Summary
Leukocyte derived pro-inflammatory mediators could be involved in tendon healing and scar formation. Hence, the effect of autologous leukocytes (PBMCs, peripheral blood mononuclear cells and neutrophils) on primary rabbit Achilles tenocytes gene expression was tested in insert assisted co-cultures.
Subsequently, tenocytes gene expression of extra-cellular matrix (ECM) components (type I collagen, decorin, fibronectin), the cell-ECM receptor β1-integrin, the angiogenic factor myodulin, ECM degrading matrix-metalloproteinase (MMP)1 and pro-inflammatory cytokines (interleukin [IL]-1β, tumour necrosis factor [TNFα] and IL-6) was analysed.
The only significant effect of leukocytes on tenocytes ECM genes expression was a suppression of type I collagen by neutrophils combined with TNFα stimulation. The same effect could be observed analysing the β1-integrin and myodulin gene expression. However, PBMCs up-regulated significantly cytokine and MMP1 gene expression in tenocytes. These in vitro results suggest that mononuclear cells could present an exogenic stimulus for the induction of pro-inflammatory and catabolic mediators in tendon.
Keywords: cytokines, IL-1β, leukocytes, myodulin, tendon, TNFα
Introduction
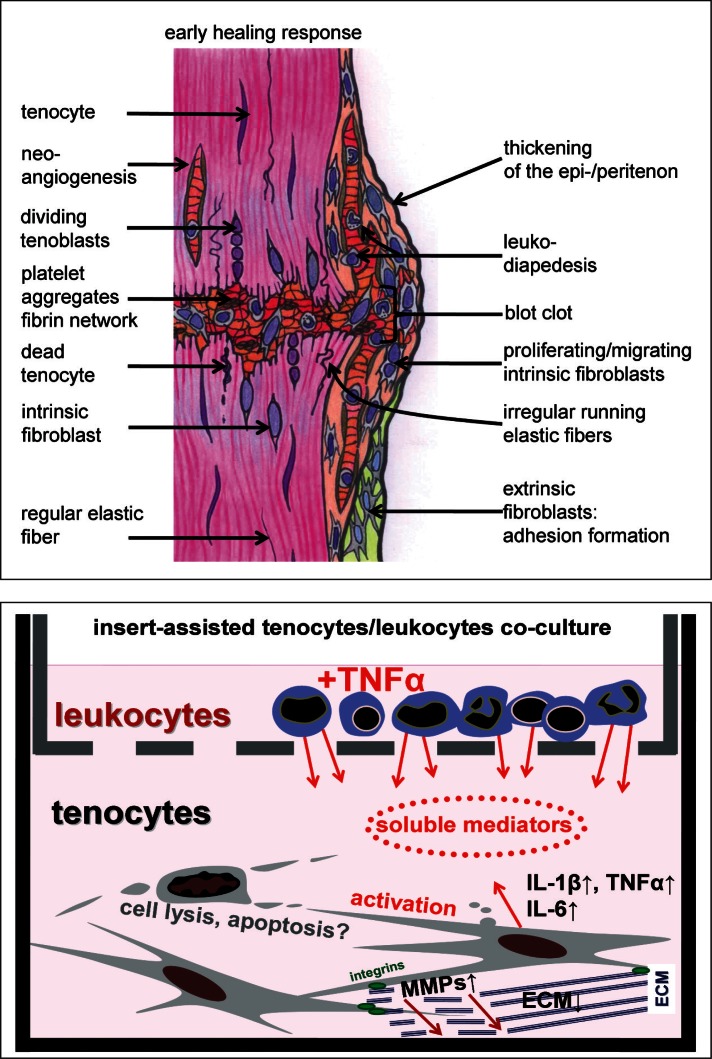
Tendon rupture and injury leads to a posttraumatic inflammatory response characterized by the presence of multiple pro-inflammatory cytokines such as IL-1β and TNFα as well as cell damage, cell loss and ECM disintegration at the site of tissue injury (1). Additionally blood clot formation, invasion of extrinsic cells and proliferation within the tendon rupture callus, ECM neo-synthesis and angiogenesis can be observed during tendon healing (2) (Fig. 1A). The main ECM component in tendon is type I collagen. The most important proteoglycan in tendon is decorin (3). Fibronectin is an ECM glycoprotein which is expressed by tenocytes involved in their adherence to the ECM (4). Fibronectin and integrin expression is up-regulated during tendon healing (5). The cell-ECM receptor β1-integrin mediate the cell-ECM interaction as an important pre-requisite for cell survival as shown in another connective tissue cell species, the chondrocytes (6, 7). During tendon healing a neoangiogenesis can be observed in the forming granulation tissue (8). Myodulin is a proangiogenic factor, which seems to promote blood vessel proliferation in the region of the myotendinous junction (9). To sustain loading and mediate regular function a remodelling of the rupture callus is necessary (2). Callus remodelling in injured tendons requires more than three months in the rabbit model (8). Remodelling is mediated by ECM degrading enzymes such as MMP1. Particularly MMP1 which is well known to be able to cleave type I collagen has been shown in tendon and cultured tenocytes (10).
Figure 1A–B.
Simplified scheme depicturing aspects of early tendon healing and tenocytes/leukocytes co-culturing using insert culture.
The impact of the inflammatory response on the tendon healing outcome is still unclear. TNFα and IL-1β stimulate tenocytes in vitro to produce further pro- and anti-inflammatory cytokines e.g. IL-1β, TNFα, IL-6 and IL-10 and ECM degrading enzymes such as MMPs (11,12). This suggests an autoactivation of tenocytes by exogenic cytokines. However, apart from IL-1β and TNFα multiple other cytokines are released by leukocytes. Krause et al., (13) reported recently that e.g. IL-2, IL-8, IL-10, IL-17, TNFα, interferon (IFN)-γ, and granulocyte-macrophage colony stimulating factor (GM-CSF) are produced by PBMCs. Some of them might probably be involved in tendon healing. The cytokine concentration produced by leukocytes might differ from that usually used in in vitro experiments with isolated recombinant cytokines. PBMCs consist of monocytes and several lymphocyte subpopulations.
