Abstract
Objective
Delirium is associated with poor outcomes following acute hospitalization. A specialized delirium management unit, the Geriatric Monitoring Unit (GMU), was established. Evening bright light therapy (2000–3000 lux; 6–10 pm daily) was added as adjunctive treatment, to consolidate circadian activity rhythms and improve sleep. This study examined whether the GMU program improved sleep, cognitive, and functional outcomes in delirious patients.
Method
A total of 228 patients (mean age = 84.2 years) were studied. The clinical characteristics, delirium duration, delirium subtype, Delirium Rating Score (DRS), cognitive status (Chinese Mini–Mental State Examination), functional status (modified Barthel Index [MBI]), and chemical restraint use during the initial and predischarge phase of the patient’s GMU admission were obtained. Nurses completed hourly 24-hour patient sleep logs, and from these, the mean total sleep time, number of awakenings, and sleep bouts (SB) were computed.
Results
The mean delirium duration was 6.7 ± 4.6 days. Analysis of the delirium subtypes showed that 18.4% had hypoactive delirium, 30.2% mixed delirium, and 51.3% had hyperactive delirium. There were significant improvements in MBI scores, especially for the hyperactive and mixed delirium subtypes (P < 0.05). Significant improvements were noted on the DRS sleep–wake disturbance subscore, for all delirium-subtypes. The mean total sleep time (7.7 from 6.4 hours) (P < 0.05) and length of first SB (6.0 compared with 5.3 hours) (P < 0.05) improved, with decreased mean number of SBs and awakenings. The sleep improvements were mainly seen in the hyperactive delirium subtype.
Conclusion
This study shows initial evidence for the clinical benefits (longer total sleep time, increased first SB length, and functional gains) of incorporating bright light therapy as part of a multicomponent delirium management program. The benefits appear to have occurred mainly in patients with hyperactive delirium, which merits further in-depth, randomized controlled studies.
Keywords: sleep, delirium, function, elderly
Introduction
Delirium is a common and serious condition in older hospitalized patients. The prevalence in hospitalized elderly patients is as high as 50%, being present in 11%–24% of older patients at admission, with another 5%–35% developing delirium during admission.1,2 It is an indicator of severe underlying illness, necessitating early diagnosis and prompt treatment. Despite varying etiologies, delirium has a characteristic constellation of symptoms, suggesting a common neural pathway. Importantly, motor symptoms are core symptoms, associated with cognitive impairments and sleep disturbances.
The usually cited factors for delirium include advanced age, preexisting cognitive impairment, serious medical conditions, medications (such as benzodiazepines), environmental factors, and sleep deprivation. Attention and memory impairment have been observed after periods of total and partial sleep deprivation,3,4 suggesting a mechanistic relationship between delirium and sleep deprivation that may be mediated through involvement of the cholinergic and dopaminergic systems, although direct relationship between the two remains to be fully elucidated. Most of the available literature on delirium and sleep have involved intensive care unit patients. Critically ill patients, especially older adults, are known to experience poor sleep quality, with severe sleep fragmentation and sleep architecture disruption.5,6
Delirium is associated with an increased need for nursing surveillance, greater hospital costs, and high mortality rates of 25%–33% during hospitalization and 35%–40% at 1 year.7–12 In partial response to this, the Geriatric Monitoring Unit (GMU) was developed in October 2010 at the Tan Tock Seng Hospital, Singapore, using an evidence-based approach incorporating specific interventions established to be beneficial for delirium care. The details of the GMU have been published previously.13 To summarize, the GMU incorporated specific measures from the following programs: (1) Delirium Room, which provides comprehensive medical care, with multidisciplinary team meetings, and employs behavioral and appropriate nonpharmacological strategies as first-line management in delirious patients,14 (2) the concept of structured core interventions from the Hospital Elder Life Program (HELP),15–22 and (3) bright light therapy to establish a healthy sleep–wake cycle, with appropriate timing to effectively shift an altered circadian sleep–wake cycle to the desired phase.
Bright light therapy has gained increasing attention in recent years, as a potential environmental modifier (zeitgeber) of circadian rhythms. Additionally, therapeutic benefits have been demonstrated in terminally ill patients,23 as well as those with seasonal affective disorders.24 In elderly patients with advanced sleep phase syndrome, evening exposure to bright light daily has been demonstrated to be beneficial.25–31 This can be achieved using a bright light box of 1000–3000 lux or natural exposure to the sun for 1–2 hours daily in the late afternoon and early evening. The aim of bright light therapy is to establish healthy sleep–wake cycles. A recent study demonstrated the utility of light therapy in adjusting the rest–activity cycle and improving bed rest in postesophagectomy patients, with decreased occurrences of incident delirium.32 Since sleep deprivation may aggravate delirium, it was anticipated that delirious patients would benefit from modulation of their sleep–wake cycle, while in the GMU. The peaceful environment of the GMU (without potential disruption by other patients) would facilitate uninterrupted sleep at night, while structured core interventions (with therapeutic activities) aimed to keep patients engaged in the day.
