Summary
Background and objective: insertional Achilles tendinopathy is a common condition among athletes and joggers. One fifth of the injuries involves the insertion of the tendon. The etiology is either due to mechanical overuse related to sports activity, or a systemic inflammatory disease. The clinical appearance includes pain and movement restriction. The primary treatment is conservative. The surgery referred to in this study (Calcaneal Osteotomy) is performed by decompression of the posterior margin of the calcaneus. If the tendon is degenerative, debridement is needed. There is controversy on the surgical outcome and the surgical approach. A retrospective analytic observational study. Methods: 20 patients who were diagnosed with IAT (21 feet) and were operated on between the years 2000–2007 by calcaneal osteotomy. Main outcome measures: the primary measure of success was diminished pain. It was demonstrated in the AOFAS score and in the VAS scale of pain. Results: the average grade in the AOFAS questionnaire improved by 20 points, and the average grading of pain in the VAS scale was decreased by 4.21. The median satisfaction rate was 8, the average was 5.81. 62% of the patients would repeat the surgery/recommend it. We found a significant relationship (p=0.022) between patients who avoided sports activity while suffering from insertional Achilles tendinopathy and the satisfaction rate from the surgery. Conclusions: using the calcaneal osteotomy technique as a surgical treatment for IAT is successful, and improves measures of pain and function. Low compliance with avoiding sports activity while suffering from an IAT might lead to a need for surgery.
Keywords: Achilles tendon, pain, tendinopathy, calcaneal osteotomy, surgical outcome
Introduction
Insertional Achilles tendinopathy (IAT) is an injury at the insertion of the Achilles tendon into the calcaneus. It is more prevalent in a young, active population. The annual incidence of disorders of the Achilles tendon in runners was reported as 7 to 9%1.
The etiology of IAT is usually mechanical overuse in professional2 and amateur athletes who admitted to performing physical activity without proper preparation. Numerous factors including pes cavus, hyperpronation, advancing age, hypertension, obesity, steroid use, use of estrogen and fluoroquinolone antibiotics have been associated with Achilles tendon disorders3. Other possibilities are connective tissue disease (Ehlers-Danlos and Marfan’s Syndromes), systemic inflammatory disease (psoriatic arthritis, spondyloarthropathy, rheumatoid arthritis, Reiter’s disease) and vascular diseases, such as diabetes 4,5.
The Achilles tendon, a continuation of the gastrocnemius muscle, inserts into the calcaneal bone. The enthesis (insertion point) is composed of the tendon itself, calcified and uncalcified cartilage, and the calcaneus. The parathenon surrounds the tendon, with an elastic capacity of 2–3 cm. Dual blood supply (muscle and bone) is recognized, but there is an avascular zone located 3 to 5 cm proximal to the insertion6. The retrocalcaneal bursa, which protects the tendon, is located between the tendon and the calcaneal bone.
The clinical presentation begins with localized pain in the insertion area on exertion, and then chronic pain. Sometimes there is a bulge in the lateral aspect of the calcaneal bone, called Haglund deformity (Fig. 1). Radiology may demonstrate calcifications in the area (Fig. 2). Edema and thickening of the distal portion of the Achilles tendon can be seen on MRI (Fig. 3).
Figure 1.
Haglund deformity on right foot.
Figure 2.
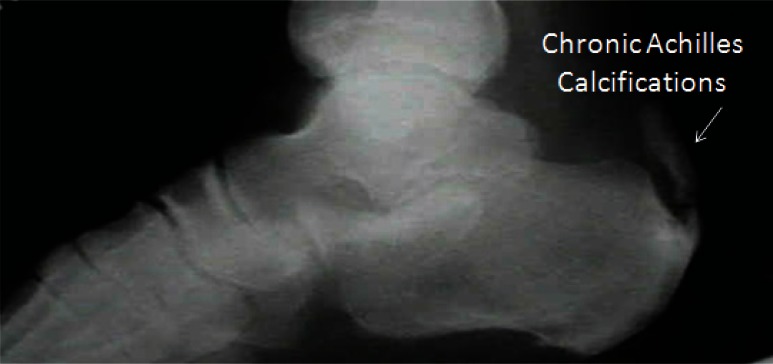
X-ray showing chronic calcifications of Achilles tendon.