Despite the stimulatory effect of platelets and their extracts on tendon healing is meanwhile intensely discussed (14–16), the effect of exogenic pro-inflammatory mediators such as cytokines released by leukocytes on tenocytes has not yet been studied in tendon tissue and tenocytes at all. Hence, this study was undertaken to assess the direct interactive response of Achilles tenocytes to leukocyte-derived soluble mediators in an indirect co-culture setting.
Materials and Methods
Tenocytes isolation and culture
Rabbit primary Achilles tenocytes were isolated as described previously (17,18) from the midsubstance of seven Achilles tendons of healthy one year-aged adult female donors post mortem. This study was approved by the Berlin review board for experiments with animals. The identity of the isolated tenocytes was confirmed by immunolabelling of tenomodulin and tenascin C. Cultures were grown at 37°C in a humidified atmosphere with 5% CO2 and the growth medium was changed every three days. Growth medium for tenocyte culture consisted of Ham’s F-12/Dulbecco’s modified Eagle’s medium (50/50, Biochrom-Seromed, Munich, Germany) containing 10% fetal calf serum (FCS, Biochrom-Seromed), 25 μg/mL ascorbic acid (Sigma-Aldrich, Munich, Germany), 50 IU/mL streptomycin, 50 IU/mL penicillin, 2.5 μg/mL amphotericin B, essential amino acids, L-glutamine (all: Biochrom-Seromed).
Immunofluorescence labelling of tenocytes
Cover slips seeded with tenocytes were fixed in 4% paraformaldehyde, then rinsed in Tris buffered saline (TBS: 0.05 M Tris, 0.015 M NaCl, pH 7.6) before blocked with protease-free donkey serum (5% diluted in TBS) for 30 min at room temperature (RT), rinsed and incubated with the polyclonal goat tenomodulin (Santa Cruz Biotechnology, Inc., USA), monoclonal mouse tenascin C antibody BC-24 (Gene-Tex Inc, Biozol, Eching, Germany), polyclonal rabbit type I collagen antibody (27.5 μg/mL, Acris Antibodies, Herford, Germany) and polyclonal rabbit decorin (0,5 mg/mL, 1:40, Acris, Hiddenhausen, Germany) antibodies in a humidifier chamber overnight at 4°C. Sections were subsequently washed with TBS before incubation with donkey-anti-rabbit-Alexa-Fluor®488 (10 mg/mL, Invitrogen) secondary antibody for 30 min at RT. Negative controls included omitting the primary antibody during the staining procedure. Cell nuclei were counterstained using 4′,6- diamidino-2-phenylindole (DAPI) (0.1 μg/mL, Roche). Cover slips were rinsed several times with TBS, embedded with Fluoromount G (Southern Biotech, Diagnostica, Birmingham, USA) and examined using fluorescence microscopy (Axioskop 40, soft imaging solution, Muenster Carl Zeiss, Jena, Germany). Images were taken using a XC30 camera system (Olympus, Germany).
Isolation of peripheral blood mononuclear cells and granulocytes
7 mL heparinized rabbit whole blood was centrifuged for 10 min at 400 g. 3 mL sedimented blood cells were mixed with 12,5 mL solution B (2% FCS in phosphate buffered saline [PBS], 100 U/mL polymixin B). Resuspended blood cells were added to 7.5 mL Biocoll (Biochrom-Seromed) and sedimented for 30 min at 400 g. The interphase was separated and mixed with 12.5 mL solution B. The cell pellet containing the red blood cells and granulocytes (predominately neutrophils) was used for isolation of the neutrophils (see below). The PBMCs were washed in solution B. To isolate the neutrophils, the pellet was mixed with 40 mL solution B. 6.6 mL dextran was added and the suspension left to form sediment for 1 h. The supernatant was then separated and mixed with solution B, before being centrifuged at 600 g for 10 min. Leukocytes were counted and immediately cryo-preserved until use.
HE staining of tendon, tenocytes and leukocytes
Haematoxylin Eosin (HE) staining were performed using paraffin-sections of tendon, cover slips seeded with tenocytes or cytospines of leukocytes as described previously (8).
Two-chamber co-culture of tenocytes and leukocytes
A two-chamber system was used for co-culturing consisting of 6-well plates and inserts (pore size 0.4 μm) (Beckton Dickinson, Franklin Lakes, USA) (Fig. 1B). For the experiments tenocytes were cultured at 15000/cm2 in 6-well plates for 24 h, subsequently serum-starved (1% FCS containing growth medium) for 2 h. The cryo-preserved autologous leukocytes were gently thawed, pelleted in serum-starved medium and then 4 mio leukocytes, suspended in 1% FCS growth medium per well were added to the insert serving as upper chamber. Some of the co-cultures were stimulated with 10 ng/mL human TNFα (peproTech EC Umkirch, Germany) under similar conditions.
RNA isolation from tenocytes
The insert containing the leukocytes was removed from the 6 well plates. Tenocytes were rinsed with PBS and incubated 5 min with RLT buffer (Qiagen, Hilden, Germany) + 10% mercaptoethanol. Total RNA was isolated using Qiagen RNA isolation mini kit (Qiagen) and the RNA quantity and quality was evaluated using the RNA 6000 Nano assay (Agilent Technologies, Waldbronn, Germany). Reverse transcription was performed using the Quanti Tect Reverse Transcription Kit according to the manufacturer’s instructions (Qiagen).