This study examined the impact of the GMU as a multicomponent intervention on outcomes of sleep, cognitive, and functional performance, in acute, hospitalized delirious older adults.
Methods
Subjects
We recruited 228 delirious patients who had been admitted to the GMU, Department of Geriatric Medicine, Tan Tock Seng Hospital, Singapore between December 2010 to August 2012. The subjects were classified into a hyperactive, hypoactive, and mixed delirium subtype, based on their activity patterns. A patient was deemed to have recovered from delirium if the Confusion Assessment Method (CAM)33 criteria were no longer met, with the diagnosis of recovery being supported by improvement in cognitive and/or delirium severity scores, based on the Delirium Rating Score–R98 (DRS-R98) 34 and CAM-severity scores as well as input from the multidisciplinary team.
Inclusion/exclusion
The admission criteria for the GMU included patients above 65 years old who were admitted to the geriatric medicine department and assessed to have delirium (either on admission or incident delirium during hospital stay), established in accordance with the CAM. Patients were excluded if they had medical illnesses that required special monitoring (eg, telemetry for arrhythmias or acute myocardial infarction); were assessed to be dangerously ill, in a coma, or had a terminal illness; uncommunicative or diagnosed with severe aphasia; demonstrated severely combative behavior with high risk of harm; or had contraindications to bright light therapy (manic disorders, severe eye disorders, photosensitive skin disorders, or use of photosensitizing medications). Patients with respiratory or contact precautions, and those with verbal refusal of GMU admission by family/patient/attending physician were also excluded. Patients who were prematurely transferred out of the GMU (for reasons such as instability of medical conditions requiring intensive monitoring, or new requirement of contact precautions) were excluded from subsequent analysis.
Ethics approval for the study was obtained from a National Healthcare Group domain specific review board (DSRB).
Procedure
The GMU consisted of a five-bed unit with a specific elder-friendly room design and lower staff-patient ratios. In addition, core interventions adopted from the HELP program (standardized protocols for managing cognitive impairment, sleep deprivation, immobility, visual impairment, hearing impairment, and dehydration) were systematically administered. Bright light therapy (2000–3000 lux) was administered via lights installed in the ceiling and turned on from 6–10 pm daily. Sleep hygiene principles were also practiced during patients’ GMU stay. All interventions were delivered in accordance with a semistructured protocol, by trained geriatric nurses in GMU, with full (100%) compliance achieved.
We collected data on patient demographics (age, gender, race, length of hospital stay [LOS]), duration of delirium [in days], the medical comorbidities and severity of illness (using a modified Charlson Comorbidity Index35 and modified Severity of Illness Index),36 and the precipitating causes of delirium. Cognitive status was assessed using a locally validated Chinese Mini–Mental State Examination (CMMSE)37 and functional status using a modified Barthel Index (MBI),38 both administered by a trained assessor during the initial and predischarge phases of the patient admission. The rate and frequency of chemical restraint use was reviewed. As the GMU was a mechanical restraint–free unit, none of the patients in the GMU were subject to physical restraint. To adjust for the different antipsychotics prescribed, we used chlorpromazine equivalence39 to assess the total antipsychotic usage during the admission and also charted the frequency of benzodiazepine use.
Cognitive assessment
All patients underwent a detailed cognitive evaluation by the consultant geriatrician (specializing in cognitive and memory disorders) upon admission to the GMU. A family member or other designated caregiver was routinely interviewed to establish the patient’s baseline cognitive functioning prior to the current admission. The medical records of all patients were reviewed to ascertain whether a diagnosis of dementia had been previously established. In patients yet to be diagnosed, a diagnosis of dementia was made in the current admission if the corroborative history suggested presence of cognitive symptoms consistent with DSM-IV criteria for dementia40 of at least 6-months duration, in accordance with the standardized process for cognitive evaluation.41
Sleep data collection
Eight specially-trained GMU nurses completed hourly patient sleep logs during the subjects’ stay in the GMU, as part of routine clinical care. The total sleep time (TST), number of awakenings, number of sleep bouts (SB), and the length of each SB was computed from the 24-hour sleep log data on admission and discharge from the GMU.
Statistical analysis
We evaluated the clinical characteristics, cognitive assessment scores, functional status, and the use of pharmacological agents for the entire cohort of GMU patients and compared among delirium subtypes, using analysis of variance (ANOVA) with Bonferroni correction and Chi-square tests for the continuous and categorical variables, respectively. Sleep parameters for the whole group and delirium subtypes were computed and the differences in the sleep data on discharge and admission were compared using paired-sample t-tests. We additionally analyzed the sleep parameters, adjusted for comorbidities, delirium days, and chemical restraint use. Statistical significance was taken to be P < 0.05.