Figure 3.

MRI showing thickened and edematous Achilles tendon.
Insertional Achilles tendinopathy is usually treated conservatively, including rest, elevated leg, cold packs and nonsteroidal anti-inflammatory treatment. Insoles and physiotherapy are also recommended7. A cast with weight bearing is an option. Rasmussen suggested the beneficial effect of shock waves8. Local steroid injection may lead to increased risk of an acute tear9.
If conservative treatment fails, surgery is usually recommended. There is little information in the literature about the surgical treatment of inflammation and there is controversy about the surgical approach, type of surgery and its effectiveness. The most common technique is a lateral approach to the insertion zone, removal of the retrocalcaneal bursa, excision of the posterior prominence of the calcaneal bone and debridement of the insertion zone. The procedure is called calcaneal osteotomy10,11. It can be performed arthroscopically12. Maffulli et al.13 recently reported on a transverse Cincinnati approach describing the debridement and calcaneal osteotomy of the posterosuperior corner of the calcaneous with excellent outcome. Other option also described by Maffulli et al.14 for calcified ITA is disinsertion of the Achilles tendon to fully excise the calcific deposit and reinsertion of the Achilles tendon in the calcaneus with suture anchors. Surgical outcome is usually good and there is improvement in measures of pain and function15–19. This paper reports on a case series of patients with Achilles tendinopathy who were operated on by a standard calcaneal osteotomy through a lateral longitudinal surgical approach.
Materials and methods
Patients: from 2000 to 2007, we operated on 38 patients with IAT. Only patients who were treated by a standard calcaneal osteotomy through a lateral longitudinal surgical approach were included. Exclusion criteria were patients who were operated on within six months of the onset of the study (approximate time of recovery). The study was approved by the local ethical committee and all patients signed an informed consent.
Data collection: chart data were reviewed and all patients were interviewed and examined. All patients underwent a physical examination. X-ray, MRI, ultrasound, CT and bone scan; results were reviewed, as available.
Patients evaluated their pain using a visual analogue pain scale (VAS) before and after surgery. Quantitative comparison between measures of success before and after surgery was made by American Orthopedics Foot and Ankle Society (AOFAS) score11. Pain is measured from 0–40, where 40 is no pain. Function is measured on a scale from 0–50, where 50 points is normal function, and Alignment is rated on a scale from 0–10, where 10 is normal. Post-operatively, patients were asked to rate their satisfaction on a scale of 0 to 10, with 0 being not satisfied and 10 being completely satisfied.
Prior to surgery, patients attempted a variety of conservative therapies. All patients were treated with NSAID’S and physiotherapy consisting of eccentric exercises of the gastrosoleus complex. Four patients were casted for more than a month and 10 (48%) patients received steroid injections at other medical facilities. Shock wave therapy was performed in 8 (38%) patients.