Messenger RNA analysis by real time detection polymerase chain reaction
Real time detection polymerase chain reaction (RTD-PCR) analyses were performed to obtain quantitative gene expression data. To assess the type I collagen gene expression specific primers for the type I collagen and the house-keeping gene β-actin both obtained from the company Qiagen were used. Specific primers for myodulin, decorin, fibronectin, β1-integrin, IL-1β, TNFα, IL-6, MMP1 and the house-keeping gene glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (3) gene sequences (Tab. 1) in the rabbit were used which derived from Applied Biosystems (ABI), Foster City USA. Type I collagen gene expression was normalized versus β-actin, expression of the other genes versus GAPDH. For RTD PCR, 1 μL aliquots of the cDNA were amplified using RTD-PCR in a 20 μL reaction mixture using the Quantitec Probe RTD-PCR kit (Qiagen) or TaqMan Gene Expression Assay. All assays were performed in an Opticon 1 – Real-Time-Cycler (Opticon™ RTD-PCR, Biorad). The conditions for TaqMan analyses were: 10 min at 90°C, and then for 41 cycles 15 s at 95°C, 30 s at 56°C and followed by 6°C cooling. The lack of primer dimers and the specifity of amplification were further confirmed by efficacy testing using rabbit Achilles tendon cDNA and agarose gel electrophoresis of PCR products all showing a single band of expected size. Relative gene expression levels were normalized versus the housekeeping genes and calculated with the 2−deltaCT method (19).
Table I.
Oligonucleotides used for RTD PCR analysis with rabbit tenocytes cDNA.
| forward/reverse primer | probe/reference | bp | ||
|---|---|---|---|---|
| β-actin | Qia | TGGGACGACATGGAGAA | GCCCCCCTGAACCCTAA | 147 |
| GAAGGTCTCAAACATGAT CTGG | ||||
| type 1 collagen | Qia | GGCAACGATGGTGCTAA | AATGCCTGGTGAACGTG | 138 |
| GACCAGCATCACCTCTGTC | ||||
| GAPDH | ABI | NA | Oc03823402_g1 | 82 |
| decorin | ABI | NA | Hs00370384_m1 | 77 |
| fibronectin | ABI | NA | Hs01549940_m1 | 66 |
| myodulin | ABI | NA | Oc03399505_m1 | 146 |
| β1-integrin | ABI | NA | Hs00559595_m1 | 75 |
| TNFα | ABI | NA | Oc03397715_m1 | 74 |
| IL-1β | ABI | NA | Oc03823250_s1 | 86 |
| IL-6 | ABI | NA | Oc04097053_m1 | 72 |
| MMP1 | ABI | NA | Oc03398637_m1 | 64 |
ABI: Applied Biosystems, Qia: Qiagen, NA: not available
Western blot analysis
Western blotting was used to determine tenocytes β1-integrin and MMP1 protein synthesis when co-cultured with leukocytes for 24 h, stimulated with TNFα or remained untreated as a control. Tenocyte monolayers were washed with PBS solution, whole cell proteins were extracted by incubation with lysis buffer (25 mM HEPES, pH 7.5, 1% Triton X-100, 5 mM CaCl2, 2 mM DTT, 1 mM EGTA [all: Carl-Roth, Karlsruhe, Germany] and proteinase inhibitors [proteinase complete mini, Roche]) on ice for 30 min. Cell debris was removed by centrifugation. Supernatants were stored at −80°C until use. Total protein concentration of whole cell extracts was normalized using Bradford protein assay (Roti-Nanquant, Carl-Roth) and bovine serum albumin (BSA) as a standard. Samples were separated by Trisglycine SDS-PAGE (12% acrylamide) under reducing conditions before being transferred to a nitrocellulose membrane (Carl-Roth), using a transblot apparatus (Bio-Rad). Equal protein loading was controlled by the use of Ponceau S staining (Sigma-Aldrich) and α-actin house-keeping protein expression. Membranes were blocked using blocking buffer (3% BSA/ PBS/ 0.05% Tween20) for 1 h at RT and incubated overnight at 4°C with primary antibodies (mouse anti-β1-integrin [Millipore Corporation/Chemicon International, Billerica, USA] monoclonal mouse anti-MMP1 [25 μg/ml, R&D systems, USA] or monoclonal mouse anti-β-actin [Sigma-Aldrich]) diluted 1:1000 in blocking buffer. Membranes were washed with PBS/ 0.05% Tween20 and incubated with horseradish peroxidase conjugated with secondary goat-anti-mouse IgG antibodies (1:5000, Dako, Glostrup, Denmark) for 2 h at RT. Specific binding was detected by chemiluminescence using RotiLumin™ (Carl-Roth) and X-ray films. The developed films were scanned and protein bands were semi quantified by densitometric scanning (AlphaDigiDoc, Cell Biosciences).
Statistical analysis
Normalized data were expressed as the mean and error of mean (mean ± SEM). Differences between experimental groups were considered significant at p <0.05 as determined by student’s paired two-tailed t test (Graph-Pad Prism 5, GraphPad software inc, San Diego, California, USA).