Statistical analyses were performed using SPSS 16.0 software (SPSS, Inc, Chicago, IL, USA).
Results
Demographics
A total of 228 patients were included in the analyses. We excluded 16 subjects who failed screening criteria, 26 subjects whose family members declined GMU admission, and 31 subjects who were prematurely transferred out of GMU due to their medical condition. There were no age, gender, or ethnic differences between the study group and those excluded from the analyses. The majority of patients had hyperactive delirium (n = 117), followed by mixed delirium (n = 69) and hypoactive delirium (n = 42). The mean age was 84.2 ± 7.4 years, and participants were predominantly female (56.4%) and of Chinese ethnicity (88.2%). There were no significant age, gender, or racial differences between the delirium subtypes (Table 1).
Table 1.
Clinical characteristics, cognitive and functional outcomes in GMU patients (n = 228) at baseline
| Total (n = 228) | Hyperactive (n = 117) | Hypoactive (n = 42) | Mixed (n = 69) | |
|---|---|---|---|---|
| Demographics | ||||
| Age (mean ± SD) | 84.2 (7.4) | 83.6 (7.5) | 84.9 (7.8) | 84.7 (6.9) |
| Gender (male %) | 43.4 | 42.7 | 47.6 | 42.0 |
| Race (Chinese %) | 88.2 | 93.2 | 80.9 | 84.1 |
| Comorbidities | ||||
| Charlson Comorbidity Index score35 | 2.3 (1.6) | 1.9 (1.3)+ | 2.9 (2.20) | 2.5 (1.6)* |
| Severity of Illness Index score36 | 2.0 (0.3) | 2.1 (0.2) | 2.0 (0.3) | 2.0 (0.4) |
| Days of delirium | 6.7 (4.6) | 5.8 (3.1) | 7.3 (6.0) | 7.9 (5.6)*,# |
| Length of stay | 15.1 (9.3) | 13.9 (7.1) | 15.0 (10.4) | 16.6 (11.4) |
| Precipitating causes of delirium | ||||
| Number of precipitating causes, n (%) | ||||
| Single precipitating cause | 67 (29.4%) | 34 (29.1%) | 9 (21.4%) | 24 (34.8%) |
| Two precipitating causes | 72 (31.6%) | 38 (32.5%) | 13 (31.0%) | 21 (30.4%) |
| More than two precipitating causes | 89 (39.0%) | 45 (38.5%) | 20 (47.6%) | 24 (34.8%) |
| Type of precipitating cause, n (%) | ||||
| Sepsis | 155 (68.0%) | 75 (64.1%) | 29 (69.0%) | 51 (73.9%) |
| Other medical cause | 48 (21.1%) | 28 (23.9%) | 8 (19.0%) | 12 (17.4%) |
| Postoperative | 7 (3.1%) | 4 (3.4%) | 1 (2.4%) | 2 (2.9%) |
| Other surgical cause | 18 (7.9%) | 10 (8.5%) | 4 (9.5%) | 4 (5.8%) |
| Cognitive status | ||||
| Prior dementia diagnosis (%) | 46.1 | 44.4 | 45.2 | 49.3 |
| Newly diagnosed dementia during admission (%) | 30.3 | 33.3 | 33.3 | 23.1 |
| Prior behavioral issues before admission (%) | 25.1 | 27.4 | 9.8 | 30.4* |
| Initial CMMSE37 (/28) | 5.8 (5.5) | 6.9 (5.9)+ | 4.3 (5.3) | 4.9 (4.4)* |
| Last CMMSE (/28) | 9.2 (6.6) | 10.5 (6.4) | 7.8 (7.2)++ | 7.9 (6.0)* |
| Change in CMMSE (/28) | 3.4 (5.5) | 3.6 (5.2) | 3.5 (6.6) | 3.0 (5.3) |
| Initial CAM33 | 5.1 (2.0) | 5.2 (2.5) | 5.3 (1.2) | 5.0 (1.2) |
| Last CAM | 2.2 (1.2) | 1.9 (0.9) | 2.3 (1.3) | 2.5 (1.4) |
| Change in CAM | −2.9 (2.3) | −3.2 (2.7) | −3.0 (1.4) | −2.4 (1.8) |
| Initial DRS severity34 (/39) | 22.5 (5.8) | 21.6 (6.3) | 23.1 (5.6) | 23.6 (4.7) |
| Last DRS severity (/39) | 14.6 (6.1) | 13.5 (95.5) | 16.0 (7.0) | 15.4 (6.3)* |
| Change in DRS severity (/39) | −6.2 (6.3) | −6.4 (5.8) | −5.3 (6.2) | −6.2 (7.1) |
| Initial DRS total (/46) | 26.2 (6.1) | 25.3 (6.5) | 26.9 (5.7) | 27.3 (5.4) |
| Last DRS total (/46) | 16.3 (6.7) | 15.2 (5.9) | 17.8 (7.7) | 17.2 (7.2) |