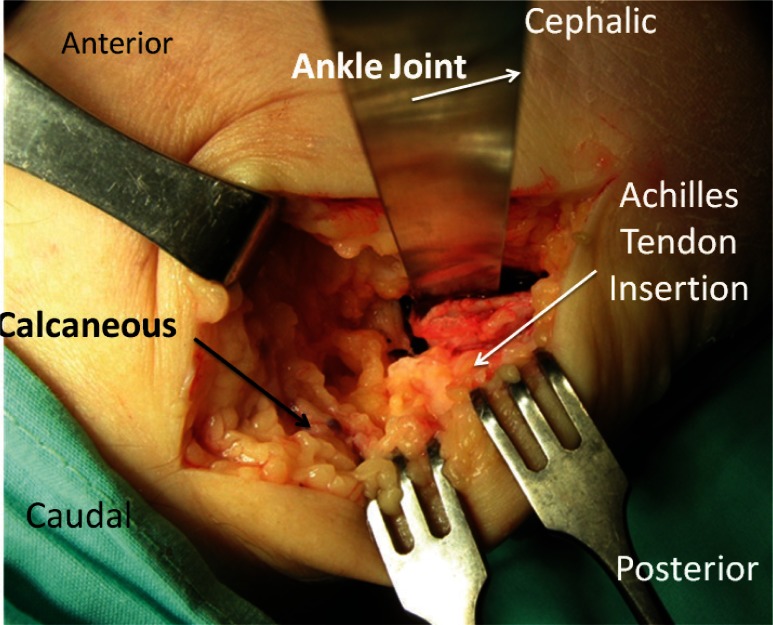
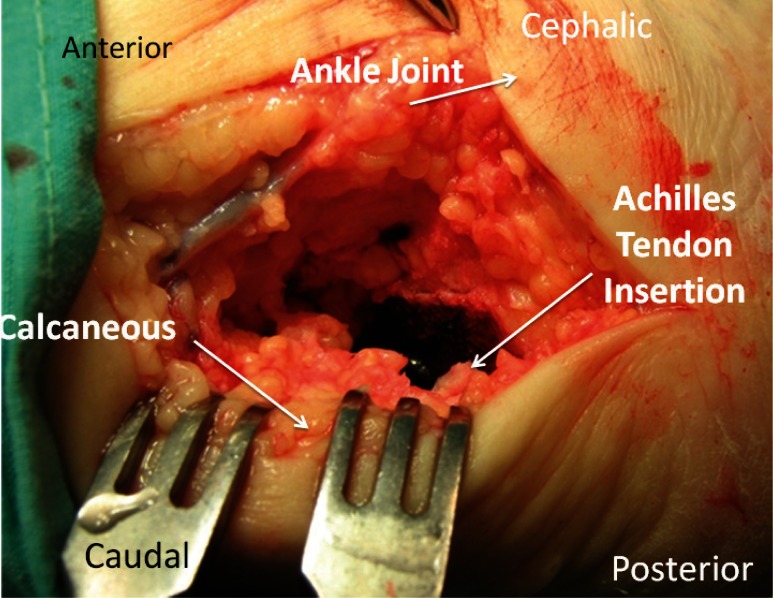
The operation was performed by two senior surgeons (M.S. and N.M.) with a standard rehabilitation protocol. Figure 4 shows the procedure before the removal of the bony prominence. Figure 5 shows the insertion site of the Achilles tendon.
Figure 4.
It shows the procedure before the removal of the bony prominence.
Figure 5.
It shows the insertion site of the Achilles tendon.
Patients were seen 2 weeks, 1, 3 and 6 months postoperatively. All the patients were immediately full weight bearing walking with well-padded bandage. They were not allowed any effort except for easy walking for 3 weeks. After 3 weeks, physiotherapy was started; first ROM of the ankle and against resistance after 6 weeks. The patients were allowed to return to full activity after 3 months.
The main outcome measures were reduced pain, improved function, return to sports and satisfaction with the procedure.
Statistical analysis: the data were analyzed with SPSS. We explored the change in quantitative parameters before and after the surgery with paired t-test and with Wilcoxon signed rank test. Comparisons between two independent groups were done with the Mann-Whitney Test. Data are presented as mean ± standard deviation (S.D.). All statistical tests were two-tailed and p-value of less than .05 was considered statistically significant.
Results
Of 38 patients operated on in the years 2000–2007, we recruited 20 patients and 21 feet. The sample ranged in age from 25 to 65 years (mean 50.62 years); 15 of the participants were males.