Results
Characterization of rabbit Achilles tendon and tenocytes in vitro
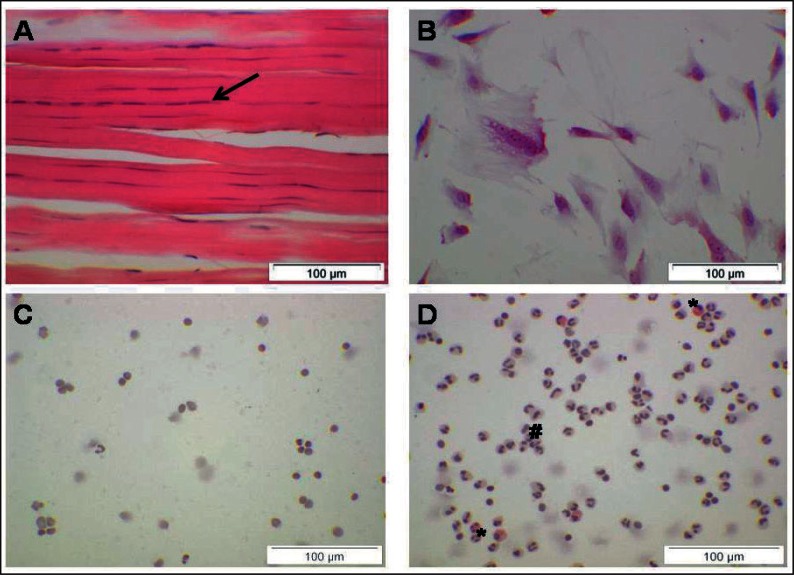
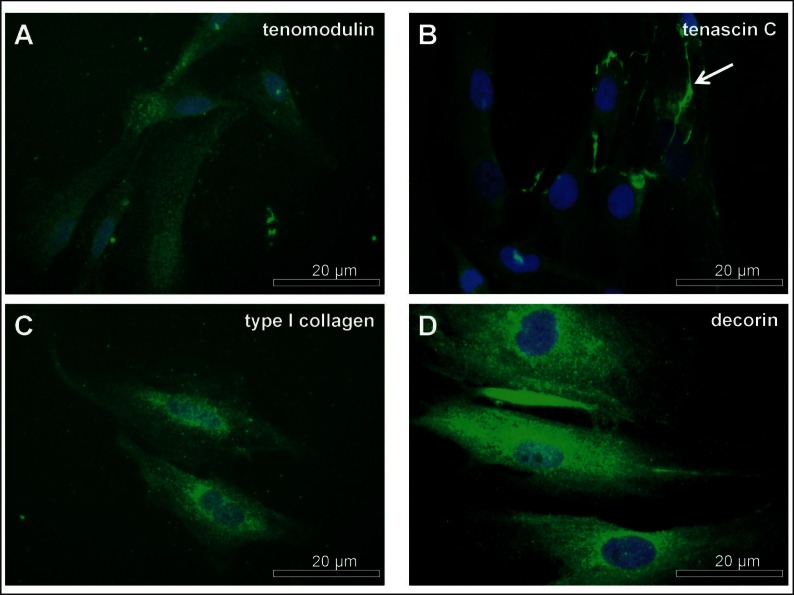
Rabbit Achilles tenocytes are lying in rows between bundles of ECM fibers and possess elongated mostly heterochromatic cell nuclei (Fig. 2A). The tenocytes in tendon were smaller than isolated and monolayer cultured primary rabbit Achilles tenocytes (Fig. 2B). Cultured tenocytes exhibited an elongated shape, rounded mostly euchromatic cell nuclei and possess long and sheet-like cytoplasmic cell appendages by which they communicated with their neighbouring cells (Fig. 2B, 3A). Isolated rabbit leukocytes were much smaller than tenocytes (Fig. 2A–D). Rounded or kidney-like nuclei with small cytoplasmic margins were discernible in PBMC preparations. Typical multi-segmented nuclei could be observed in granulocytes cell preparations. Some eosinophils were also detectable in the granulocytes preparations (Fig. 2C–D). Rabbit Achilles tenocytes expressed at the protein level the anti-angiogenic tendon marker tenomodulin (20), the ECM glycoprotein tenascin C, the main ECM protein type I collagen, the ubiquitous protein fibronectin (not shown) and the typical tendon proteoglycan decorin (Fig. 3A–D).
Figure 2A–D.
Tenocytes and leukocytes.
Figure 3A–D.
Characterization of cultured tenocytes.
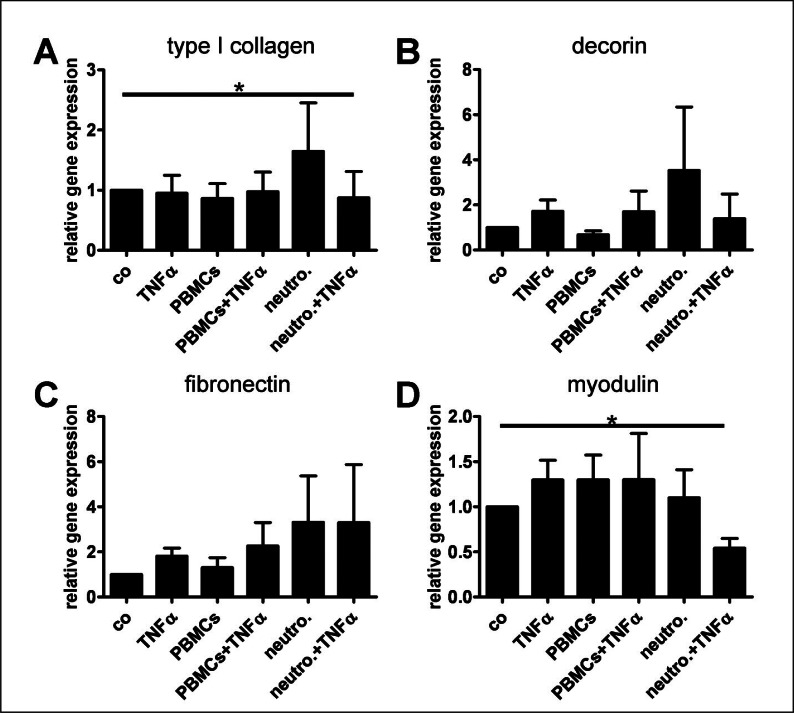
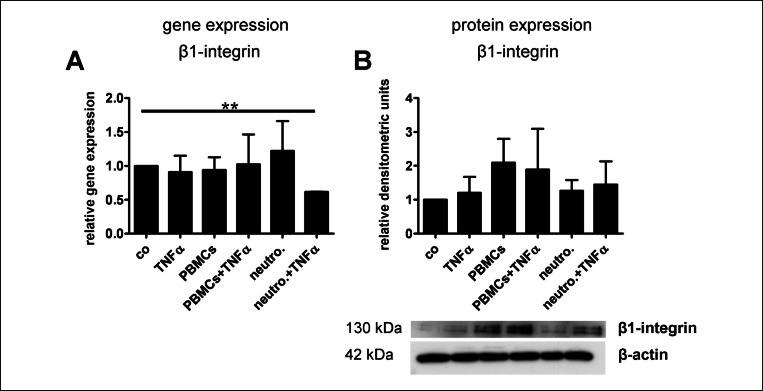
ECM gene expression in tenocytes/leukocytes co-culture
Irrespective of the treatment course, the rabbit tenocytes expressed myodulin, which is known to be expressed at the myotendinous junction and to mediate angiogenesis (9). When tenocytes were stimulated with neutrophils combined with TNFα they down-regulated their type I collagen, myodulin and β1-integrin gene expression significantly (Fig. 4A,D, 5A). At a non significant level co-culturing with PBMCs impaired tenocytes decorin gene expression and the TNFα treatment induced slightly decorin and fibronectin expression (Fig. 4B,C). Effects on β1-integrin protein expression were not significant (Fig. 5B).