| Change in DRS total (/46) | −11.6 (6.1) | −11.7 (5.9) | −10.9 (5.7) | −11.8 (6.9) |
| Initial DRS subitem sleep–wake disturbance (/3) | 1.9 (0.8) | 1.8 (0.8) | 1.9 (0.9) | 1.9 (0.6) |
| Last DRS subitem sleep–wake disturbance (/3) | 0.7 (0.8) | 0.7 (0.8) | 0.6 (0.7) | 0.6 (0.9) |
| Change in DRS subitem sleep–wake disturbance (/3) | −1.2 (1.1)** | −1.1 (1.1)** | −1.3 (0.9)** | −1.4 (1.3)** |
| Functional scores | ||||
| MBI38 admission (/100) | 29.1 (24.1) | 36.8 (25.9) | 16.9 (18.7) | 23.4 (19.2)* |
| MBI discharge (/100) | 47.4 (26.1) | 56.4 (22.5) | 30.9 (26.3) | 42.3 (25.7)* |
| Improvement in MBI scores | 18.4 (18.1)** | 19.6 (18.6)** | 14.0 (2.5)** | 19.0 (18.4)** |
| Pharmacological agent use | ||||
| Chemical restraints (%) | 39.5 | 47.9 | 9.5 | 43.5* |
| Total antipsychotic use (CPZ equivalent) | 0.9 (1.6) | 1.2 (1.6) | 0 (0) | 1.0 (1.7) |
| Benzodiazepine usage (%) | 24.6 | 26.5 | 9.5 | 30.4 |
Notes:
ANOVA P < 0.05 across delirium subtypes;
paired sample t-test P < 0.05 for GMU cohort and specific delirium subtypes;
post hoc results (with Bonferroni correction) between hyperactive delirium and hypoactive delirium (P < 0.05);
post hoc results (with Bonferroni correction) between hypoactive delirium and mixed delirium (P < 0.05);
post hoc results (with Bonferroni correction) between hyperactive delirium and mixed delirium (P < 0.05).
Abbreviations: ANOVA, analysis of variance; CAM, Confusion Assessment Method; CMMSE, Chinese Mini−Mental State Examination; CPZ, chlorpromazine; DRS, Delirium Rating Scale; GMU, Geriatric Monitoring Unit; MBI, modified Barthel Index; SD, standard deviation.
Patients with the hyperactive delirium subtype had significantly fewer comorbidities compared with those with hypoactive and mixed delirium (mean Charlson Comorbidity Index score 1.9, 2.9, and 2.5, respectively). Those with hyperactive delirium also had a significantly shorter mean duration of delirium (5.8 ± 3.1 days) compared with those with hypoactive and mixed delirium (7.3 ± 6.0 and 7.9 ± 5.6 days respectively). However, there were no significant differences in LOS across the delirium subtypes.
There were no significant differences in the prevalence of background dementia or number of precipitating causes of delirium. Sepsis was the predominant precipitating cause of delirium (64%–73.9%) among the delirium subtypes.
CMMSE
Although there were significant differences in CMMSE scores among the delirium subtypes on admission and discharge, there was no significant difference in the extent of improvement on the CMMSE nor in any of the delirium indicators among the delirium subtypes upon further analyses.
Functional status
There was significant improvement in functional status (MBI) at discharge, especially in the hyperactive and mixed delirium subtype (19.6 ± 18.6 and 19.0 ± 18.4 for the hyperactive and mixed delirium subtypes, respectively, compared with 14.0 ± 2.5 for the hypoactive delirium subtype) (P < 0.05).
Restraint and medication use
None of the subjects were physically restrained. There was decremental chemical restraint use across the hyperactive, mixed, and hypoactive delirium subtypes (47.9%, 43.5%, and 9.5%, respectively) (P < 0.001). However, benzodiazepine use exhibited a different decremental trend across the mixed, hyperactive, and hypoactive delirium subtypes (30.4%, 26.5%, and 9.5% respectively) (P = 0.23). (see Table 1).
