviles E, Deren S, Torian L, Glebatis D, Murrill C, Monterroso E, Friedman SR. HIV incidence among injection drug users in New York City, 1992-1997: Evidence for a declining epidemic. American Journal of Public Health. 2000;90(3):352–359. doi: 10.2105/ajph.90.3.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Marmor M, Paone D, Titus S, Shi Q, Perlis T, Jose B, Friedman SR. HIV incidence among injecting drug users in New York City syringe-exchange programmes. Lancet. 1996;348:987–991. doi: 10.1016/s0140-6736(96)02536-6. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC, Perlis T, Arasteh K, Hagan H, Milliken J, Braine N, Yancovitz S, Mildvan D, Perlman DC, Maslow C, Friedman SR. “Informed altruism” and “partner restriction” in the reduction of HIV infection in injecting drug users entering detoxification treatment in New York City, 1990-2001. Journal of Acquired Immune Deficiency Syndrome. 2004;35(2):158–166. doi: 10.1097/00126334-200402010-00010. [DOI] [PubMed] [Google Scholar]
- Diaz T, Vlahov D, Greenberg B, Cuevas Y, Garfein R. Sexual orientation and HIV infection prevalence among young Latino injection drug users in Harlem. Journal of Women’s Health & Gender-based Medicine. 2001;10(4):371–380. doi: 10.1089/152460901750269698. [DOI] [PubMed] [Google Scholar]
- Dushay RA, Singer M, Weeks MR, Rohena L, Gruber R. Lowering HIV risk among ethnic minority drug users: Comparing culturally targeted intervention to a standard intervention. American Journal of Drug and Alcohol Abuse. 2001;27:501–524. doi: 10.1081/ada-100104515. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Morton SC. Identifying adolescents at risk for hard drug use: racial/ethnic variations. Journal of Adolescent Health. 1999;25(6):382–395. doi: 10.1016/s1054-139x(98)00144-x. [DOI] [PubMed] [Google Scholar]
- Estrada AL. Health disparities among African-American and Hispanic drug injectors--HIV, AIDS, hepatitis B virus and hepatitis C virus: a review. AIDS. 2003;19(Suppl 3):S47–S52. doi: 10.1097/01.aids.0000192070.95819.7c. [DOI] [PubMed] [Google Scholar]
- Freeman RC, Williams ML, Saunders LA. Drug use, AIDS knowledge, and HIV risk behaviors of Cuban-, Mexican-, and Puerto-Rican- born drug injectors who are recent entrants into the United States. Substance Use and Misuse. 1999;34(13):1765–1793. doi: 10.3109/10826089909039426. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Cooper HL, Osborne AH. Structural and social contexts of HIV risk among African Americans. American Journal of Public Health. 2009;99(6):1002–1009. doi: 10.2105/AJPH.2008.140327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Kottiri BJ, Neaigus A, Curtis R, Vermund SH, Des Jarlais DC. Network-related mechanisms may help explain long-term HIV-1 seroprevalence levels that remain high but do not approach population-group saturation. American Journal of Epidemiology. 2000;152(10):913–922. doi: 10.1093/aje/152.10.913. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Neaigus A, Des Jarlais DC, Sotheran JL, Woods J, Sufian M, Stepherson B, Sterk C. Social intervention against AIDS among injecting drug users. British Journal of Addiction. 1992;87(3):393–404. doi: 10.1111/j.1360-0443.1992.tb01940.x. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Neaigus A, Jose B, Curtis R, Goldstein M, Ildefonso G, Rothenberg RB, Des Jarlais DC. Sociometric risk networks and risk for HIV infection. American Journal of Public Health. 1997;87(8):1289–1296. doi: 10.2105/ajph.87.8.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller CM, Absalon J, Ompad DC, Nash D, Koblin B, Blaney S, Galea S, Vlahov D. A comparison of HIV seropositive and seronegative young adult heroin- and cocaine-using men who have sex with men in New York City, 2000-2003. Journal of Urban Health. 2005;82(1):i51–i61. doi: 10.1093/jurban/jti024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller CM, Borrell LN, Latkin CA, Galea S, Ompad DC, Strathdee SA, Vlahov D. Effects of race, neighborhood, and social network on age at initiation of injection drug use. American Journal of Public Health. 2005;95(4):689–695. doi: 10.2105/AJPH.2003.02178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller CM, Galea S, Blaney S, Ompad DC, Deren S, Des Jarlais D, Vlahov D. Explaining the relationship between race/ethnicity and pharmacy purchased syringes among injection drug users in New York City. Ethnicity & Disease. 2004;14:589–595. [PubMed] [Google Scholar]