Figure 4A–D.
Type I collagen, decorin, fibronectin and myodulin gene expression in tenocytes co-cultured with leukocytes.
Figure 5A–B.
β1-integrin gene and protein expression in tenocytes co-cultured with leukocytes.
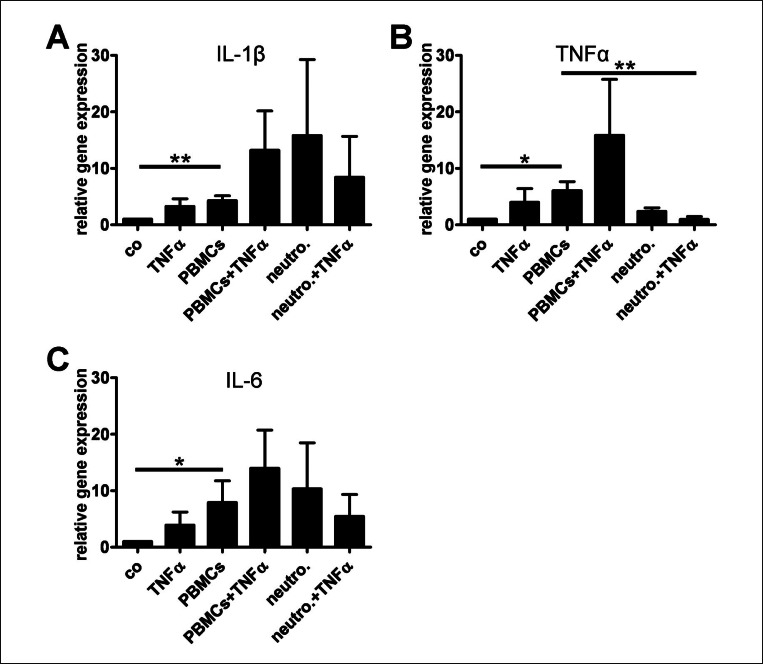
Cytokine gene expression in tenocytes in response to autologous leukocytes co-culture
PBMCs up-regulated significantly tenocytes gene expression of the key pro-inflammatory cytokines investigated here: IL-1β, TNFα, and IL-6 (Fig. 6A–C). The combination of PBMCs with TNFα had a further inductive, but not any longer significant effect. TNFα stimulation had an inductive effect on rabbit tenocytes cytokine expression which did not achieve significance. When the tenocytes were co-cultured with neutrophils without TNFα stimulation, tenocytes cytokine expression was induced but the effect was not significant. The combination of neutrophils with TNFα in co-culture with tenocytes lead to lower mean expression values of cytokines compared with the treatment with neutrophils alone.
Figure 6A–C.
Cytokine gene expression in tenocytes co-cultured with leukocytes.
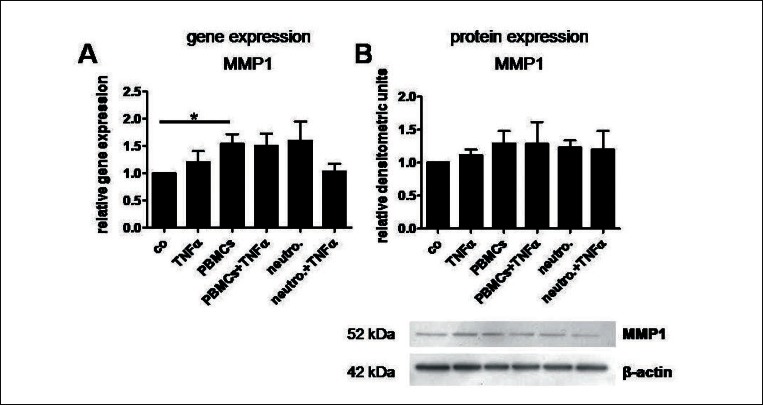
MMP1 expression in tenocytes/leukocytes co-culture
The ECM degrading enzyme MMP1 was significantly up-regulated in the tenocytes/PBMCs co-cultures (Fig. 7A). The stimulation with TNFα or neutrophils induced also MMP1 expression in tenocytes but to a lesser (non significant) extent. The protein expression of MMP1 shown by western blotting revealed mostly similar results despite not significant (Fig. 7B).
Figure 7A–B.
MMP1 gene and protein expression in tenocytes co-cultured with leukocytes.