Most patients engaged in sports activity, including free running, marathon running, swimming, football, gymnastics, and dancing. Despite deterioration of their symptoms, 16 (79%) athletes continued to participate in sports. 4 (19%) had a systemic inflammatory disease including seronegative spondylopathy, systemic lupus erythematosis, antiphospholipid antibody syndrome, ankylosing spondylitis and gout; 3 patients had diabetes.
Physical examination: on the day of surgery, patients presented with tenderness at the Achilles tendon insertion zone. A bony prominence was present at the lateral aspect of the calcaneous (Haglund deformity) in five patients (Fig. 1).
An average of 3.47 (S.D. 2.9; range 0–11) years elapsed from the onset of pain until surgery. The majority of patients (11) had pain duration of less than 3 years before surgery. Preoperative pain was described as increasing. At first it appeared only during effort, but later also at rest. Most patients did not describe a significant decrease in daily function, except for disruption in their sport activities; although many also had limited range of motion, difficulty walking on uneven surfaces (such as stairs or a ladder), or a limp.
Most patients had an ultrasound of the Achilles insertion zone; diagnostic features of edema and calcifications were present in more than 19 (92%). Preoperative X-ray was less demonstrative.
Postoperatively, all subjects had a longitudinal scar left in the lateral heel. Swollen tissue, a bone bulge, and a limp were observed in three patients. Sensitivity to heel palpation was noted in 11 (52.4%) of the subjects, but only one had pain located specifically in the insertion zone. The other patients had pain in the tendon itself, in the lateral aspect of the surgical scar or a general sensitivity in the heel.
As preoperative range of motion was conserved in most patients, the majority did not demonstrate limited range of motion after surgery. The patients who had sensitivity to palpation appeared to feel pain while performing plantar-flexion. Pain: the average VAS pain scale score before surgery was 7.94 ± 1.76 (where 0 describes no pain and 10 describes the most pain imaginable). In the AOFAS questionnaire, pain before the surgery was on average 10 (S.D. 10.9) (40 is absence of pain). Postoperative pain was decreased significantly according to both the VAS pain scale and the AO-FAS pain score. The average VAS score after surgery was 3.7 (S.D. 3.8) (P=.001) and the AOFAS pain category score after surgery was 30 (S.D. 13.04; P=.001) (Tab. 1).
Table 1.
Pre- and post-operative changes in pain, function and total score (N=21)
| Measure | Pre-operative Mean (± S.D.) | Post-operative Mean (± S.D.) | P-value |
|---|---|---|---|
| VAS pain | 7.9±1.8 | 3.7±3.8 | .001 |
| AOFAS Pain | 10.0±11.9 | 30.0±13.0 | .001 |
| AOFAS Function | 31.9±15.4 | 42.9±9.2 | .005 |
| AOFAS Total Score | 52.0±22.9 | 83.1±21.3 | .0003 |
Functional improvement: the average score in the AOFAS questionnaire function section improved from 31.9 (S.D. 15.4) before surgery to 42.9 (S.D. 9.2) postoperatively (P=0.005). The AOFAS total score increased on average by 31.14 (S.D. 32.22) points (P = 0.003).
Return to activity: patients who returned to sports activity did so in about 4.5 (S.D. 3.6) months after surgery. 11 (57%) of patients returned to full activity including sports, 5 (24%) returned to partial activity, while 4 (19%) did not resume sports activity. Of these, 14 (67%) returned to activity within 6 months or less and 3 (14%) within 6 to 12 months.