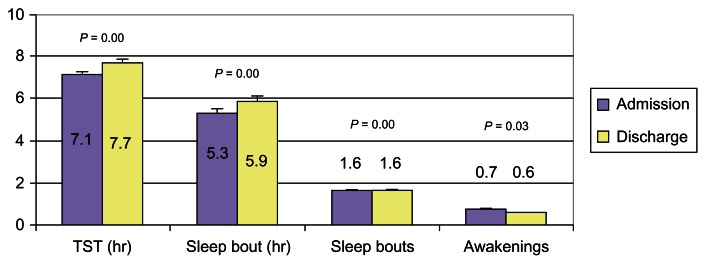
Sleep
All delirium subtypes showed significant improvement in the DRS sleep–wake disturbance subscore at discharge (Table 1). The GMU cohort also exhibited significant improvement in sleep parameters at discharge from the GMU compared with baseline, with increased TST (7.7 ± 2.5 hours versus 7.1 ± 2.9 hours) (P < 0.01), increased length of first SB (5.9 ± 3.6 hours versus 5.3 ± 3.7 hours) (P < 0.01), decreased number of SB (1.57 ± 0.8 versus 1.59 ± 0.9) (P < 0.01), and fewer number of awakenings (0.6 ± 0.8 versus 0.7 ± 0.8) (P = 0.03) (see Figure 1). In the subgroup analyses of delirium subtypes, there was a significant increase in TST (7.4 ± 2.4 hours versus 6.7 ± 2.8 hours) (P < 0.01) and decreases in number of SB (1.6 ± 0.8 versus 1.7 ± 0.9) (P < 0.01) and length of first SB (5.7 ± 3.4 versus 4.9 ± 3.5) (P = 0.002) for hyperactive delirium subtype. For hypoactive delirium, there was a small but significant increase in TST (7.8 ± 3.1 hours versus 7.7 ± 2.7 hours) (P = 0.05) (see Table 2). However, upon adjustment for comorbidity, duration of delirium, and chemical restraint use, the differences were no longer statistically significant for any of the sleep parameters except length of SB in hypoactive delirium (Table 2).
Figure 1.
GMU patient sleep data (n = 228).
Abbreviations: GMU, Geriatric Monitoring Unit; TST, total sleep time.
Table 2.
Sleep parameters for delirium subtypes of GMU patients
| Hyperactive (n = 117) | Hypoactive (n = 42) | Mixed (n = 69) | P-value (for change across delirium subtype) | Adjusted P-value^ (for change across delirium subtype) | Adjusted difference (P-value)^ Hyperactive |
Adjusted difference (P-value)^ Hypoactive |
Adjusted difference (P-value)^ Mixed |
|
|---|---|---|---|---|---|---|---|---|
| Initial total sleep time (hr) | 6.7 (2.8) | 7.7 (2.7) | 7.5 (3.0) | – | – | – | – | – |
| Last total sleep time (hr) | 7.4 (2.4) | 7.8 (3.1) | 8.1 (2.1) | – | – | – | – | – |
| Change in total sleep time (hr) | 0.7 (3.0)# | 0.1 (3.5)# | 0.7 (3.3) | 0.61 | 0.51 | 0.20 | 0.26 | 0.28 |
| Initial number of awakenings | 0.8 (0.8) | 0.6 (0.8) | 0.7 (0.8) | – | – | – | – | – |
| Last number of awakenings | 0.7 (0.8) | 0.3 (0.5) | 0.6 (0.8) | – | – | – | – | – |
| Change in number of awakenings | −0.1 (1.1) | −0.2 (0.8) | −0.1 (1.0) | 0.55 | 0.93 | 0.82 | 0.11 | 0.67 |
| Initial number of sleep bouts | 1.7 (0.9) | 1.5 (0.9) | 1.6 (0.8) | – | – | – | – | – |
| Last number of sleep bouts | 1.6 (0.8) | 1.3 (0.6) | 1.7 (0.9) | – | – | – | – | – |
| Change in number of sleep bouts | −0.04 (1.1)# | −0.2 (0.9) | 0.1 (1.1) | 0.41 | 0.95 | 0.82 | 0.11 | 0.74 |
| Length of first sleep bout (hr) | 4.9 (3.5) | 5.7 (3.9) | 5.8 (3.8) | – | – | – | – | – |
| Last length of first sleep bout (hr) | 5.7 (3.4) | 6.6 (3.9) | 6.0 (3.7) | – | – | – | – | – |
| Change in length of sleep bout (hr) | 0.8 (4.2)# | 0.9 (4.6) | 0.2 (4.8) | 0.60 | 0.57 | 0.35 | 0.01 | 0.38 |
Notes:
Statistically significant differences in change across the sleep parameters (total sleep time, number of awakenings, number of sleep bouts, and length of first sleep bout) for the specific delirium subtype;
differences adjusted for Charlson Comorbidity Index,35 days of delirium, and use of chemical restraints.
Abbreviation: GMU, Geriatric Monitoring Unit.
Discussion
Our study contributes to the presently still limited literature on sleep outcomes following interventions in delirious older hospitalized adults, with demonstrated improvements in sleep and functional outcomes using bright light therapy as part of a multicomponent intervention program provided in the GMU.
We found significant improvements, with longer TST at night, increased length of the first SB, and decreased number of SBs and thus fewer awakenings in delirious older hospitalized adults admitted to the GMU. The sleep–wake disturbance measured on DRS-subscores also improved, indicating likely consolidation of sleep rhythms. This may be attributed to the increased physical activity, mental stimulation via reorientation, and structured activity programs in the day, along with evening bright light therapy as well as adherence to sleep hygiene principles during the GMU stay.