Discussion
Healing of ruptured tendons is influenced by the early post-traumatic inflammatory response (Fig. 1A), whereby the pro-inflammatory cytokines IL-1β, TNFα and other immunoregulatory cytokines such as IL-6 might play a role. Generally, tendon healing is a time consuming reparative process leading to scar tissue formation whereby scars are associated with an altered function of tendon. IL-1β and TNFα are able to strongly activate tenocytes to up-regulate their gene expression for multiple cytokines such as IL-1β, TNFα, IL-6 and IL-10 via auto- and paracrinic amplification loops. Additionally, these cytokines induce ECM degrading enzymes such as MMPs and suppress their type I collagen synthesis initiating a catabolic cascade (11,12).
Immigrating leukocytes are an important exogenic source for pro-inflammatory cytokines in healing tendons. They are directly released during post-traumatic bleeding or recruited from blood vessels by chemotactic signals due to tissue damage (Fig. 1A). Hence, in this study rabbit tenocytes were co-cultured with autologous leukocytes to study the effect of leukocytes on tenocytes induced by soluble mediators. The rabbit was used as a cell source since it is a common experimental surgery model to study tendon repair. Additionally, rabbit tenocytes are also well characterized in vitro (21). Tenocytes were combined with autologous leukocytes in the present study to exclude effects of an immunogenic response against allogenic cells influencing the results of co-culturing. However, when as a confirmation experiment human hamstring tenocytes were combined with allogenic human blood-derived leukocytes similar effects in regard to tenocytes cytokine induction by PBMCs were detectable (not shown). PBMCs induced the gene expression of the ECM degradative enzyme MMP1, the pro-inflammatory cytokines IL-1β, TNFα and IL-6 in tenocytes. MMP1, once activated, can cleave type I collagen. Hence, it is important for callus remodelling in the advanced tendon healing phase. However, the activation of MMP1 was not assessed in the present study: the non-glycosylated 52 kDa pro-enzyme was detected by western blotting. IL-1β is a typical pro-inflammatory cytokine, up-regulated in injured tendons (22). A blockade of TNFα improved early tendon healing in a rotator cuff healing model in the rat (23). In contrast, IL-6 has been implicated to play essential roles in the wound healing process (24). Tendon healing was reduced in IL-6 knock out mice (25). Nakama et al. (26) showed that IL-6 promotes blood vessel proliferation induced by vascular endothelial growth factor (VEGF)-dependent angiogenesis via the Signal Transducer and Activator of Transcription (STAT3) signalling pathway. STAT3 activation may therefore play a critical role in tendon adaptation to ischaemic stress by maintaining the intratendinous vasculature after tendon injury. Since IL-6 can increase vascular permeability, leading to oedema, this may explain the occurrence of swelling which is a typically feature in the first hours and days after a tendon injury and maybe necessary for the wound healing processes.
Myodulin is a pro-angiogenic factor and could be demonstrated in the present study in cultured rabbit tenocytes. Myodulin expression was not restricted to the myotendinous junction as suggested by (9) since in the present study the midsubstance of tendon was used for tenocyte isolation. However, tenocytes myodulin gene expression was neither induced by PBMCs nor by neutrophils in a significant manner but rather suppressed by neutrophils combined with TNFα.
Peripheral blood-derived leukocytes were used in the present study, but one can assess that leukocytes immigrating in response to chemotactic signals and hence, activated, might present a different cytokine expression profile and release further growth factors and mediators influencing tendon healing. Leukocytes cytokine expression pattern might also be influenced by direct cell-cell contacts between tenocytes and leukocytes and hereby, lead to a modified/enhanced response of tenocytes. So a direct co-culture system should be applied in future studies. Additionally, the soluble mediators released by the autologous leukocytes into the culture supernatants should be further characterised to identify key effector cytokines and chemokines. Not only typical pro-inflammatory cytokines but also growth factors are released by leukocytes such as transforming growth factor (TGF)β1 or vascular endothelial growth factor (VEGF) (14,27). In comparison to the effect of leukocytes, tenocytes were stimulated with TNFα alone. At all the effect by TNFα alone was weaker compared with that of PBM-Cs. Since human TNFα was used a reduced stimulatory effect on rabbit tenocytes can be supposed caused by interspecies differences in susceptibility. However, a mixture of several soluble mediators released by the PBMCs might exhibit additive effects when tenocytes were exposed to them. Irrespective of the presence of growth factors produced by leukocytes, tenocytes ECM and β1-integrin gene expression revealed no major changes except for a suppression of type I collagen and β1-integrins by neutrophils combined with TNFα. However, the inconsistency between β1-integrin gene and protein expression level might depend on translational and posttranslational regulatory effects.
The, probably, divergent effects of particular PBMC effector cell subpopulations should be further analysed in future. The neutrophil cell fraction contained also some eosinophil granulocytes. This heterogeneicity might be responsible for the high standard deviations observed in response to stimulation of tenocytes with neutrophils.
Conclusion with some perspectives for the future
Taken together, this study indicates an interplay between leukocytes and tenocytes via soluble mediators: tenocytes can be activated by leukocytes to express several pro-inflammatory cytokines, MMPs and probably other factors. The particular impact of this interplay on tendon healing should be further investigated. Nevertheless, it should be considered that the behavior of peripheral blood derived leukocytes may be quite different if they are stimulated/ activated by the in vivo injury environment. Similarly, the tenocytes may respond differently in an injured tendon in contrast to the in vitro conditions studied here. When comparing the setting with in vivo conditions, tenocytes stress and injury might amplify the susceptibility of them to leukocyte derived mediators. Furthermore, the consequence of direct cell-cell contacts between both cell types remained up to now disregarded in this study.