- Fuller CM, Galea S, Caceres W, Blaney S, Sisco S, Vlahov D. Multilevel community-based intervention to increase access to sterile syringes among injection drug users through pharmacy sales in New York City. American Journal of Public Health. 2007;97(1):117–112. doi: 10.2105/AJPH.2005.069591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller CM, Vlahov D, Arria AM, Ompad DC, Garfein R, Strathdee SA. Factors associated with adolescent initiation of injection drug use. Public Health Reports. 2001;116(Suppl 1):136–145. doi: 10.1093/phr/116.S1.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller CM, Vlahov D, Ompad DC, Shah N, Arria A, Strathdee SA. High-risk behaviors associated with transition from illicit non-injection to injection drug use among adolescent and young adult drug users: a case-control study. Drug and Alcohol Dependence. 2002;66:189–198. doi: 10.1016/s0376-8716(01)00200-9. [DOI] [PubMed] [Google Scholar]
- Galea S, Vlahov D. Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public Health Reports. 2002;117(Suppl 1):S135–S145. [PMC free article] [PubMed] [Google Scholar]
- Golub A, Johnson BD. Variation in youthful risks of progression from alcohol and tobacco to marijuana and to hard drugs across generations. American Journal of Public Health. 2001;91:225–232. doi: 10.2105/ajph.91.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groseclose SL, Weinstein B, Jones TS, Valleroy LA, Fehrs LJ, Kassler WJ. Impact of increased legal access to needles and syringes on practices of injecting-drug users and police officers—Connecticut, 1992-1993. Journal of Acquired Immune Deficiency Syndrome & Human Retrovirology. 1995;10(1):82–89. [PubMed] [Google Scholar]
- Harawa NT, Greenland S, Bingham TA, Johnson DF, Cochran SD, Cunningham WE, Celentano DD, Koblin BA, LaLota M, Mackellar DA, McFarland W, Shehan D, Stoyanoff S, Thiede H, Torian L, Valleroy LA. Associations of Race/Ethnicity With HIV Prevalence and HIV-Related Behaviors Among Young Men Who Have Sex With Men in 7 Urban Centers in the United States. Journal of Acquired Immune Deficiency Syndrome. 2004;35(5):526–536. doi: 10.1097/00126334-200404150-00011. [DOI] [PubMed] [Google Scholar]
- Holmberg SD. The estimated prevalence and incidence of HIV in 96 large US metropolitan areas. American Journal of Public Health. 1996;86:642–654. doi: 10.2105/ajph.86.5.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kottiri BJ, Friedman SR, Neaigus A, Curtis R, Des Jarlais D. Risk networks and racial/ethnic differences in the prevalence of HIV infection among injection drug users. Journal of Acquired Immune Deficiency Syndrome. 2002;30:95–104. doi: 10.1097/00042560-200205010-00013. [DOI] [PubMed] [Google Scholar]
- Kral AH, Lorvick J, Edlin BR. Sex- and drug-related risk among populations of younger and older injection drug users in adjacent neighborhoods in San Francisco. Journal of Acquired Immune Deficiency Syndrome. 2000;24:162–167. doi: 10.1097/00126334-200006010-00011. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Kuramoto SJ, Davey-Rothwell MA, Tobin KE. Social norms,social networks, and HIV risk behavior among injection drug users. AIDS & Behavior. 2009 doi: 10.1007/s10461-009-9576-4. Epub ahead of print, Accessed online on November 18, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychology. 2003;22(4):332–339. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- MacDonald M, Law M. Effectiveness of needle and syringe programmes for preventing HIV transmission. International Journal of Drug Policy. 2003;14:353–357. [Google Scholar]
- Mauskopf J, Turner BJ, Markson LE, Houchens RL, Fanning TR, McKee L. Patterns of ambulatory care for AIDS patients, and association with emergency room use. Health Services Research. 1994;29:489–510. [PMC free article] [PubMed] [Google Scholar]
- Moore RD, Hidalgo J, Bareta JC, Chaisson RE. Zidovudine therapy and health resource utilization in AIDS. Journal of Acquired Immune Deficiency Syndrome. 1994;7:349–354. [PubMed] [Google Scholar]
- National Institutes on Drug Abuse. Principles of HIV prevention in drug-using populations. National Institutes on Drug Abuse. Bethesda, MD: Department of Health and Human Development; 2000. [Google Scholar]
- Neaigus A, Friedman SR, Jose B, Goldstein MF, Curtis R, Ildefonso G, Des Jarlais DC. High-risk personal networks and syringe sharing as risk factors for HIV infection among new drug injectors. Journal of Acquired Immune Deficiency Syndrom and Human Retrovirology. 1996;11(5):499–509. doi: 10.1097/00042560-199604150-00011. [DOI] [PubMed] [Google Scholar]
- NYC HIV/AIDS Annual Surveillance Statistics. HIV Epidemiology and Field Services Program. [Accessed October 26, 2009];New York City Department of Health and Mental Hygiene. 2007 [Google Scholar]
- Ompad DC, Fuller CM, Galea S, Del Vecchio, Vlahov D. HIV risk behaviors among young female drug users who have sex with women in New York City; Oral Presentation. Paper presented at the XV International Conference on AIDS; Bangkok, Thailand. 2004. [Google Scholar]