Of important clinical relevance were the short-term functional improvements, evident in the improvements achieved on MBI for all delirious subtypes, especially in the hyperactive delirium and mixed delirium subtypes. This will promote the geriatric management principles of early intervention and mobilization, and avoidance of physical restraint use, to prevent the complications of hospitalization and immobility.42 The mean LOS of 15.1 ± 9.3 days in the acute hospital setting compares favorably with the 20.9 ± 2.1 days observed for delirious hospitalized older adults prior to the establishment of the GMU (point prevalence survey). The LOS was longer compared with that of US hospitals due to the funding, subvention structure, and models of geriatric care.
Interestingly, we noted phenomenological differences in delirious patients, where background dementia and behavioral issues prior to admission were more common in hyperactive and mixed delirium. This also related to the nonsignificant differences noted in sedative-hypnotic usage during the delirium episode. This interesting phenomenon is yet to be fully understood in delirium, although Cunningham and MacLullich43 suggested delirium could be a maladaptive sickness behavioral response, with psychoneuroimmunological changes occurring with a systemic inflammation (for example infection) to manifest severe deleterious effects on brain function (during old age or in the presence of neurodegenerative disease). It was not unexpected that cognitive scores and DRS rating remained impaired despite a clinical impression of delirium resolution and adequate treatment of acute precipitating factors, thus supporting the concept of subsyndromal delirium,44 even in the resolution stage, and the findings of longer-term cognitive impairment following a delirium episode.
There were some limitations to this study. Since all patients were given the treatment protocol, there was no control group. These results need to be replicated in a randomized controlled study. Sleep parameters were collected via nurse observations through 24-hour sleep logs, with no objective data collected. However, this was a specialized unit with trained GMU nurses completing the sleep logs thus decreasing the risk of observer bias. We were not able to examine circadian activity rhythm changes without the use of wrist actigraphy and therefore could not ascertain whether this multicomponent program would restore rhythms in the delirious hospitalized elderly. Lastly, given that the interventions were performed on all the patients, with 100% compliance, we are not able to accurately delineate the benefits of the individual components of this multicomponent intervention program.
In summary, we have demonstrated improvements in short-term outcomes related to improved function and sleep in delirious hospitalized older adults, in a real-life geriatric setting with bright light therapy as part of a multicomponent delirium program. Longitudinal follow up of cognitive and sleep outcomes and further studies of pharmacologic agents that may help restore sleep and circadian rhythms in delirious hospitalized older adults and the delirium subtypes would facilitate further understanding of this complex phenomenon.
Acknowledgments
We would like to thank the GMU nurses and multidisciplinary team involved in the GMU.
This study was funded by FY2010 Ministry of Health Quality of Improvement Funding (MOH HQIF) “Optimising Acute Delirium Care in Tan Tock Seng Hospital” (Grant No HQIF 2010/17). CMS is supported by the National Healthcare Group (NHG) Clinician Scientist Career Scheme 2012/12002.
Footnotes
Disclosure
Dr Ancoli-Israel received a loan of light boxes from Lightbook, Inc for other research she is conducting. The authors report no conflicts of interest in this work.
References
- 1.Agnostini JV. Inouye Sk. Delirium. In: Hazzard WR, Blass JP, Halter JB, Ouslander JG, Tinetti ME, editors. Principles of Geriatric Medicine and Gerontology. 5th ed. New York: McGraw-Hill; 2003. pp. 1503–1515. [Google Scholar]
- 2.Inouye SK. Delirium in hospitalized older patients. Clin Geriatr Med. 1998;14(4):745–764. [PubMed] [Google Scholar]
- 3.Mograss MA, Guillem F, Brazzini-Poisson V, Godbout R. The effects of total sleep deprivation on recognition memory processes: a study of event-related potential. Neurobiol Learn Mem. 2009;91(4):343–352. doi: 10.1016/j.nlm.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Fisher S. The microstructure of dual-task interaction. Sleep deprivation and the control of attention. Perception. 1980;9(3):327–337. doi: 10.1068/p090327. [DOI] [PubMed] [Google Scholar]