The implications of the expression of pro-inflammatory mediators by tenocytes should be addressed in ongoing experiments to answer the question whether these factors ultimately impair the tendon reparative process or whether they are required for an effective tendon callus remodeling. The use of non-steroidal anti-inflammatory drugs (NSAID) is a common clinical practice (28). Hence, the possible effects of anti-inflammatory medications, e.g. the application of particular NSAIDs following tendon injury could be addressed in this model in future. It has been shown that both, the prostaglandin (PG) E2 release, but also the adaptive collagen synthesis in tendon was inhibited by NSAIDs during exercise (29). In addition, adhesion formation was reduced in healing tendons by the NSAID ibuprofen. On the contrary, tenocyte proliferation and migration was impaired and MMP expression was induced in cultured tenocytes whereby the expressions of types I and III collagen remained mostly unaffected (28,30–32). The results of these previous studies suggest that anti-inflammatory therapy with NSAIDs might also interfere with some features of the natural healing response in tendon.
Acknowledgments
We gratefully acknowledge the support by Dr. Christiane Stoll. The authors would like to acknowledge the support of the Jürgen Manchot, Else Kröner-Fresenius and the Sonnenfeld Foundations.
Abbreviations
- ABI
applied Biosystems
- BSA
bovine serum albumine
- DAPI
4′,6- diamidino-2-phenylindole
- ECM
extracellular matrix
- FCS
fetal calf serum
- GAPDH
glyceraldehyde-3-phosphate dehydrogenase
- GM-CSF
granulocyte-macrophage colony stimulating factor
- HE
haematoxylin Eosin
- IFN-γ
interferon-γ
- IL
interleukin
- MMP
matrix-metalloproteinase
- NSAID
non-steroidal anti-inflammatory drugs
- PBMC
peripheral blood mononuclear cells
- PBS
phosphate buffered saline
- STAT3
signal transducer and activator of transcription
- TBS
tris buffered saline
- TGF-β
transforming growth factor-β
- RT
room temperature
- TNF
tumor necrosis factor
- VEGF
vascular endothelial growth factor
References
- 1.Schulze-Tanzil G, Al-Sadi O, Wiegand E, et al. The role of pro-inflammatory and immunoregulatory cytokines in tendon healing and rupture: new insights. Scand J Med Sci Sports. 2011 Jun;21(3):337–351. doi: 10.1111/j.1600-0838.2010.01265.x. [DOI] [PubMed] [Google Scholar]
- 2.Aspenberg P. Stimulation of tendon repair: mechanical loading, GDFs and platelets. A mini-review. Int Orthop. 2007 Dec;31(6):783–789. doi: 10.1007/s00264-007-0398-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abrahamsson SO, Lundborg G, Lohmander LS. Segmental variation in microstructure, matrix synthesis and cell proliferation in rabbit flexor tendon. Scandinavian journal of plastic and reconstructive surgery and hand surgery / Nordisk plastikkirurgisk forening [and] Nordisk klubb for handkirurgi. 1989;23(3):191–198. doi: 10.3109/02844318909075117. [DOI] [PubMed] [Google Scholar]
- 4.Tillander B, Franzen L, Norlin R. Fibronectin, MMP-1 and histologic changes in rotator cuff disease. J Orthop Res. 2002 Nov;20(6):1358–1364. doi: 10.1016/S0736-0266(02)00057-8. [DOI] [PubMed] [Google Scholar]
- 5.Harwood FL, Monosov AZ, Goomer RS, et al. Integrin expression is upregulated during early healing in a canine intrasynovial flexor tendon repair and controlled passive motion model. Connect Tissue Res. 1998;39(4):309–316. doi: 10.3109/03008209809021505. [DOI] [PubMed] [Google Scholar]
- 6.Hirsch MS, Lunsford LE, Trinkaus-Randall V, Svoboda KK. Chondrocyte survival and differentiation in situ are integrin mediated. Dev Dyn. 1997 Nov;210(3):249–263. doi: 10.1002/(SICI)1097-0177(199711)210:3<249::AID-AJA6>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 7.Cao L, Lee V, Adams ME, et al. beta-Integrin-collagen interaction reduces chondrocyte apoptosis. Matrix Biol. 1999 Aug;18(4):343–355. doi: 10.1016/s0945-053x(99)00027-x. [DOI] [PubMed] [Google Scholar]
- 8.Stoll C, John T, Conrad C, et al. Healing parameters in a rabbit partial tendon defect following tenocyte/biomaterial implantation. Biomaterials. 2011 Jul;32(21):4806–4815. doi: 10.1016/j.biomaterials.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 9.Pisani DF, Pierson PM, Massoudi A, et al. Myodulin is a novel potential angiogenic factor in skeletal muscle. Exp Cell Res. 2004 Jan 1;292(1):40–50. doi: 10.1016/j.yexcr.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 10.Nagase H, Visse R, Murphy G. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc Res. 2006 Feb 15;69(3):562–573. doi: 10.1016/j.cardiores.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Tsuzaki M, Guyton G, Garrett W, et al. IL-1 beta induces COX2, MMP-1, -3 and -13, ADAMTS-4, IL-1 beta and IL-6 in human tendon cells. J Orthop Res. 2003 Mar;21(2):256–264. doi: 10.1016/S0736-0266(02)00141-9. [DOI] [PubMed] [Google Scholar]
- 12.John T, Lodka D, Kohl B, et al. Effect of pro-inflammatory and immunoregulatory cytokines on human tenocytes. J Orthop Res. 2010 Aug 2;28(8):1071–1077. doi: 10.1002/jor.21079. [DOI] [PubMed] [Google Scholar]