- Ompad DC, Fuller CM, Galea S, Wu Y, Nash D, Benjamin E, Vlahov D. Sexual risk is associated with HIV among injection and non-injection drug users: Implications for intervention strategies; Paper presented at the XV International Conference on AIDS; Bangkok, Thailand. 2004. [Google Scholar]
- Rich JD, Strong L, Towe CA, McKenzie M .Obstacles to needle exchange participation in Rhode Island. Journal of Acquired Immune Deficiency Syndrome. 1999;21:396–400. [PubMed] [Google Scholar]
- Robles RR, Matos TD, Colon HM, Marrero CA, Reyes JC. Effects of HIV testing and counseling on reducing HIV risk behavior among two ethnic groups. Drugs and Society. 1996;9:173–184. doi: 10.1300/J023v09n01_10. [DOI] [PubMed] [Google Scholar]
- Robles RR, Reyes JC, Colon HM, Sahai H, Marrero CA, Matos TD, Calderon JM, Shepard EW. Effects of combined counseling and case management to reduce HIV risk behaviors among Hispanic drug injectors in Puerto Rico. Journal of Substance Abuse Treatment. 2004;27(2):145–152. doi: 10.1016/j.jsat.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Wilson WJ. Toward a theory of race, crime and urban inequality. In: Hagan J, Petersen RD, editors. Crime and Inequality. Stanford, Calif: Stanford University Press; 1995. pp. 37–54. [Google Scholar]
- Schilling RF, Fernando D, Fontdevila J, El-Bassel N. HIV risk reduction among injection drug users: Explaining the lack of anticipated outcomes in a community-level controlled comparison study. Evaluation and Program Planning. 2000;23:301–313. [Google Scholar]
- Sinclair M, Bor R, Evans A, Glass D, Levitt D, Johnson MA. The sociodemographic profile, risk categories and prevalence of HIV infection among people attending a London same-day testing clinic, 2000-2001. International Journal of STDs and AIDS. 2004;15:33–37. doi: 10.1258/095646204322637236. [DOI] [PubMed] [Google Scholar]
- Solomon L, Frank R, Vlahov D, Astemborski J. Utilization of health services in a cohort of injection drug users with known HIV-1 serostatus. American Journal of Public Health. 1991;81:1285–1290. doi: 10.2105/ajph.81.10.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Piette J, Mor V, Wachtel TJ, Fleishman J, Mayer KH, Carpenter CC. Differences in access to zidovudine (AZT) among symptomatic HIV-infected persons. Journal of General Internal Medicine. 1991;6:35–40. doi: 10.1007/BF02599388. [DOI] [PubMed] [Google Scholar]
- Sterk CE, Theall KP, Elifson KW, Kidder D. HIV risk reduction among African-American women who inject drugs: a randomized controlled trial. AIDS & Behavior. 2003;7(1):73–86. doi: 10.1023/a:1022565524508. [DOI] [PubMed] [Google Scholar]
- Strathdee S. Facilitating entry into drug treatment among injection drug users referred from a needle exchange program: Results from a community-based behavioral intervention trial. Drug and Alcohol Dependence. 2006;83(3):225–232. doi: 10.1016/j.drugalcdep.2005.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Palepu A, Cornelisse PG, Yip B, O'Shaughnessy MV, Montaner JS, Schechter MT, Hogg RS. Barriers to use of free antiretroviral therapy in injection drug users. Journal of the American Medical Association. 1998;280:547–549. doi: 10.1001/jama.280.6.547. [DOI] [PubMed] [Google Scholar]
- Sumartojo E. Structural factors in HIV prevention: concepts, examples, and implications for research. AIDS. 2000;(Suppl 1):S3–S10. doi: 10.1097/00002030-200006001-00002. [DOI] [PubMed] [Google Scholar]
- Turner BJ, Markson LE, McKee LJ, Houchens R, Fanning T. Health care delivery, zidovudine use, survival of women and men with AIDS. Journal of Acquired Immune Deficiency Syndrome. 1994a;7:1250–1262. [PubMed] [Google Scholar]
- Turner BJ, McKee L, Fanning T, Markson LE. AIDS specialist versus generalist ambulatory care for advanced HIV infection and impact on hospital use. Medical Care. 1994b;32:902–916. doi: 10.1097/00005650-199409000-00002. [DOI] [PubMed] [Google Scholar]
- Valleroy LA, Weinstein B, Jones TS, Groseclose SL, Rolfs RT, Kassler WJ. Impact of increased legal access to needles and syringes on community pharmacies’ needle and syringe sales-Connecticut, 1992-1993. Journal of Acquired Immune Deficiency Syndrome & Human Retrovirology. 1995;10:73–81. [PubMed] [Google Scholar]
- Vlahov D, Junge B. The role of needle exchange programs in HIV prevention. Public Health Reports. 1998;113(Suppl 1):75–80. [PMC free article] [PubMed] [Google Scholar]
- Watters JK, Estilo MJ, Clark GL, Lorvick J. Syringe and needle exchange as HIV/AIDS prevention for injection drug users. Journal of the American Medical Association. 1994;271:115–120. [PubMed] [Google Scholar]
- Weeks MR, Li J, Dickson-Gomez J, Convey M, Martinez M, Radda K, Clair S. Outcomes of a peer HIV prevention program with injection drug and crack users: the Risk Avoidance Partnership. Substance Use and Misuse. 2009;44(2):253–281. doi: 10.1080/10826080802347677. [DOI] [PMC free article] [PubMed] [Google Scholar]