- 5.Feedman NS, Gazendam J, Leval L, Pack AI, Schwab RJ. Abnormal sleep/wake cycles and the effect of environmental noise on sleep disruption in the intensive care unit. Am J Respir Crit Care Med. 2001;163(2):451–457. doi: 10.1164/ajrccm.163.2.9912128. [DOI] [PubMed] [Google Scholar]
- 6.Gabor JY, Cooper AB, Cromback SA, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med. 2003;167(5):708–715. doi: 10.1164/rccm.2201090. [DOI] [PubMed] [Google Scholar]
- 7.Cole MG, Primeau FJ. Prognosis of delirium in elderly hospital patients. CMAJ. 1993;149(1):41–46. [PMC free article] [PubMed] [Google Scholar]
- 8.Moran JA, Dorevitch MI. Delirium in the hospitalised elderly. Aust J Hosp Pharm. 2001;31:35–40. [Google Scholar]
- 9.Murray AM, Levkoff SE, Wetle TT, et al. Acute delirium and functional decline in the hospitalized elderly patient. J Gerontol. 1993;48(5):M181–M186. doi: 10.1093/geronj/48.5.m181. [DOI] [PubMed] [Google Scholar]
- 10.Inouye SK, Viscoli CM, Horwitz RI, Hurst LD, Tinetti ME. A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Int Med. 1993;119(6):474–481. doi: 10.7326/0003-4819-119-6-199309150-00005. [DOI] [PubMed] [Google Scholar]
- 11.McAvay GJ, Van Ness PH, Bogardus ST, Jr, et al. Older adults discharged from the hospital with delirium: 1-year outcomes. J Am Geriatr Soc. 2006;54(8):1245–1250. doi: 10.1111/j.1532-5415.2006.00815.x. [DOI] [PubMed] [Google Scholar]
- 12.Leslie DL, Zhang Y, Bogardus ST, Holford TR, Leo-Summers LS, Inouve SK. Consequences of preventing delirium in hospitalized older adults on nursing home costs. J Am Geriatr Soc. 2005;53(3):405–409. doi: 10.1111/j.1532-5415.2005.53156.x. [DOI] [PubMed] [Google Scholar]
- 13.Chong MS, Chan MP, Kang J, Han HC, Ding YY, Tan TL. A new model of delirium care in the acute geriatric setting: geriatric monitoring unit. BMC Geriatr. 2011;11:41. doi: 10.1186/1471-2318-11-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flaherty JH, Tariq SH, Raghavan S, Bakshi S, Moinuddin A, Morley JE. A model for managing delirious older inpatients. J Am Geriatr Soc. 2003;51(7):1031–1035. doi: 10.1046/j.1365-2389.2003.51320.x. [DOI] [PubMed] [Google Scholar]
- 15.Lunström M, Edlund A, Karlsson, Brännström B, Bucht G, Gustafson Y. A multifactorial intervention program reduces the duration of delirium, length of hospitalization, and mortality in delirious patients. J Am Geriatr Soc. 2005;53(4):622–628. doi: 10.1111/j.1532-5415.2005.53210.x. [DOI] [PubMed] [Google Scholar]
- 16.Pitkälä KH, Laurila JV, Strandberg TE, Tilvis RS. Multicomponent geriatric intervention for the elderly inpatients with delirium: a randomized, controlled trial. J Gerontol A Biol Sci Med Sci. 2006;61(2):176–181. doi: 10.1093/gerona/61.2.176. [DOI] [PubMed] [Google Scholar]
- 17.Pitkala KH, Laurila JV, Strandberg TE, Kautiainen H, Sintonen H, Tilvis RS. Multicomponent geriatric intervention for elderly inpatients with delirium: effects on costs and health-related quality of life. J Gerontol A Biol Sci Med Sci. 2008;63(1):56–61. doi: 10.1093/gerona/63.1.56. [DOI] [PubMed] [Google Scholar]
- 18.Inouye SK, Bogardus ST, Jr, Charpentier PA, et al. A Multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–676. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- 19.Inouye SK, Bogardus ST, Jr, Baker DI, Leo-Summers L, Cooney LM., Jr The Hospital Elder Life Program: A model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life Program. J Am Geriatr Soc. 2000;48(12):1697–1706. doi: 10.1111/j.1532-5415.2000.tb03885.x. [DOI] [PubMed] [Google Scholar]
- 20.Inouye SK, Baker DI, Fugal P, Bradley EH HELP Dissemination Project. Dissemination of the Hospital Elder Life Program: implementation, adaptation, and successes. J Am Geriatr Soc. 2006;54(10):1492–1499. doi: 10.1111/j.1532-5415.2006.00869.x. [DOI] [PubMed] [Google Scholar]
- 21.Bradley EH, Webster TR, Schlesinger M, Baker D, Inouye SK. Patterns of diffusion of evidence-based clinical programmes: a case study of the Hospital Elder Life Program. Qual Saf Health Care. 2006;15(5):334–338. doi: 10.1136/qshc.2006.018820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rubin FH, Williams JT, Lescisin DA, Mook WJ, Hassan S, Inouye SK. Replicating the Hospital Elder Life Program in a community hospital and demonstrating effectiveness using quality improvement methodology. J Am Geriatr Soc. 2006;54(6):969–974. doi: 10.1111/j.1532-5415.2006.00744.x. [DOI] [PubMed] [Google Scholar]
- 23.Cohen SR, Steiner W, Mount BM. Phototherapy in the treatment of depression in the terminally ill. J Pain Symptom Manage. 1994;9(8):534–536. doi: 10.1016/0885-3924(94)90116-3. [DOI] [PubMed] [Google Scholar]