- 13.Krause ML, Davis JM, 3rd, Knutson KL, et al. Assessing immune function by profiling cytokine release from stimulated blood leukocytes and the risk of infection in rheumatoid arthritis. Clin Immunol. 2011 May 30; doi: 10.1016/j.clim.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zumstein MA, Berger S, Schober M, et al. Leukocyte- and Platelet-Rich Fibrin (L-PRF) for Long-Term Delivery of Growth Factor in Rotator Cuff Repair: Review, Preliminary Results and Future Directions. Curr Pharm Biotechnol. 2011 Jul 8; doi: 10.2174/138920112800624337. [DOI] [PubMed] [Google Scholar]
- 15.de Mos M, van der Windt AE, Jahr H, et al. Can platelet-rich plasma enhance tendon repair? A cell culture study. Am J Sports Med. 2008 Jun;36(6):1171–1178. doi: 10.1177/0363546508314430. [DOI] [PubMed] [Google Scholar]
- 16.Kajikawa Y, Morihara T, Sakamoto H, et al. Platelet-rich plasma enhances the initial mobilization of circulation-derived cells for tendon healing. J Cell Physiol. 2008 Jun;215(3):837–845. doi: 10.1002/jcp.21368. [DOI] [PubMed] [Google Scholar]
- 17.Schulze-Tanzil G, Mobasheri A, Clegg PD, Sendzik J, John T, Shakibaei M. Cultivation of human tenocytes in high-density culture. Histochem Cell Biol. 2004 Sep;122(3):219–228. doi: 10.1007/s00418-004-0694-9. [DOI] [PubMed] [Google Scholar]
- 18.Stoll C, John T, Endres M, et al. Extracellular matrix expression of human tenocytes in three-dimensional air-liquid and PLGA cultures compared with tendon tissue: Implications for tendon tissue engineering. J Orthop Res. 2010 Sep 24;28(9):1170–1177. doi: 10.1002/jor.21109. [DOI] [PubMed] [Google Scholar]
- 19.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods (San Diego, Calif. 2001 Dec;25(4):402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 20.Docheva D, Hunziker EB, Fassler R, Brandau O. Tenomodulin is necessary for tenocyte proliferation and tendon maturation. Mol Cell Biol. 2005 Jan;25(2):699–705. doi: 10.1128/MCB.25.2.699-705.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bernard-Beaubois K, Hecquet C, Houcine O, Hayem G, Adolphe M. Culture and characterization of juvenile rabbit tenocytes. Cell Biol Toxicol. 1997 Feb;13(2):103–113. doi: 10.1023/b:cbto.0000010395.51944.2a. [DOI] [PubMed] [Google Scholar]
- 22.Berglund M, Hart DA, Wiig M. The inflammatory response and hyaluronan synthases in the rabbit flexor tendon and tendon sheath following injury. J Hand Surg. 2007 Oct;32(5):581–587. doi: 10.1016/J.JHSE.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 23.Gulotta LV, Kovacevic D, Cordasco F, Rodeo SA. Evaluation of Tumor Necrosis Factor alpha Blockade on Early Tendon-to-Bone Healing in a Rat Rotator Cuff Repair Model. Arthroscopy. 2011 Jun 25; doi: 10.1016/j.arthro.2011.03.076. [DOI] [PubMed] [Google Scholar]
- 24.Gallucci RM, Simeonova PP, Matheson JM, et al. Impaired cutaneous wound healing in interleukin-6-deficient and immunosuppressed mice. Faseb J. 2000 Dec;14(15):2525–2531. doi: 10.1096/fj.00-0073com. [DOI] [PubMed] [Google Scholar]
- 25.Lin TW, Cardenas L, Glaser DL, Soslowsky LJ. Tendon healing in interleukin-4 and interleukin-6 knockout mice. J. Biomech. 2006;39(1):61–69. doi: 10.1016/j.jbiomech.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 26.Nakama K, Gotoh M, Yamada T, et al. Interleukin-6-induced activation of signal transducer and activator of transcription-3 in ruptured rotator cuff tendon J Int Med Res November–Dec2006346624–631. [DOI] [PubMed] [Google Scholar]
- 27.Dohan Ehrenfest DM, Bielecki T, Jimbo R, et al. Do the Fibrin Architecture and Leukocyte Content Influence the Growth Factor Release of Platelet Concentrates? An Evidence-Based Answer Comparing a Pure Platelet-Rich Plasma (P-PRP) Gel and a Leukocyte- and Platelet-Rich Fibrin (L-PRF) Curr Pharm Biotechnol. 2011 Jul 8; doi: 10.2174/138920112800624382. [DOI] [PubMed] [Google Scholar]
- 28.Tsai WC, Hsu CC, Chang HN, Lin YC, Lin MS, Pang JH. Ibuprofen upregulates expressions of matrix metalloproteinase-1, -8, -9, and -13 without affecting expressions of types I and III collagen in tendon cells. J Orthop Res. 2010 Apr;28(4):487–491. doi: 10.1002/jor.21009. [DOI] [PubMed] [Google Scholar]
- 29.Christensen B, Dandanell S, Kjaer M, Langberg H. Effect of anti-inflammatory medication on the running-induced rise in patella tendon collagen synthesis in humans. J Appl Physiol. 2011 Jan;110(1):137–141. doi: 10.1152/japplphysiol.00942.2010. [DOI] [PubMed] [Google Scholar]
- 30.Tan V, Nourbakhsh A, Capo J, Cottrell JA, Meyenhofer M, O'Connor JP. Effects of nonsteroidal anti-inflammatory drugs on flexor tendon adhesion. J Hand Surg. 2010 Jun;35(6):941–947. doi: 10.1016/j.jhsa.2010.02.033. [DOI] [PubMed] [Google Scholar]
- 31.Tsai WC, Tang FT, Hsu CC, Hsu YH, Pang JH, Shiue CC. Ibuprofen inhibition of tendon cell proliferation and upregulation of the cyclin kinase inhibitor p21CIP1. J Orthop Res. 2004 May;22(3):586–591. doi: 10.1016/j.orthres.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 32.Tsai WC, Hsu CC, Chen CP, Chen MJ, Lin MS, Pang JH. Ibuprofen inhibition of tendon cell migration and down-regulation of paxillin expression. J Orthop Res. 2006 Mar;24(3):551–558. doi: 10.1002/jor.20069. [DOI] [PubMed] [Google Scholar]