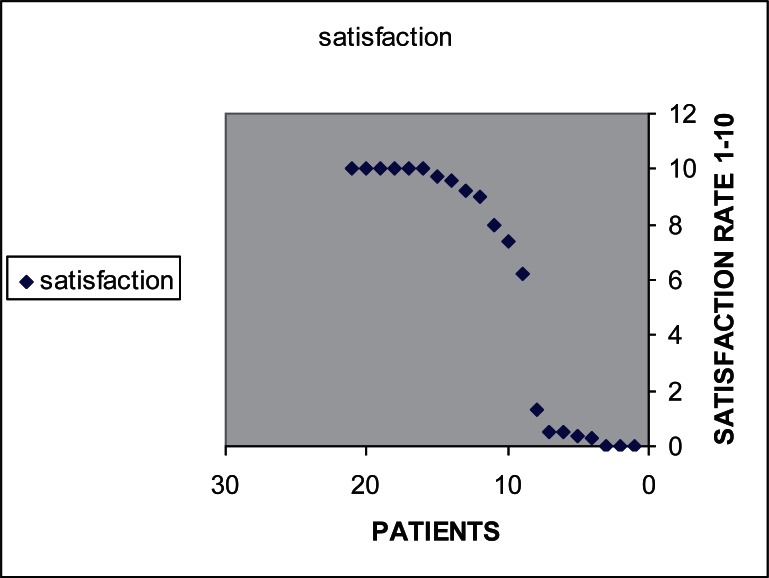
Satisfaction: a majority of patients 13 (62%) noted that they would recommend the surgery to others. While 8 patients rated their satisfaction as 1.5 or lower, 13 patients reported it as 6 or higher. There were no intermediate measures. (Fig. 6). On average, satisfaction rate with surgery was 5.81 (S.D. 4.48) (median 8). Patients with decreased postoperative pain had very high success rates in terms of function and satisfaction. The opposite was true for patients in whom the surgery did not decrease the pain level. Satisfaction was also measured indirectly by asking if the patient would recommend the surgery to others and/or would have repeated it; 62% of the patients responded in the affirmative.
Figure 6.
Patient satisfaction was either high or low, with no intermediate measures.
Discussion
This study examined the success rate of a relatively rare surgery that has not been described widely in the literature. Only patients who were treated by a standard surgical approach (calcaneal osteotomy with a lateral longitudinal section) were included. Results of this study demonstrate a high success rate for the indices examined.
Important measures of success that have proven to be significant were improvement in pain, function, and AOFAS total score (P ≤ 0.05). The most significant correlation was between the decrease in VAS pain scores and a high level of satisfaction (0.884).
We tried to find a statistical correlation between measures of success [reduction in pain (VAS) and satisfaction level] and possible reasons. No correlation was found between outcome measures and the patients’ age (Pearson Correlation: −0.021) or time between the appearance of pain and surgery date (Pearson Correlation: −0.267). In addition, there was no statistically significant association between outcome measures and possible etiologies (chronic inflammatory disease, diabetes, local trauma to the tendon, sport, etc.). The small sample size precluded detailed analysis. We also examined whether conservative treatment with shock waves improved the surgical prognosis. Eight (38%) of subjects were treated with shock waves before surgery. We found no statistically significant association between receiving this treatment and effectiveness of the surgical procedure. There was no significant association between local steroid injection and effectiveness of the operation (P=0.78). Given that there is a contraindication of steroid injection due to a risk of Achilles tendon rupture, we expected that the results of surgery would have been worse in those patients9. Of all the relationships examined, a significant association (P ≤ 0.022) was only found between rest/avoiding sports activity during inflammation and satisfaction with surgical outcomes. This can be explained in several ways. First of all, avoiding exertion decreases mechanical damage to the inflamed tendon. In addition, it can be assumed that participants who avoided sports activity during inflammation were more compliant with medical treatment, and therefore have a better chance of recovery. Patients who are highly compliant would be more likely to follow the recovery protocol than patients with low compliance.
In our sample, 76% were engaged in some sport before the inflammation; almost all of these in intensive sports (e.g. running, soccer). Contrary to the recommendation of their physicians, 79% continued to engage in sports activities. They resorted to surgery only when they could not tolerate the pain any longer. Mechanical etiology is described in the literature12. It involves athletes, some professional athletes, who are unwilling to stop practicing sports. Lack of adherence to conservative treatment has led them to surgery, and could also affect the success of the surgery in terms of recovery. It is also possible that patients who were able to return to sport activity, reported greater satisfaction than those who did not discontinue the activity.