- 24.Levitan RD. What is the optimal implementation of bright light therapy for seasonal affective disorder (SAD)? J Psychiatry Neurosci. 2005;30(1):72. [PMC free article] [PubMed] [Google Scholar]
- 25.Ancoli-Israel S, Martin JL, Kripke DF, Marler M, Klauber MR. Effect of light treatment on sleep and circadian rhythms in demented nursing home patients. J Am Geriatr Soc. 2002;50(2):282–289. doi: 10.1046/j.1532-5415.2002.50060.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burns A, Allen H, Tomenson B, Duignan D, Byrne J. Bright light therapy for agitation in dementia: a randomized controlled trial. Int Psychogeriatr. 2009;21(4):711–721. doi: 10.1017/S1041610209008886. [DOI] [PubMed] [Google Scholar]
- 27.Gammack JK. Light therapy for insomnia in older adults. Clin Geriatr Med. 2008;24(1):139–149. doi: 10.1016/j.cger.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 28.Martin JL, Marler MR, Harker JO, Josephson KR, Alessi CA. A multicomponent nonpharmacological intervention improves activity rhythms among nursing home residents with disrupted sleep/wake patterns. J Gerontol A Biol Sci Med Sci. 2007;62(1):67–72. doi: 10.1093/gerona/62.1.67. [DOI] [PubMed] [Google Scholar]
- 29.Fetveit A, Bjorvatn B. Bright-light treatment reduces actigraphic-measured daytime sleep in nursing home patients with dementia: a pilot study. Am J Geriatr Psychiatry. 2005;13(5):420–423. doi: 10.1176/appi.ajgp.13.5.420. [DOI] [PubMed] [Google Scholar]
- 30.Ancoli-Israel S, Gehrman P, Martin JL, Shochat, et al. Increased light exposure consolidates sleep and strengthens circadian rhythms in severe Alzheimer’s disease patients. Behav Sleep Med. 2003;1(1):22–36. doi: 10.1207/S15402010BSM0101_4. [DOI] [PubMed] [Google Scholar]
- 31.Skjerve A, Holsten F, Aarsland D, Bjorvatn B, Nygaard HA, Johansen IM. Improvement in behavioral symptoms and advance of activity acrophase after short-term bright light treatment in severe dementia. Psychiatry Clin Neurosci. 2004;58(4):343–347. doi: 10.1111/j.1440-1819.2004.01265.x. [DOI] [PubMed] [Google Scholar]
- 32.Ono H, Toguchi T, Kido Y, Fujino Y, Doki Y. The usefulness of bright light therapy for patients after oesophagectomy. Intensive Crit Care Nurs. 2011;27(3):158–166. doi: 10.1016/j.iccn.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 33.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the Confusion Assessment Method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 34.Trzepacz PT, Mittal D, Torres R, Kanary K, Norton J, Jimerson N. Validation of the Delirium Rating Scale-revised-98: comparison with the delirium rating scale and the cognitive test for delirium. J Neuropsychiatry Clin Neurosci. 2001;13(2):229–242. doi: 10.1176/jnp.13.2.229. [DOI] [PubMed] [Google Scholar]
- 35.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 36.Wong WC, Sahadevan S, Ding YY, Tan HN, Chan SP. Resource consumption in hospitalised, frail older patients. Ann Acad Med Singapore. 2010;39(11):830–836. [PubMed] [Google Scholar]
- 37.Sahadevan S, Lim PP, Tan NJ, Chan SP. Diagnostic performance of two mental status tests in the older Chinese: influence of education and age on cut-off values. Int J Geriatr Psychiatry. 2000;15(3):234–241. doi: 10.1002/(sici)1099-1166(200003)15:3<234::aid-gps99>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 38.Mahoney FI, Barthel DW. Functional Evaluation: The Barthel Index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 39.Atkins M, Burgess A, Bottomley C, Massino R. Chlorpromazine equivalents: a consensus of opinion for both clinical and research applications. Psychiatr Bull. 1997;21:224–226. [Google Scholar]
- 40.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 41.Chong MS, Sahadevan S. An evidence-based clinical approach to the diagnosis of dementia. Ann Acad Med Singapore. 2003;32(6):740–748. [PubMed] [Google Scholar]
- 42.Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118(3):219–223. doi: 10.7326/0003-4819-118-3-199302010-00011. [DOI] [PubMed] [Google Scholar]
- 43.Cunningham C, Maclullich AM. At the extreme end of the psychoneuroimmunological spectrum: delirium as a maladaptive sickness behaviour response. Brain Behav Immun. 2013;28:1–13. doi: 10.1016/j.bbi.2012.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Trzepacz PT, Franco JG, Meagher DJ, et al. Phenotype of subsyndromal delirium using pooled multicultural Delirium Rating Scale – Revised-98 data. J Psychosom Res. 2012;73(1):10–17. doi: 10.1016/j.jpsychores.2012.04.010. [DOI] [PubMed] [Google Scholar]