Most of the participants returned to full activity after surgery. Five patients returned to partial activity and four participants did not return to sports activity. A borderline significance correlation (P ≤ 0.068) was found between the difference in VAS score and the time until return to activity after surgery. This further strengthens pain intensity (VAS score) as a measure of success after surgery. There is no doubt that pain effects function and that regaining function depends on improvement in pain.
This study examined a relatively large series of patients. It is limited by the retrospective follow up and possible recall bias of patients regarding their pain and functional limitations pre- and post-operatively. As noted before, most of our patients indicated no significant loss of function before surgery, so the improvement is less impressive than was the decline in pain intensity. The main measure of success was pain reduction.
Johnson et al.16 conducted a similar study on a population of 22 patients with insertional Achilles tendinopathy who underwent surgical treatment using a central longitudinal incision. Their results were also analyzed using the AOFAS questionnaire. They found an average improvement of 26 points in the pain section (p ≤ 0.001), but did not specify a standard deviation. Compared to this report16 our results are good. The function score improvement was 10 points (P ≤ 0.001) and general questionnaire score was 36 points (P ≤ 0.001).
Toolan et al.11 found an average difference of 5.3 points between AOFAS before and after surgery. They showed that patients have tendency to remember the situation before surgery as worse than that reported in real time.
There was a wide range in satisfaction with results among patients. It should be noted that the level of satisfaction was either very high or very low. An indirect measure of satisfaction found that a majority of patients responded that they would recommend the surgery to others and/or would repeat it, if necessary.
McGarvey et al.17 conducted a similar study on 22 patients with Achilles tendinitis who were operated on using a central longitudinal incision. They also inquired whether patients would repeat surgery and 77% responded in the affirmative. Although they had better results compared to ours, this article does not detail the level of satisfaction among the patients who would repeat the surgery. Also, only 59% of the patients in that study reported no pain after surgery and returned to normal function, compared to 81% of our patients. The significant statistical relationship that we found between resting from sports activity during inflammation and the success rate of the surgery emphasizes the relationship between compliance with treatment and treatment success. We suggest further, prospective research that will compare two groups of patients with insertional Achilles tendinopathy – one group that continued to engage in sports activity during the inflammation, and a control group of patients who discontinued sports. The conclusions of such research will assist in determining candidacy for surgery.
In conclusion, the results of this study indicate that surgical treatment for insertional Achilles tendinopathy can be effective mainly in improving pain and function.
A prospective study will allow a more accurate preoperative evaluation of pain and function and therefore, a more accurate estimate of improvement.
References
- 1.Lysholm J. Injuties in runners. Injuries in runners. Am J Sports Med. 1987;15:168–171. doi: 10.1177/036354658701500213. [DOI] [PubMed] [Google Scholar]
- 2.Jhingan S, Perry M, O'Driscoll G, Lewin C, Teatino R, Malliaras P, Maffulli N, Morrissey D. Thicker Achilles tendons are a risk factor to develop Achilles tendinopathy in elite professional soccer players. MLTJ. 2011;2:53–58. [PMC free article] [PubMed] [Google Scholar]
- 3.Irwin TA. Current concepts review: insertional achilles tendinopathy. Foot Ankle Int. 2010;31(10):933–939. doi: 10.3113/FAI.2010.0933. [DOI] [PubMed] [Google Scholar]
- 4.Myerson MS, McGarvey W. Disorders of the insertion of Achilles tendon and Achilles tendonitis. The Journal of Bone and Joint Surgery. 1999;48-A:211–8. [PubMed] [Google Scholar]
- 5.Novacheck TF. Running injuries: a biomechanical approach, an instructional course lecture. J Bone Joint Surg. 1998;80-A:1220–1233. [PubMed] [Google Scholar]
- 6.Aström M, Westlin N. Blood flow in the human Achilles tendon assessed by laser Doppler flowmetry. J Orthop Res. 1994;12(2):246–252. doi: 10.1002/jor.1100120214. [DOI] [PubMed] [Google Scholar]
- 7.Loppini M, Maffulli N. Conservative management of tendinopathy: an evidence-based approach. MLTJ. 2011;1:133–136. [PMC free article] [PubMed] [Google Scholar]
- 8.Rasmussen S, Christiansen M, Mathiesen I, Simonson O. Shockwave therapy for Achilles tendinopathy: a double blind, randomized trial of efficacy. Acta Orthop. 2008;79(2):249–256. doi: 10.1080/17453670710015058. [DOI] [PubMed] [Google Scholar]
- 9.Kleinman M, Gross AE. Achilles tendon rupture following steroid injection. Report of three cases. J Bone Surg Am. 1983;65(9):1345–1347. [PubMed] [Google Scholar]
- 10.Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology. 2006;45(5):508–521. doi: 10.1093/rheumatology/kel046. [DOI] [PubMed] [Google Scholar]
- 11.Toolan BC, Wright Quinones VJ, Cunningham BJ, Brage ME. An evaluation of the use of retrospectively acquired preoperative AOFAS clinical rating scores to assess surgical outcome after elective foot and ankle surgery. Foot Ankle Int. 2001;22:775–778. doi: 10.1177/107110070102201002. [DOI] [PubMed] [Google Scholar]
- 12.Lui TH. Arthroscopy and endoscopy of the foot and ankle: indications for new techniques. Arthroscopy. 2007;23(8):889–902. doi: 10.1016/j.arthro.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 13.Maffulli N, DBA, Testa V, Capasso G, Oliva F, Denaro V. Safety and outcome of surgical debridement of insertional Achilles tendinopathy using a transverse (Cincinnati) incision. J Bone Joint Surg Br. 2011;93-B:1503–1507. doi: 10.1302/0301-620X.93B11.27379. [DOI] [PubMed] [Google Scholar]
- 14.Maffulli N, Testa V, Capasso G, Sullo A. Calcific insertional Achilles tendinopathy: reattachment with bone anchors. Am J Sports Med. 2004;32:174–182. doi: 10.1177/0363546503258923. [DOI] [PubMed] [Google Scholar]
- 15.Vulpiani MC, Guzzini M, Ferretti A. Operative treatment of chronic Achilles tendinopathy. Int Orthop. 2003;27(5):307–310. doi: 10.1007/s00264-003-0472-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson KW, Zalavras C, Thordarson DB. Surgical management of insertional calcific Achilles tendinosis with a central tendon splitting approach. Foot Ankle Int. 2006;27(4):245–250. doi: 10.1177/107110070602700404. [DOI] [PubMed] [Google Scholar]
- 17.McGarvey WC, Palumbo RC, Baxter DE, Leibman BD. Insertional Achilles tendinosis: surgical treatment through a central tendon splitting approach. Foot and Ankle Int. 2002;23(1):19–25. doi: 10.1177/107110070202300104. [DOI] [PubMed] [Google Scholar]
- 18.Schepsis AA, Leach RE. Surgical management of Achilles tendon overuse injuries. Am J Sports Med. 1994;22:611–619. doi: 10.1177/036354659402200508. [DOI] [PubMed] [Google Scholar]
- 19.Wagner E, Gould JS, Kneidel M, Fleisig GS, Fowler R. Technique and results of Achilles tendon detachment and reconstruction for insertional Achilles tendinosis. Foot Ankle Int. 2006;27(9):677–684. doi: 10.1177/107110070602700904. [DOI] [PubMed] [Google Scholar]